Abstract
Background
Studies of specific groups such as military veterans have found that posttraumatic stress disorder (PTSD) is linked to adverse health outcomes including unhealthy weight. The aim of this study was to examine the relationship between PTSD symptoms, experiences of childhood trauma and weight in a community sample.
Methods
A stratified random probability survey was conducted in Denmark by the Danish National Centre for Social Research between 2008 and 2009 with 2,981 participants born in 1984, achieving a response rate of 67%. The participants were interviewed with a structured interview with questions pertaining PTSD symptomatology, exposure to childhood abuse, exposure to potentially traumatizing events, height, and weight. Underweight was defined by a body mass index (BMI) <18.5, overweight was defined by a BMI ≥25 and <30 and obesity was defined by a BMI ≥30.
Results
PTSD symptomatology and childhood abuse were significantly associated with both underweight and overweight/obesity. Childhood emotional abuse was especially associated with underweight, whereas sexual abuse and overall abuse were particularly associated with overweight/obesity.
Conclusion
These findings indicate that health care professionals may benefit from assessing PTSD and childhood abuse in the treatment of both overweight and underweight individuals.
Keywords: PTSD, childhood abuse, eating disorders, weight
Over the last number of years the obesity rate has reached epidemic proportions in most countries (WHO, 2000), and new studies show that 52% of the Danish population is overweight (Larsen, Ankersen, Poulsen & Christensen, 2010). The parallel rise in the prevalence of eating disorders such as Anorexia Nervosa (Hay, Mond, Buttner & Darby, 2008; Hudson, Hiripi, Pope & Kessler, 2007) has been mentioned less frequently.
Posttraumatic stress disorder (PTSD) and exposure to potentially traumatic events have been linked to adverse health outcomes, the onset of specific diseases, and premature death (Boscarino, 2004; Scott et al., 2011). One of these adverse health outcomes may be unhealthy weight. Some studies have focused on possible explanations for the connection between adverse life events and weight. A recent study (Akkermann et al., 2012) showed that adverse experiences in childhood may heighten susceptibility to serotonergic dysregulation, which was associated with both binge eating and drive for thinness in a cohort of the European Youth Heart Study. Several studies of specific groups such as military veterans (Vieweg et al., 2006) have found that the prevalence of overweight and obesity among male veterans with PTSD significantly exceeds national findings. Also studies with samples from the general population have found an association between PTSD and obesity (Mamun et al., 2007; Scott, McGee, Wells & Oakley Browne, 2008). A nationally representative survey in New Zealand (Scott et al., 2008) found that obesity was significantly associated with both mood disorders and anxiety disorders. The specific disorder that was most strongly associated with obesity was PTSD. Furthermore, studies (Swinbourne & Touyz, 2007) investigating the other end of the weight spectrum have shown that stressful life events are associated with anorexia nervosa. One study (Tagay, Schlegl & Senf, 2010) found that 63% of the anorectic patients in an outpatient treatment sample had experienced at least one trauma in their life, and 10% fulfilled the criteria for a current diagnosis of PTSD. A Danish study found that women with a history of eating disorders had experienced significantly more childhood abuse than women with no prior history of eating disorder (Blaase & Elklit, 2001).
However, most studies on the relationship between weight and PTSD have focused on obesity or have focused solely on eating disorder patients (Perkonigg, Owashi, Stein, Kirschbaum, & Wittchen, 2009; Scott et al., 2008). This article is an attempt to extend the knowledge of factors involved in a potential unhealthy weight at both ends of the weight spectrum. Additionally, a number of studies have found that childhood trauma is associated with both being underweight (Reyes-Rodriguez et al., 2011) and overweight (Mamun et al., 2007; Midei, Matthews & Bromberger, 2010; Pederson & Wilson, 2009). Despite these consistent findings, the mechanism for the added risk of obesity following childhood trauma is unknown. A recent review (Gustafson & Sarwer, 2004) suggested that disordered eating behavior, psychological, and/or physiological reactions to a traumatic experience may account for the added risk of adult obesity. For example, binge-eating behavior has been associated with childhood sexual abuse and an increased incidence of obesity (Gunstad, Schofield, et al., 2006). Therefore, the objective of the present study was to compare some core PTSD symptoms in a group of normal weight individuals with a group of persons with underweight and overweight respectively. To our knowledge, there have been no previous attempts to include both underweight and overweight, respectively in a general population sample. Also, this study explored the association between different categories of childhood abuse and weight status.
