Abstract
Background
Building on previous research with disaster-exposed children and adolescents, a randomised clinical trial was performed in the treatment of trauma-related symptoms. In the current study two active treatments were compared among children in a broad age range and from a wide diversity of ethnic populations.
Objective
The primary aim was to compare the effectiveness and efficiency of Cognitive Behavioural Therapy (CBT) and Eye Movement Desensitisation and Reprocessing (EMDR).
Design
Children (n=52, aged 4–18) were randomly allocated to either CBT (n=26) or EMDR (n=26) in a disaster mental health after-care setting after an explosion of a fireworks factory. All children received up to four individual treatment sessions over a 4–8 week period along with up to four sessions of parent guidance. Blind assessment took place pre- and post-treatment and at 3 months follow-up on a variety of parent-rated and self-report measures of post-traumatic stress disorder symptomatology, depression, anxiety, and behaviour problems. Analyses of variance (general linear model repeated measures) were conducted on the intention-to-treat sample and the completers.
Results
Both treatment approaches produced significant reductions on all measures and results were maintained at follow-up. Treatment gains of EMDR were reached in fewer sessions.
Conclusion
Standardised CBT and EMDR interventions can significantly improve functioning of disaster-exposed children.
Keywords: Randomised controlled trial, eye movement desensitisation and reprocessing (EMDR), cognitive behavioural therapy (CBT), post-traumatic stress disorder (PTSD), disaster
Disaster-exposed children often experience symptoms of post-traumatic stress-disorder (PTSD), depression, anxiety, and behavioural problems, which may persist for years thereby potentially disrupting biological, psychological, and social development (Goenjian et al., 2001, 2005; La Greca, 2008; Yule et al., 2000). Despite the enormous public health significance of this problem and the value of making effective intervention available (Cohen et al., 2006), very few randomised controlled studies on treatment of disaster-exposed children have been reported.
Chemtob, Nakashima, and Hamada (2002) provided 248 hurricane-exposed elementary school children a series of four individual or group sessions of psycho-education and graded exposure. Compared to the waiting list control group, treated participants reported significant reductions in trauma symptoms that were maintained at 1-year follow-up. Thirty-two participants who still met criteria for PTSD were later randomised to three sessions of eye movement desensitisation and reprocessing (EMDR) or to a waiting list control group. Compared to the control group, those receiving EMDR showed significant reductions of PTSD symptoms, anxiety, and depression with improvements maintained at 6-month follow-up (Chemtob, Nakashima, & Carlson, 2002). Four months after Hurricane Katrina in 2005, 56 children (7–12 years old) with moderate to severe levels of post-traumatic stress symptoms were randomly assigned to 10 sessions of group or individual trauma/grief-focused treatment combining cognitive-behavioural and narrative strategies plus one parent meeting (Salloum & Overstreet, 2008). Participants in both conditions showed significant post-treatment decreases in symptoms of post-traumatic stress, depression, traumatic grief, and distress. In another study after Hurricane Katrina, 118 children (9–15 years old) were randomly allocated to individual Trauma-Focused Cognitive Behavioural Therapy (TF-CBT; 12 sessions) at a mental health clinic and a group CBT intervention (10 group sessions and 1–3 individual sessions) at school (Jaycox et al., 2010). Both interventions led to significant symptom reduction of PTSD symptoms, but many still had elevated PTSD symptoms at post-treatment. Finally, 31 children (8–14 years old) with a preliminary diagnosis of PTSD subsequent to war and the tsunami in north-eastern Sri Lanka were randomly assigned to six sessions of either narrative exposure therapy for children (KIDNET) or meditation–relaxation (Med-Relax; Catani et al., 2009). At 6-months follow-up, recovery rates were 81% for the children in the KIDNET group and 71% for those in the Med-Relax group (not significantly different).
The most common treatments for child PTSD are CBT and EMDR with a greater research base for CBT and related approaches (Adler-Nevo & Manassis, 2005; La Greca, 2008; Stallard, 2006). Although both treatments have been proven to be efficacious in children and adolescents with post-traumatic stress reactions, only one direct comparison has been published. Jaberghaderi, Greenwald, Rubin, Zand, and Dolatabadi (2004) randomised 14 sexually abused Iranian girls (ages 12–13) to EMDR or CBT. Participants in both groups showed significant post-treatment reductions in post-traumatic stress symptoms. The EMDR group used fewer sessions. However, this study had many limitations including a small sample size, a single therapist for each treatment condition, and no verification of treatment fidelity.
