Abstract
Epidemiological studies of categorical mental disorders consistently report that gender differences exist in many disorder prevalence rates, and that disorders are often comorbid. Can a dimensional multivariate liability model be developed to clarify how gender impacts diverse, comorbid mental disorders? We pursued this possibility in the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC; N = 43,093). Gender differences in prevalence were systematic such that women showed higher rates of mood and anxiety disorders and men showed higher rates of antisocial and substance use disorders. We next investigated patterns of disorder comorbidity and found that a dimensional internalizing (mood and anxiety)-externalizing (antisocial and substance use) liability model fit the data well. This model was gender invariant, indicating that observed gender differences in prevalence rates originate from women and men's different average standings on latent internalizing and externalizing liability dimensions. As hypothesized, women showed a higher mean level of internalizing while men showed a higher mean level of externalizing. We discuss implications of these findings for understanding gender differences in psychopathology and for classification and intervention.
Keywords: comorbidity, gender differences, internalizing-externalizing, prevalence rates
Previous epidemiological studies have shown that there are sizable gender differences in the prevalence rates of many common mental disorders (for recent reviews, see Grant & Weissman, 2007; Shear, Halmi, Widiger, & Boyce, 2007; Widiger, 2007). For example, 12-month and lifetime prevalence rates from the National Comorbidity Survey indicated that women showed markedly higher (and often approximately double) prevalence rates of major depression, dysthymia, generalized anxiety disorder, panic disorder, social phobia, and specific phobia than did men, while men showed higher prevalence rates of antisocial personality disorder and alcohol and drug dependence (Kessler et al., 1993, 1994). Similar gender differences have been observed in the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC), the largest epidemiological study of psychopathology yet undertaken (Dawson et al., 2010; Keyes, Grant, & Hasin, 2008; Grant et al., 2004; Grant & Weissman, 2007; Trull et al., 2010; Vesga-López et al., 2008).
The origins of these gender differences in prevalence rates are not well understood, although various theories have been posited to explain how they arise. These explanations include response bias, differential service utilization rates, and various biological, social, and demographic influences (see Klose & Jacobi, 2004; Piccinelli & Wilkinson, 2000). Psychological explanations, such as increased rumination in women partially accounting for higher rates of unipolar depression, have also been posited (Nolen-Hoeksema, 1987; Nolen-Hoeksema, Wisco, & Lyubomirksy, 2008).
These theories of gender differences focus primarily on specific disorders, and rarely take into account comorbidity. A compelling account of the meaning of mental disorder comorbidity focuses on shared associations with unifying latent dimensional liabilities to experience multiple internalizing (mood and anxiety) or externalizing (antisocial and substance use) disorders (Eaton, South, & Krueger, 2010; Krueger, 1999; Slade & Watson, 2006; Vollebergh et al., 2001). Indeed, this internalizing-externalizing liability model is likely to frame key parts of the “meta-structure,” or overall organization, of DSM-5 (e.g., Andrews et al., 2009; Regier et al., 2011). The internalizing dimension can be bifurcated into distress and fear sub-factors; distress relates to disorders such as major depression, dysthymia, and generalized anxiety, and fear relates to disorders such as panic disorder, social phobia, and specific phobia. The externalizing dimension is associated with disorders such antisocial personality disorder and alcohol, nicotine, and drug dependence. Further, these factors relate to normal personality: Internalizing correlates with neuroticism/negative affectivity (Griffith et al., 2010), and externalizing correlates with disinhibition (Krueger et al., 2002).
When gender differences in prevalence rates and the internalizing-externalizing liability structure of psychopathology are considered simultaneously, the possibility of a unifying model of gender and comorbidity emerges. Specifically, women show significantly higher prevalence rates of internalizing disorders, while men show significantly higher rates of externalizing disorders (Grant & Weissman, 2007; Kessler et al., 1993, 1994). This observation suggests that gender differences in categorical prevalence rates might be due to gender differences in latent internalizing and externalizing liability dimensions. The utility of a dimensional liability model for public health, epidemiology, psychopathology, and intervention research would be notably enhanced if it could encompass the role of gender in mental disorder prevalence.