Methods
Procedure
A stratified random probability survey was conducted in Denmark by the Danish National Centre for Social Research between 2008 and 2009 in order to retrieve mental health related data from young Danish people. Statistics Denmark randomly selected 4,718 participants, aged 24 in 2008, from the total birth cohort of Denmark in 1984. To increase the number of participants who had experienced childhood abuse and neglect, children who had been in child protection were over-sampled by stratifying the number of “child protection cases” versus “non-child protection cases” (1/3:2/3) (see Table 1). A child protection case was defined as a case where the council (according to the files of local social workers) had provided support for the child and the family or placement with a foster family due to concerns about the well-being and development of the child. Individuals who had previously refused to participate in national research, who were incarcerated, deemed to have learning difficulties and who had moved out of the country were excluded. Individuals who were deemed to be child-protection cases (as evidenced through the files of local social work departments) were oversampled. Structured interviews were conducted by trained interviewers either in the home or via the telephone. Due to the sensitive nature of a number of the questions, those respondents who were interviewed in their homes could respond by entering their answers into a laptop computer. The average duration of the interviews equated to 43 min. Participation was entirely voluntary and post-interview psychological help was offered to all respondents via a telephone help-line. The study was approved by the Danish Data Protection Agency. Further details pertaining to the procedure will be published elsewhere.
Table 1.
Distribution of child non-protection cases and child protection cases
| Gender | Total sample weighted N=2,980 (%) | Child non-protection sample N=2,128 (%) | Child protection case N=852 (%) |
|---|---|---|---|
| Male | 1,555 (52.2) | 1,106 (52.0) | 473 (55.5) |
| Female | 1,425 (47.8) | 1,022 (48.0) | 379 (44.5) |
Participants
A total of 2,981 interviews were successfully conducted, equating to a response rate of 67%. Eight hundred and fifty-two interviews were conducted with individuals who had been previously identified by the Danish authorities as child protection cases. The most common reasons for non-participation were: refusal to take part in the study (21%), being uncontactable (13%), and illness or disability (2%). Unfortunately, a non-response analysis was not possible. Fifty-two percent of the sample was men. All demographics were analyzed employing a weight variable to account for the oversampling of child protection cases. Child protection status (weighted) was given to 6% of the total sample. The data was also weighted for non-response and the proportions in socio- demographic factors found in the general population.
Measures
The interview administered a series of questions pertaining to several psychological and physical domains. The response format was pre-coded; however, respondents were given the opportunity to elaborate if they wanted.
PTSD symptomatology was measured through four questions reflecting some core symptoms of PTSD: avoidance, re-experience, numbing, and hypervigility. The four questions were:
Have you had unpleasant experiences that you sometimes re-experience?
Have you experienced an event that was so terrifying that you have tried not to think of the event and avoid things that remind you of the event during the last month?
Have you experienced an event that was so terrifying that you have felt alert during the last month?
Have you experienced an event that was so terrifying that you have felt numb and detached from other people during the last month?
Because of the small numbers of individuals in some categories participants were categorized based on number of PTSD symptoms; (1) no symptoms, (2) 1–2 symptoms, or (3) 3–4 symptoms. Furthermore, because the number of traumatic experiences have been linked to adverse negative health outcomes (Kolassa, Kolassa, Ertl, Papassotiropoulos & De Quervain, 2010), this was also included in the analyses. The participants were asked to point out which of 17 selected, potentially traumatizing events they had been exposed to (see Table 2). The included events were selected from literature (Rhiger, Elklit & Lasgaard, 2008) and clinical experience, covering a broad spectrum of possible life-threatening experiences and distressing conditions. Data from previously similar studies supports that the included events are frequently experienced by youths across nations and cultures, and that these events may be potentially traumatizing (Elklit & Petersen, 2008). There exists conceptual overlap between a few of the potentially traumatizing events and the questions pertaining to child abuse experiences in this study.
Table 2.
Potentially traumatizing events
| 1 | Traffic accident |
| 2 | Fire |
| 3 | Accident |
| 4 | Physical assault |
| 5 | Threats of being beaten |
| 6 | Drowning |
| 7 | Robbery |
| 8 | Maltreatment |
| 9 | Humiliation |
| 10 | Rape |
| 11 | Suicide (self-attempted) |
| 12 | Suicide/suicide attempt (family) |
| 13 | Suicide/suicide attempt (friend) |
| 14 | Death (family) |
| 15 | Serious illness |
| 16 | Sexual abuse |
| 17 | Punishment |
Weight status was measured as Body Mass Index (kg/m2) calculated from self-reported height and weight. BMI is regarded as an accurate method for comparing weight status (Deitel & Greenstein, 2003). Participants were divided into four sub-groups according to their BMI: Underweight was defined as a BMI < 18.5, normal weight as a BMI ≥18.5 and <25, overweight as a BMI ≥25 and <30, and obesity as a BMI ≥30.
Childhood abuse was measured using a similar approach as May-Chacal and Cawson (2005). The present study asked participants questions regarding specific experiences of four types of maltreatment; physical abuse, sexual abuse, emotional maltreatment and physical neglect, a method not dependent of subjective interpretations of whether maltreatment has occurred or not. Childhood abuse categories were based on latent class analyses (further information will published elsewhere) and the respondents were divided into four distinct childhood abuse categories:
Non-abused.
Emotional abused.
Sexual abused.
Abused overall.
The category of “abused overall” covers a distinct group of individuals who were exposed to all three types of abuse (i.e., physical abuse, emotional abuse, and neglect).