A large fireworks factory exploded in Enschede, the Netherlands on May 13, 2000 killing 22 people, injuring many, destroying more than 500 houses, and damaging 1,500 more. In total about 10,000 people were affected, of which the number of children and adolescents is unknown. One-third of the affected area's inhabitants were first- and second-generation immigrants mostly of Turkish origin (Committee Oosting 2001). The primary aim of the present study was to compare the effectiveness of an exposure-based cognitive behavioural treatment (CBT, “opvangprotocol”)—the most widely used treatment for pediatric PTSD in the Netherlands—and EMDR among disaster-exposed children. The second aim of the present study was to compare the efficiency of both treatments, because a treatment's efficiency has direct consequences for health resource utilisation and costs and may also affect client retention and satisfaction.
Method
Participants
This field study was initiated 6 months after the fireworks factory exploded and ran from 2001 to 2004 at the disaster mental health after-care centre Mediant in Enschede, the Netherlands. Inclusion criteria were: (1) aged between 4 and 18 years, (2) having firework disaster-related symptoms, and (3) willingness to participate voluntarily. Exclusion criteria were: (1) problems were not disaster-related, (2) severe psychiatric conditions occurred requiring an emergency response (suicidal intent, psychosis), or (3) he/she was already receiving psychotherapy elsewhere. Use of such broad inclusion criteria is common in field studies and is deemed to strengthen their ecological validity.
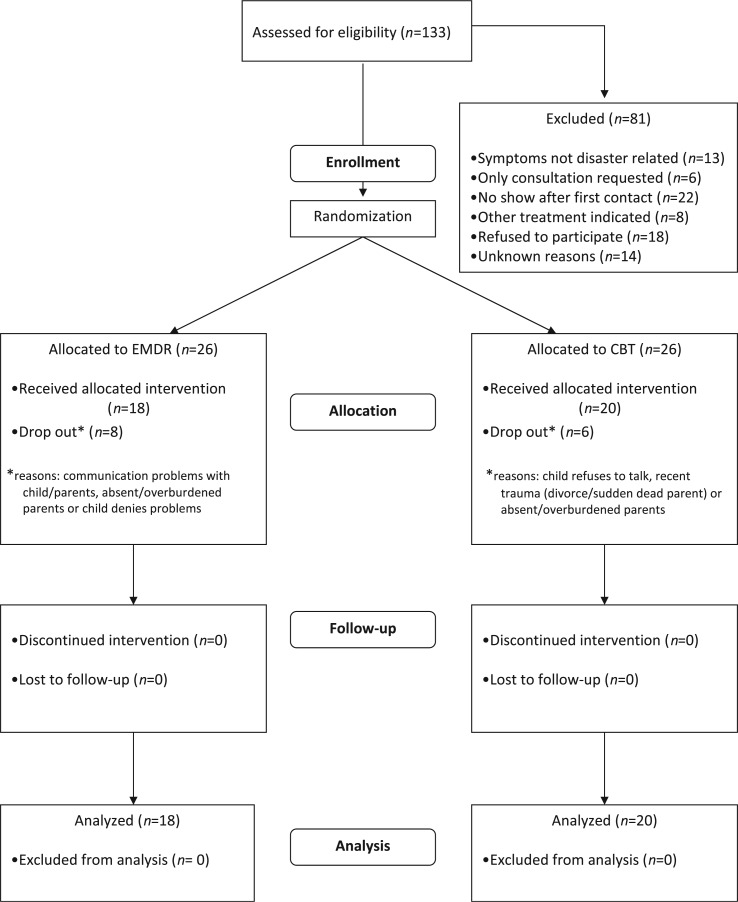
Recruitment occurred as a routine procedure when parents approached Mediant for help with their children. Of the 133 children and adolescents assessed for eligibility, 13 (9.8%) reported symptoms that were not disaster-related, 6 (4.5%) only requested consultation (the parents), 22 (16.5%) did not show up after the first contact, 18 (13.5%) refused participation to the study, 14 (10.5%) were excluded for an unknown reason, and 8 (6%) because another treatment was indicated. The 52 survivors were randomly allocated to EMDR (n=26) and CBT (n=26). The trial profile is shown in Fig. 1.
Fig. 1.
Flow of participants through the study.
Procedure
The protocol and informed consent form had been approved by the local ethics committee. Children were first screened by a senior psychologist who conducted the initial interview meant for gathering of information on medical and psychiatric history including trauma history. The results of the screening were discussed by the fireworks after-care team. If they agreed that symptoms were disaster-related and the child fulfilled other inclusion criteria for this study, they were eligible to participate. Written consents were obtained. The manager of the after-care team then randomised participants to either CBT or EMDR by flipping a coin and assigned participants to therapists on the basis of availability. Assessments pre-treatment, post-treatment, and at follow-up were conducted by one independent assessor who was blind to the treatment conditions. Parents completed paper-and-pencil measures at pre-treatment, post-treatment, and at follow-up, and only children of 7 years and older completed self-report measures.
