Abstract
Affect regulation is often compromised as a result of early life interpersonal traumatization and disruption in caregiving relationships like in situations where the caretaker is emotionally, sexually or physically abusing the child. Prior studies suggest a clear relationship between early childhood attachment-related psychological trauma and affect dysregulation. We evaluated the relationship of retrospectively recalled childhood traumatization by primary caretaker(s) (TPC) and affect dysregulation in 472 adult psychiatric patients diagnosed with borderline personality disorder (BPD), somatoform disorder (SoD), both BPD and SoD, or disorders other than BPD or SoD, using the Bermond-Vorst Alexithymia Questionnaire, the self-report version of the Structured Interview for Disorders of Extreme Stress, the Self-rating Inventory for Posttraumatic Stress Disorder (SRIP) and the Traumatic Experiences Checklist. Almost two-thirds of participants reported having experienced childhood TPC, ranging from approximately 50% of patients with SoD or other psychiatric disorders to more than 75% of patients with comorbid BPD+SoD. Underregulation of affect was associated with emotional TPC and TPC occurring in developmental epoch 0–6 years. Over-regulation of affect was associated with physical TPC. Childhood trauma by a primary caretaker is prevalent among psychiatric patients, particularly those with BPD, and differentially associated with underand over-regulation of affect depending on the type of traumatic exposure.
Keywords: Borderline personality disorder, somatoform disorders, child abuse, affect dysregulation
Affect dysregulation has been defined in two distinct ways (Paivio & Laurent, 2001; Taylor, Bagby, & Parker, 1997; Van Dijke, 2008; Van Dijke, Ford, et al., 2010). In the borderline personality disorder (BPD) literature, affect dysregulation refers to a deficiency in the capacity to modulate affect such that emotions become uncontrolled, expressed in intense and unmodified forms, and overwhelm reasoning (Koeningberg et al., 2002; Zittel Conklin, Bradley, & Westen, 2006; Zittel Conklin & Westen, 2005). These problems have been described as under-regulation of affect and include extremely intense affective distress (e.g., overwhelming rage or fear) and affectively driven behavioral disinhibition (e.g., impulsivity, aggression). Under-regulation of affect has been shown to be a common and potentially severe sequela of childhood sexual (Carey, Walker, Rossouw, Seedat, & Stein, 2008; Putnam, 2003), physical (Dodge, Lochman, Harnish, Bates, & Pettit, 1997; Ford et al., 2000), and emotional (Goldsmith & Freyd, 2005; Teicher, Samson, Polcari, & McGreenery, 2006) abuse.
In the somatoform disorder (SoD) literature, affect dysregulation has been referred to as alexithymia (Waller & Scheidt, 2004, 2006). Alexithymia, generally understood as “no words for feelings,” encompasses: (a) difficulty identifying emotions, (b) difficulty describing emotions to others, (c) pensée opératoire, and (d) limited imaginal capacity (e.g., Sifneos, 1973). Alexithymia has also been shown to be associated with a history of childhood abuse (Bermond, Moormann, Albach, & Van Dijke, 2008; Greenberg & Bolger, 2001; Moormann, Bermond, & Albach, 2004; Moormann, Bermond, Albach, & Van Dorp, 1997; Paivio & Laurent, 2001). In addition to involving an inhibition of the cognitive capacity to differentiate and articulate affects, alexithymia also tends to involve a suppression or numbing of affect that may be considered a form of over-regulation of affect. In posttraumatic stress disorder (PTSD; Lanius, Vermetten, et al., 2010; Lanius, Frewen, et al., 2010), complex PTSD (Şar, 2011), and in SoD and BPD (Van Dijke, Ford, et al., 2010), over-regulation of affect may represent a sub-type that is associated with negative symptoms of somatoform and psychoform dissociation (e.g., Van Dijke, Van der Hart et al., 2010).
Affective disruptions including under-regulation and over-regulation of affect are at the heart of disturbances stemming from childhood victimization (Cook et al., 2005; Ford, 2005), especially when this involves a caretaker (Freyd, DePrince, & Gleaves, 2007; Paivio & Laurent, 2001). Adults who have experienced childhood victimization consistently are found to be at risk for problems with under-regulation of affect, but over-regulation of affect also may be a clinically important sequela of childhood interpersonal trauma. For example, Marx and Sloan (2002) found that among survivors of child sexual abuse, over-regulation and under-regulation of affect were significantly related to psychological distress. However, over-regulation (but not under-regulation) mediated the relationship between child sexual abuse status and distress, indicating that over-regulation also may be influential in the development of psychological symptoms in child sexual abuse survivors.
Childhood traumatization is known to be associated with psychiatric disorders such as BPD (Yen et al., 2002; Zanarini, Yonge, & Frankenburg, 2002), SoD (Brown, Schrag, & Trimble, 2005; Teicher et al., 2006), and dissociative disorders (Nijenhuis, Van der Hart, Kruger, & Steele, 2004; Roelofs, Keijsers, Hoogduin, Näring, & Moene, 2002; Şar, Akyuz, Kugu, Ozturk, & Ertem-Vehid, 2006).
Although contemporary researchers consider the causal association between child abuse and psychiatric disorders to be an oversimplification (e.g., Van der Kolk et al., 1996), sexual, physical, and emotional abuse have been hypothesized to be important etiological contributors to BPD (Bradley, Jenei, & Westen, 2005), SoD (Brown et al., 2005), and dissociative disorders (e.g., Roelofs et al., 2002; Şar & Ross, 2006). However, relatively little is known about how child abuse contributes to the etiology of these psychiatric disorders (Verdurmen et al., 2007). One possible factor contributing to the association of child abuse with subsequent BPD and SoD is affect dysregulation. Therefore, the present study investigated the relationship of childhood victimization and both forms of affect dysregulation in adults diagnosed with BPD, SoD, and comorbid BPD and SoD.
Childhood traumatization for which the primary caretaker was the agent has been hypothesized to have special importance in the etiology of severe psychiatric disorders (Allen, 2001). Caretaker-caused traumatic stressors are likely to occur in and contribute to result in a relational growth-inhibiting early environment in which caretakers not only play less with the infant but also evoke stress (in the case of an abusive caretaker) or fail to protect the child from post-traumatic states of enduring negative affect (Fonagy, Gergely, Jurist, & Target, 2002; Lieberman, 2007; Lieberman & Amaya-Jackson, 2005). In addition, the caretaker might provide insufficient protection against other potential abusers of the child (Lieberman, 2007). The caretaker also often is inaccessible and reacts unattuned and/or with rejection to the infants’ expressions of emotions and stress. Therefore, the caretaker shows minimal or unpredictable participation in the various types of arousal regulating processes (Lyons-Ruth, Dutra, Schuder, & Bianchi, 2006). Instead of modulating extreme levels of stimulation and arousal, the infant and caretaker tend to experience high levels of arousal episodically when abuse has occurred and/or low levels of arousal when neglect has occurred. If interactive repair from a caretaker is not available or responsive to the infant, intense negative states can persist and be experienced by the infant as unmanageable. Until these states subside, the infant must devote most or all of their available biological and affective resources to withstand this state of distress and dysregulation (Tronick & Weinberg, 1997). Thus, the combination of the psychobiological challenge posed by traumatic stressors and the absence of consistent and effective co-regulation by a responsive available caretaker might compromise the child's capacity to regulate excessive levels of high and/or low arousal negative affect; and, when this persists in early development, it may result in persistent problems with under- or over-regulation of affect in adulthood.