Statistical analyses
Chi-square analyses were conducted to examine the relationship between (1) PTSD symptomatology and BMI categories, (2) PTSD symptomatology and child abuse categories, and (3) child abuse categories and BMI categories. A one way ANOVA analysis was used to examine the relationship between BMI categories and number of potential traumatic events. All analyses were conducted using IBMs SPSS statistics 19. Finally, logistic regression was performed to assess the impact of a number of factors on the likelihood that respondents would be in either the normal weight group or in the underweight, overweight or obese group, respectively.
Results
Descriptives
BMI
The mean BMI was 23.84 (SD 3.81). Of the included participants 83 (3%) of the participants were underweight, 2,018 (68%) of the participants were normal weight, 650 (22%) of the participants were overweight, and the remaining 197 (7%) participants were obese. Information on BMI was lacking on 33 individuals (1%).
PTSD
The majority, 2,176 (73%) of the included participants, did not have any symptoms of PTSD. A total of 637 (21%) individuals reported having one or two symptoms of PTSD, and 168 individuals (6%) had three or four symptoms of PTSD.
Childhood abuse
Two hundred and sixty-three (9%) of the participants reported being emotionally abused during childhood, 59 individuals (2%) reported being sexually abused, and 64 (2%) of the participants had experienced overall abuse (e.g., physical abuse, emotional abuse, and neglect).
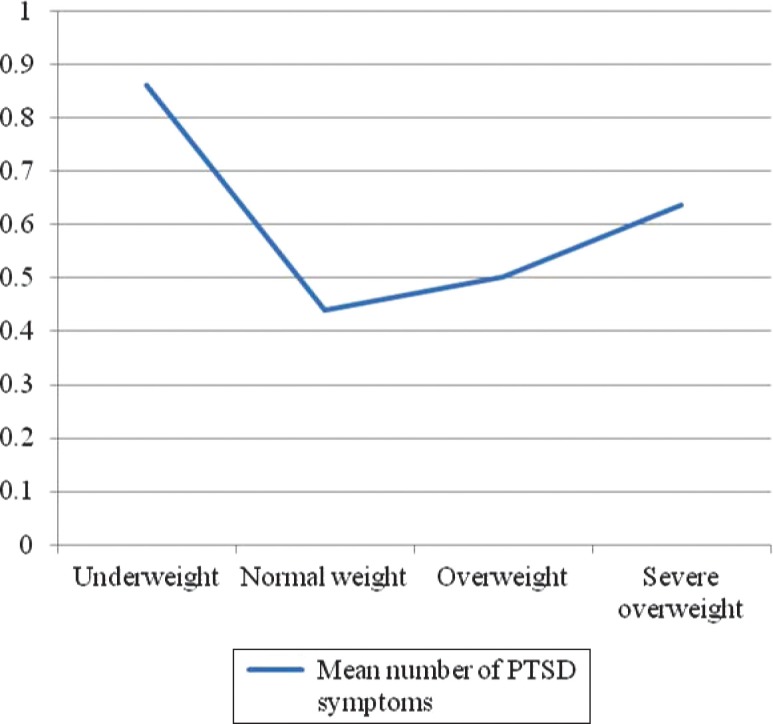
Relationships between BMI categories and PTSD symptom categories
The chi-square for independence indicated a significant association between BMI categories and PTSD status (χ 2 =20.23, p < .001; see Table 3). As illustrated in Fig. 1, people who were underweight or overweight/obese reported more PTSD symptoms than respondents with a normal BMI. Furthermore, the percentage of persons with 3–4 symptoms of PTSD was higher in the population of underweight individuals compared to the group of overweight and obese individuals.
Table 3.
BMI and PTSD symptom categories
| Number of PTSD symptoms | ||||
|---|---|---|---|---|
|
|
||||
| 0 | I–II | III–IV | ||
| Underweight | n | 50 | 21 | 12 |
| % of PTSD class | 2.3 | 3.3 | 7.3 | |
| Normal weight | n | 1,503 | 417 | 98 |
| % of PTSD class | 69.7 | 66.5 | 59.4 | |
| Overweight | n | 478 | 131 | 42 |
| % of PTSD class | 22.2 | 20.9 | 25.5 | |
| Obese | n | 126 | 58 | 13 |
| % of PTSD class | 5.8 | 9.3 | 7.9 | |
Fig. 1.
Associations between BMI categories and average number of PTSD symptoms.
Post hoc tests were performed comparing respondents in the normal weight group with the respondents in the underweight group, the overweight group, and the obese group independently. These analyses revealed that there was no statistically significant differences between the normal weight group and the overweight group in the number of reported PTSD symptoms (χ 2=.29, p=.287). The largest difference found in the analysis was between the underweight group and the normal weight group (χ 2 =17.41, p < .002) followed by the difference between the obese group and the normal weight group (χ 2 =10.28, p<.006).