A few studies have evaluated the structure of psychopathology separately in women and men (e.g., Krueger, 1999; Kendler et al. 2003). However, we are aware of only two studies that have formally tested whether the latent structure of common mental disorders is gender invariant (Hicks et al., 2007; Kramer et al., 2008). While generally supportive of a gender invariant model, the generalizability of these studies was limited by non-representative samples. Further, neither study focused on DSM-IV diagnoses. Addressing these limitations is critical given the potential use of a dimensional liability model to frame key aspects of DSM-5. If the model is to be applied to DSM-5 mental disorders—and to both women and men—factorial invariance (a lack of bias) across gender should be demonstrated in a maximally representative sample.
The current study examined a nationally representative sample of 43,093 individuals assessed in the first wave of the NESARC. Our initial goal was to examine and present any gender differences in prevalence rates of common mental disorders in this sample. We were interested not only in the significance of these gender differences but also their directionality: We hypothesized that women would show significantly higher rates of internalizing disorders than men, and men would show significantly higher rates of externalizing disorders. Second, we sought to determine the latent comorbidity structure of these disorders in women and men separately. Third, we aimed to test formally whether the emergent structures in women and men could be considered gender invariant (i.e., women and men showing equivalent structures of psychopathology). Finally, if invariance were found, we hypothesized that women would have a higher mean standing on the internalizing liability dimension than men, and men would have a higher mean standing on the externalizing liability dimension. The presence of a gender invariant structure of common mental disorders would indicate that these gender differences in latent internalizing and externalizing liabilities account for the observed gender differences in prevalence rates. That is, gender differences in the prevalence of different manifest categorical disorders would be a function of mean-level gender differences in underlying liability dimensions. As such, these underlying dimensions, as opposed to their manifestations as specific observed categories of psychopathology, would be highlighted as important organizing constructs for official nosologies and for research on the role of gender in psychopathology.
Method
Participants
This study utilized data from 43,093 individuals who participated in the first wave of the NESARC, conducted in 2001-2002. The NESARC study's design has been detailed elsewhere (Grant & Dawson, 2006). The first wave of NESARC was a representative sample of the civilian, non-institutionalized United States population, aged 18 and older. Young adults, African Americans, and Hispanics were oversampled. Women composed 57% (n = 24,575). Race/ethnicity was selected by participants using census-defined categories: White (56.9%), Hispanic or Latino (19.3%), African-American (19.1%), Asian/Native Hawaiian/Pacific Islander (3.1%), and American Indian/Alaska Native (1.6%). Participants provided written informed consent after a complete description of the study.
Assessment
Lifetime and past 12-month DSM-IV diagnoses were made using the Alcohol Use Disorder and Associated Disabilities Interview Schedule—DSM-IV Version (AUDADIS-IV; Grant et al., 1995), a structured interview designed for experienced lay interviewers. Major depressive disorder, dysthymic disorder, generalized anxiety disorder, panic disorder, social phobia, specific phobia, alcohol dependence, nicotine dependence, marijuana dependence, other drug dependence, and antisocial personality disorder AUDADIS diagnoses were examined. The other drug dependence variable was created to collapse relatively uncommon forms of drug dependence (i.e., stimulants, opioids, sedatives, tranquilizers, cocaine, solvents, hallucinogens, heroin, and any other drug not assessed) into one variable whose variance would be sufficient for covariance structure modeling; the internal consistency of this variable was good (alpha = .77). In keeping with DSM-IV notions of personality disorder stability, antisocial personality disorder was assessed on a lifetime basis only; this lifetime diagnosis was used in both lifetime and 12-month analyses. The reliability of the AUDADIS diagnoses examined have been reported elsewhere and are generally good to excellent (e.g., kappas = .42 to .84; see Hasin et al., 2005). Test-retest estimates for AUDADIS-IV disorders are similar to other structured interviews (e.g., the DIS, the CIDI) used in large psychiatric epidemiologic surveys (reviewed in Wittchen, 1994). Further, the AUDADIS-IV has advantages over structured interviews such as the DIS, including assessment of clinically significant distress and impairment after the syndrome is fully characterized (Hasin et al., 2005).