Although theory and research have emphasized the adverse impact of caretaker-related abuse that occurs in the earliest years of development, abuse or neglect by primary caretakers that occurs later in childhood or adolescence also may have detrimental effects. Prospective (Dodge, Pettit, Bates, & Valente, 1995) and retrospective (Teicher et al., 2006; Zinzow et al., 2009) studies of emotional, physical, and sexual abuse have found evidence of deleterious effects on functioning, mental health, and health in the aftermath of abuse in the school years and adolescence. However, studies that systematically examined the relationship between a history of exposure to traumatic stressors for which a primary caretaker is the agent at differing developmental epochs with psychiatric and psychosocial morbidity were not found. Therefore, in the present study, trauma by a primary caretaker is assessed in each of three developmental epochs, early childhood (ages 0–6 years old), middle childhood (ages 7–12 years old), and adolescence (ages 13–18 years old). We hypothesized that trauma by a primary caretaker would be associated with particularly severe under-regulation of affect in adults diagnosed with BPD and over-regulation of affect in adults diagnosed with SoD. We also hypothesized that these relationships would be strongest when trauma by a primary caretaker occurred during early childhood, compared to middle-childhood or adolescence.
Method
Participants and procedure
Participants were 472 consecutive admissions to two adult treatment centers, Eikenboom Center for Psychosomatic Medicine, Altrecht Utrecht (N=117) and De Waard, Centre for Personality Disorders, Delta Psychiatric Center, Rotterdam (N=355) who participated in the multi-center project “Clinical Assessment of Trauma-Related Self and Affect Dysregulation” (Van Dijke, 2008).
According to the DSM-IV criteria (APA, 2000), diagnoses of BPD and SoD (i.e., somatization disorder, undifferentiated somatoform disorder, severe conversion, and pain disorder) were confirmed by clinical interviewers (general health psychologists and master students in clinical psychology who were trained and supervised by the first author, a certified clinical psychologist/clinical neuropsychologist). The diagnosis of SoD additionally was confirmed by a psychiatrist with somatic experience, a specialist in internal medicine, or a general practitioner with psychiatric experience. Where possible, general practice and former hospital records were obtained (with patient's consent) and studied by the interviewer in addition to using the results of the structured interviews in order to ascertain diagnoses. All participants had a well-documented history of somatic and/or psychiatric symptoms. All had received previous inpatient or outpatient treatment at psychiatric or somatic hospitals and were referred for specialized treatment. Next, self-report measures were administered under supervision of formerly described interviewers.
Table 1 presents the demographic characteristics of the four study groups and the total sample. No significant differences were found between the diagnostic sub-groups in the distribution of genders or levels of education.
Table 1.
Demographic characteristics of the study groups and the total sample
| BPD | SoD | BPD+SoD | PC | Total sample | |
|---|---|---|---|---|---|
| N= | 120 | 159 | 129 | 64 | 472 |
| Male | 40 | 47 | 30 | 28 | 145 |
| Female | 80 | 112 | 99 | 36 | 327 |
| Age M (SD) | 29.9 (8.8) | 38.3 (10.5) | 33.6 (9.1) | 36.8 (9.9) | 34.7 (10.1) |
| Social N | 30.8% | 45.3% | 40.3% | 28.1% | 37.9% |
| T | 60.8 | 41.5 | 47.3 | 56.3 | 50.0 |
| S | 8.3 | 13.2 | 12.4 | 15.6 | 12.1 |
| Educ L | 24.2% | 22.6% | 27.1% | 23.4% | 24.4% |
| M | 35.8 | 45.9 | 37.2 | 46.9 | 41.1 |
| H | 40 | 31.4 | 35.7 | 29.7 | 34.5 |
Note: BPD, borderline personality disorder; SoD, somatoform disorder; BPD+SoD, borderline personality disorder and somatoform disorder; PC, psychiatric comparison group; Social, primary relationship status; N, no primary partner; T, living together; S, separated by death or divorce; Educ, highest level of education attained; L, primary and low-level secondary education; M, middle level secondary education; H, high-level secondary education.
This study was approved by the local ethics committee. After complete description of the study and procedure, participants provided written informed consent to participate according to the Declaration of Helsinki.
Measures
The Composite International Diagnostic Interview, section C (CIDI; World Health Organization, WHO, 1997; Dutch version Ter Smitten, Smeets, & Van den Brink, 1998) is a comprehensive, standardized instrument for assessing mental disorders according to the definitions and diagnostic criteria of DSM-IV and ICD-10. The CIDI has been shown to have good reliability and validity (Andrews & Peters, 1998).
The Borderline Personality Disorder Severity Index (BPDSI; Dutch version IV, Arntz, 1999; Weaver & Clum, 1993) is a semi-structured interview that contains nine sections and 70 items (Abandonment, 7 items; Relationships, 8 items; Self-image, 8 items; Impulsivity, 11 items; Parasuicide, 13 items; Affect, 5 items; Emptiness, 4 items; Anger, 6 items; and Dissociation/Paranoia, 8 items) corresponding to the symptom clusters of BPD. Each section contains items asking about events, for example, “Did you, during the last 3 months, ever become desperate when you thought that someone you cared for was going to leave you?” The items are scored by the interviewer using a 10-point scale, indicating how often the event happened during the last 3 months. An average score was calculated for each section, total scores were calculated by summing the section scores. The BPDSI has been shown to have good validity and reliability (Arntz et al., 2003), for inclusion and categorical analyses a cutoff score of 20 was used.
In order to assess “under-regulation of affect,” each subject completed the Dutch self-report version of the Structured Interview for Disorders of Extreme Stress Not Otherwise Specified, Revised (SIDES-rev; Ford & Kidd, 1998), an adaptation of the interview that provides a subscale for dysregulated affect (Ford & Kidd, 1998; Dutch translation Van Dijke & Van der Hart, 2002). The SIDES-rev was translated into Dutch and retranslated by a near-native speaker (Cronbach's α=.75). The criterion for presence of pathological under-regulation of affect and categorical analyses was adopted from the SIDES scoring manual (Ford & Kidd, 1998; from criterion I.a. “affect dysregulation”: two out of three items rated with severity ≥2). The items include: (1) often getting “quite upset” over daily matters; (2) being unable to get over the upset for hours or not being able to stop thinking about it; and (3) having to “stop everything to calm down and it took all your energy” or “getting drunk, using drugs or harming yourself” to cope with emotional distress. Thus, the measure addresses the core components of under-regulation of affect; that is, frequent/intense distress, inability to modulate or recover from distress, and use of self-defeating coping to deal with distress.