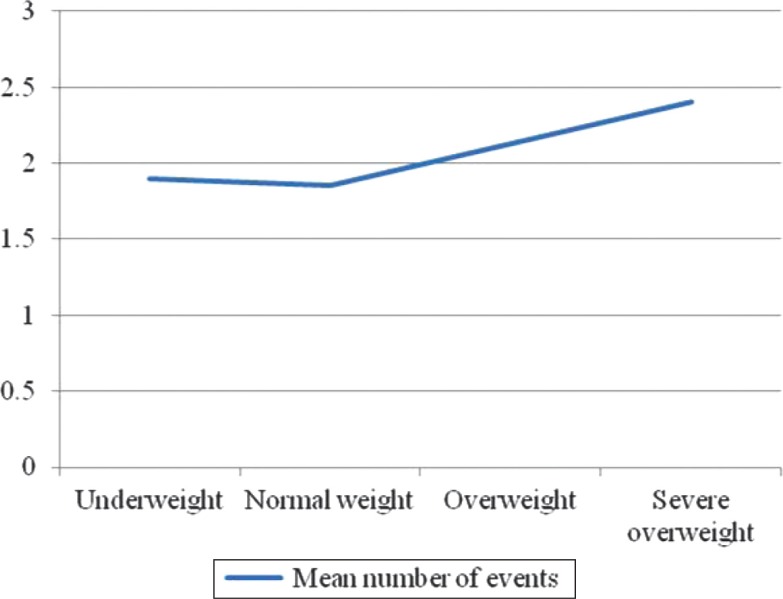
Relationships between BMI and total number of potential traumatic events
A one-way ANOVA was conducted to compare the number of reported potentially traumatic events between the different BMI categories. The means and standard deviations are presented in Table 4. As illustrated in Fig. 2 the number of potential traumatic events were highest in the groups of overweight and obese individuals (F (3.2944) = 8.02, p<.001).
Table 4.
BMI categories and number of events
| N | Mean | SD | |
|---|---|---|---|
| Underweight | 83 | 1.89 | 1.96 |
| Normal weight | 2,018 | 1.85 | 1.67 |
| Overweight | 650 | 2.12 | 1.85 |
| Obese | 197 | 2.40 | 1.88 |
Fig. 2.
Associations between BMI categories and average number of total events.
Relationships between BMI, PTSD symptoms, and childhood trauma categories
The chi-square for independence indicated a significant association between childhood trauma categories and PTSD symptoms (χ 2=309.20, p<.001). Specifically, the categories of sexual abuse and overall abuse were associated with a higher number of PTSD symptoms.
The chi-square for independence also indicated a significant association between childhood trauma categories and BMI categories (χ 2=20.36, p<.016). Cross tabulations revealed that different categories of childhood abuse were related to underweight and overweight/obesity, respectively (see Table 5). Childhood emotional abuse was especially associated with underweight, whereas sexual abuse and overall abuse were associated with overweight/obesity in specific.
Table 5.
BMI and childhood abuse categories
| Childhood abuse categories | |||||
|---|---|---|---|---|---|
|
|
|||||
| Emotionally abused | Sexually abused | Abused overall | Non-abused | ||
| Underweight | n | 13 | 0 | 2 | 68 |
| % within abuse class | 5.0 | .0 | 3.2 | 2.6 | |
| Normal weight | n | 166 | 44 | 35 | 1,773 |
| % within abuse class | 64.3 | 74.6 | 55.6 | 69.0 | |
| Overweight | n | 62 | 8 | 17 | 563 |
| % within abuse class | 24.0 | 13.6 | 27.0 | 21.9 | |
| Obese | n | 17 | 7 | 9 | 164 |
| % within abuse class | 6.6 | 11.9 | 14.3 | 6.4 | |
Post hoc test was performed comparing respondents in the normal weight group with the respondents in the underweight group, the overweight group, and the obese group independently. These analyses revealed that the only statistically significant difference was between the obese group and the normal weight group in the type of childhood trauma reported (χ 2 =9.20, p<.027). The result of the analysis of the underweight group versus normal weight group approached statistical significance (p = .057).
Impact of a number of factors on weight status
Logistic regression was performed to assess the impact of a number of factors on the likelihood that respondents would be in either the normal weight group or in the underweight, overweight or obese group, respectively. The model contained four independent variables (gender, number of PTSD symptoms, type of childhood trauma, and total number of potentially traumatizing events).
Underweight versus normal weight
The model reached statistical significance (χ 2(4, 2026) = 36.91, p<.001) indicating that the model was able to distinguish between respondents who were underweight or normal weight. The model as a whole explained between 1.7% (Cox and Snell R 2) and 6.2% (Nagelkerke R 2) of the variance in BMI. As shown in Table 6, only two of the independent variables made a unique statistically significant contribution to the model (gender [being female] and number of PTSD symptoms).
Table 6.