Statistical Analyses
All analyses were conducted in Mplus version 6 (Muthén & Muthén, 2010) using the Mplus defaults of delta parameterization and WLSMV estimator. WLSMV allowed us to treat diagnostic variables as categorical and use the NESARC's weighting, clustering, and stratification variables. Odds ratios used men as the reference comparison group. To evaluate model fit in confirmatory factor analyses (CFAs), we considered the comparative fit index (CFI), Tucker-Lewis index (TLI), root mean squared error of approximation (RMSEA), and the number of freely estimated parameters in the model. CFI/TLI values > .95 and RMSEA values < .06 suggest good model fit (Hu & Bentler, 1999). Based on simulations, Cheung and Rensvold (2002) proposed a CFI difference critical value of .01 be used to test whether the addition of constraints leads to notably worse model fit in factorial invariance studies. More parsimonious models use fewer freely estimated parameters. In model comparisons, we therefore defined the optimal model by means of the best fit (CFI, TLI, and RMSEA), model parsimony (number of free parameters), and the CFI critical difference of .01. Distress and fear loadings on higher-order internalizing were constrained to equality to ensure model identification.
Results
Prevalence Rates
Table 1 presents the prevalence rates for the disorders included in the current study separately for men and women and for lifetime and 12-month disorders. All odds ratios were significant (all p < .001 except other drug dependence at p = .005). Across lifetime and 12-month prevalence rates, women showed higher rates for all internalizing disorders, and men showed higher rates for all externalizing disorders.
Table 1. Disorder prevalence rates and odds ratios by gender.
| Lifetime Disorders | 12-Month Disorders | |||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| Women (%) | Men (%) | Odds Ratio | Women (%) | Men (%) | Odds Ratio | |
| Depression | 22.9 | 13.1 | 1.46 (1.41-1.51) | 10.1 | 5.5 (1.32-1.45) | 1.38 |
| Dysthymia | 6.2 | 3.5 | 1.31 (1.25-1.38) | 2.9 | 1.6 (1.20-1.39) | 1.29 |
| Generalized Anxiety | 5.8 | 3.1 | 1.34 (1.27-1.42) | 3.1 | 1.4 (1.28-1.47) | 1.37 |
| Panic Disorder | 7.2 | 3.7 | 1.39 (1.32-1.47) | 3.1 | 1.4 (1.29-1.49) | 1.39 |
| Social Phobia | 5.8 | 4.3 | 1.16 (1.10-1.22) | 3.4 | 2.1 (1.15-1.29) | 1.22 |
| Specific Phobia | 12.4 | 6.2 | 1.47 (1.41-1.53) | 9.6 | 4.6 (1.40-1.53) | 1.46 |
| Alcohol Dependence | 8.0 | 17.4 | 0.63 (0.60-0.65) | 2.3 | 5.4 (0.64-.0.72) | 0.68 |
| Nicotine Dependence | 15.6 | 20.0 | 0.84 (0.81-0.87) | 11.5 | 14.1 (0.85-0.91) | 0.88 |
| Marijuana Dependence | 0.9 | 1.7 | 0.77 (0.71-0.83) | 0.2 | 0.5 (0.63-0.83) | 0.72 |
| Other Drug Dependence | 1.4 | 2.2 | 0.84 (0.79-0.90) | 0.3 | 0.5 (0.72-0.95) | 0.83* |
| Antisocial Personality | 1.9 | 5.5 | 0.68 (0.59-0.66) | |||
Note: All ORs significant at p < .001 except
p = .005.
Men are OR comparison group. 95% confidence intervals are given in parentheses. Antisocial personality disorder was only assessed as a lifetime disorder.
Comorbidity Structure
In CFAs (Table 2), guided by previous studies and exploratory factor analyses (not reported here for brevity), we parameterized each diagnosis to load on one of three factors: (1) distress: major depression, dysthymia, and generalized anxiety disorder; (2) fear: panic disorder, social phobia, and specific phobia; and (3) externalizing: alcohol dependence, nicotine dependence, marijuana dependence, and antisocial personality disorder. Distress and fear were parameterized to load on a higher-order internalizing factor, which was allowed to correlate with the externalizing factor. This internalizing-externalizing model provided a very good fit in the total sample for both lifetime and 12-month diagnoses. Within each gender modeled separately, this internalizing-externalizing model continued to fit very well for lifetime and 12-month diagnoses.
