Abstract
Many of the live human and animal vaccines that are currently in use are attenuated by virtue of their temperature-sensitive (TS) replication. These vaccines are able to function because they can take advantage of sites in mammalian bodies that are cooler than the core temperature, where TS vaccines fail to replicate. In this article, we discuss the distribution of temperature in the human body, and relate how the temperature differential can be exploited for designing and using TS vaccines. We also examine how one of the coolest organs of the body, the skin, contains antigen-processing cells that can be targeted to provoke the desired immune response from a TS vaccine. We describe traditional approaches to making TS vaccines, and highlight new information and technologies that are being used to create a new generation of engineered TS vaccines. We pay particular attention to the recently described technology of substituting essential genes from Arctic bacteria for their homologues in mammalian pathogens as a way of creating TS vaccines.
Keywords: Essential gene, Psychrophile, Vaccine, Temperature-sensitive, Body temperature
Introduction
Despite years of advances in the field of vaccines, the fact remains that most vaccines cannot offer the immunity gained from a real infection, which, provided the patient survives, often gives life-long immunity to that disease. This observation, paired with the idea that immunity to some diseases can be induced by a live vaccine but not by a killed or component vaccine, has long suggested that optimal protection requires vaccination with live, replicating organisms or viruses. Killed or subunit vaccines are especially poor in preventing disease caused by pathogens that require a Type 1 helper T cell response (Th1 response) to activate cytotoxic T cells. For this class of pathogens, a common approach is to engineer attenuated forms of the organism by inactivating virulence factors. Prominent examples of attenuated live vaccines include the Bacillus Calmette-Guérin (BCG) [1] vaccine for tuberculosis and the Ty21a vaccine for typhoid fever [2].
Another common approach to contain a live vaccine is to engineer strains that are sensitive to small increases in temperature, and these types of vaccines are referred to as cold-adapted or temperature-sensitive (TS) vaccines. Typically, a TS vaccine is introduced at a relatively cool site in the body, either subcutaneously or intramuscularly at a peripheral site, or via droplets into the nose. Such sites provide an opportunity for the TS agent to multiply before encountering the warmer temperatures of the body core and dying.
All current human TS vaccines are for viral diseases and include the recently released FluMist influenza vaccine. Recent advances in genetics and synthetic biology are opening up new approaches to TS vaccines that make a TS vaccine strategy broadly applicable to bacterial diseases. These new approaches also offer more control over safety, such as an ability to engineer the exact range of temperature in which the pathogen will live or die, and an ability to provide a greater genetic stability of the TS phenotype. Regardless of the approach, all TS vaccines rely on understanding the temperature distribution in mammals and understanding how to produce a strong immune response at the site of vaccination. Thus, this work will cover the biology of mammalian body temperature control and distribution, followed by an overview of antigen processing by immune cells in the skin. We finish by describing examples of existing temperature-sensitive vaccines, and methodologies for creating new TS vaccines using genes from psychrophilic (cold-loving) bacteria.
Distribution and regulation of body temperatures in humans
To understand the potential use of temperature-sensitive vaccines, one must appreciate the mechanisms of mammalian temperature regulation and the distribution of body temperatures. Human body temperatures vary noticeably from the deep visceral tissues and the central nervous system to the body surface (Fig. 1). Even within the cranium from the third and fourth ventricles to the meninges there are centrifugal temperature gradients of up to 1°C [3, 4]. In addition, within the airways there are pronounced variations of temperatures from the nares to the lower respiratory tract [5]. Irrespective of these regional variations, the core temperature (TC) is regulated at approximately 37°C [6–9] and autonomic thermoregulatory responses are induced by a control system to maintain TC through increases in heat loss or heat gain.
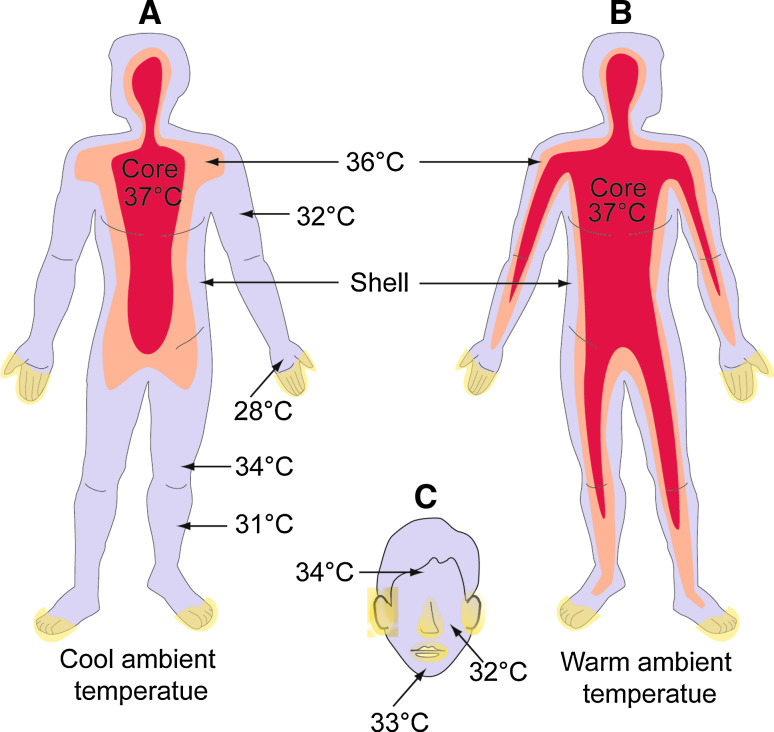
Fig. 1.
Diagrammatic illustration of body temperature in the human body. a In cold environments, the area preserved at 37°C contracts and the shell area expands. b The body volume preserved at 37°C expands. Yellow areas in a, b, and c illustrate the "acral" regions that help control body temperature by constricting blood vessels when the body temperature falls. Arteriovenous anastomoses (AVA) found in the cutaneous vasculature of the acral regions open and close to allow or prevent, respectively, rapid heat loss from the skin. The concepts presented here are generalizations; a number of variables, such as gender, age, and individual difference can affect the temperature distribution (adapted from [10])
The distinction between the terms regulation and control are important in the study of autonomic as well as behavioral temperature regulation [10]. The sources of these two terms in the biology and physiology literature come from cybernetics—the study of automatic control systems. With respect to human and mammalian physiological systems, control refers to the action of a physiological system’s set of responses that act to regulate a given variable. For example, the human thermoregulatory system acts by inducing shivering or sweating responses to facilitate heat gain or heat loss. For the thermoregulatory control system, the regulated variable is TC whereas surface skin temperatures follow TC in an open loop. The negative feedback control employed to regulate TC [7] includes three main components: temperature-sensitive neurons in the skin and at all spinal levels of the CNS, an integration center in the hypothalamus in the brain stem, and thermoeffectors including sweat glands, skeletal muscle, and cutaneous blood vessels.
The physiological control system to enable regulation of body TC has autonomic and behavioral components [11]. Behavioral components include changes of clothing, seeking warmth or shade or limiting activity, and these components have important contributions to the regulation of TC. If these behaviors are restricted, such as in a laboratory setting, following decreases in body surface and TC, shivering and cutaneous vasoconstriction are the main autonomic thermoregulatory effector responses. These responses contribute to heat balance by generating heat from shivering and restricting surface heat loss by convection or conduction; this helps to regulate TC in cold environments. In contrast, increases in body temperatures are coupled with increased surface sweat production from sweat glands and vasodilatation of cutaneous blood vessels. If the ambient environment permits evaporation of the sweat, a powerful surface cooling ensues. Likewise, vasodilatation increases the volume of warm core blood closer to the skin surface and heat is lost from convection, conduction, and radiation at the body surface.
Core and shell compartments change with ambient temperature
The distribution of temperatures is best understood using a 2-compartment model of body temperatures [12]. The two compartments in this model are the shell and the core (Fig. 1). The boundaries of these 2 compartments are indefinite and change according to ambient environmental conditions. At a cold ambient temperature (Fig. 1a), the surface temperatures are the lowest in the extremities (approximately 28–31°C) and the core compartment is regulated at 37°C. At warm ambient temperatures (Fig. 1b), two main changes are evident in the core and shell compartments. First, the physical size of the core compartment increases and the shell compartment decreases. Second, there is a reduction in the large gradient of surface temperatures evident in the cold (i.e., 28–31°C). In the cold (Fig. 1a), there is a pronounced peripheral vasoconstriction that physically increases the size of the shell compartment as warm blood is shifted to a smaller core compartment. In warm ambient conditions (Fig. 1b), more blood perfuses the vasodilated cutaneous vascular beds and the shell compartment physically expands in size.
