Sir,
Cutaneous fungal infections have been reported worldwide as being one of the most common human infectious diseases in clinical practice. In spite of therapeutic advances in the last decades, the prevalence of cutaneous mycoses is still increasing.[1] The skin constitutes the main site of recognizable fungal infections in humans.[2]
The present study is undertaken with a view to identify and isolate the species of the fungi from the clinical specimens. One hundred and fifty patients, clinically suspected for dermatophytosis, attending the outpatient department of our hospital, who consented to the investigations, were studied for a period of 18 months after approval from the Institution Ethical Committee.
A detailed clinical history, general physical, and systemic examination were conducted in all cases and investigations were carried out whenever necessary. All new cases of dermatophytosis, who gave consent for required investigations, were included in the study after excluding patients on antifungal treatment and non-dermatophytic fungal infections.
The specimen collected was subjected to potassium-hydroxide (KOH) wet preparation of various concentrations depending on the type of clinical specimen for the presence of fungal elements. Following this, the specimen was inoculated into three sets of test tubes — Sabouraud dextrose agar with 0.05%, chloramphenicol with and without 0.5% cycloheximide, and the third to a dermatophyte test medium. If no growth was found after four weeks, it was taken as negative for growth of fungi.
Fungal isolates were identified based on the colony morphology, pigmentation, growth rate, microscopy, slide culture, urease test, hair perforation test, and rice grain test.
Incidence of dermatophytosis in the present study constitutes 6.09% among the patients attending the outpatient department of skin and STD. Dermatophytosis was common among the age group of 21-30 years (24%) with a male to female ratio of 1.94 : 1, which was similar to other studies by Singh S et al.[2] A majority of the patients were manual laborers (30.6%) from a rural background (54.6%) and belonged to the lower socioeconomic status (65.4%). Tinea corporis was the most common clinical type with 33.3%, and Tinea capitis was more common in the age group of less than 10 years (94.1%).
The results of KOH and fungal culture were as per Table 1. The clinicomycological correlation was seen in only 48.6% as in Table 2.
Table 1.
KOH and culture findings
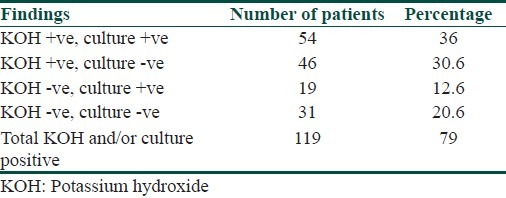
Table 2.
Dermatophytes isolated in relation to clinical types
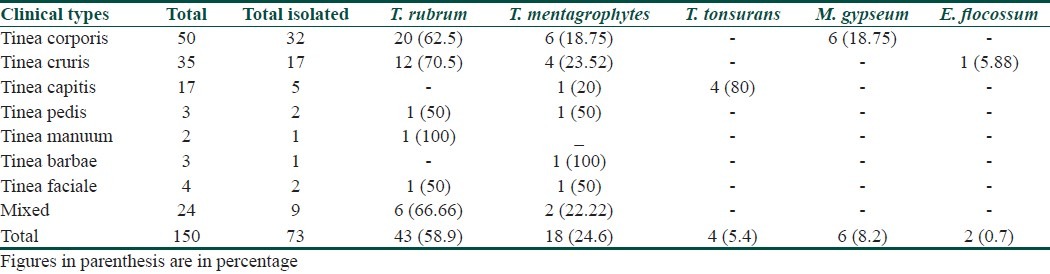
Trichophyton rubrum was the most common isolate (58.9%) followed by Trichophyton mentagrophytes (24.6%), which was comparable to a study by Venkatesan et al.[3] The highest culture isolate was seen in Tinea corporis, in 43.8% of the cases. These culture results were almost comparable with the studies by Bindu.[4] In the present study, however, the percentage of M. gypseum was higher, which could be due to the patients’ interaction with soil and domestic animals.
The Wood's lamp examination was performed in eight out of seventeen cases of tinea capitis. All the eight cases were negative for fluorescence. The common isolate of Tinea capitis in the present study was T. tonsurans (80%). The diagnosis of Tinea capitis caused by the Trichophyton species with Wood's lamp was difficult, as the infected hair did not exhibit the characteristic fluorescence.
To conclude, the present study shows that tinea corporis is the most common clinical type of dermatophytosis and Trichophyton rubrum is the most common isolate in this part of South Karnataka.
References
- 1.Valdigem GL, Pereira T, Macedo C, Duarte ML, Oliveira P, Ludovico P, et al. Atwenty year survey of dermatophytoses in Braga, Portugal. Int J Dermatol. 2006;45:822–7. doi: 10.1111/j.1365-4632.2006.02886.x. [DOI] [PubMed] [Google Scholar]
- 2.Singh S, Beena PM. Profile of dermatophyte infections in Baroda. Indian J Dermatol Venereol Leprol. 2003;69:281–3. [PubMed] [Google Scholar]
- 3.Venkatesan G, Singh R, Murugessan AG, Janaki C, Shankar GS. Trichophytonrubrum-the predominant etiological agent in humandermatophytoses in Chennai, India. Afr J Microbiol Res. 2007;1:9–12. [Google Scholar]
- 4.Bindu V. Clinico-mycological study of dermatophytosis in Calicut. Indian J Dermatol Venereol Leprol. 2002;68:259–61. [PubMed] [Google Scholar]