Table 2. Model fit statistics.
| CFI | TLI | RMSEA | # Free | |
|---|---|---|---|---|
| Total sample (N = 43,093) | ||||
| Lifetime diagnoses | .992 | .989 | .012 | -- |
| 12-month diagnoses | .988 | .984 | .010 | -- |
| Women (n = 24,575) | ||||
| Lifetime diagnoses | .993 | .991 | .009 | -- |
| 12-month diagnoses | .990 | .987 | .008 | -- |
| Men (n = 18,518) | ||||
| Lifetime diagnoses | .988 | .984 | .008 | -- |
| 12-month diagnoses | .982 | .976 | .007 | -- |
| Multigroup (Women and Men) | ||||
| Lifetime diagnoses | ||||
| Unconstrained model | .991 | .989 | .012 | 48 |
| Constrained model | .991 | .989 | .012 | 38 |
| 12-month diagnoses | ||||
| Unconstrained model | .987 | .983 | .010 | 48 |
| Constrained model | .988 | .986 | .009 | 38 |
Note: Total sample analyses modeled women and men together. Multigroup analyses modeled women and men simultaneously as two separate groups. Unconstrained models allowed each gender to have unique model parameters; constrained (invariant) models constrained factor loadings and thresholds to equality across genders. CFI: comparative fit index. TLI: Tucker-Lewis index. RMSEA: root mean squared error of approximation. # Free: number of freely estimated parameters.
Invariance
Because an internalizing-externalizing model fit well in women and men, our next question was how similar these models were across gender in terms of model parameters—that is, whether the magnitude of parameters differed by gender or whether they showed invariance. Tests of invariance for indicators such as diagnoses require methodology appropriate for modeling categorical variables (Millsap & Yun-Tein, 2004). In this approach, factor loadings and thresholds are constrained to equality or freed, in tandem, across genders. In our first model (the “unconstrained model”), loadings and thresholds were free across genders, factor means were set to zero in both genders, and scaling factors were fixed to one in both genders. In the second model (the “constrained model”), loadings and thresholds were constrained to equality across genders, factor means were set to zero in men and were free in women, and scaling factors were fixed to one in men and were free in women. This model represented a gender invariant psychopathology structure.
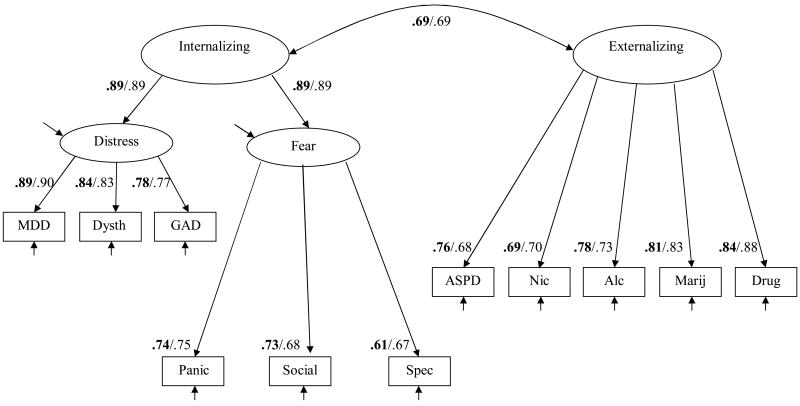
We fit the unconstrained and constrained models in men and women simultaneously via a multi-group CFA, separately for lifetime and 12-month diagnoses (see Table 2). For lifetime diagnoses, the fits of the two models were identical, but the constrained model had fewer freely estimated parameters than the unconstrained model. The constrained model for lifetime diagnoses is depicted in Figure 1. For 12-month diagnoses, the constrained model had a better fit with greater parsimony than did the unconstrained model. For lifetime and 12-month diagnoses, the CFI critical difference of .01 was not exceeded, further supporting the constrained model. These findings indicated that, in addition to the general structure, factor loadings and thresholds for all diagnoses were equivalent for women and men. Thus, the structure of these common mental disorders, including the connections between individual diagnoses and the underlying factors, could be considered gender invariant.
Figure 1.
The constrained (gender invariant) model in women and men using lifetime diagnoses.
Note. Values are standardized factor loadings (all significant p < .001). Values before slash and bolded are for women; values after slash are for men. Values differ slightly across gender due to standardization. MDD: major depressive disorder. Dysth: dysthymic disorder. GAD: generalized anxiety disorder. Panic: panic disorder. Social: social phobia. Spec: specific phobia. ASPD: antisocial PD. Nic: nicotine dependence. Alc: alcohol dependence. Marij: marijuana dependence. Drug: other drug dependence. Arrows without numbers indicate unique variances, including error.