Surface skin temperature depends on the type of underlying cutaneous vasculature that varies in differing anatomical locations. Acral regions include the hands, feet, nose, and ears. These areas have arteriovenous anastomoses (AVA) in the cutaneous vasculature that are under sympathetic control. The non-acral surface regions of the integument are the non-extremities and resolving the mechanism(s) of control of the cutaneous vasculature in these regions is an active area of research [13]. During thermal challenges, these acral surface regions act as thermoregulatory organs. Opening or closing of the AVA allow rapid shifts of blood to or from the skin surface so as to allow increases or decreases of surface heat exchange, mainly through conduction and convection. The AVA explains the ability of the extremities to rapidly give large changes in perfusion as well as surface skin temperature. This results in changes in heat loss or gain and assists in thermoregulation. Consequently, the acral regions of the body can have rapid and pronounced swings in their surface skin temperature during changes in environmental conditions. The temperature of the extremities, in the shell compartment, can in cold environments reach temperatures less than 10°C and these temperatures show a volatility to changes in ambient environmental conditions.
Airway temperatures vary with every breath
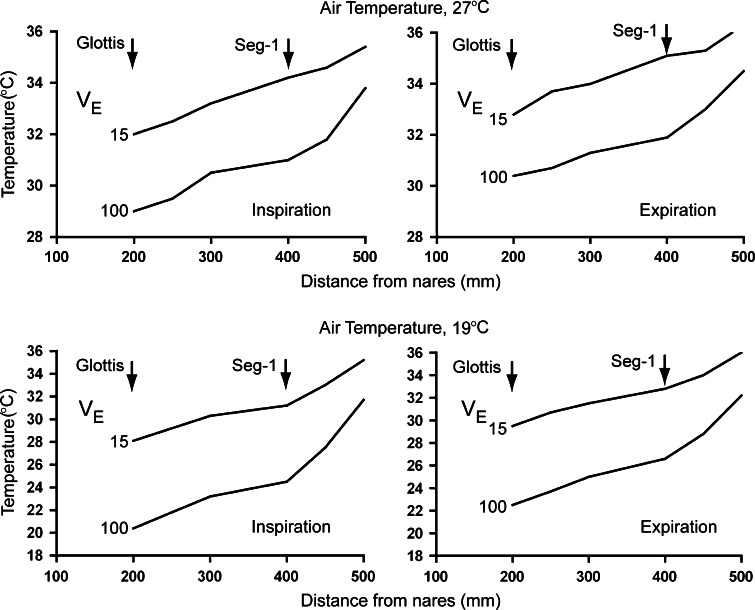
During normal breathing by non-exercising humans, there is considerable variability in the temperature of the airways during inspiration and expiration. In one study [5] (Fig 2) researchers examined the effect of different ambient temperature (19 or 27°C) together with incremental changes in the pulmonary ventilation rate (VE) on the temperature of the air at different locations in the respiratory tract. At the level of the glottis, that is part of the larynx, in the warmer ambient conditions of 27°C, inspiratory and expiratory temperatures ranged from 32 to 33°C at a VE of 15 l/min, and this decreased to 29–30°C at a VE of 100 l/min. At this same ambient temperature, deep in the airways at a VE of 15 l/min, airway temperatures were 35–36°C, and this decreased to 34–35°C when VE increased to 100 l/min.
Fig. 2.
Air temperature in the human respiratory tract. The rate of breathing (VE) and the air temperature affect the air temperature in the respiratory tract, but it usually does not reach the temperature of the body core (in moderate ambient temperatures). The arrow for "glottis" and "Seg-1" represent the level of the larynx and the bronchopulmonary segment 1, respectively (adapted from [3])
At the lower ambient air temperature of 19°C (Fig. 2b), the spread in temperature was even more impressive. Inspiratory and expiratory temperatures at the glottis ranged from 28 to 29°C (VE of 15 l/min) to 20–23°C (VE of 100 l/min). Deep in the airways, the airway temperature ranged from 35 to 37°C (VE of 15 l/min) to 32–32.5°C (VE of 100 l/min). At elevated ambient temperatures of 37°C, there were diminished gradients in temperature from the upper airways to the right lower lobe of the lung (not shown).
To summarize these findings in relation to a TS vaccine design, one can assume that overall for individuals at rest in an ambient temperature of 27°C, the entire airway temperature is below a normal TC of 37°C. Deeper within the airway, temperatures approach TC. With hyperventilation there are substantial drops in airway temperature relative to a normal VE. At a normal ambient room temperature, the upper airways (glottis) are typically about 4–5°C below TC and lower airways are 0.5–1.0°C below TC. At lower ambient temperatures there are more pronounced gradients between the upper and lower airways and between the airways and the core compartment.
Other considerations: natural and pathological variations in body temperatures
There are natural variations in human body temperatures caused by circadian rhythms, menstruation, and repeated exposure to different climates, and illnesses can also produce significant variations in body temperatures. The circadian variation in body temperatures has a period of 24–25 h [12, 14] and follows an approximately sinusoidal pattern for both TC and surface skin temperatures. For TC the nadir is a few hours before waking in the morning with a value of 0.5–1.0°C below mid-day resting TC and the zenith occurs in the late afternoon with a value of 0.5–1.0°C above mid-day resting TC [12]. For surface skin temperatures, this circadian variation follows a similar sinusoidal pattern as TC but generally has bigger amplitudes [15].
During menstruation, the TC is lowest in the follicular phase and following ovulation at the midpoint in the 28-day cycle there is a 0.5–1.0°C increase in TC that is maintained throughout the luteal phase [14, 16]. These menstrual cycle changes in TC do not appear to be followed by parallel changes in skin temperatures.
Humans also have the ability to change their responses to environmental temperatures. Repetitive exposure to hot humid or hot dry [12] as well as to cold environments [17, 18] gives adaptations of body temperatures and thermoregulatory responses. With repetitive exposure to hot environments the resting TC and surface skin temperatures are lower than in unhabituated people, and even small increases in the Tc will initiate surface sweating responses, as well as cutaneous vasodilatation responses. Following cold acclimation, TC and surface skin temperatures are also lower than in unhabituated individuals, but here a larger decrease in TC is needed to induce a shivering response and vasoconstriction to promote heat conservation [17].
A variety of pathologies can affect body temperatures more dramatically. During fever (pyrexia), a higher body TC is maintained and variations from this TC give the appropriate thermoregulatory responses [10]. For example, for a febrile TC of 40°C the thermoregulatory responses are minimal or dormant. A decrease from the TC of 40°C induces shivering and heat conservation responses whereas an elevation in TC from 40°C induces surface sweating. The corresponding increases and decreases in heat exchange follow these thermoregulatory responses. Hyperhidrosis is an elevation of surface sweat production that is normally benign but can be associated with lower surface skin temperature and TC, whereas hypohidrosis (reduced sweating) or anhidrosis (absence of sweating) can lead to hyperthermia with elevations of skin temperature and TC [19].
Although it is prudent to consider the problems that variation in human body temperatures pose to designing TS vaccines, it is also important to remember the extensive history of success in using TS viral vaccines. Some of the new approaches discussed below that can be used to create TS vaccines allow one to choose the precise temperature of inactivation of the TS agent. Thus, new vaccines should be able to accommodate the variety of factors that affect human body temperatures.
Effective antigen processing by immune cells in the skin
One of the important challenges in vaccinology is developing a convenient delivery strategy, such as inoculating the skin, while inducing a systemic immunity that includes mucosal sites, such as the respiratory tract. Administration of vaccines via scarification, which involves deposition of the vaccine material on the skin and then scratching or puncturing the skin to introduce the vaccine material into the different skin layers, has been an accepted method of antigen delivery for decades. For example, the live vaccines used to prevent tuberculosis and tularemia are administered in this fashion, as was the vaccinia (anti-smallpox) vaccine. These vaccines demonstrate that it is possible to generate mucosal immunity following vaccination at peripheral sites.
The development of this immunity is thought to be largely dependent on the presence of dendritic cells patrolling the dermal compartments for foreign antigen to be taken up and presented to T cells in the local lymph node. There are several reasons why a live organism induces a better immune response from dendritic cells than a dead or component vaccine. First, adequate immune responses are rarely directed against a single antigen or epitope. Intact microorganisms are complex and likely possess an array of antigens required for protection against virulent strains. Second, live organisms have pathogen associated molecular patterns (PAMPs) that are recognized by specific host cells, including dendritic cells. Engagement of PAMPs by dendritic cells increases the uptake of the vaccine strain by these important host cells and ultimately facilitates the process of antigen presentation that is required for the generation of long-lived immunity against most pathogens. Finally, live attenuated pathogens may also provoke inflammatory responses that aid in activating host cells, which could help drive development of adaptive immunity.