In order to assess “over-regulation of affect,” each subject completed the Bermond Vorst Alexithymia Questionnaire (BVAQ; Vorst & Bermond, 2001), which is a Dutch 40-item questionnaire with good psychometric qualities (Vorst & Bermond, 2001), encapsulating two distinct second-order factor groupings: cognitive dimensions (diminished ability to verbalize, identify, and analyze emotions) and affective dimensions (diminished ability to emotionalize and fantasize). High scores represent stronger alexithymic tendencies. The reliability for the total scale and its subscales is good and varies between .75 and .85 (Vorst & Bermond, 2001). A reliability analysis was performed for the whole sample and the BVAQ proved to be reliable for our purposes (Cronbach's α=.88). The cognitive factor of the BVAQ was used to assess over-regulation in order to enable comparison with previous studies (Waller & Scheidt, 2004, 2006). The cognitive factor of the BVAQ is highly correlated with the Toronto Alexithymia Scale (TAS-20; Bagby, Parker, & Taylor, 1994; r=.80). The cutoff score for pathological alexithymia/over-regulation of affect of the BVAQ cognitive factor is in agreement with the cutoff scores used in TAS-20 studies (Taylor et al., 1997) and were used for categorical analyses.
Reports of potentially traumatic events were collected using the Traumatic Experiences Checklist (TEC; Dutch version, Nijenhuis, Van der Hart, & Kruger, 2002), a retrospective self-report questionnaire concerning adverse experiences and potential traumatic events. Reports of traumatic experiences were confirmed by close relatives in a sub-sample of Delta Psychiatric Center participants, with 100% agreement. Participants stated for each item at what age this first happened. Three specific developmental epochs were considered in the present study (age 0–6 years, age 7–12 years, and age 13–18 years) and only events that directly involved a primary caretaker were used to identify the presence of three types (emotional, physical, and sexual) of potentially traumatizing events caused by a primary caretaker (TPC). For categorical assessment, epochs in which the traumatic event first occurred was used in categorical analyses. The TEC has been shown to have good reliability and validity among psychiatric outpatients (Nijenhuis et al., 2002).
The PTSD was assessed with a sub-sample of patients from the Delta PC study site (N=138) using Self-Rating Inventory for Posttraumatic Stress Disorder (SRIP; Davidson, Smith Kudler, 1989). This inventory has 22 items reflecting the 17 symptoms from DSM-IV. The sequence of the items does not follow DSM-IV but has been randomized. All items are scored on a 4-point rating scale with anchors of 1=not at all and 4=very much, indicating intensities. A total score is calculated by adding all scores. Scores for the subscales of Intrusion, Avoidance, and Hyper-arousal can be calculated by adding the scores on the relevant items. Further, a DSM-IV diagnosis can be calculated by using an algorithm (Hovens, Bramsen, & Van der Ploeg, 2000). This sub-sample did not differ significantly from the total sample on age, gender, and group.
Statistical analysis
All analyses were performed using SPSS, version 16 (SPSS Chicago). Pearson product moment correlations were calculated for the whole sample in order to describe the bivariate relationships among affect dysregulation (under-regulation and over-regulation), TPC-types, and developmental epochs. For categorical analyses, cutoff scores computed as mentioned in the measures section were applied. To compare the likelihood of reporting TPC and under-regulation and over-regulation for each diagnostic cohort (BPD, SoD, BPD+SoD, and psychiatric controls), cross-tabulations with standard residuals were performed. A multivariate analysis of variance (MANOVA) was performed to identify diagnostic group differences on severity scores for TPC and the reporting of TPC in three developmental epochs (0–6, 7–12, and 13–18 years old). Finally, a multivariate analysis of covariance (MANCOVA) was conducted on scores for over-regulation and under-regulation of affect, with diagnostic group as the independent variable and severity of sexual, physical, and sexual TPC and the occurrence of TPC in early childhood (ages 0–6 years old) as covariates, in order to determine if differences between the diagnostic groups in affect regulation (Van Dijke, Ford, et al., 2010) could be accounted for by the severity or epoch of TPC.
Results
Almost two-thirds (63.6%) of participants reported at least one instance of traumatization by a primary caretaker. Table 2 presents the bivariate correlations between the trauma history and under- and over-regulation of affect variables. The relationships generally were not strong, with statistically significant correlations only between physical TPC and over-regulation of affect, and adolescent-epoch caretaker traumatization and emotional TPC and under-regulation of affect. For a sub-sample of the patients meeting DSM-IV-TR criteria for PTSD, analyses were repeated. On a dimensional level, only associations for under-regulation of affect with total SRIP proved significant (r=.41; p<.000), and for over-regulation with total SRIP (r=.27; p<.001) and over-regulation with developmental epoch 0–6 years (r=.17; p<.05). On a categorical level, only the association between over-regulation and total SRIP (r=.31; p<.01) remained significant but disappeared for developmental epoch 0–6 years and for under-regulation of affect with total SRIP.
Table 2.
Correlations between affect dysregulation and TPC for total sample
| N=471 | Over-regulation of affect | Under-regulation of affect |
|---|---|---|
| Developmental epoch 0–6 years | .05 | .11* |
| Developmental epoch 7–12 years | .03 | .02 |
| Developmental epoch 13–18 years | .00 | .08 |
| Sexual TPC | .05 | .02 |
| Emotional TPC | .01 | .14** |
| Physical TPC | .10* | .04 |
Note: p≤.05;
p≤.01.
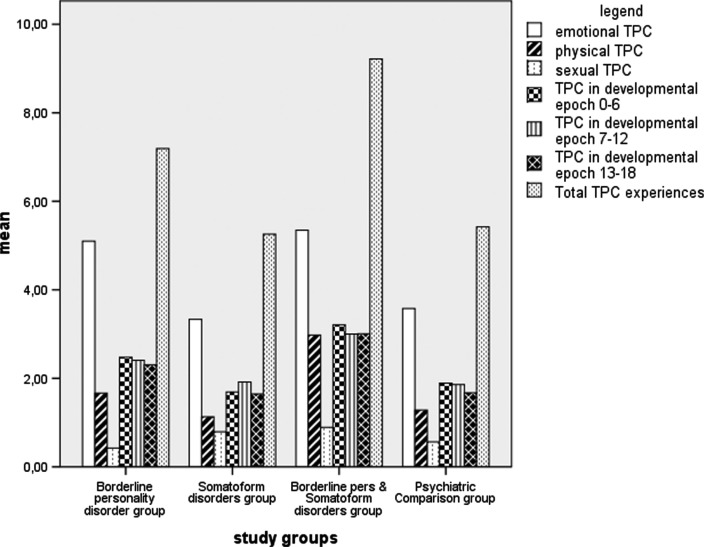
Table 3 presents the results from cross-tabulation analyses of the likelihood of reporting TPC for the BPD, SoD, BPD+SoD, and psychiatric control groups. Approximately 50% of the SoD and psychiatric control participants reported a history of TPC, compared to 70–80% of the BPD and BPD+SoD participants. The BPD+SoD group was significantly more likely than other groups to report TPC and the SoD group was significantly less likely to report TPC (χ2=28.34, df=3, p<.000). Fig. 1 presents the comparison of mean scores for TPC types, developmental epochs, and total TPC experiences for diagnostic study groups.