Logistic regression predicting likelihood of being underweight
| p | Odds ratio | |
|---|---|---|
| No. of PTSD symptoms | .001 | 1.45 |
| Total no. of events | .212 | .91 |
| Gender | <.001 | 1.31 |
| Type of childhood trauma | .319 | .89 |
| Constant | <.001 | .02 |
Overweight versus normal weight
The model reached statistical significance (χ 2(4, 2604) = 44.25, p<.001) indicating that the model was able to distinguish between respondents who were underweight or normal weight. The model as a whole explained between 1.6% (Cox and Snell R 2) and 2.5% (Nagelkerke R 2) of the variance in BMI. As shown in Table 7, only two of the independent variables made a unique statistically significant contribution to the model (gender [being male] and total number of potentially traumatizing events).
Table 7.
Logistic regression predicting likelihood of being overweight
| p | Odds ratio | |
|---|---|---|
| No. of PTSD symptoms | .416 | 1.05 |
| Total no. of events | .010 | 1.08 |
| Gender | <.001 | .88 |
| Type of childhood trauma | .951 | 1.0 |
| Constant | <.001 | .40 |
Obesity versus normal weight
The model reached statistical significance (χ 2(4, 2173) = 17.81, p < .001) indicating that the model was able to distinguish between respondents who were obese or normal weight. The model as a whole explained between 0.8% (Cox and Snell R2) and 1.8% (Nagelkerke R 2) of the variance in BMI. As shown in Table 8, only the total number of potentially traumatizing events made a unique statistically significant contribution to the model.
Table 8.
Logistic regression predicting likelihood of being obese
| p | Odds ratio | |
|---|---|---|
| No. of PTSD symptoms | .192 | 1.12 |
| Total no. of events | .001 | 1.15 |
| Gender | .831 | .99 |
| Type of childhood trauma | .729 | 1.03 |
| Constant | <.001 | .06 |
Discussion
The specific aims of the current study were two-fold. First, we wanted to determine if there was an association between BMI and PTSD symptomatology in a general population based survey of Danish young adults. Secondly we wanted to explore the association between different categories of childhood abuse and BMI status. In relation to the first objective of this study, results supported an association between PTSD symptomatology and BMI status. Both underweight and obese participants reported significantly more PTSD symptoms than participants within a normal weight range. Participants with PTSD symptoms were more than twice as likely to be underweight than participants in the general sample. Likewise, respondents with PTSD symptoms were more prevalent among obese individuals than among participants in the normal weight range. Post hoc analyses revealed that the association between PTSD symptoms and obesity was less pronounced as the association between PTSD symptoms and underweight. Furthermore, PTSD symptoms were not significantly associated with overweight but only with obesity.
In relation to the second objective of this study, results indicated a significant association between childhood abuse and BMI. Post hoc analyses revealed that the only statistical significant difference was between the obese group and the normal weight group in the type of childhood trauma reported, whereas the result of the analysis of the underweight group versus normal weight group approached statistical significance. Recent research suggests that obesity and eating disorders such as Anorexia Nervosa may have both shared and distinct susceptibility factors (Day, Ternouth & Collier, 2009). Although Anorexia Nervosa is not necessarily equal to the concept of underweight, this study indicates that PTSD symptomatology and exposure to childhood abuse may be shared susceptibility factors for developing both underweight and overweight. It has been suggested that childhood abuse may interfere with mechanisms of emotional regulation (Wonderlich et al., 2007). Emotional dysregulation has been associated with both traditional eating disorders and obesity. Wonderlich et al. (2007) suggest that restrictive eating or binge-purge behavior may reflect instrumental behaviors aimed at regulating negative affect. Similarly, emotional eating has been associated with obesity, and it is described as the tendency to eat in an effort of regulating negative emotions. Research shows that obese individuals engage in significantly more emotional eating compared to non-obese people (Pinaquy, Chabrol, Simon, Louvet & Barbe, 2003). Other studies have focused on other risk factors involved in both under- and overweight. These factors include various physiological factors such as similar genetic dispositions (Gunstad, Paul et al., 2006) and changes in the serotonin system, which have been linked to PTSD (Bremner, Southwick & Charney, 1999) and to both overeating and a drive for thinness (Akkermann et al., 2012). Finally, changes in the HPA axis and thereby the secretion of cortisol have been linked to both PTSD (Nemeroff et al., 2006) and the metabolic syndrome which is closely associated to overweight (Rosmond, 2005).
However, research (Day et al., 2009) also indicates that other risk factors affect whether a person becomes underweight or overweight after experiencing a shared risk factor. The present study indicates that type of childhood abuse may act as a separating susceptibility factor. The reporting of a history of childhood emotional abuse was associated with underweight, whereas reporting a history of childhood sexual abuse and overall abuse were associated with overweight. These results are consistent with other research supporting that different forms of child maltreatment may bear specific relationships to different health behaviors (Wonderlich et al., 2007). Although research on eating disorders are not directly transferable to underweight Wonderlich et al. (2007) have found that emotional abuse was particularly associated with bulimia nervosa and anorexia nervosa, and suggests that emotional abuse may influence risk factors that are especially relevant for those disorders. Furthermore, our study indicates that sexual abuse and overall abuse may influence risk factors of special relevance for the development of obesity. Authors have suggested that obesity might be a defense mechanism for victims of sexual abuse, seeking to minimize the risk of future abuse by the opposite sex (Ray, Nickels, Sayeed & Sax, 2003). More research is needed in order to fully understand the effect of distinct childhood abuse categories on the development of underweight and overweight. Furthermore, the performing of logistic regression analyses in this study indicated that PTSD symptoms were a significant predictor of underweight whereas the exposure of several traumatic events was a significant predictor of obesity. These findings may indicate that PTSD and the amount of traumatic experiences may be important factors in the understanding of the association between trauma and BMI. Prospective studies are needed in the future to understand the causal connections between childhood abuse, PTSD and BMI.