Following engagement of PAMPs and phagocytosis of antigen or pathogens, dendritic cells produce an array of pro-inflammatory cytokines and chemokines [20]. These cytokines and chemokines serve two purposes. First, they alert the host of the presence of an invading pathogen and allow for recruitment of effector cells, such as neutrophils, capable of immediately controlling the infection. Second, many of these cytokines induce dendritic cells to undergo maturation. This maturation process is marked by a shift in surface expression of the chemokine receptor CCR5 to CCR7. Loss of CCR5 and increase in CCR7 on the surface of the dendritic cell allows for migration of the dendritic cell to the local lymph node [21]. Dendritic cell maturation also includes increased surface expression of antigen-bearing MHC receptors and costimulatory receptors, i.e., CD80 and CD86, that are required for presentation of antigen to T cells residing in the lymph node [21]. Lastly, it has been suggested that the dynamics of specific dendritic cell subsets arriving in the draining lymph node may affect the type of T cell response that develops, i.e., Th1 versus Th2.
The skin contains different sub-populations of dendritic cells and the precise role of different subpopulations of skin dendritic cells in stimulating humoral or cellular immunity is not entirely clear. The outermost skin layer is the epidermis, which is about 1 mm in thickness, depending on the anatomical location. The major immune sentinel cells in the epidermis are the Langerhans cells, a form of dendritic cell that self-proliferates and is not replenished by cells originating from the bone marrow. Lying beneath the epidermis is the dermis layer, which is about 2–3 mm thick and contains sweat glands, nerves and blood vessels and a second population of dendritic cells coined “dermal dendritic cells.” Both Langerhans cells and dermal dendritic cells can take up antigen and migrate to the local lymph node where they present antigen to resident T cells.
There are at least two key differences between Langerhans cells and dermal dendritic cells in their function as antigen presenting cells. First, even in the context of inflammation, Langerhans cells take about 72 h following encounter with antigen to migrate to the lymph node [22]. In contrast, dermal dendritic cells that express langerin (but are distinct from Langerhans cells) have been noted to arrive in the lymph node within 18 h after exposure to antigen [23]. Thus, dermal dendritic cells may represent the first cells capable of alerting T cells to foreign antigen present in the skin.
A second important difference between Langerhans cells and dermal dendritic cells lies in their ability to cross present antigen to CD8+ T cells. Activation of CD8+ T cells is especially important for defense against a wide array of intracellular pathogens. CD8+ T cells have the ability to both activate infected phagocytes following secretion of IFN-γ and lyse infected cells via direct cytotoxicity. Stimulation of CD8+ T cells by dendritic cells requires cross-presentation of antigen. Langerhans cells are not able to cross-present antigen to CD8+ T cells. Rather, dermal dendritic cells that possess langerin on their surface are the cell types that perform this function in the local lymph node [24].
The differences between Langerhans cells and dermal dendritic cells extend beyond their ability to present antigen to different subsets of T cells. Recent evidence suggests that both cell types can differentially polarize T cell responses, and that populations of Langerhans cells and dermal dendritic cells vary depending on specific anatomical locations [25]. In that report, it was shown that in mice the ear contained both Langerhans cells and dermal dendritic cells, whereas the footpad had a surprising lack of dermal dendritic cells. Furthermore, Langerhans cells were found to provoke strong Th2 responses, whereas dermal dendritic cells appear to promote strong Th1 responses. Th2 responses are considered especially effective against extracellular pathogens. In contrast, it is widely accepted that Th1 responses are required for defense against infection with intracellular pathogens [26–28]. Thus, if a vaccine is designed to generate immunity against an intracellular pathogen such as M. tuberculosis or F. tularensis, one would target dermal tissues that are rich in dermal dendritic cells. Alternatively, vaccines directed against extracellular pathogens may be more effective if delivered to sites dominated by Langerhans cells.
Although we have discussed vaccination at skin sites, mucosal tissues, especially those in the gastrointestinal or respiratory tracts, could also be used as sites for introducing a live vaccine. However, there is considerable controversy over the requirement of mucosal vaccination for inducing immune protection at mucosal sites, and addressing these issues as they relate to vaccination with TS live vaccines is beyond the scope of this review.
TS viral vaccines
Viral vaccinology is rich in the number and variety of vaccine types that have been successfully used, and provides the best set of examples of TS vaccines. Many of these live TS vaccines were selected by repeatedly subculturing the virus at cool (26–29°C) temperatures either in chicken embryos or in tissue culture [29–31]. Some examples of vaccines developed using this approach include the Sabin polio vaccine [32], the rubella vaccine (Meruvax® II) [33] and the FluMist® intranasal vaccine [30]. Mutant viruses that grow better than their parent strains at the cool temperatures are said to be cold adapted and are often attenuated in their virulence. However, multiple changes to the viral genome usually occur during the cold-adaptation process, and mutations that lead to cold adaptation can sometimes be distinct from mutations that lead to attenuation or temperature sensitivity.
A cold-adapted phenotype simply indicates that a virus replicates better than its wild-type parent at cool temperatures, whereas a TS phenotype means that one or more viral macromolecules cannot fully function at elevated temperatures (usually 38–40°C). In viruses that have been passaged at cool temperatures it is common to find any of the following: (1) mutations that induce an attenuating phenotype but do not contribute to cold adaptation nor temperature sensitivity, (2) mutations that induce both temperature sensitivity and cold adaptation, (3) mutations that induce temperature sensitivity without affecting cold adaptation, or (4) mutations that induce cold adaptation without affecting temperature sensitivity. Usually a TS mutation is also attenuating, simply by the fact that the virus is unable to replicate at core body temperatures.
In some cases, researchers have characterized the contribution of different mutations in cold-adapted viruses and surmised the phenotype that the mutations impart on the virus. Murphy and colleagues have documented just such an array of mutations found in influenza and parainfluenza TS variants. For example, of the 15 non-silent nucleotide changes in the cold passaged parainfluenza virus cp45, three mutations in the L polymerase resulted in amino acid changes that induce a TS and attenuation phenotype but did not contribute to cold adaptation [34]. Surprisingly, construction of recombinant virus that lacked some of the mutations known to render a TS phenotype, were more TS [35]. This suggests that protein–protein interactions lead to the overall TS phenotype rather than several separate mutations that independently contributed to the TS phenotype. They also showed that multiple mutations, different from those that imparted a TS phenotype, contributed to the cold adaptation of the cp45 virus.
In a separate study of parainfluenza virus, Subbarao et al. [36] showed that multiple TS lesions were additive; that is, the introduction of more TS lesions lead to a lower restrictive temperature. They also showed that, as expected, the lower the restrictive temperature the lower the yield of virus from infected hamster tissue. As well, they showed that virus with restrictive temperatures of 36, 37, and 38°C could replicate in the upper respiratory tract but not in the lower respiratory tract, which is presumably at a warmer temperature. However, virus strains that could replicate at 39°C or higher were competent for robust replication in the lower respiratory tract.
The most recently introduced cold-adapted viral vaccine is the FluMist influenza vaccine. This vaccine is a derivative of the cold-passaged A/Ann Arbor/6/60 strain [37]. Jin and co-workers showed that five amino acid changes are responsible for the TS and attenuation phenotypes of the strain [38, 39]. The restrictive temperature is about 39°C where it has 2–5 log less cell culture growth (depending on the multiplicity of infection) than a wild-type strain [40]. Clinical trials of FluMist have shown that it provides better protection against both antigenically matched and unmatched influenza virus [41], and that it can be safely used in immunocompromised individuals [42].
TS bacterial vaccines used in veterinary medicine
Live vaccines have been common in veterinary medicine for decades, but only a handful are TS vaccines. Between 1980 and 2000, TS vaccines for Chlamydophila abortus [43–45], Mycoplasma synoviae [46–48], Mycoplasma gallisepticum [49], and Bordetella avium [50] were developed. All of these vaccines were produced using chemical mutagenesis (nitrosoguanidine) to create the TS mutations, and powerful chemical mutagens are known to create multiple mutations in the targeted chromosome. At the time these TS vaccine strains were made, rapid DNA sequencing technologies were not available, and thus, the mutants were not analyzed sufficiently to know the nature of the mutations in the vaccine strains. Because there was limited genetic analysis of these TS strains, one cannot conclude that the primary attenuating mutations are those that confer a TS phenotype. Had these vaccines been developed in the era of rapid genome sequencing, it would have been possible to make some surmises as to the mutations that affected virulence and temperature sensitivity. Despite these drawbacks, these vaccines provide validation that TS bacterial vaccines can be effective and acceptable to the agricultural community.
New approach to creating TS bacterial vaccines using psychrophilic essential genes
Advances in molecular biology and microbial genomics over the past few decades have made it possible to understand the role and functioning of a large portion of the genes in a bacterial chromosome, and furthermore, to rapidly alter its gene composition and regulate individual or large blocks of genes. As well, decades of work by microbial geneticists has established the identity of dozens of common essential genes that are found in intensely studied model bacteria, such as Escherichia coli and Bacillus subtilis. The identification of essential genes has been greatly expanded in the last decade due to the explosion in the number of sequenced bacterial genomes. The availability of a sequenced genome allows researchers to apply saturation transposon mutagenesis and identify the insertion point of every transposon insert [51–64]. Although each bacterium has a different number of essential genes, all bacteria share a common set of at least 100 highly conserved genes that are essential in almost all bacteria [55].