Table 3.
Presence of trauma-by-primary-caretaker for diagnostic groups
| No traumatic events by primary caretaker | Traumatic events by primary caretaker | Total | ||
|---|---|---|---|---|
| BPD | Frequency | 34 | 85 | 119 |
| % group | 28.6% | 71.4% | 100.0% | |
| Std. residual | −1.4 | 1.1 | ||
| SoD | Frequency | 77 | 81 | 158 |
| % group | 48.7% | 51.3% | 100.0% | |
| Std. residual | 2.6 | –1.9 | ||
| BPD+SoD | Frequency | 29 | 100 | 129 |
| % group | 22.5% | 77.5% | 100.0% | |
| Std. residual | −2.6 | 2.0 | ||
| PC | Frequency | 31 | 33 | 64 |
| % group | 48.4% | 51.6% | 100.0% | |
| Std. residual | 1.6 | –1.2 | ||
| Total | Total | 171 | 229 | 470 |
| % group | 36.4% | 63.6% | 100.0% |
Note: BPD, borderline personality disorder; SoD, somatoform disorder; BPD+SoD, borderline personality disorder and somatoform disorder; PC, psychiatric comparison group; Std. residual, standardized residual values. Cells with values less than –2 or greater than 2 are statistically significant and are identified in bold type. A negative value indicates “less frequent than expected” and a positive value indicates “more frequent than expected.”
Fig. 1.
Comparison of TPC types, developmental epochs, and total TPC experiences for diagnostic study groups.
The MANOVA exploring group differences in the severity of each TPC-type, the developmental epochs at which TPC occurred in childhood, and the two types of affect dysregulation resulted in a statistically significant difference overall: F (24, 1,326)=5.62; p<.000; Wilks’ Lambda=.76; partial eta squared=.09. When the results for the dependent variables were considered separately, between group differences were found for emotional-, physical-, and total TPC experiences, as well as for developmental epoch 0–6 years, developmental epoch 7–12 years, developmental epoch 13–18 years, but not for sexual TPC. All effect sizes were small (see Table 4).
Table 4.
Between group differences for TPC experiences, developmental epochs and affect dysregulation
| F(3, 464) | Partial eta-squared | |
|---|---|---|
| Emotional TPC | 6.79*** | .04 |
| Physical TPC | 8.08*** | .05 |
| Sexual TPC | 1.43 | .01 |
| Total TPC experiences | 7.81*** | .05 |
| Developmental epoch 0–6 | 6.01*** | .04 |
| Developmental epoch 7–12 | 4.57** | .03 |
| Developmental epoch 13–18 | 7.64*** | .05 |
| Under-regulation of affect | 26.1*** | .14 |
| Over-regulation of affect | 5.33*** | .03 |
Note: p≤.01;
p≤.001.
Results of the MANCOVA comparing the four diagnostic groups on the affect regulation scores while controlling for sexual, physical, and emotional TPC severity and early developmental TPC showed a significant overall between group effect: F (6, 920)=13.13; p<.001; Wilks’ Lambda=.85; partial eta squared=.08. Under-regulation levels differed between the diagnostic sub-groups after controlling for the effect of trauma history, with a large effect size: F (3, 461)=24.12; p<.001; partial eta squared=.14. Over-regulation of affect also differed between the diagnostic sub-groups after controlling for the effect of trauma history, although with a smaller effect size: F (3, 461)=4.30; p=.005; partial eta squared=.03.
Table 5 shows the means and SDs of TPC experiences, developmental epochs, and affect dysregulation for the BPD, SoD, BPD+SoD, and psychiatric control groups. Overall, the BPD+SoD group reported the most complex trauma histories, with significant more reports for severe physical-TPC across all three childhood developmental epochs. Both the BPD+SoD and BPD groups reported more emotional TPC, under- and over-regulation of affect than did the SoD and psychiatric control groups.
Table 5.
Means and SD for scores for TPC types, developmental epochs, and affect dysregulation
| Group | Emotional TPC | Physical TPC | Sexual TPC | Epoch 0–6 | Epoch 7–12 | Epoch 13–18 | Total TPC | Over-regulation of affect | Under-regulation of affect | |
|---|---|---|---|---|---|---|---|---|---|---|
| BPD | 5.11 (4.37) | 1.61 (3.23) | .43 (1.61) | 2.45 (2.89) | 2.40 (2.47) | 2.28 (2.39) | 7.19 (7.21) | 77.06 (17.89) | 8.29 (1.84) | |
| SoD | 3.35 (4.22) | 3.80 (.61) | .79 (2.07) | 1.70 (2.89) | 1.93 (2.64) | 1.66 (2.48) | 5.26 (7.18) | 72.77 (17.51) | 6.64 (2.02) | |
| Mean (SD) | ||||||||||
| BPD+SoD | 5.35 (4.43) | 4.05 (.78) | .89 (2.19) | 3.21 (3.42) | 3.00 (2.76) | 3.01 (2.81) | 9.22 (8.26) | 79.26 (17.90) | 8.44 (1.83) | |
| PC | 3.64 (4.40) | 3.67 (.61) | .56 (1.90) | 1.92 (3.36) | 1.89 (2.74) | 1.70 (2.33) | 5.42 (7.63) | 70.70 (19.55) | 7.19 (2.30) |
Note: BPD, borderline personality disorder; SoD, somatoform disorder; BPD+SoD, borderline personality disorder and somatoform disorder; PC, psychiatric comparison group; SD, standard deviation.
Discussion
The findings are consistent with recent neuro-imaging results (Lanius, Vermetten, et al., 2010; Lanius, Frewen, et al., 2010) and recent proposals for DSM V (Şar, 2011) that suggest that there may be an over-regulated sub-type of PTSD associated with negative dissociative symptoms. The BPD and SoD may be among the numerous final common pathways that occur when affect regulation is compromised as a result of early life interpersonal traumatization and disruption in (or unavailability of) caregiving relationships. Although the relationship of childhood sexual abuse to dissociative symptoms has been investigated in a small sample of adults with psychotic disorders (Offen, Waller, & Thomas, 2003), this is the first study to our knowledge that examined the potential differential relationship of several forms of trauma by a caretaker (TPC) within distinct epochs of childhood with affect dysregulation in a large sample of adults with well-defined severe psychiatric illnesses. Almost two-thirds of participants reported having experienced childhood TPC, ranging from approximately 50% of patients with SoD or other psychiatric disorders to more than 75% of patients with comorbid BPD+SoD. Consistent with our hypotheses, under-regulation of affect was associated with emotional TPC and TPC occurring in developmental epoch 0–6, particularly among adults with BPD. Over-regulation of affect was associated with physical TPC, although this was not limited to participants diagnosed with SoD but also included those diagnosed with BPD. Thus study findings suggest that childhood trauma by primary caretaker is prevalent among psychiatric patients, particularly those with BPD, and differentially associated with under- and over-regulation of affect depending on the type of traumatic exposure.