In terms of factor means, means of these latent internalizing and externalizing factors were fixed to zero in men and freely estimated as .445 and -.378 in women, respectively, for lifetime diagnoses and as .428 and -.308 for 12-month diagnoses. All mean gender differences were significant at p < .01. These standardized means can be interpreted as z-scores (e.g., women were approximately .45 standard deviations higher on lifetime internalizing liability than men). Because complete factorial invariance had been established, these results demonstrated that the observed differences in the prevalence rates of the specific disorders modeled between women and men could be accounted for by the genders' different average levels of latent internalizing and externalizing.
Discussion
The current study sought to synthesize these two lines of research—patterns of gender differences in prevalence rates and a potentially gender invariant latent structure of psychopathology—via factorial invariance analyses of liability dimensions underlying DSM-IV disorder comorbidity. We found that the underlying structure of common mental disorders was gender invariant with significant gender differences in mean liability levels. This provides compelling evidence that observed gender differences in prevalence rates of many common mental disorders originate at the level of latent internalizing and externalizing liabilities.
Limitations
This study is not without its limitations. First, we examined lifetime diagnoses, which can be subject to memory biases. However, our results from lifetime diagnoses were highly congruent with results from 12-month diagnoses, which required much less retrospection. Second, our diagnostic information was collected by extensively trained lay interviewers rather than clinicians. This being said, it is noteworthy that the instrument used to assess symptomatology was fully structured, which resulted in generally good diagnostic reliability levels. Finally, the current study investigated only common mental disorders and thus did not include other debilitating forms of psychopathology, such as schizophrenia. There are indications that some symptoms of psychotic disorders may relate to a separate liability factor (e.g., thought disorder liability) while also showing associations with internalizing liability/neuroticism (e.g., Barrantes-Vidal, Ros-Morente, & Kwapil, 2009; Markon, 2010).
Implications
Classification
DSM-IV is currently under revision, and there has been a great deal of discussion about the general organization of DSM-5 (Regier et al., 2011). Based largely on replications of the internalizing-externalizing model, an organizational meta-structure for many common disorders reflecting this structure has been advocated (Andrews et al., 2009). Our findings support this proposal in two ways. First, we replicated the internalizing-externalizing structure in the NESARC, the largest epidemiologic study of psychopathology yet undertaken. Second, our results indicated that this structure is gender invariant. The current study represents the first time that gender invariance has been tested and successfully incorporated into the internalizing-externalizing liability model of comorbidity among categorical DSM-IV mental disorders in a representative sample. Taken together, these findings support an internalizing-externalizing meta-structure for many disorders in DSM-5, especially because the model is applicable in both women and men.
Gender differences research
Our conclusion that observed gender differences in prevalence rates systematically reflect gender differences in broad latent liability factors ties together distinct lines of research and theory on gender differences in prevalence rates for specific disorders. For instance, one major theory to account for gender differences in depression involves the notion that women ruminate more frequently than men, focusing repetitively on their negative emotions and problems rather than engaging in more active problem solving (Nolen-Hoeksema, 1987; Nolen-Hoeksema, Wisco, & Lyubomirksy, 2008). This theory can be readily extended to anxiety (and other internalizing disorders) by noting that neuroticism, or negative affectivity, is strongly related to rumination such that individuals who are more neurotic ruminate more frequently (Lam, Smith, Checkley, Rijsdijk, & Sham, 2003). Neuroticism is also strongly related to (r = .98), and nearly isomorphic with, the latent internalizing dimension reflecting the multivariate comorbidity among DSM mood and anxiety disorders (Griffith et al., 2010). This link between internalizing and trait neuroticism is itself accounted for largely by genetic effects (Hettema et al., 2006). Finally, previous research has indicated that women tend to report higher levels of trait neuroticism (as well as conscientiousness and agreeableness) on average than do men (e.g., Donnellan & Lucas, 2008), which mirrors our finding that women had significantly higher mean levels of internalizing than did men. It may be through neuroticism (and disinhibition-related traits in the case of externalizing and men; e.g., Krueger et al., 2002; Miller & Lynam, 2001; Slutske et al., 2002) that psychological processes impact latent propensities to experience comorbid mental disorders. Given that women tend to report higher frequencies of some stressful life events than men prior to disorder onset (Harkness et al., 2010), the interaction between these liabilities and environmental stressors seems a particularly worthwhile focus for gender differences research.