The findings of the present study must be interpreted in the context of several limitations. A limitation pertaining to this study is inherent in the research concerned with childhood maltreatment. Different definitions of what constitutes childhood abuse exist, and there appears to be no standardized measure of childhood maltreatment. Therefore, comparisons of results between studies are fraught with difficulty. Furthermore, the current study did not assess the frequency, or duration of abuse; rather participants were asked to endorse an experience by responding yes or no. Other studies have shown that severity of childhood abuse affect the magnitude of psychological disorders (Wonderlich et al., 2007). In addition, the current study relies on the self-reporting of abuse. Another limitation in the present study is the measure of PTSD symptomatology. The study did not include a complete PTSD measurement but consisted of only four PTSD symptoms which limit the possibility of comparing the results of our study with findings from other studies. Furthermore, using a measure of only four PTSD symptoms is a very brief measure and provides only an estimate of PTSD symptomatology. However, the four symptoms included in this study are representative of the three PTSD clusters—re-experiencing, avoidance, and hypervigility—and are considered central to the PTSD diagnosis. Earlier studies with brief measures of PTSD like SPAN (4 items; Sijbrandij, Olff, Opmeer, Carlier & Gersons, 2008) and PTSD-8 (8 items; Hansen et al., 2010) have shown that using core symptoms as a screening measure accurately predict trauma survivors at risk for developing PTSD. A third limitation concerns the limited age-span. The participants in this study were 24 years of age, and therefore the results of the present study might not be representative of other age groups. Additionally, BMI was calculated from self-reported height and weight. Studies have shown that overweight individuals have a tendency to underreport weight (Roberts, 1995). Finally, the cross-sectional design limits the ability to examine causal relationships between the investigated variables.
In the context of these limitations, this study provides valuable knowledge of possible associations between PTSD and BMI, and childhood abuse and BMI. To our knowledge, this is the first study that has included individuals with both an underweight and overweight BMI in relation to PTSD. Research in this area seems only present in relation to clinical populations, i.e., anorexia nervosa and bulimia nervosa or in studies on the association between psychological distress and weight not including a PTSD measure (Hwang, Lee, Kim, Chung & Kim, 2010; Zhao et al., 2009). The results of this study seem to support findings from this research and extend earlier findings to a specific birth cohort in the general population.
Conclusion
The serious health risks associated with an unhealthy body weight demand attention to the potential risk factors for an unhealthy weight status. Therefore, this study set out to explore potential relationships between PTSD, childhood abuse and weight status in a national sample. This study indicates that PTSD symptomatology and exposure to childhood abuse may be shared susceptibility factors for developing both underweight and obesity. Furthermore, different types of childhood abuse categories may be particularly relevant for underweight or obesity, respectively. These findings indicate that health care professionals may profit from assessing PTSD in the treatment of both obese and underweight individuals. Prospective studies are needed in order to fully understand the causal relationship between PTSD, childhood abuse and unhealthy body weight.
For the abstract or full text in other languages, please see Supplementary files under Reading Tools online
Conflict of interest and funding
There is no conflict of interest in the present study for any of the authors.
