Sir,
Association of systemic lupus erythematosus (SLE) or discoid lupus erythematosus (DLE) with human immuno-deficiency virus (HIV) infection in the same patient is rare. Both conditions have similar clinical and serologic features, making their coexistence a diagnostic and therapeutic challenge. Moreover, HIV infection appears to have a favorable impact in the clinical course of SLE. On the other hand, immunosuppressive therapy given for SLE activity has been associated with worsening of HIV infection.[1] We report a case of a HIV-infected patient, who developed extensive DLE and responded quickly to systemic hydroxychloroquine therapy.
A 55-year-old lady, house wife by occupation, detected to be HIV positive 6 months back with CD4 count 340 cells/mm3, not on antiretroviral therapy (ART), presented to our OPD with history of depigmented, asymptomatic skin lesions over the face and both the forearms of 2 months duration. They started as small papules and gradually evolved into larger, depigmented plaques with dry scaly surface. She complained of burning sensation in the lesions on exposure to sunlight. Her husband died 4 years back due to some HIV-related illness, details of which are not available.
Her general physical examination and systemic examinations were normal. Cutaneous examination revealed multiple, depigmented plaques measuring 2 cm × 1 cm to 5 cm × 4 cm, with dry surface covered with thick, grayish adherent scales, distributed over both the forearms [Figure 1], forehead, nose, and cheeks [Figure 2]. The carpet tag sign was positive. On investigation, routine blood and urine investigations were within normal limits. The ANA profile was negative. A biopsy taken from the lesion was subjected to histopathological examination which confirmed the diagnosis of DLF [Figure 3]. After complete ophthalmological examination, she was started on tablet hydroxychloroquine 200 mg twice daily. Within 3 weeks, all the lesions healed with postinflammatory depigmentation [Figures 4 and 5]. She was followed up for 4 months. There was no recurrence. Later on, her CD4 count dropped to below 200 and she was started on ART.
Figure 1.

Extensive discoid lupus erythematosus lesions over both the forearms
Figure 2.

Discoid lupus erythematosus lesions over the face
Figure 3.
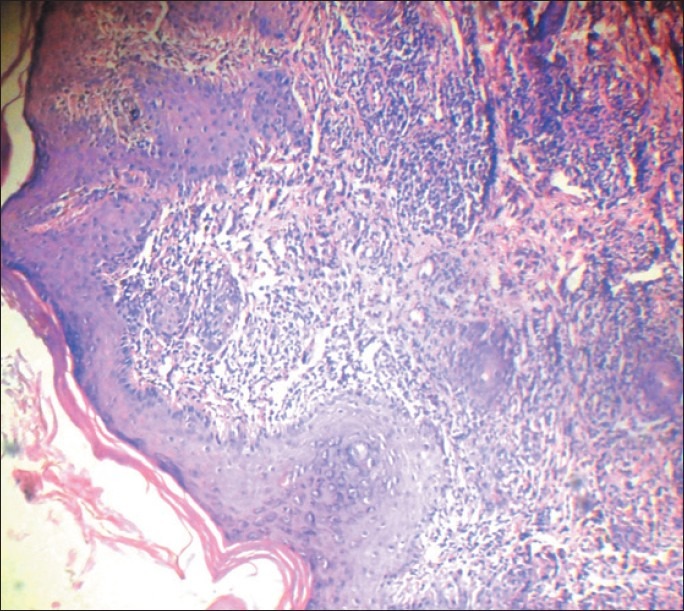
Histopathology showing follicular plugging and perivascular cuffing with lymphocytes
Figure 4.

DLE lesions over the face subsiding within 3 weeks after hydroxychloroquine monotherapy
Figure 5.

DLE lesions over the forearms subsiding within 3 weeks after hydroxychloroquine monotherapy leaving behind postinflammatory depigmentation
Although HIV infection is often associated with several rheumatic diseases, the coexistence of this retroviral infection and SLE is extremely uncommon. Generally, HIV-related immunosuppression improves SLE symptoms and ART may lead to an autoimmune disease flare subsequent to the increase of circulating CD4+ cell number. There are reports of SLE and DLE with HIV infection improving after initiation of ART.[2] Whereas, in our case, the lesions of DLE improved with hydroxychloroquine monotherapy and the patient was not on ART during the treatment with hydroxychloroquine. Many studies on cutaneous manifestations of HIV infection revealed that occurrence of DLF in HIV patients is rare.[3] There are reports of SLE and chronic cutaneous lupus erythematosus,[2,4,5] but occurrence of DLE with HIV infection appears to be extremely rare. We report this case for its rarity and peculiarity.
References
- 1.Colon M, Martinez DE. Clinical remission of systemic lupus erythematosus after human immunodeficiency virus infection. Puerto Rico Health SciJ. 2007;26:79–81. [PubMed] [Google Scholar]
- 2.Calza L, Manfredi R, Colangeli V, D’Antuono A, Passarini B, Chiodo F. Systemic and discoid lupus erythematosus in HIV-infected patients treated with highly active antiretroviral therapy. Int J STD AIDS. 2003;14:356–9. doi: 10.1258/095646203321605585. [DOI] [PubMed] [Google Scholar]
- 3.Supanaranond W, Desakorn V, Sitakalin C, Naing N, Chirachankul P. Cutaneous manifestations in HIV positive patients. Southeast Asian J Trop Med Public Health. 2001;32:171–6. [PubMed] [Google Scholar]
- 4.Montero A, Jorfen M, Arpini R. Chronic cutaneous lupus erythematosus and subsequent infection with HIV1. Mater Med Pol. 1992;24:21–3. [PubMed] [Google Scholar]
- 5.Palacios R, Santos J, Valdivielso P, Márquez M. Human immunodeficiency virus infection and systemic lupus erythematosus: An unusual case and a review of the literature. Lupus. 2002;11:60–3. doi: 10.1191/0961203302lu141cr. [DOI] [PubMed] [Google Scholar]