Intervention and prevention
Our results support recent efforts to develop interventions that target latent disorder liabilities. For instance, both anxious and depressive symptoms often respond to the same pharmacologic interventions (Goldberg et al., 2011). Similarly, anxiety and depression both respond well to cognitive-behavioral therapy, and there have been efforts to develop psychotherapeutic interventions that address the shared internalizing liability rather than solely focusing on its manifestations (Barlow et al., 2011). Along these lines, prevention efforts that focus on gender-linked core psychological processes are likely to be effective in impacting multiple disorders. In women, these preventative measures might focus, for instance, on coping and cognitive restructuring skills to reduce the likelihood of rumination and cognitive distortions developing into clinically significant depression or anxiety. In men, prevention might focus on rewarding planful behaviors and shaping disinhibitory tendencies into outlets that are not destructive to the self or others.
Acknowledgments
U01AA018111, R01DA018652, and K05AA014223 (Hasin); F31DA026689 (Keyes). The NESARC was sponsored by NIAAA and funded, in part, by the Intramural Program, NIAAA, with additional support from NIDA.
Footnotes
Declarations of interest: None.
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at www.apa.org/pubs/journals/abn
References
- Andrews G, Goldberg DP, Krueger RF, Carpenter WT, Jr, Hyman SE, Sachdev P, Pine DS. Exploring the feasibility of a meta-structure for DSM-V and ICD-11: Could it improve utility and validity? Psychological Medicine. 2009;39:1993–2000. doi: 10.1017/S0033291709990250. [DOI] [PubMed] [Google Scholar]
- Barlow DH, Farchione TJ, Fairholme CP, Ellard KK, Boisseau CL, Allen LB, Ehrenreich-May J. Unified protocol for transdiagnostic treatment of emotional disorders: Therapist guide. New York: Oxford University Press; 2011. [Google Scholar]
- Barrantes-Vidal N, Ros-Morente A, Kwapil TR. An examination of neuroticism as a moderating factor in the association of positive and negative schizotypy with psychopathology in a nonclinical sample. Schizophrenia Research. 2009;115:303–309. doi: 10.1016/j.schres.2009.09.021. [DOI] [PubMed] [Google Scholar]
- Cheung GW, Rensvold RB. Evaluating goodness-of-fit indexes for testing measurement invariance. Structural Equation Modeling. 2002;9:233–255. [Google Scholar]
- Dawson DA, Goldstein RB, Moss HB, Li TK, Grant BF. Gender differences in the relationship of internalizing and externalizing psychopathology to alcohol dependence: Likelihood, expression and course. Drug and Alcohol Dependence. 2010;112:9–17. doi: 10.1016/j.drugalcdep.2010.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donnellan MB, Lucas RE. Age differences in the Big Five across the life span: Evidence from two national samples. Psychology and Aging. 2009;23:558–566. doi: 10.1037/a0012897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eaton NR, South SC, Krueger RF. The meaning of comorbidity among common mental disorders. In: Millon T, Krueger RF, Simonsen E, editors. Contemporary directions in psychopathology. 2nd. New York: Guilford Publications; 2010. pp. 223–241. [Google Scholar]
- Goldberg D, Simms LJ, Gater R, Krueger RF. Integration of dimensional spectra for depression and anxiety into categorical diagnoses for general medical practice. In: Regier DA, Narrow WE, Kuhl EA, Kupfer DJ, editors. The conceptual evolution of DSM-5. Arlington, VA: American Psychiatric Publishing, Inc; 2011. pp. 19–35. [Google Scholar]
- Grant BF, Dawson DA. Introduction to the National Epidemiologic Survey on Alcohol and Related Conditions. Alcohol Research & Health. 2006;29(2):74–78. [Google Scholar]
- Grant BF, Dawson DA, Stinson FS, Chou SP, Dufour MC, Pickering RP. The 12-month prevalence and trends in DSM-IV alcohol abuse and dependence: United States, 1991-1992 and 2001-2002. Drug and Alcohol Dependence. 2004;74:223–234. doi: 10.1016/j.drugalcdep.2004.02.004. [DOI] [PubMed] [Google Scholar]