References
- Akkermann K, Kaasik K, Kiive E, Nordquist N, Oreland L, Harro J. The impact of adverse life events and the serotonin transporter gene promoter polymorphism on the development of eating disorder symptoms. Journal of Psychiatric Research. 2012;46(1):38–43. doi: 10.1016/j.jpsychires.2011.09.013. [DOI] [PubMed] [Google Scholar]
- Blaase H, Elklit A. Psychological characteristics of women with eating disorders: Permanent or transient features? Scandinavian Journal of Psychology. 2001;42(5):467–478. doi: 10.1111/1467-9450.00260. [DOI] [PubMed] [Google Scholar]
- Boscarino J. A. Posttraumatic stress disorder and physical illness: Results from clinical and epidemiologic studies. In: Yehuda R, McEwen B, editors. Biobehavioral stress response: Protective and damaging effects. New York: New York Academy of Sciences, NY; 2004. pp. 141–153. [DOI] [PubMed] [Google Scholar]
- Bremner J. D, Southwick S. M, Charney D. S. The neurobiology of posttraumatic stress disorder: An integration of animal and human research. In: Saigh R, Bremner J, editors. Posttraumatic stress disorder: A comprehensive text. Needham Heights, MA: Allyn & Bacon; 1999. pp. 103–143. [Google Scholar]
- Day J, Ternouth A, Collier D. A. Eating disorders and obesity: Two sides of the same coin? Epidemiology and Psychiatric Sciences. 2009;18(2):96–100. [PubMed] [Google Scholar]
- Deitel M, Greenstein R. J. Recommendations for reporting weight loss. Obese Surgery. 2003;13(2):159–160. doi: 10.1381/096089203764467117. [DOI] [PubMed] [Google Scholar]
- Elklit A, Petersen T. Exposure to traumatic events among adolescents in four nations. Torture. 2008;18(1):2–11. [PubMed] [Google Scholar]
- Gunstad J, Paul R. H, Spitznagel M. B, Cohen R. A, Williams L. M, Kohn M, et al. Exposure to early life trauma is associated with adult obesity. Psychiatry Research. 2006;142(1):31–37. doi: 10.1016/j.psychres.2005.11.007. [DOI] [PubMed] [Google Scholar]
- Gunstad J, Schofield P, Paul R. H, Spitznagel M. B, Cohen R. A, Williams L. M, et al. BDNF Val66Met polymorphism is associated with body mass index in healthy adults. Neuropsychobiology. 2006;53(3):153–156. doi: 10.1159/000093341. [DOI] [PubMed] [Google Scholar]
- Gustafson T. B, Sarwer D. B. Childhood sexual abuse and obesity. Obesity Review. 2004;5(3):129–135. doi: 10.1111/j.1467-789X.2004.00145.x. [DOI] [PubMed] [Google Scholar]
- Hansen M, Andersen T. E, Armour C, Elklit A, Palic S, Mackrill T. PTSD-8: A short PTSD inventory. [Peer Reviewed] Clinical Practice and Epidemiology in Mental Health. 2010;6:101–108. doi: 10.2174/1745017901006010101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hay P. J, Mond J, Buttner P, Darby A. Eating disorder behaviors are increasing: Findings from two sequential community surveys in South Australia. PLoS One. 2008;3(2):e1541. doi: 10.1371/journal.pone.0001541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hudson J. I, Hiripi E, Pope H. G, Jr, Kessler R. C. The Prevalence and Correlates of Eating Disorders in the National Comorbidity Survey Replication. Biological Psychiatry. 2007;61(3):348–358. doi: 10.1016/j.biopsych.2006.03.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hwang J. Y, Lee S. E, Kim S. H, Chung H. W, Kim W. Y. Psychological distress is associated with inadequate dietary intake in Vietnamese marriage immigrant women in Korea. Journal of the American Dietetic Association. 2010;110(5):779–785. doi: 10.1016/j.jada.2010.02.004. [DOI] [PubMed] [Google Scholar]
- Kolassa I. T, Kolassa S, Ertl V, Papassotiropoulos A, De Quervain D. J. The risk of posttraumatic stress disorder after trauma depends on traumatic load and the catechol-o-methyltransferase Val(158)Met polymorphism. Biological Psychiatry. 2010;67(4):304–308. doi: 10.1016/j.biopsych.2009.10.009. [DOI] [PubMed] [Google Scholar]
- Larsen F. B, Ankersen P. V, Poulsen S, Søe D, Christensen S. M. Hvordan har du det 2010? Sundhedsprofil for region og kommuner. 2010. Retrieved September 2011, from http://test1.rm.dk/files/Sundhed/CFK%20Folkesundhed%20og%20Kvalitetsudvikling/Projekter%20-%20subsites/HHDD%20-%20sundhedsprofil/HVORDAN%20HAR%20DU%20DET_2010/Rapporter%20-%20sundhedsprofil%202010/Hvordan%20har%20du%20det%202010_hovedrapport_samlet_til%20CFF.pdf.