In a recent study we combined many of the methods of modern microbial genetics and applied them to the goal of creating TS bacterial vaccines [65], and the potential significance of this work is discussed in two commentaries [66, 67]. The conserved nature of essential genes inspired us to test the idea that substituting an essential gene from a psychrophilic (cold-loving) bacterium for its counterpart in the chromosome of a mesophilic (moderate-loving) bacterium would render the latter temperature-sensitive. A relatively large fraction of psychrophilic essential genes indeed did function properly in a mesophilic host, and created a TS strain. Importantly for the use of TS bacteria as vaccines, we found that most of the psychrophilic essential genes did not mutate at detectable rates to produce temperature-resistant products. Hence, most hybrid strains had a stable TS phenotype.
At the time we began our work, there were only a few sequenced genomes of psychrophilic bacteria [68–70]. Fortunately, the G+C content of the DNA of one of the better-studied psychrophiles, Colwellia psychrerythraea, was reasonably close to that of the G+C content of our targeted mesophile, Francisella novicida [71], a facultative intracellular, rodent pathogen that induces disease in mice similar to human tularemia [72]. Having similar G+C content reduces the need to codon optimize the foreign gene. F. novicida was well suited for our needs, since it can be transformed with linear or circular DNA that readily integrates into the chromosome [73]. Its biology as an intracellular pathogen also makes it ideal to test TS forms as live vaccines since intracellular pathogens usually require cellular immunity for effective clearance, and live vaccines are particularly good at inducing a cell mediated response.
Our concept of a TS vaccine strain was of a bacterium that retained all of its virulence properties but was TS in an essential function and thus restricted in where it could grow in the body by the different temperatures of mammalian tissues. For example, we envisioned a TS pathogen that was introduced into the skin where the pathogen would be engulfed by dermal dendritic cells. At some point, the pathogen-laden dendritic cells would migrate to a local lymph node where the pathogen would encounter elevated body temperatures and die. It was hoped that the TS pathogen would have enough "normal" growth in the antigen-processing cell so as to induce an immune response that mimicked that induced by the wild-type pathogen, before the TS pathogen died due to elevated temperature.
When we constructed TS forms of F. novicida by inserting TS essential genes from C. psychrerythraea we wanted to test if the TS F. novicida would replicate at a relatively cool site in a mammalian host without replicating in warmer, deep tissue. Four strains of TS F. novicida with restrictive (lethal) temperatures of 35, 37, 38, and 41°C were injected subcutaneously at the base of the tail in rats and mice. For all of the strains, bacteria could be found at the site of inoculation 3 days later. For the strains with restrictive temperatures of 35 and 37°C no bacteria could be found in the spleen at the same time point. For the strain with the 38°C restrictive temperature, bacteria could be found in the spleen at numbers about 100-fold less than found with the wild-type F. novicida strain. After inoculating with the strain with the 41°C restrictive temperature, bacteria were found in rat spleens at numbers about tenfold less than when the wild-type strain was used for the inoculation; the wild-type strain has a maximal growth temperature of about 45°C.
A strain with a restrictive temperature of 37°C was used to test for its ability to induce protective immunity. A subcutaneous inoculation at the base of the tail with the TS strain was followed 3 weeks later with a lethal challenge with the wild-type F. novicida strain, which was delivered intranasally. The inoculation with the TS strain provided immune protection as measured by the reduced bacterial organ burden, reduced weight changes, and survival of the vaccinated mice as compared to mock-vaccinated mice.
Factors that affect a successful substitution of an essential gene
One of the goals in engineering a TS vaccine strain is to have its growth at a permissive temperature to be as close to the wild-type strain as possible. When substituting a gene encoding a psychrophilic essential protein into a mesophilic chromosome there are a number of issues one needs to consider in attempting to ensure that the function of the psychrophilic gene product matches that of its mesophilic host counterpart. First and foremost is the properties (kcat, KM, half-life) of the psychrophilic product itself. These factors are the most difficult to control, and testing a variety of psychrophilic forms to find a good candidate is probably easier than attempting to engineer a psychrophilic enzyme to be similar to its mesophilic counterpart. The transcription of the psychrophilic gene can be engineered to be at a physiological level simply by fusing the psychrophilic gene to the mesophilic gene’s first few codons. However, a number of subtle differences between the mRNA sequence of the psychrophilic and mesophilic gene can potentially affect the rate of translation of the foreign gene. The strength of the ribosome binding site (RBS) is strongly influenced by the surrounding sequence, both upstream and downstream of the RBS [74], and the introduction of a foreign gene could affect the amount of protein translated. Even if the psychrophilic protein were to have identical amino acid sequence at the N-terminus as the mesophilic protein, just a change in the nucleotide sequence (different synonymous codons) could affect translation initiation. Also, changes in the nucleotide sequence could affect the efficiency of translation if rare codons [75, 76] or rare codon pairs [77] for the host organism are introduced. This last issue can be addressed by carefully designing codon-optimized genes.
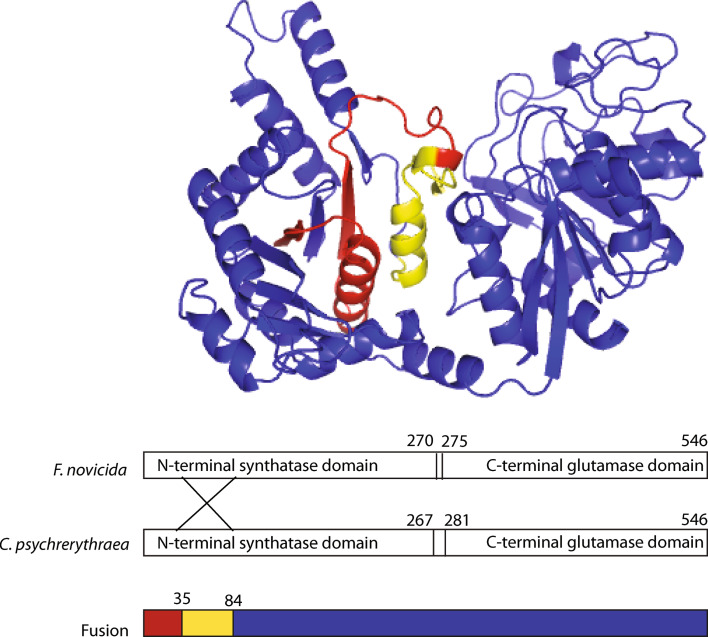
One gene substitution (the pyrG gene) made us ponder the issues discussed above. The pyrG gene encodes the essential protein, CTP synthetase, which converts UTP to CTP. When we introduced the C. psychrerythraea pryG gene into F. novicida we found that two separate successful substitutions both contained hybrid genes, with the F. novicida portion occupying the first 57 or 156 codons of the 544 codon gene (Fig. 3). It could be that the Colwellia CTP synthetase could not function without the amino terminus of the F. novicida enzyme. It could also be that one of the mRNA features, such as the RBS required the F. novicida mRNA sequence at the 5′-end. However, the case of pyrG may represent an even more complicated situation. In some bacteria pyrG transcription has been shown to be controlled by attenuation in which the cellular concentration of CTP affects the 5′-secondary structure of the mRNA and different mRNA structures lead either to transcription termination or transcription anti-termination [78–80]. This example emphasizes the need to consider a number of factors, including those that affect transcription, translation, and enzyme function.
Fig. 3.
Hybrid protein of F. novicida and C. psychrerythraea CTP synthetases (product of pyrG gene). The area in red represents the F. novicida sequence and the area in yellow represents the amino acid sequence that is identical between the two protein forms. The area in blue represents the C. psychrerythraea sequence. The enzymes from the two bacteria are 70% identical in amino acid sequence. The only successful C. psychrerythraea pyrG gene substitutions in F. novicida were genes with a hybrid structured, and two similar hybrid structured were found. The retention of the F. novicida portion at the N-terminus may represent the need for that amino acid sequence to maintain enzymatic activity or may reflect the requirement to conserve the mRNA sequence at the 5′-end of the transcript
How much diversity in TS essential genes can we expect to find?
Optimally one would like to discover a panel of TS essential proteins that can be mixed and matched to meet the requirements of any genome engineering. This is similar to the notion of "biological parts" that are often discussed as the basis of much of synthetic biology [81]. For example, for any one essential protein one would like to have variants that are inactivated at a range of different temperatures depending on how one would like to use the encoding gene. Also, as we have found for some TS psychrophilic genes, one may need to examine a number of variants in order to find one that is incapable of mutating to a temperature-resistant form. In some cases one would like to have TS products encoded by genes that lie in widely dispersed locations in the target mesophilic chromosome so that a lateral gene transfer event would be unlikely to replace both in a single gene transfer event.