For a sub-sample of patients with comorbid PTSD, interestingly no significant associations between affect dysregulation and developmental epochs or TPC were found, and over-regulation of affect (and not under-regulation) remained significantly related to PTSD severity across developmental epochs. In line with previous calls for the assessment of the nature of affect dysregulation and differentiating between inhibitory and excitatory regulation in BPD and SoD patients (Van Dijke, Ford, et al., 2010; Van Dijke, Van der Hart, et al., 2010), also for PTSD patients, difficulty with addressing and analyzing emotions or “mentalising emotions” (Fonagy et al., 2002) and inhibitory regulation seem to have been overlooked and may be of particular importance in the assessment and treatment of complex TPC-related pathology such as comorbid BPD+SoD or complex PTSD (Ford, 2005). These findings are consistent with recent neuroimaging results that suggested that there may be a dissociative (over-regulated) sub-type of PTSD (Lanius et al., 2010).
The presence of a BPD diagnosis was more consistently associated with a history of emotional TPC and with both under- and over-regulation of affect than the presence of a SoD diagnosis. This finding is in accordance with previous findings that child abuse and neglect are associated with BPD (Yen et al., 2002; Zanarini et al., 2002) and affect dysregulation (Ford, 2005). However, whereas prior studies have emphasized the role of TPC in early childhood as a contributor to BPD and affect dysregulation, in this study BPD was associated with TPC that occurred in each of the three childhood developmental epochs. This suggests that early life attachment-trauma might have adverse effects on affect regulation and interpersonal functioning as a result of cumulative (re)traumatization (Follette & Vijay, 2008) as well as (or instead of) due to its neurobiological and psychological effects on early childhood development per se. The findings also suggest that factors other than childhood traumatization by a primary caretaker are likely to account for subsequent affect dysregulation, particularly under-regulation of affect. This is consistent with prior evidence that BPD is not primarily a disorder related to childhood traumatic victimization (Golier et al., 2003), although the present study's results do not rule out a potential role for childhood traumatization by other adults in the under-regulation of affect characterizing BPD or in the weaker but still evident association between BPD and over-regulation of affect.
The finding that the comorbid diagnosis of BPD+SoD—even more so than BPD alone—was particularly associated with the severity of physical TPC and over-regulation of affect, suggest that there may be more extensive sequelae associated with violations of bodily integrity (which may include but does not specifically involve sexual violations) than are accounted for by the BPD diagnosis alone. This is consistent with a complex post-traumatic stress disorder (CPTSD) formulation (Ford, 2008) in which early childhood developmentally adverse interpersonal trauma (Ford, 2005) is associated with affect dysregulation and somatic dysregulation (as well as dissociation and significant changes in core beliefs).
The finding that emotional TPC was most consistently associated with BPD and with under-regulation of affect is consistent with the findings of Teicher and colleagues (2006) that emotional abuse was a more robust predictor of biological and psychological dysregulation than was physical or sexual abuse. Emotional abuse can often occur with physical or sexual abuse, especially in poly-victimized children (Finkelhor, Ormrod, & Turner, 2007), and warrants attention as a less obvious but potentially pernicious source of affect dysregulation and personality pathology.
Future directions
Study findings are consistent with prior calls for more systematic differentiation between under-regulation and over-regulation of affect (Van Dijke, 2008 , Van Dijke et al., in press) in the study of the traumatic antecedents of affect dysregulation (Herman, 1992; McLean et al., 2006; Pelcovitz, Van der Kolk, Roth, Mandel, & Resick, 1997; Roth, Newman, Pelcovitz, Van der Kolk, & Mandel, 1997; Van der Kolk et al., 1996). The interrelationships between under-regulation or over-regulation of affect, different types and developmental epochs of exposure to psychological trauma and associated disruptions in attachment, and the range of psychiatric disorders remain to be explored. It would be interesting to assess reported attachment-trauma and over-regulation of affect relative to the revised CPTSD/DESNOS symptom set identified in a recent factor analytic study (Ford, 2009), because the differential roles of violations of bodily integrity relative to over-regulation of affect and wounding of one's feelings or lack of appreciation of the self/identity relative to under-regulation of affect might be distinguished for patients with the CPTSD/DESNOS symptom set.
Limitations
This study explored the potential role of childhood traumatization caused by a primary caretaker occurring during discrete developmental epochs in the development of affect dysregulation. Data were obtained from a psychiatric population consisting of clinically admitted psychiatric patients with persistent psychopathology. Retrospectively self-reported types and times of exposure to psychological trauma may be inaccurate under these circumstances due to the potential influence of current PTSD symptom severity on trauma history reporting (Sutherland & Bryant, 2008) or may be hampered due to psychological defense against remembering early childhood TPC and holding on to a “belief in a just world” (Herman, 1992). Nevertheless, efforts were made (with patient consent) to confirm the reported traumatic events with close relatives following procedures described in the “Clinical Assessment of Trauma-Related Self and Affect Dysregulation” (Van Dijke, 2008). Overall, the clinical observations is that participants who did report early TPC experiences found it difficult to do so; therefore, there might have been more under-reporting than over-reporting of these events due to the emotions that were evoked and the difficulty in handling these emotions and cognitions. Psychopathology does not necessarily equate with inaccuracy of trauma memory reporting. For instance, while showing evidence of “enhanced cognitive schemata” that may bias recall, schizophrenic patients were found to reliably report sexual trauma history over a 1-year period (Klewchuk, McCusker, Mulholland, & Shannon, 2007). The finding that sexual abuse was infrequently reported also may have reduced the study's ability to detect relationships with this type of TPC. Infrequent reports of sexual abuse may also be related to the fact that participants were diagnosed with comorbid PTSD (not primarily diagnosed with PTSD). This may perhaps constrain the generalizability of the findings for PTSD-only populations.
Conclusion
This study assessed the relationship between self-reported childhood traumatization caused by a primary caretaker for specific childhood developmental epochs and affect dysregulation in BPD, SoD, BPD+SoD, and psychiatric control patients. When considering our sample population as a whole, under-regulation of affect was significantly related to emotional TPC and the 0–6 year old developmental epoch, while over-regulation of affect was related to physical TPC. However, the relationships were relatively weak, suggesting that heterogeneity within the samples may have diluted the findings. When diagnostic groups were examined separately, BPD was associated with emotional TPC across all developmental epochs of childhood and emotional TPC was associated with under-regulation of affect. The BPD+SoD group was the most likely to report early TPC and both forms of affect dysregulation. Thus, our findings indicate the importance of examining the role of emotional abuse in severe psychiatric disorders, and the combination of affect under-regulation and over-regulation associated with early TPC especially in more complex disorders such as the combination of BPD and SoD.