- Mamun A. A, Lawlor D. A, O'Callaghan M. J, Bor W, Williams G. M, Najman J. M. Does childhood sexual abuse predict young adult's BMI? A birth cohort study. Obesity. 2007;15(8):2103–2110. doi: 10.1038/oby.2007.250. [DOI] [PubMed] [Google Scholar]
- May-Chacal C, Cawson P. Measuring child maltreatment in the United Kingdom: A study of child abuse and neglect. Child Abuse and Neglect. 2005;29(9):969–984. doi: 10.1016/j.chiabu.2004.05.009. [DOI] [PubMed] [Google Scholar]
- Midei A. J, Matthews K. A, Bromberger J. T. Childhood abuse is associated with adiposity in midlife women: Possible pathways through trait anger and reproductive hormones. Psychosomatic Medicine. 2010;72(2):215–223. doi: 10.1097/PSY.0b013e3181cb5c24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nemeroff C. B, Bremner J, Foa E. B, Mayberg H. S, North C. S, Stein M. B. Posttraumatic stress disorder: A state-of-the-science review. Journal of Psychiatric Research. 2006;40(1):1–21. doi: 10.1016/j.jpsychires.2005.07.005. [DOI] [PubMed] [Google Scholar]
- Pederson C. L, Wilson J. F. Childhood emotional neglect related to posttraumatic stress disorder symptoms and body mass index in adult women. Psychological Reports. 2009;105(1):111–126. doi: 10.2466/PR0.105.1.111-126. [DOI] [PubMed] [Google Scholar]
- Perkonigg A, Owashi T, Stein M. B, Kirschbaum C, Wittchen H.-U. Posttraumatic stress disorder and obesity evidence for a risk association. American Journal of Preventive Medicine. 2009;36(1):1–8. doi: 10.1016/j.amepre.2008.09.026. [DOI] [PubMed] [Google Scholar]
- Pinaquy S, Chabrol H, Simon C, Louvet J. P, Barbe P. Emotional eating, alexithymia, and binge-eating disorder in obese women. Obesity Research. 2003;11(2):195–201. doi: 10.1038/oby.2003.31. [DOI] [PubMed] [Google Scholar]
- Ray E. C, Nickels M. W, Sayeed S, Sax H. C. Predicting success after gastric bypass: The role of psychosocial and behavioral factors. Surgery. 2003;134(4):555–563. doi: 10.1016/s0039-6060(03)00279-4. discussion 563–554. [DOI] [PubMed] [Google Scholar]
- Reyes-Rodriguez M. L, Von Holle A, Ulman T. F, Thornton L. M, Klump K. L, Brandt H, et al. Posttraumatic stress disorder in anorexia nervosa. Psychosomatic Medicine. 2011;73(6):491–497. doi: 10.1097/PSY.0b013e31822232bb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhiger M, Elklit A, Lasgaard M. Traumatic in Israeli youth sample: An investigation of the prevalence and psychological impact of exposure to traumatic experiences. Nordic Psychology. 2008;60(2):101–113. [Google Scholar]
- Roberts R. J. Can self-reported data accurately describe the prevalence of overweight? Public Health. 1995;109(4):275–284. doi: 10.1016/s0033-3506(95)80205-3. [DOI] [PubMed] [Google Scholar]
- Rosmond R. Role of stress in the pathogenesis of the metabolic syndrome. Psychoneuroendocrinology. 2005;30(1):1–10. doi: 10.1016/j.psyneuen.2004.05.007. [DOI] [PubMed] [Google Scholar]
- Scott K. M, McGee M. A, Wells J. E, Oakley Browne M. A. Obesity and mental disorders in the adult general population. Journal of Psychosomatic Research. 2008;64(1):97–105. doi: 10.1016/j.jpsychores.2007.09.006. [DOI] [PubMed] [Google Scholar]
- Scott K. M, Von Korff M, Angermeyer M. C, Benjet C, Bruffaerts R, de Girolamo G, et al. Association of childhood adversities and early-onset mental disorders with adult-onset chronic physical conditions. Archives of General Psychiatry. 2011;68(8):838–844. doi: 10.1001/archgenpsychiatry.2011.77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sijbrandij M, Olff M, Opmeer B. C, Carlier I. V, Gersons B. P. Early prognostic screening for posttraumatic stress disorder with the Davidson Trauma Scale and the SPAN. Depression and Anxiety. 2008;25(12):1038–1045. doi: 10.1002/da.20441. [DOI] [PubMed] [Google Scholar]
- Swinbourne J. M, Touyz S. W. The co-morbidity of eating disorders and anxiety disorders: A review. European Eating Disorders Review. 2007;15(4):253–274. doi: 10.1002/erv.784. [DOI] [PubMed] [Google Scholar]
- Tagay S, Schlegl S, Senf W. Traumatic events, posttraumatic stress symptomatology and somatoform symptoms in eating disorder patients. European Eating Disorders Review. 2010;18(2):124–132. doi: 10.1002/erv.972. [DOI] [PubMed] [Google Scholar]
- Vieweg W. V, Julius D. A, Fernandez A, Tassone D. M, Narla S. N, Pandurangi A. K. Posttraumatic stress disorder in male military veterans with comorbid overweight and obesity: Psychotropic, antihypertensive, and metabolic medications. The Primary Care Companion to the Journal of Clinical Psychiatry. 2006;8(1):25–31. doi: 10.4088/pcc.v08n0104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO Consultation on Obesity. Obesity: Preventing and managing the global epidemic; Geneva, Switzerland: World Health Organization; 2000. WHO Technical Report Series 894. [PubMed] [Google Scholar]
- Wonderlich S. A, Rosenfeldt S, Crosby R. D, Mitchell J. E, Engel S. G, Smyth J, et al. The effects of childhood trauma on daily mood lability and comorbid psychopathology in bulimia nervosa. Journal of Traumatic Stress. 2007;20(1):77–87. doi: 10.1002/jts.20184. [DOI] [PubMed] [Google Scholar]
- Zhao G, Ford E. S, Li C, Strine T. W, Dhingra S, Berry J. T, et al. Serious psychological distress and its associations with body mass index: Findings from the 2007 Behavioral Risk Factor Surveillance System. International Journal of Public Health. 2009;54(Suppl 1):30–36. doi: 10.1007/s00038-009-0004-3. [DOI] [PubMed] [Google Scholar]