The task of finding multiple forms of a psychrophilic essential gene has been made easier by the recent explosion of the number of sequenced genomes of psychrophilic bacteria. Although an expanded number of genome sequences clearly enhance the diversity of available psychrophilic essential genes, this library of genes is probably only a small part of the readily available diversity. Studies of ocean bacterial biodiversity have shown that there is a great micro-diversity of a bacterial species at any one location [82]. In other words, several variants of the same species appear to co-exist in an ocean environment, and they may exhibit a wide range of sequence identity to the reference genomic sequence. This has been demonstrated primarily with pelagic photosynthetic bacteria in tropical and subtropical areas of the ocean. If the same phenomenon holds true for psychrophilic bacteria in cold ocean waters then this would imply that multiple forms of TS essential protein encoding genes can be isolated from a single sample of ocean water.
The high conservation of essential proteins also makes them amenable to the formation of hybrid proteins through recombining portions of different variants of the same gene. In many essential proteins, there are several regions of high identity, and these represent regions that can be used as combining sites. This largely alleviates the worry that artificially combining two proteins would disrupt an unidentified protein domain.
Appropriate uses of TS bacterial vaccines
The current use of TS vaccines in veterinary medicine suggests that the introduction of new, well-defined TS live veterinary vaccines would be widely accepted. As live vaccines are relatively inexpensive to produce and administer, this would make them particularly attractive as veterinary vaccine, where low cost is essential. TS veterinary vaccines would be advantageous in combating pathogens that require a T cell response for the best protection. These include Brucella abortus, Salmonella enterica, and Mycobacterium bovis.
The use of live vaccines for humans is likely to be restricted to those diseases for which subunit vaccines have not worked despite intensive efforts. Vaccine manufacturers prefer vaccines that have a minimal number of components, and thus variables, so that they can rationally test and control for the possibility of adverse reactions. However, some important human pathogens have been poorly controlled by current vaccines, and improved live TS vaccines are reasonable candidates as replacements. Such pathogens include M. tuberculosis and S. typhi, which kill over 1.5 M and 200,000 people each year, respectively.
Although we have discussed the use of TS bacteria as live vaccines that can replicate in cool sites in the body, and preferably induce cellular immunity, there is also a case for using TS bacteria as components of mucosal vaccines. We found that some TS psychrophilic essential genes were inactivated in the range of 32–33°C, and it is likely that many can be found that are inactivated at even lower temperatures. A pathogen engineered with an essential gene whose product is inactivated, e.g., at 30°C, would be unable to replicate at any site in the human body. Thus, intestinal pathogens TS at 30°C could be used as orally administered vaccines much as the anti-cholera/traveler's diarrhea vaccine is currently used. The Vibrio cholerae cells in the Dukoral vaccine are a mixture of formaldehyde and heat inactivated cells. Both killing treatments potentially alter protective antigens, and there is the possibility of traces of formaldehyde in the vaccine preparation. The use of a TS vaccine that dies at a low temperature would avoid the problems associated with both chemical killing or killing of the pathogen at elevated temperatures. Another potential advantage of using TS strains as vaccine components is that the bacterial cells may have residual metabolic activity, allowing them to maintain protective antigens identically to the wild-type strain.
The future: the role of synthetic biology in the development of TS vaccines
As genomic information grows and more tools become available for genome engineering, live attenuated viral and bacterial vaccine strains will be better designed and characterized. Already, researchers have made synthetic polio and influenza virus strains which are attenuated by deliberately changing the codon pair bias in open reading frames so that encoded proteins are made less efficiently [83–85]. This technology, called "synthetic attenuated virus engineering" (SAVE), can probably be applied to a wide variety of viruses. Although viral genomes are much smaller than bacterial genomes it is now also possible to completely engineer the latter. One of the important areas of research is reducing genomes to their minimal size by eliminating mobile elements and inactive vestigial genes [86]. Bacteria with "reduced genomes" are less likely to suffer genome rearrangements, and thus will express foreign genes in a predictable way. As well, researchers at the J. Craig Venter Institute have demonstrated that it is feasible to design and chemically synthesize large fragments of a bacterial chromosome, including a whole chromosome [87, 88]. These advances will make it possible to optimize the expression of foreign genes by planning gene regulatory loops, codon and paired codon contents of genes, and other factors that affect mRNA and protein expression. All of these developments will prove useful in designing better live vaccine strains.
Acknowledgments
The authors thank Jordon Drew for artwork and Sheila Potter for editorial assistance.
References
- 1.Calmette LCA, Guérin C, Négre L, Bouquet A. Sur la vaccination preventive des enfants nouveau-nes contre la tuberculose par le BCG. Ann Inst Pasteur. 1927;41:201–232. [Google Scholar]
- 2.Germanier R, Fuer E. Isolation and characterization of Gal E mutant Ty 21a of Salmonella typhi: a candidate strain for a live, oral typhoid vaccine. J Infect Dis. 1975;131:553–558. doi: 10.1093/infdis/131.5.553. [DOI] [PubMed] [Google Scholar]
- 3.Mariak Z, Lewko J, Luczaj J, Polocki B, White MD. The relationship between directly measured human cerebral and tympanic temperatures during changes in brain temperatures. Eur J Appl Physiol Occup Physiol. 1994;69:545–549. doi: 10.1007/BF00239873. [DOI] [PubMed] [Google Scholar]
- 4.Mellergard P, Nordstrom CH. Epidural temperature and possible intracerebral temperature gradients in man. Br J Neurosurg. 1990;4:31–38. doi: 10.3109/02688699009000679. [DOI] [PubMed] [Google Scholar]
- 5.McFadden ER, Jr, Pichurko BM, Bowman HF, Ingenito E, Burns S, Dowling N, Solway J. Thermal mapping of the airways in humans. J Appl Physiol. 1985;58:564–570. doi: 10.1063/1.335663. [DOI] [PubMed] [Google Scholar]
- 6.Cabanac M, Massonnet B. Thermoregulatory responses as a function of core temperature in humans. J Physiol (Lond) 1977;265:587–596. doi: 10.1113/jphysiol.1977.sp011732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hammel HT, Jackson DC, Stolwijk JA, Hardy JD, Stromme SB. Temperature regulation by hypothalamic proportional control with an adjustable set point. J Appl Physiol. 1963;18:1146–1154. doi: 10.1152/jappl.1963.18.6.1146. [DOI] [PubMed] [Google Scholar]
- 8.Lopez M, Sessler DI, Walter K, et al. Rate- and gender-dependence of the sweating, vasoconstriction, and shivering thresholds in humans. Anesthesiology. 1994;80:780–788. doi: 10.1097/00000542-199404000-00009. [DOI] [PubMed] [Google Scholar]
- 9.Mekjavic IB, Sundberg CJ, Linnarsson D. Core temperature “null zone”. J Appl Physiol. 1991;71:1289–1295. doi: 10.1152/jappl.1991.71.4.1289. [DOI] [PubMed] [Google Scholar]
- 10.Cabanac M. Adjustable set point: to honor Harold T Hammel. J Appl Physiol. 2006;100:1338–1346. doi: 10.1152/japplphysiol.01021.2005. [DOI] [PubMed] [Google Scholar]