For the abstract or full text in other languages, please see Supplementary files under Reading Tools online
Conflict of interest and funding
There is no conflict of interest in the present study any of the authors.
References
- APA. Diagnostic and statistical manual of mental disorders: DSM-IV-TR. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- Allen J. G. Traumatic relationships and serious mental disorders. London: John Wiley & Sons; 2001. [Google Scholar]
- Andrews G., Peters L. The psychometric properties of the Composite International Diagnostic Interview. Social Psychiatry and Psychiatric Epidemiology. 1998;33:80–88. doi: 10.1007/s001270050026. [DOI] [PubMed] [Google Scholar]
- Arntz A. BPDSI Borderline Personality Disorder Severity Index. The Netherlands: Department of Medical, Clinical and Experimental Psychology, Maastricht University; 1999. Dutch version IV. [Google Scholar]
- Arntz A., Van der Hoorn M., Cornelis J., Verheul R., Van den Bosch W., De Bie A. Reliability and validity of the borderline personality disorder severity index. Journal Personality Disorders. 2003;17:45–49. doi: 10.1521/pedi.17.1.45.24053. [DOI] [PubMed] [Google Scholar]
- Bagby R. M., Parker J. D. A., Taylor G. J. The Twenty-Item Toronto Alexithymia Scale—I. Item selection and cross-validation of the factor structure. Journal of Psychosomatic Research. 1994;38:23–32. doi: 10.1016/0022-3999(94)90005-1. [DOI] [PubMed] [Google Scholar]
- Bermond B., Moormann P. P., Albach F., Van Dijke A. Impact of severe childhood sexual abuse on the development of alexithymia in adulthood. Psychotherapy and Psychosomatics. 2008;77:260–262. doi: 10.1159/000128167. [DOI] [PubMed] [Google Scholar]
- Bradley R., Jenei J., Westen D. Etiology of personality disorder: Disentangling the contributors of intercorrelated antecedents. Journal of Nervous and Mental Diseases. 2005;193:24–31. doi: 10.1097/01.nmd.0000149215.88020.7c. [DOI] [PubMed] [Google Scholar]
- Brown R. J., Schrag A., Trimble M. R. Dissociation, childhood interpersonal trauma, and family functioning in patients with somatization disorder. American Journal of Psychiatry. 2005;162:899–905. doi: 10.1176/appi.ajp.162.5.899. [DOI] [PubMed] [Google Scholar]
- Carey P. D., Walker J. L., Rossouw W., Seedat S., Stein D. J. Risk indicators and psychopathology in traumatised children and adolescents with a history of sexual abuse. European Child & Adolescent Psychiatry. 2008;17(2):93–98. doi: 10.1007/s00787-007-0641-0. [DOI] [PubMed] [Google Scholar]
- Cook A., Spinazzola J., Ford J., Lanktree C., Blaustein M., Cloitre M., et al. Complex trauma in children and adolescents. Psychiatric Annals. 2005;35:390–398. [Google Scholar]
- Dodge K. A., Lochman J. E., Harnish J. D., Bates J. E., Pettit G. S. Reactive and proactive aggression in school children and psychiatrically impaired chronically assaultive youth. Journal of Abnormal Psychology. 1997;106(1):37–51. doi: 10.1037//0021-843x.106.1.37. [DOI] [PubMed] [Google Scholar]
- Dodge K. A., Pettit G. S., Bates J. E., Valente E. Social information-processing patterns partially mediate the effect of early physical abuse on later conduct problems. Journal of Abnormal Psychology. 1995;104(4):632–643. doi: 10.1037//0021-843x.104.4.632. [DOI] [PubMed] [Google Scholar]
- Finkelhor D., Ormrod R., Turner H. Poly-victimization: A neglected component in child victimization. Child Abuse and Neglect. 2007;31:7–26. doi: 10.1016/j.chiabu.2006.06.008. [DOI] [PubMed] [Google Scholar]
- Follette V., Vijay A. Retraumatization. In: Reyes G., Elhai J. D., Ford J. D., editors. Encyclopedia of psychological trauma. Hoboken, NJ: John Wiley & Sons; 2008. pp. 586–589. [Google Scholar]
- Fonagy P., Gergely G., Jurist E., Target M. Affect regulation, mentalization and the development of the self. New York: Other Press; 2002. [Google Scholar]
- Ford J. D. Treatment implications of altered neurobiology, affect regulation and information processing following child abuse. Psychiatric Annals. 2005;35:410–419. [Google Scholar]
- Ford J. D. Complex posttraumatic stress disorder. In: Reyes G., Elhai J. D., Ford J. D., editors. Encyclopedia of psychological trauma. Hoboken, NJ: John Wiley & Sons; 2008. pp. 152–154. [Google Scholar]
- Ford J. D. Dissociation in complex posttraumatic stress disorder or disorders of extreme stress not otherwise specified (DESNOS) In: Dell P. F., J. A. O'Neil, editors. Dissociation and the dissociative disorders: DSM-V and beyond. New York: Routledge; 2009. pp. 471–485. [Google Scholar]
- Ford J. D., Kidd P. Early childhood trauma and disorders of extreme stress as predictors of treatment outcome with chronic posttraumatic stress disorder. Journal of Traumatic Stress. 1998;11:743–761. doi: 10.1023/A:1024497400891. [DOI] [PubMed] [Google Scholar]
- Ford J. D., Racusin R., Ellis C. G., Daviss W. B., Reiser J., Fleischer A., et al. Child maltreatment, other trauma exposure, and posttraumatic symptomatology among children with oppositional defiant and attention deficit hyperactivity disorders. Child Maltreatment. 2000;5:205–217. doi: 10.1177/1077559500005003001. [DOI] [PubMed] [Google Scholar]
- Freyd J. J., DePrince A. P., Gleaves D. H. The state of betrayal trauma theory. Memory. 2007;15:295–311. [Google Scholar]
- Goldsmith R. E., Freyd J. J. Awareness for emotional abuse. Journal of Emotional Abuse. 2005;5:95–123. [Google Scholar]
- Golier J. A., Yehuda R., Bierer L. M., Mitropoulou V., New A. S., Schmeidler J., et al. The relationship of borderline personality disorder to posttraumatic stress disorder and traumatic events. American Journal of Psychiatry. 2003;160:2018–2024. doi: 10.1176/appi.ajp.160.11.2018. [DOI] [PubMed] [Google Scholar]
- Greenberg L., Bolger L. An emotion-focused approach to the over-regulation of emotion and emotional pain. Journal of Clinical Psychology. 2001;57:197–211. doi: 10.1002/1097-4679(200102)57:2<197::aid-jclp6>3.0.co;2-o. [DOI] [PubMed] [Google Scholar]
- Herman J. Complex PTSD. Journal of Traumatic Stress. 1992;5:377–391. [Google Scholar]
