Abstract
Fusarium spp are non-dermatophytic hyaline moulds found as saprophytes and plant pathogens. Human infections are probably a result of various precipitating predisposing factors of impaired immune status. Immunocompetent individuals of late are also vulnerable to various unassuming saprophytic and plant pathogens. To stress the need to identify correctly and institute appropriate antifungal therapy in newly emerging human fungal infectious agents. Repeated mycological sampling of the skin and nails of the suspected fungal infection were processed as per the standard format including direct microscopy and fungal culture on Sabouraud's dextrose agar. The fungus was isolated as Fusarium solani. Fusarium is an important plant pathogen and soil saprophyte. Infection is acquired by direct inoculation or inhalation of spores. It is associated with a variety of diseases like keratitis, onychomycosis, eumycetoma, skin lesions and disseminated diseases.
Keywords: Fusarium solani, onychomycosis, agriculturists, immunocompetent individuals
Introduction
Fungal infection may occur following trauma or wound contamination.[1] New opportunistic pathogens have now emerged as a cause of life-threatening infections worldwide. Fusarium is associated with a high mortality and may respond to novel therapies. Disseminated fusariosis is seen in high-risk patients with hematological cancers,[2,3] organ transplant recipients and in burns injuries.[4] However, little is known about the pathogenesis, clinical characteristics and management of these infections.[2] We report here three cases of fusariosis in individuals with normal immune status.
Case Reports
The following cases had come to the dermatology OPD of a medical college hospital. All patients were diagnosed based on repeat mycological examination by direct microscopy and fungal culture. Samples of nail and skin plaques previously cleaned with 70% alcohol were collected with a sterilized scalpel. Ten percent KOH wet mount of the sample was examined followed by inoculation onto Sabourauds dextrose agar.
Case 1
A 50-year-old male diagnosed presumptively as onychomycosis presented with a white superficial lesion on the right index finger. The lesions appeared 4 months back. There was no history of itching, pain or discharge from the lesion.
Case 2
A 70-year-old male presented with erythematous scaly plaques on the left little finger since 3 years with no itching, pain and discharge from the lesion.
Case 3
A 45-year-old male presented with interdigital plaques on the right foot since 5-6 years with no itching, pain or exacerbation.
Direct wet mounts revealed hyaline, septate, branched hyphae. Culture on Sabouraud's dextrose agar grew white, cottony colonies which later turned pink in color. Lactophenol cotton blue mount of colony revealed septate, branched hyphae with microconidia and many sickle shaped macroconidia [Figure 1]. The fungus was identified as Fusarium solani. All the cases were treated with oral Itraconazole 200 mg per day for 2 months and significant clinical and mycological recovery was achieved in all three cases.
Figure 1.
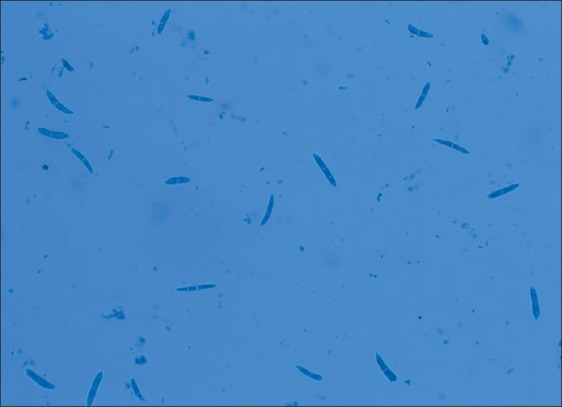
Fusarium solani in lactophenol cotton blue stain
Discussion
Onychomycosis is caused by dermatophytes and non dermatophyte fungi like Acremonium, Altenaria, Aspergillus, Scytalidium, Fusarium and Candida species.[5] Fusarium is a large genus of filamentous fungi widely distributed in soil and in association with plants. Most species are harmless saprobes, relatively abundant members of the soil microbial community.[6]
Some species may cause a range of opportunistic infections in humans. In humans with normal immune systems, fusarial infections may occur in the nails and in the cornea. Onychomycosis by Fusarium species usually involves the toe nails and enter the body through trauma. This was noted in two of our cases and the likely route of entry was probably due to trauma as both patients were agriculturists.[7]
Fusarial onychomycosis is seen as white superficial lesions in immunocompetent patients, with these lesions presenting as only a cosmetic effect requiring long-term treatment but in immunocompromised patients they can cause disseminated infections with poor response to antifungals. Disseminated infections are seen in patients with hematological malignancies[2,5,4] and even extensive burns.[4] In immunocompromised individuals, onychomycosis may act as a portal for life-threatening systemic infection.[3] These infections require proper identification and early treatment. Hence, severely immunocompromised patients with skin or other tissue breakdown conditions should avoid exposure to environmental sources of Fusarium species like tap water and soil which may be potentially contaminated with Fusarium species.[7]
Infections due to Fusarium involving skin and nails should be thoroughly investigated[8] in the laboratory down to the species level before discarding them as laboratory contaminants and reporting the same to the treating clinician keeping in mind the invasive potential[9] of this emerging pathogen so as to bring down mortality with appropriate treatment particularly among agricultural workers and laborers.[10]
![]()
Footnotes
Source of Support: Nil
Conflict of Interest: Nil.
References
- 1.Yu WK. Fusarium infection. Hong Kong Dermatol Venerol Bull. 2001;9:71–4. [Google Scholar]
- 2.Eleni IB, Elias JA. Fusarium a significant pathogen in patients with haematological malignancies. Blood. 1997;90:999–1008. [PubMed] [Google Scholar]
- 3.Krcmery V., Jr Fungemia due to Fusarium species in cancer patients. J Hosp Infect. 1997;36:223–8. doi: 10.1016/s0195-6701(97)90197-3. [DOI] [PubMed] [Google Scholar]
- 4.Dignani MC, Anaissie E. Human fusariosis. Clin Microbiol Inf. 2004;10:65–75. doi: 10.1111/j.1470-9465.2004.00845.x. [DOI] [PubMed] [Google Scholar]
- 5.Kaur R. Onychomycosis: Epidemiology, diagnosis and management. Indian J Med Microbiol. 2008;26:108–16. doi: 10.4103/0255-0857.40522. [DOI] [PubMed] [Google Scholar]
- 6.Elewski BE. Onychomycosis: Pathogenesis, diagnosis and management. Clin Microbiol Rev. 1998;11:415–29. doi: 10.1128/cmr.11.3.415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nucci M, Anaissie E. Cutaneous infection by Fusarium species in healthy and immunocompromised hosts: Implications for diagnosis and management. Clin Infect Dis. 2002;35:909–20. doi: 10.1086/342328. [DOI] [PubMed] [Google Scholar]
- 8.Nicacia BC. Fusarium of nail and skin infection: A report of eight cases from native Brazil. Mycopathologia. 2006;161:27–31. doi: 10.1007/s11046-005-0136-9. [DOI] [PubMed] [Google Scholar]
- 9.Godoy P. Onychomycosis caused by Fusarium solani and Fusarium oxysporum in Sao Paulo, Brazil. Mycopathologia. 2004;157:287–90. doi: 10.1023/b:myco.0000024186.32367.d4. [DOI] [PubMed] [Google Scholar]
- 10.Veer P. Study of onychomycosis.Prevailing fungi and pattern of infection. Indian J Med Microbiol. 2007;25:53–6. doi: 10.4103/0255-0857.31063. [DOI] [PubMed] [Google Scholar]