- 11.Bligh J (1984) Regulation of body temperature in man and other mammals. In: Shitzer A, Eberhart R (eds) Heat transfer and medicine in biology. Plenum Pub Co, pp 15–51
- 12.Wenger CB (2008) Human adaptations to hot environments. In: Taylor N, Groeller H (eds) Physiological bases of human performance during work and exercise. Elsevier, London
- 13.Kellogg DL., Jr In vivo mechanisms of cutaneous vasodilation and vasoconstriction in humans during thermoregulatory challenges. J Appl Physiol. 2006;100:1709–1718. doi: 10.1152/japplphysiol.01071.2005. [DOI] [PubMed] [Google Scholar]
- 14.Stephenson LA, Kolka MA. Effect of gender, circadian period and sleep loss on thermal responses during exercise. In: Pandolf KB, Sawka MN, Gonzalez RR, editors. Human performance physiology and environmental medicine at terrestrial extremes. Indianapolis: Benchmark Inc; 1988. pp. 267–304. [Google Scholar]
- 15.Krauchi K, Wirz-Justice A. Circadian rhythm of heat production, heart rate, and skin and core temperature under unmasking conditions in men. Am J Physiol. 1994;267:R819–R829. doi: 10.1152/ajpregu.1994.267.3.R819. [DOI] [PubMed] [Google Scholar]
- 16.Marsh SA, Jenkins DG. Physiological responses to the menstrual cycle: implications for the development of heat illness in female athletes. Sports Med. 2002;32:601–614. doi: 10.2165/00007256-200232100-00001. [DOI] [PubMed] [Google Scholar]
- 17.Young A. Human adaptation to cold. In: Pandolf KB, Sawka MN, Gonzalez RR, editors. Human performance physiology and environmental medicine at terrestrial extremes. Indianapolis: Benchmark Inc; 1988. pp. 401–434. [Google Scholar]
- 18.LeBlanc J (1975) Man in the cold Charles C Thomas. Springfield, Illinois
- 19.Cheshire WP, Freeman R. Disorders of sweating. Semin Neurol. 2003;23:399–406. doi: 10.1055/s-2004-817724. [DOI] [PubMed] [Google Scholar]
- 20.Banchereau J, Steinman RM. Dendritic cells and the control of immunity. Nature. 1998;392:245–252. doi: 10.1038/32588. [DOI] [PubMed] [Google Scholar]
- 21.Sallusto F, Schaerli P, Loetscher P, Schaniel C, Lenig D, Mackay CR, Qin S, Lanzavecchia A. Rapid and coordinated switch in chemokine receptor expression during dendritic cell maturation. Eur J Immunol. 1998;28:2760–2769. doi: 10.1002/(SICI)1521-4141(199809)28:09<2760::AID-IMMU2760>3.0.CO;2-N. [DOI] [PubMed] [Google Scholar]
- 22.Henri S, Vremec D, Kamath A, Waithman J, Williams S, Benoist C, Burnham K, Saeland S, Handman E, Shortman K. The dendritic cell populations of mouse lymph nodes. J Immunol. 2001;167:741–748. doi: 10.4049/jimmunol.167.2.741. [DOI] [PubMed] [Google Scholar]
- 23.Ginhoux F, Collin MP, Bogunovic M, Abel M, Leboeuf M, Helft J, Ochando J, Kissenpfennig A, Malissen B, Grisotto M, Snoeck H, Randolph G, Merad M. Blood-derived dermal langerin + dendritic cells survey the skin in the steady state. J Exp Med. 2007;204:3133–3146. doi: 10.1084/jem.20071733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bedoui S, Whitney PG, Waithman J, Eidsmo L, Wakim L, Caminschi I, Allan RS, Wojtasiak M, Shortman K, Carbone FR, Brooks AG, Heath WR. Cross-presentation of viral and self antigens by skin-derived CD103+ dendritic cells. Nat Immunol. 2009;10:488–495. doi: 10.1038/ni.1724. [DOI] [PubMed] [Google Scholar]
- 25.Sen D, Forrest L, Kepler TB, Parker I, Cahalan MD. Selective and site-specific mobilization of dermal dendritic cells and Langerhans cells by Th1- and Th2-polarizing adjuvants. Proc Natl Acad Sci USA. 2010;107:8334–8339. doi: 10.1073/pnas.0912817107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Allen WP. Immunity against tularemia: passive protection of mice by transfer of immune tissues. J Exp Med. 1962;115:411–420. doi: 10.1084/jem.115.2.411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.North RJ. Importance of thymus-derived lymphocytes in cell-mediated immunity to infection. Cell Immunol. 1973;7:166–176. doi: 10.1016/0008-8749(73)90193-7. [DOI] [PubMed] [Google Scholar]
- 28.Orme IM, Collins FM. Protection against Mycobacterium tuberculosis infection by adoptive immunotherapy. Requirement for T cell-deficient recipients. J Exp Med. 1983;158:74–83. doi: 10.1084/jem.158.1.74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gelb J, Jr, King DJ, Wisner WA, Ruggeri PA. Attenuation of lentogenic Newcastle disease virus strain B-1 by cold adaptation. Avian Dis. 1996;40:605–612. doi: 10.2307/1592271. [DOI] [PubMed] [Google Scholar]
- 30.Maassab HF, DeBorde DC. Development and characterization of cold-adapted viruses for use as live virus vaccines. Vaccine. 1985;3:355–369. doi: 10.1016/0264-410X(85)90124-0. [DOI] [PubMed] [Google Scholar]
- 31.Matsuno S, Murakami S, Takagi M, Hayashi M, Inouye S, Hasegawa A, Fukai K. Cold-adaptation of human rotavirus. Virus Res. 1987;7:273–280. doi: 10.1016/0168-1702(87)90033-5. [DOI] [PubMed] [Google Scholar]
- 32.Chapin M, Dubes GR. Cold-adapted genetic variants of polio viruses. Science. 1956;124:586–587. doi: 10.1126/science.124.3222.586-a. [DOI] [PubMed] [Google Scholar]
- 33.Plotkin SA, Farquhar JD, Katz M, Buser F. Attenuation of RA 27–3 rubella virus in WI-38 human diploid cells. Am J Dis Child. 1969;118:178–185. doi: 10.1001/archpedi.1969.02100040180004. [DOI] [PubMed] [Google Scholar]
- 34.Skiadopoulos MH, Durbin AP, Tatem JM, Wu SL, Paschalis M, Tao T, Collins PL, Murphy BR. Three amino acid substitutions in the L protein of the human parainfluenza virus type 3 cp45 live attenuated vaccine candidate contribute to its temperature-sensitive and attenuation phenotypes. J Virol. 1998;72:1762–1768. doi: 10.1128/jvi.72.3.1762-1768.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Skiadopoulos MH, Surman S, Tatem JM, Paschalis M, Wu SL, Udem SA, Durbin AP, Collins PL, Murphy BR. Identification of mutations contributing to the temperature-sensitive, cold-adapted, and attenuation phenotypes of the live-attenuated cold-passage 45 (cp45) human parainfluenza virus 3 candidate vaccine. J Virol. 1999;73:1374–1381. doi: 10.1128/jvi.73.2.1374-1381.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Subbarao EK, Park EJ, Lawson CM, Chen AY, Murphy BR. Sequential addition of temperature-sensitive missense mutations into the PB2 gene of influenza A transfectant viruses can effect an increase in temperature sensitivity and attenuation and permits the rational design of a genetically engineered live influenza A virus vaccine. J Virol. 1995;69:5969–5977. doi: 10.1128/jvi.69.10.5969-5977.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Maassab HF. Adaptation and growth characteristics of influenza virus at 25 degrees c. Nature. 1967;213:612–614. doi: 10.1038/213612a0. [DOI] [PubMed] [Google Scholar]
- 38.Jin H, Lu B, Zhou H, Ma C, Zhao J, Yang CF, Kemble G, Greenberg H. Multiple amino acid residues confer temperature sensitivity to human influenza virus vaccine strains (FluMist) derived from cold-adapted A/Ann Arbor/6/60. Virology. 2003;306:18–24. doi: 10.1016/S0042-6822(02)00035-1. [DOI] [PubMed] [Google Scholar]
- 39.Jin H, Zhou H, Lu B, Kemble G. Imparting temperature sensitivity and attenuation in ferrets to A/Puerto Rico/8/34 influenza virus by transferring the genetic signature for temperature sensitivity from cold-adapted A/Ann Arbor/6/60. J Virol. 2004;78:995–998. doi: 10.1128/JVI.78.2.995-998.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chan W, Zhou H, Kemble G, Jin H. The cold-adapted and temperature-sensitive influenza A/Ann Arbor/6/60 virus, the master donor virus for live attenuated influenza vaccines, has multiple defects in replication at the restrictive temperature. Virology. 2008;380:304–311. doi: 10.1016/j.virol.2008.07.027. [DOI] [PubMed] [Google Scholar]
- 41.Belshe RB, Edwards KM, Vesikari T, Black SV, Walker RE, Hultquist M, Kemble G, Connor EM. Live attenuated versus inactivated influenza vaccine in infants and young children. N Engl J Med. 2007;356:685–696. doi: 10.1056/NEJMoa065368. [DOI] [PubMed] [Google Scholar]