- Grant BF, Harford TC, Dawson DA, Chou PS, Pickering RP. The Alcohol Use Disorder and Associated Disabilities Interview Schedule (AUDADIS): Reliability of alcohol and drug modules in a general population sample. Drug and Alcohol Dependence. 1995;39:37–44. doi: 10.1016/0376-8716(95)01134-k. [DOI] [PubMed] [Google Scholar]
- Grant BF, Weissman MM. Gender and the prevalence of psychiatric disorders. In: Narrow WE, First MB, Sirovatka PJ, Regier DA, editors. Age and gender considerations in psychiatric diagnosis: A research agenda for DSM-V. Washington, DC: American Psychiatric Association; 2007. pp. 31–46. [Google Scholar]
- Griffith JW, Zinbarg RE, Craske MG, Mineka S, Rose RD, Waters AM, Sutton JM. Neuroticism as a common dimension in the internalizing disorders. Psychological Medicine. 2010;40:1125–1136. doi: 10.1017/S0033291709991449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harkness KL, Alavi N, Monroe SM, Slavich GM, Gotlib IH, Bagby RM. Gender differences in life events prior to onset of major depressive disorder: The moderating effect of age. Journal of Abnormal Psychology. 2010;119(4):791–803. doi: 10.1037/a0020629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasin DS, Goodwin RD, Stinson FS, Grant BF. Epidemiology of major depressive disorder: Results from the National Epidemiologic Survey on Alcoholism and Related Conditions. Archives of General Psychiatry. 2005;62:1097–1106. doi: 10.1001/archpsyc.62.10.1097. [DOI] [PubMed] [Google Scholar]
- Hettema JM, Neale MC, Myers JM, Prescott CA, Kendler KS. A population-based twin study of the relationship between neuroticism and internalizing disorders. American Journal of Psychiatry. 2006;163:857–864. doi: 10.1176/ajp.2006.163.5.857. [DOI] [PubMed] [Google Scholar]
- Hicks BM, Blonigen DM, Kramer MD, Krueger RF, Patrick CJ, Iacono WG, McGue M. Gender differences and developmental change in externalizing disorders from late adolescence to early adulthood: A longitudinal twin study. Journal of Abnormal Psychology. 2007;116:433–447. doi: 10.1037/0021-843X.116.3.433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6:1–55. [Google Scholar]
- Kendler KS, Prescott CA, Myers J, Neale MC. The structure of genetic and environmental risk factors for common psychiatric and substance use disorders in men and women. Archives of General Psychiatry. 2003;60:929–937. doi: 10.1001/archpsyc.60.9.929. [DOI] [PubMed] [Google Scholar]
- Kessler RC, McGonagle KA, Swartz M, Blazer DG, Nelson CB. Sex and depression in the National Comorbidity Survey I: Lifetime prevalence, chronicity and recurrence. Journal of Affective Disorders. 1993;29:85–96. doi: 10.1016/0165-0327(93)90026-g. [DOI] [PubMed] [Google Scholar]
- Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, Wittchen HU, Kendler KS. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: Results from the National Comorbidity Survey. Archives of General Psychiatry. 1994;51:8–19. doi: 10.1001/archpsyc.1994.03950010008002. [DOI] [PubMed] [Google Scholar]
- Keyes KM, Grant BF, Hasin DS. Evidence for a closing gender gap in alcohol use, abuse, and dependence in the United States population. Drug and Alcohol Dependence. 2008;93:21–29. doi: 10.1016/j.drugalcdep.2007.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klose M, Jacobi F. Can gender differences in the prevalence of mental disorders be explained by sociodemographic factors? Archives of Women's Mental Health. 2004;7:133–148. doi: 10.1007/s00737-004-0047-7. [DOI] [PubMed] [Google Scholar]
- Kramer MD, Krueger RF, Hicks BM. The role of internalizing and externalizing liability factors in accounting for gender differences in the prevalence of common psychopathological syndromes. Psychological Medicine. 2008;38:51–61. doi: 10.1017/S0033291707001572. [DOI] [PubMed] [Google Scholar]
- Krueger RF. The structure of common mental disorders. Archives of General Psychiatry. 1999;56:921–926. doi: 10.1001/archpsyc.56.10.921. [DOI] [PubMed] [Google Scholar]