- Hovens J. E., Bramsen I., Van der Ploeg H. M. Zelfinventarisatielijst Posttraumatische Stressstoornis (ZIL): Handleiding [Self-Rating Inventory for PTSD: Manual] Lisse, the Netherlands: Swets & Zeitlinger; 2000. [Google Scholar]
- Hovens J. E., Van der Ploeg H. M., Bramsen I., Klaarenbeek M. T. A., Schreuder J. N., Rivero V. V. The development of the self-rating inventory for posttraumatic stress disorder. Acta Psychiatrica Scandinavica. 1994;90:172–183. doi: 10.1111/j.1600-0447.1994.tb01574.x. [DOI] [PubMed] [Google Scholar]
- Klewchuk E. M., McCusker C. G., Mulholland C., Shannon C. Cognitive biases for trauma stimuli in people with schizophrenia. British Journal of Clinical Psychology. 2007;46:333–345. doi: 10.1348/014466507X173385. [DOI] [PubMed] [Google Scholar]
- Koenigsberg H. W., Harvey P. D., Mitropoulou V., Schmeidler J., New A. S., Goodman M., et al. Characterizing affective instability in borderline personality disorder. American Journal of Psychiatry. 2002;159:784–788. doi: 10.1176/appi.ajp.159.5.784. [DOI] [PubMed] [Google Scholar]
- Lanius R. A., Frewen P. A., Vermetten E., Yehuda R., et al. Fear conditioning and early life vulnerabilities: two distinct pathways of emotional dysregulation and brain dysfunction in PTSD. European Journal of Psychotraumatology. 2010;1(5467) doi: 10.3402/ejpt.v1i0.5467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lanius R. A., Vermetten E., Loewenstein R. J., Brand B., Schmalhl C., Bremner J. D., et al. American Journal of Psychiatry. 2010;167:640–647. doi: 10.1176/appi.ajp.2009.09081168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lieberman A. F. Ghosts and angels: Intergenerational patterns in the transmission and treatment of the traumatic sequelae of domestic violence. Infant Mental Health Journal. 2007;28:422–439. doi: 10.1002/imhj.20145. [DOI] [PubMed] [Google Scholar]
- Lieberman A. F., Amaya-Jackson L. Reciprocal influences of attachment and trauma: Using a dual lens in the assessment and treatment of infants, toddlers, and preschoolers. In: Berlin L. J., Ziv Y., Amaya-Jackson L., Greenberg M. T., editors. Enhancing early attachments: Theory, research, intervention, and policy. New York: Guilford Press; 2005. pp. 100–124. [Google Scholar]
- Lyons-Ruth K., Dutra L., Schuder M., Bianchi I. From infant attachment disorganization to adult dissociation: Relational adaptations or traumatic experiences? Psychiatric Clinics of North America. 2006;29:63–86. doi: 10.1016/j.psc.2005.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marx B., Sloan D. The role of emotion in the psychological functioning of adult survivors of childhood sexual abuse. Behaviour Therapy. 2002;33:563–577. [Google Scholar]
- McLean L. M., Toner B., Jackson J., Desrocher M., Stuckless N. The relationship between childhood sexual abuse, complex traumatic stress disorder and alexithymia in two outpatient samples: Examination of women treated in community and institutional clinics. Journal of Child Sexual Abuse. 2006;15(3):1–17. doi: 10.1300/J070v15n03_01. [DOI] [PubMed] [Google Scholar]
- Moormann P. P., Bermond B., Albach F. The reality escape model: The intricate relation between alexithymia, dissociation, and anaesthesia in victims of child sexual abuse. In: Nyklicek I., Vingerhoets A., Temoshok L., editors. Emotional expression and health. Advances in theory, assessment, and clinical applications. Hove, UK: Brunner Routledge; 2004. pp. 82–89. [Google Scholar]
- Moormann P. P., Bermond B., Albach F., Van Dorp I. The aetiology of alexithymia from the perspective of childhood sexual abuse. In: Vingerhoets A., van Bussel F., Boelhouwer A, editors. The non-expression of emotions in health and disease. Tilburg, The Netherlands: Tilburg University Press; 1997. pp. 139–153. [Google Scholar]
- Nijenhuis E. R. S., Van der Hart O., Kruger K. The psychometric characteristics of the Traumatic Experiences Checklist (TEC): First findings among psychiatric outpatients. Clinical Psychology and Psychotherapy. 2002;9:200–210. [Google Scholar]
- Nijenhuis E. R. S., Van der Hart O., Kruger K., Steele K. Somatoform dissociation, reported abuse and animal defence-like reactions. Australian and New Zealand Journal of Psychiatry. 2004;38:678–686. doi: 10.1080/j.1440-1614.2004.01441.x. [DOI] [PubMed] [Google Scholar]
- Offen L., Waller G., Thomas G. Is reported childhood sexual abuse associated with the psychopathological characteristics of patients who experience auditory hallucinations? Child Abuse and Neglect. 2003;27:919–927. doi: 10.1016/s0145-2134(03)00139-x. [DOI] [PubMed] [Google Scholar]
- Paivio S. C., Laurent C. Empathy and emotion regulation: Reprocessing memories of childhood abuse. Journal of Clinical Psychology. 2001;57:213–226. doi: 10.1002/1097-4679(200102)57:2<213::aid-jclp7>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- Pelcovitz D., Van der Kolk B., Roth S., Mandel F., Resick P. Development of a criteria set and a Structured Interview for Disorders of Extreme Stress (SIDES) Journal of Traumatic Stress. 1997;10:3–16. doi: 10.1023/a:1024800212070. [DOI] [PubMed] [Google Scholar]
- Putnam F. W. Ten-year research update review: Child sexual abuse. Journal of American Academic Child and Adolescent Psychiatry. 2003;42:269–278. doi: 10.1097/00004583-200303000-00006. [DOI] [PubMed] [Google Scholar]
- Roelofs K., Keijsers G. P. J., Hoogduin K. A. L., Näring G. W. B., Moene F. C. Childhood abuse in patients with conversion disorder. American Journal of Psychiatry. 2002;159:1908–1913. doi: 10.1176/appi.ajp.159.11.1908. [DOI] [PubMed] [Google Scholar]
- Roth S., Newman E., Pelcovitz D., Van der Kolk B., Mandel F. S. Complex PTSD in victims exposed to sexual and physical abuse: Results from the DSM-IV field trial for Posttraumatic Stress Disorder. Journal of Traumatic Stress. 1997;10:539–555. doi: 10.1023/a:1024837617768. [DOI] [PubMed] [Google Scholar]