- 42.King JC, Jr, Treanor J, Fast PE, Wolff M, Yan L, Iacuzio D, Readmond B, O’Brien D, Mallon K, Highsmith WE, Lambert JS, Belshe RB. Comparison of the safety, vaccine virus shedding, and immunogenicity of influenza virus vaccine, trivalent, types A and B, live cold-adapted, administered to human immunodeficiency virus (HIV)-infected and non-HIV-infected adults. J Infect Dis. 2000;181:725–728. doi: 10.1086/315246. [DOI] [PubMed] [Google Scholar]
- 43.Chalmers WS, Simpson J, Lee SJ, Baxendale W. Use of a live chlamydial vaccine to prevent ovine enzootic abortion. Vet Rec. 1997;141:63–67. doi: 10.1136/vr.141.3.63. [DOI] [PubMed] [Google Scholar]
- 44.Rodolakis A. In vitro and in vivo properties of chemically induced temperature-sensitive mutants of Chlamydia psittaci var. ovis: screening in a murine model. Infect Immun. 1983;42:525–530. doi: 10.1128/iai.42.2.525-530.1983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Rodolakis A, Souriau A. Response of ewes to temperature-sensitive mutants of Chlamydia psittaci (var ovis) obtained by NTG mutagenesis. Ann Rech Vet. 1983;14:155–161. [PubMed] [Google Scholar]
- 46.Markham JF, Morrow CJ, Scott PC, Whithear KG. Safety of a temperature-sensitive clone of Mycoplasma synoviae as a live vaccine. Avian Dis. 1998;42:677–681. doi: 10.2307/1592702. [DOI] [PubMed] [Google Scholar]
- 47.Markham JF, Morrow CJ, Whithear KG. Efficacy of a temperature-sensitive Mycoplasma synoviae live vaccine. Avian Dis. 1998;42:671–676. doi: 10.2307/1592701. [DOI] [PubMed] [Google Scholar]
- 48.Morrow CJ, Markham JF, Whithear KG. Production of temperature-sensitive clones of Mycoplasma synoviae for evaluation as live vaccines. Avian Dis. 1998;42:667–670. doi: 10.2307/1592700. [DOI] [PubMed] [Google Scholar]
- 49.Barbour EK, Hamadeh SK, Eidt A. Infection and immunity in broiler chicken breeders vaccinated with a temperature-sensitive mutant of Mycoplasma gallisepticum and impact on performance of offspring. Poult Sci. 2000;79:1730–1735. doi: 10.1093/ps/79.12.1730. [DOI] [PubMed] [Google Scholar]
- 50.Jackwood MW, Saif YM. Efficacy of a commercial turkey coryza vaccine (Art-Vax) in turkey poults. Avian Dis. 1985;29:1130–1139. doi: 10.2307/1590467. [DOI] [PubMed] [Google Scholar]
- 51.Akerley BJ, Rubin EJ, Novick VL, Amaya K, Judson N, Mekalanos JJ. A genome-scale analysis for identification of genes required for growth or survival of Haemophilus influenzae . Proc Natl Acad Sci USA. 2002;99:966–971. doi: 10.1073/pnas.012602299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.de Berardinis V, Vallenet D, Castelli V, Besnard M, Pinet A, Cruaud C, Samair S, Lechaplais C, Gyapay G, Richez C, Durot M, Kreimeyer A, Le Fevre F, Schachter V, Pezo V, Doring V, Scarpelli C, Medigue C, Cohen GN, Marliere P, Salanoubat M, Weissenbach J. A complete collection of single-gene deletion mutants of Acinetobacter baylyi ADP1. Mol Syst Biol. 2008;4:174. doi: 10.1038/msb.2008.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Forsyth RA, Haselbeck RJ, Ohlsen KL, Yamamoto RT, Xu H, Trawick JD, Wall D, Wang L, Brown-Driver V, Froelich JM, KG C, King P, McCarthy M, Malone C, Misiner B, Robbins D, Tan Z, Zhu Zy ZY, Carr G, Mosca DA, Zamudio C, Foulkes JG, Zyskind JW. A genome-wide strategy for the identification of essential genes in Staphylococcus aureus . Mol Microbiol. 2002;43:1387–1400. doi: 10.1046/j.1365-2958.2002.02832.x. [DOI] [PubMed] [Google Scholar]
- 54.Gallagher LA, Ramage E, Jacobs MA, Kaul R, Brittnacher M, Manoil C. A comprehensive transposon mutant library of Francisella novicida, a bioweapon surrogate. Proc Natl Acad Sci USA. 2007;104:1009–1014. doi: 10.1073/pnas.0606713104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Gerdes SY, Scholle MD, Campbell JW, Balazsi G, Ravasz E, Daugherty MD, Somera AL, Kyrpides NC, Anderson I, Gelfand MS, Bhattacharya A, Kapatral V, D’Souza M, Baev MV, Mseeh F, Fonstein MY, Overbeek R, Barabasi A-L, Oltvai ZN, Osterman AL. Experimental determination and system level analysis of essential genes in Escherichia coli MG1655. J Bacteriol. 2003;185:5673–5684. doi: 10.1128/JB.185.19.5673-5684.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Glass JI, Assad-Garcia N, Alperovich N, Yooseph S, Lewis MR, Maruf M, Hutchison CA, 3rd, Smith HO, Venter JC. Essential genes of a minimal bacterium. Proc Natl Acad Sci USA. 2006;103:425–430. doi: 10.1073/pnas.0510013103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Jacobs MA, Alwood A, Thaipisuttikul I, Spencer D, Haugen E, Ernst S, Will O, Kaul R, Raymond C, Levy R, Chun-Rong L, Guenthner D, Bovee D, Olson MV, Manoil C. Comprehensive transposon mutant library of Pseudomonas aeruginosa . Proc Natl Acad Sci USA. 2003;100:14339–14344. doi: 10.1073/pnas.2036282100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ji Y, Zhang B, Van SF, Horn Warren P, Woodnutt G, Burnham MK, Rosenberg M. Identification of critical staphylococcal genes using conditional phenotypes generated by antisense RNA. Science. 2001;293:2266–2269. doi: 10.1126/science.1063566. [DOI] [PubMed] [Google Scholar]
- 59.Knuth K, Niesalla H, Hueck CJ, Fuchs TM. Large-scale identification of essential Salmonella genes by trapping lethal insertions. Mol Microbiol. 2004;51:1729–1744. doi: 10.1046/j.1365-2958.2003.03944.x. [DOI] [PubMed] [Google Scholar]
- 60.Kobayashi K, Ehrlich SD, Albertini A, Amati G, Andersen KK, Arnaud M, Asai K, Ashikaga S, Aymerich S, Bessieres P, Boland F, Brignell SC, Bron S, Bunai K, Chapuis J, Christiansen LC, Danchin A, Debarbouille M, Dervyn E, Deuerling E, Devine K, Devine SK, Dreesen O, Errington J, Fillinger S, Foster SJ, Fujita Y, Galizzi A, Gardan R, Eschevins C, Fukushima T, Haga K, Harwood CR, Hecker M, Hosoya D, Hullo MF, Kakeshita H, Karamata D, Kasahara Y, Kawamura F, Koga K, Koski P, Kuwana R, Imamura D, Ishimaru M, Ishikawa S, Ishio I, Le Coq D, Masson A, Mauel C, Meima R, Mellado RP, Moir A, Moriya S, Nagakawa E, Nanamiya H, Nakai S, Nygaard P, Ogura M, Ohanan T, O’Reilly M, O’Rourke M, Pragai Z, Pooley HM, Rapoport G, Rawlins JP, Rivas LA, Rivolta C, Sadaie A, Sadaie Y, Sarvas M, Sato T, Saxild HH, Scanlan E, Schumann W, Seegers JF, Sekiguchi J, Sekowska A, Seror SJ, Simon M, Stragier P, Studer R, Takamatsu H, Tanaka T, Takeuchi M, Thomaides HB, Vagner V, van Dijl JM, Watabe K, Wipat A, Yamamoto H, Yamamoto M, Yamamoto Y, Yamane K, Yata K, Yoshida K, Yoshikawa H, Zuber U, Ogasawara N. Essential Bacillus subtilis genes. Proc Natl Acad Sci USA. 2003;100:4678–4683. doi: 10.1073/pnas.0730515100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Salama NR, Shepherd B, Falkow S. Global transposon mutagenesis and essential gene analysis of Helicobacter pylori . J Bacteriol. 2004;186:7926–7935. doi: 10.1128/JB.186.23.7926-7935.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Sassetti CM, Boyd DH, Rubin EJ. Genes required for mycobacterial growth defined by high density mutagenesis. Mol Microbiol. 2003;48:77–84. doi: 10.1046/j.1365-2958.2003.03425.x. [DOI] [PubMed] [Google Scholar]
- 63.Thanassi JA, Hartman-Neumann SL, Dougherty TJ, Dougherty BA, Pucci MJ. Identification of 113 conserved essential genes using a high-throughput gene disruption system in Streptococcus pneumoniae . Nucleic Acids Res. 2002;30:3152–3162. doi: 10.1093/nar/gkf418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Xu HH, Trawick JD, Haselbeck RJ, Forsyth RA, Yamamoto RT, Archer R, Patterson J, Allen M, Froelich JM, Taylor I, Nakaji D, Maile R, Kedar GC, Pilcher M, Brown-Driver V, McCarthy M, Files A, Robbins D, King P, Sillaots S, Malone C, Zamudio CS, Roemer T, Wang L, Youngman PJ, Wall D. Staphylococcus aureus TargetArray: comprehensive differential essential gene expression as a mechanistic tool to profile antibacterials. Antimicrob Agents Chemother. 2010;54:3659–3670. doi: 10.1128/AAC.00308-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Duplantis BN, Osusky M, Schmerk CL, Ross DR, Bosio CM, Nano FE. Essential genes from Arctic bacteria used to construct stable, temperature-sensitive bacterial vaccines. Proc Natl Acad Sci USA. 2010;107:13456–13460. doi: 10.1073/pnas.1004119107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.de Lorenzo V. Genes that move the window of viability of life: Lessons from bacteria thriving at the cold extreme: mesophiles can be turned into extremophiles by substituting essential genes. Bioessays. 2010;33:38–42. doi: 10.1002/bies.201000101. [DOI] [PubMed] [Google Scholar]