- Krueger RF, Hicks BM, Patrick CJ, Carlson SR, Iacono WG, McGue M. Etiologic connections among substance dependence, antisocial behavior, and personality: Modeling the externalizing spectrum. Journal of Abnormal Psychology. 2002;3:411–424. [PubMed] [Google Scholar]
- Lam D, Smith N, Checkley S, Rijsdijk F, Sham P. Effect of neuroticism, response style and information processing on depression severity in a clinically depressed sample. Psychological Medicine. 2003;33:469–479. doi: 10.1017/s0033291702007304. [DOI] [PubMed] [Google Scholar]
- Markon KE. Modeling psychopathology structure: A symptom-level analysis of Axis I and II disorders. Psychological Medicine. 2010;40:273–288. doi: 10.1017/S0033291709990183. [DOI] [PubMed] [Google Scholar]
- Miller JD, Lynam D. Structural models of personality and their relation to antisocial behavior: A meta-analytic review. Criminology. 2001;39:765–798. [Google Scholar]
- Millsap RE, Yun-Tein J. Assessing factorial invariance in ordered-categorical measures. Multivariate Behavioral Research. 2004;39(3):479–515. [Google Scholar]
- Muthén LK, Muthén BO. Mplus user's guide. 5th. Los Angeles: Author; 2010. [Google Scholar]
- Nolen-Hoeksema S. Sex differences in unipolar depression: Evidence and theory. Psychological Bulletin. 1987;2:259–282. [PubMed] [Google Scholar]
- Nolen-Hoeksema S, Wisco BE, Lyubomirsky S. Rethinking rumination. Perspectives on Psychological Science. 2008;3(5):400–424. doi: 10.1111/j.1745-6924.2008.00088.x. [DOI] [PubMed] [Google Scholar]
- Piccinelli M, Wilkinson G. Gender differences in depression: Critical review. British Journal of Psychiatry. 2000;177:486–492. doi: 10.1192/bjp.177.6.486. [DOI] [PubMed] [Google Scholar]
- Regier DA, Narrow WE, Kuhl EA, Kupfer DJ, editors. The conceptual evolution of DSM-5. Arlington, VA: American Psychiatric Publishing, Inc; 2011. [Google Scholar]
- Shear K, Halmi KA, Widiger TA, Boyce C. Sociocultural factors and gender. In: Narrow WE, First MB, Sirovatka PJ, Regier DA, editors. Age and gender considerations in psychiatric diagnosis: A research agenda for DSM-V. Washington, DC: American Psychiatric Association; 2007. pp. 65–79. [Google Scholar]
- Slade T, Watson D. The structure of common DSM-IV and ICD-10 mental disorders in the Australian general population. Psychological Medicine. 2006;36:1593–1600. doi: 10.1017/S0033291706008452. [DOI] [PubMed] [Google Scholar]
- Trull TJ, Jahng S, Tomko RL, Wood PK, Sher KJ. Revised NESARC personality disorder diagnoses: Gender, prevalence, and comorbidity with substance dependence disorders. Journal of Personality Disorders. 2010;24(4):412–426. doi: 10.1521/pedi.2010.24.4.412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slutske WS, Heath AC, Madden PA, Bucholz KK, Statham DJ, Martin NG. Personality and the genetic risk for alcohol dependence. Journal of Abnormal Psychology. 2002;111:124–133. [PubMed] [Google Scholar]
- Vesga-López O, Schneier FR, Wang S, Heimberg RG, Liu SM, Hasin DS, Blaco C. Gender differences in generalized anxiety disorder: Results from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) Journal of Clinical Psychiatry. 2008;69:1606–1616. [PMC free article] [PubMed] [Google Scholar]
- Vollebergh WAM, Iedema J, Bijl RV, de Graaf R, Smit F, Ormel J. The structure and stability of common mental disorders: The NEMESIS study. Archives of General Psychiatry. 2001;58:597–603. doi: 10.1001/archpsyc.58.6.597. [DOI] [PubMed] [Google Scholar]
- Widiger TA. DSM's approach to gender: history and controversies. In: Narrow WE, First MB, Sirovatka PJ, Regier DA, editors. Age and gender considerations in psychiatric diagnosis: A research agenda for DSM-V. Washington, DC: American Psychiatric Association; 2007. pp. 31–46. [Google Scholar]
- Wittchen HU. Reliability and validity studies of the WHO-Composite International Diagnostic Interview (CIDI): A critical review. Journal of Psychiatry Research. 1994;28:57–84. doi: 10.1016/0022-3956(94)90036-1. [DOI] [PubMed] [Google Scholar]