- Şar V. Developmental trauma, complex PTSD, and the current proposal of DSM-5. European Journal of Psychotraumatology. 2011;2(5622) doi: 10.3402/ejpt.v2i0.5622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Şar V., Akyuz G., Kugu N., Ozturk E., Ertem-Vehid H. Axis-I dissociative disorder comorbidity in borderline personality disorder and reports of childhood trauma. Journal of Clinical Psychiatry. 2006;67:1583–1590. doi: 10.4088/jcp.v67n1014. [DOI] [PubMed] [Google Scholar]
- Sar V., Ross C. A. Dissociative disorders as a confounding factor in psychiatric research. Psychiatric Clinics of North America. 2006;29:129–144. doi: 10.1016/j.psc.2005.10.008. [DOI] [PubMed] [Google Scholar]
- Sutherland K., Bryant R. A. Autobiographical memory and the self-memory system in posttraumatic stress disorder. Journal of Anxiety Disorders. 2008;22:555–560. doi: 10.1016/j.janxdis.2007.03.008. [DOI] [PubMed] [Google Scholar]
- Taylor G. K., Bagby R. M., Parker J. D. A. Disorders of affect regulation: Alexithymia in medical and psychiatric illness. Cambridge: Cambridge University Press; 1997. [Google Scholar]
- Teicher M., Samson J., Polcari A., McGreenery C. Sticks, stones, and hurtful words: Relative effects of various forms of childhood abuse. American Journal of Psychiatry. 2006;163:993–1000. doi: 10.1176/ajp.2006.163.6.993. [DOI] [PubMed] [Google Scholar]
- Ter Smitten M. H., Smeets R. M. W., Van den Brink W. Composite International Diagnostic Interview (CIDI), version 2.1, 12 months [in Dutch] Amsterdam: World Health Organization; 1998. [Google Scholar]
- Tronick E., Weinberg K. Depressed mothers and infants: The failure to form dyadic states of consciousness. In: Murray L., Coopers P., editors. Postpartum depression and child development. New York: Guilford; 1997. pp. 54–85. [Google Scholar]
- Van der Kolk B. A., Pelcovitz M. D., Roth S., Mandel F. S., McFarlane A., Herman J. L. Dissociation, somatization, and affect dysregulation: The complexity of adaptation to trauma. American Journal of Psychiatry. 1996;153:83–93. doi: 10.1176/ajp.153.7.83. [DOI] [PubMed] [Google Scholar]
- Van Dijke A. The clinical assessment and treatment of trauma-related self- and affect dysregulation. In: Vingerhoets A., Nyklicek I., Denollet J., editors. Emotion regulation: Conceptual and clinical issues. New York: Springer; 2008. pp. 150–169. [Google Scholar]
- Van Dijke A., Ford J. D., Van der Hart O., Van Son M. J. M., Van der Heijden P. G. M., Buhring M. Affect dysregulation in borderline personality disorder and somatoform disorder: Differentiating under- and over-regulation. Journal of Personality Disorders. 2010;24:296–311. doi: 10.1521/pedi.2010.24.3.296. [DOI] [PubMed] [Google Scholar]
- Van Dijke A., Van der Hart O. The Dutch self report version of the Structured Interview for Disorders of Extreme Stress (SIDES-r-nl) Utrecht: Utrecht University; 2002. Unpublished manual. [Google Scholar]
- Van Dijke A., Van der hart O., Ford J. D., Van Son M., Van der Heijden P., Buhring M. Affect dysregulation and dissociation in borderline personality disorder and somatoform disorder: Differentiating inhibitory and excitatory experiencing states. Journal of Trauma and Dissociation. 2010;11:424–443. doi: 10.1080/15299732.2010.496140. [DOI] [PubMed] [Google Scholar]
- Verdurmen J., Ten Have M., De Graaf R., Van Dorsselaer S., Van 't Land H., Vollebergh. W. Utrecht: Nationale Monitor Geestelijke Gezondheid (NMG); 2007. Psychological aftermath of child abuse in adulthood. Results from the “Netherlands Mental Health Survey and Incidence Study” (NEMESIS) [Psychische gevolgen van kindermishandeling op volwassen leeftijd] [Google Scholar]
- Vorst H. C. M., Bermond B. Validity and reliability of the Bermond-Vorst Alexithymia Questionnaire. Personality and Individual Differences. 2001;30:413–434. [Google Scholar]
- Waller E., Scheidt C. E. Somatoform disorders as disorders of affect regulation: A study comparing the TAS-20 with non-self-report measures of alexithymia. Journal of Psychosomatic Research. 2004;57:239–247. doi: 10.1016/S0022-3999(03)00613-5. [DOI] [PubMed] [Google Scholar]
- Waller E., Scheidt C. E. Somatoform disorders as disorders of affect regulation: A development perspective. International Review of Psychiatry. 2006;18:13–24. doi: 10.1080/09540260500466774. [DOI] [PubMed] [Google Scholar]
- Weaver T. L., Clum G. A. Early family environments and traumatic experiences associated with borderline personality disorder. Journal of Consulting and Clinical Psychology. 1993;61:1068–1075. doi: 10.1037//0022-006x.61.6.1068. [DOI] [PubMed] [Google Scholar]
- WHO. Composite International Diagnostic Interview. Geneva: Mental Health Division; 1997. [Google Scholar]
- Yen S., Shea M. T., Battle C. L., Johnson D. M., Zlotnick C., Dolan-Sewell R., et al. Traumatic exposure and posttraumatic stress disorder in borderline, schizotypal, avoidant, and obsessive-compulsive personality disorders: Findings from the Collaborative Longitudinal Personality Disorders Study. Journal of Nervous and Mental Diseases. 2002;190:510–518. doi: 10.1097/00005053-200208000-00003. [DOI] [PubMed] [Google Scholar]
- Zanarini M., Yonge L., Frankenburg F. Severity of reported childhood sexual abuse and its relationship to severity of borderline psychopathology and psychosocial impairment among borderline inpatients. Journal of Nervous and Mental Diseases. 2002;190:381–387. doi: 10.1097/00005053-200206000-00006. [DOI] [PubMed] [Google Scholar]
- Zinzow H. M., Ruggiero K. J., Resnick H., Smith D., Saunders B., Kilpatrick D. Prevalence and mental health correlates of witnessed parental and community violence in a national sample of adolescents. Journal of Child Psychology and Psychiatry. 2009;50:441–450. doi: 10.1111/j.1469-7610.2008.02004.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zittel Conklin C., Westen D. Borderline personality disorder in clinical practice. American Journal of Psychiatry. 2005;162:867–875. doi: 10.1176/appi.ajp.162.5.867. [DOI] [PubMed] [Google Scholar]
- Zittel Conklin C., Bradley R., Westen D. Affect regulation in borderline personality disorder. Journal of Nervous and Mental Disease. 2006;194:69–77. doi: 10.1097/01.nmd.0000198138.41709.4f. [DOI] [PubMed] [Google Scholar]