- 67.Duplantis BN, Bosio CM, Nano FE (2011) Temperature-sensitive bacterial pathogens generated by the substitution of essential genes from cold-loving bacteria: potential use as live vaccines. J Mol Med. doi:10.1007/s00109-010-0721-3 [DOI] [PubMed]
- 68.Aurilia V, Parracino A, Saviano M, Rossi M, D’Auria S. The psychrophilic bacterium Pseudoalteromonas halosplanktis TAC125 possesses a gene coding for a cold-adapted feruloyl esterase activity that shares homology with esterase enzymes from gamma-proteobacteria and yeast. Gene. 2007;397:51–57. doi: 10.1016/j.gene.2007.04.004. [DOI] [PubMed] [Google Scholar]
- 69.Medigue C, Krin E, Pascal G, Barbe V, Bernsel A, Bertin PN, Cheung F, Cruveiller S, D’Amico S, Duilio A, Fang G, Feller G, Ho C, Mangenot S, Marino G, Nilsson J, Parrilli E, Rocha EP, Rouy Z, Sekowska A, Tutino ML, Vallenet D, von Heijne G, Danchin A. Coping with cold: the genome of the versatile marine Antarctica bacterium Pseudoalteromonas haloplanktis TAC125. Genome Res. 2005;15:1325–1335. doi: 10.1101/gr.4126905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Methe BA, Karen E, Nelson KE, Deming JW, Momen B, Melamud E, Xijun Zhang X, John Moult J, Madupu R, Nelson WC, Dodson RJ, Brinkac LM, Daugherty SC, Durkin AS, DeBoy RT, Kolonay JF, Sullivan SA, Zhou L, Davidsen TM, Wu M, Huston AL, Lewis M, Weaver B, Weidman JW, Khouri H, Utterback TR, Feldblyum TV, Fraser CM. The psychrophilic lifestyle as revealed by the genome sequence of Colwellia psychrerythraea 34H through genomic and proteomic analyses. Proceedings of the National Academy of Sciences. 2005;102:10913–10918. doi: 10.1073/pnas.0504766102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Rohmer L, Fong C, Abmayr S, Wasnick M, Larson Freeman TJ, Radey M, Guina T, Svensson K, Hayden HS, Jacobs M, Gallagher LA, Manoil C, Ernst RK, Drees B, Buckley D, Haugen E, Bovee D, Zhou Y, Chang J, Levy R, Lim R, Gillett W, Guenthener D, Kang A, Shaffer SA, Taylor G, Chen J, Gallis B, D’Argenio DA, Forsman M, Olson MV, Goodlett DR, Kaul R, Miller SI, Brittnacher MJ. Comparison of Francisella tularensis genomes reveals evolutionary events associated with the emergence of human pathogenic strains. Genome Biol. 2007;8:R102. doi: 10.1186/gb-2007-8-6-r102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Sharma J, Li Q, Mishra BB, Georges MJ, Teale JM. Vaccination with an attenuated strain of Francisella novicida prevents T-cell depletion and protects mice infected with the wild-type strain from severe sepsis. Infect Immun. 2009;77:4314–4326. doi: 10.1128/IAI.00654-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Anthony LS, Gu MZ, Cowley SC, Leung WW, Nano FE. Transformation and allelic replacement in Francisella spp. J Gen Microbiol. 1991;137:2697–2703. doi: 10.1099/00221287-137-12-2697. [DOI] [PubMed] [Google Scholar]
- 74.Salis HM, Mirsky EA, Voigt CA. Automated design of synthetic ribosome binding sites to control protein expression. Nat Biotechnol. 2009;27:946–950. doi: 10.1038/nbt.1568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Grosjean H, Fiers W. Preferential codon usage in prokaryotic genes: the optimal codon-anticodon interaction energy and the selective codon usage in efficiently expressed genes. Gene. 1982;18:199–209. doi: 10.1016/0378-1119(82)90157-3. [DOI] [PubMed] [Google Scholar]
- 76.Rocha EP. Codon usage bias from tRNA’s point of view: redundancy, specialization, and efficient decoding for translation optimization. Genome Res. 2004;14:2279–2286. doi: 10.1101/gr.2896904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Gutman GA, Hatfield GW. Nonrandom utilization of codon pairs in Escherichia coli . Proc Natl Acad Sci USA. 1989;86:3699–3703. doi: 10.1073/pnas.86.10.3699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Meng Q, Switzer RL. Regulation of transcription of the Bacillus subtilis pyrG gene, encoding cytidine triphosphate synthetase. J Bacteriol. 2001;183:5513–5522. doi: 10.1128/JB.183.19.5513-5522.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Meng Q, Switzer RL. cis-acting sequences of Bacillus subtilis pyrG mRNA essential for regulation by antitermination. J Bacteriol. 2002;184:6734–6738. doi: 10.1128/JB.184.23.6734-6738.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Meng Q, Turnbough CL, Jr, Switzer RL. Attenuation control of pyrG expression in Bacillus subtilis is mediated by CTP-sensitive reiterative transcription. Proc Natl Acad Sci USA. 2004;101:10943–10948. doi: 10.1073/pnas.0403755101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Voigt CA. Genetic parts to program bacteria. Curr Opin Biotechnol. 2006;17:548–557. doi: 10.1016/j.copbio.2006.09.001. [DOI] [PubMed] [Google Scholar]
- 82.Rusch DB, Halpern AL, Sutton G, Heidelberg KB, Williamson S, Yooseph S, Wu D, Eisen JA, Hoffman JM, Remington K, Beeson K, Tran B, Smith H, Baden-Tillson H, Stewart C, Thorpe J, Freeman J, Andrews-Pfannkoch C, Venter JE, Li K, Kravitz S, Heidelberg JF, Utterback T, Rogers YH, Falcon LI, Souza V, Bonilla-Rosso G, Eguiarte LE, Karl DM, Sathyendranath S, Platt T, Bermingham E, Gallardo V, Tamayo-Castillo G, Ferrari MR, Strausberg RL, Nealson K, Friedman R, Frazier M, Venter JC. The Sorcerer II Global Ocean Sampling expedition: northwest Atlantic through eastern tropical Pacific. PLoS Biol. 2007;5:e77. doi: 10.1371/journal.pbio.0050077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Coleman JR, Papamichail D, Skiena S, Futcher B, Wimmer E, Mueller S. Virus attenuation by genome-scale changes in codon pair bias. Science. 2008;320:1784–1787. doi: 10.1126/science.1155761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Mueller S, Coleman JR, Papamichail D, Ward CB, Nimnual A, Futcher B, Skiena S, Wimmer E. Live attenuated influenza virus vaccines by computer-aided rational design. Nat Biotechnol. 2010;28:723–726. doi: 10.1038/nbt.1636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Mueller S, Papamichail D, Coleman JR, Skiena S, Wimmer E. Reduction of the rate of poliovirus protein synthesis through large-scale codon deoptimization causes attenuation of viral virulence by lowering specific infectivity. J Virol. 2006;80:9687–9696. doi: 10.1128/JVI.00738-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Posfai G, Plunkett G, 3rd, Feher T, Frisch D, Keil GM, Umenhoffer K, Kolisnychenko V, Stahl B, Sharma SS, de Arruda M, Burland V, Harcum SW, Blattner FR. Emergent properties of reduced-genome Escherichia coli . Science. 2006;312:1044–1046. doi: 10.1126/science.1126439. [DOI] [PubMed] [Google Scholar]
- 87.Gibson DG, Glass JI, Lartigue C, Noskov VN, Chuang RY, Algire MA, Benders GA, Montague MG, Ma L, Moodie MM, Merryman C, Vashee S, Krishnakumar R, Assad-Garcia N, Andrews-Pfannkoch C, Denisova EA, Young L, Qi ZQ, Segall-Shapiro TH, Calvey CH, Parmar PP, Hutchison CA, 3rd, Smith HO, Venter JC. Creation of a bacterial cell controlled by a chemically synthesized genome. Science. 2010;329:52–56. doi: 10.1126/science.1190719. [DOI] [PubMed] [Google Scholar]
- 88.Lartigue C, Vashee S, Algire MA, Chuang RY, Benders GA, Ma L, Noskov VN, Denisova EA, Gibson DG, Assad-Garcia N, Alperovich N, Thomas DW, Merryman C, Hutchison CA, III, Smith HO, Venter JC, Glass JI. Creating bacterial strains from genomes that have been cloned and engineered in yeast. Science. 2009;325:1693–1696. doi: 10.1126/science.1173759. [DOI] [PubMed] [Google Scholar]