Both CBT and EMDR treatment were manualised to ensure that the respective interventions were standardised across clinicians. Psycho-education regarding explanation of post-traumatic symptoms and the treatment were part of both methods. Both CBT and EMDR entailed a focus on the identified disaster-related trauma memory. To equalise the treatment conditions, the therapist was allowed to treat other trauma memories if they spontaneously arose while working with the index trauma but was not allowed to systematically work through all trauma memories as might normally be done by some therapists (but not others) in clinical practice. Participants received up to four individual weekly sessions of 60 min duration. As in clinical practice, termination criteria were: (1) children were asymptomatic according to participant and parent verbal report, and (2) therapist and child (>12 years)/parents agreed that no additional sessions were necessary. When there were still severe complaints after four sessions, the multidisciplinary team could decide to offer more trauma treatment. Three participants were referred for additional treatment (not trauma-related) after the research protocol was completed: one in the EMDR condition and two in the CBT condition.
Because parent guidance is an integral part of treatment for child and adolescent trauma, parents in both groups attended up to four sessions provided by the child's therapist or by a trained colleague. Parent sessions were typically held on the same day as the child sessions and were discontinued upon termination of the child's treatment. The child plus parent sessions in each treatment condition provided a total of up to 8 hours of treatment.
Interventions
CBT
The exposure-based CBT intervention (originally opvangprotocol; Eland, de Roos, & Kleber, 2002; see Table 1) was the predominant trauma treatment available to children in the Netherlands at the time of the study. The most important elements of the treatment are psycho-education about trauma and its effects, repeated exposure to the trauma memory via the development of a detailed trauma narrative, cognitive restructuring, exploring and correcting undesired or unhelpful coping behaviour, and relapse prevention. The trauma narrative is constructed over the course of several sessions by having the client describe the trauma in detail including thoughts, feelings, images/sensations, and events as they occurred. If the narrative exposure did not by itself lead to changes in dysfunctional trauma-related beliefs or behaviours, cognitive restructuring and advice about changing unhelpful coping behaviour was provided. Conjoint parent–child feedback is a common element in all sessions, giving children an opportunity to share their trauma narratives and other aspects of the session with their parents. Because of the wide age range of our sample, developmentally appropriate modifications were incorporated into the child sessions. This primarily involved using age-appropriate language to describe the events and its effects in the narrative, add drawings where necessary to the narrative to increase detail and clarity, and using age-appropriate language to provide advice about changing dysfunctional beliefs and coping skills. The applicability of this CBT protocol had previously been examined in a feasibility study (N=47, age 4–18, single trauma) and showed that it was effective in reducing post-traumatic stress reactions and behaviour problems (Eland, de Roos, & Kleber, 1999).
Table 1.
Overview of child session by session content for CBT and EMDR
| Session | EMDR | CBT |
|---|---|---|
| 1 | • Psycho-education • EMDR protocol on target memory with highest level of disturbance |
• Psycho-education • exposure to the trauma memory via development of trauma narrative |
| 2 | • Finishing reprocessing previous target or start reprocessing next target memory | • Exposure to the trauma memory via development of trauma narrative • Cognitive restructuring and exploring and correcting undesired or unhelpful coping behaviour |
| 3 | • Finishing reprocessing previous target or start reprocessing next target memory | • Exposure to the trauma memory via development of trauma narrative • Cognitive restructuring and exploring and correcting undesired or unhelpful coping behaviour |
| 4 | • Finishing reprocessing previous target or start reprocessing next target memory | • Relapse prevention |
EMDR treatment
EMDR is a treatment for traumatic memories and their sequelae requiring the client to attend a distracting (or “dual attention”) stimulus (typically the therapist's fingers moving back and forth in front of client's face and sometimes audio tones or hand taps are used) while concentrating on the trauma memory (Shapiro, 2001). Briefly, EMDR treatment consists of (1) Taking history and planning treatment. (2) Explanation of and preparation for EMDR. (3) Preparation of the target memory. The client is asked to focus on the worst moment of the memory in a multi-modal manner including image, thought, emotion, and physical sensation. (4) Desensitisation of the memory. The therapist asks the patient to hold the target image in mind while concentrating on the stimulus for about 30 seconds. The client reports briefly what comes up and is guided by the clinician to refocus on that during further exposure to the distracting stimulus. This continues until the client reports no remaining distress related to the memory. (5) Guiding the client to embrace a relevant positive belief regarding the event. (6) Identification and processing of any residual disturbing body sensations. (7) Closure of the session. (8) Re-evaluation, in which the patient comments on previously processed targets as a basis for guiding further intervention.
The EMDR procedure in the present study was based on Shapiro's (2001) protocol, with age-appropriate modifications suggested by Tinker and Wilson (1999) and Greenwald (1999). In this study, mainly the therapist's moving hand was used as the distracting stimulus.
Parent guidance
Parent guidance sessions were equivalent across treatment conditions. Goals of the parent guidance were to resolve parents’ own emotional upset about the child's traumatic exposure and to correct cognitive distortions that the parents may have had. Parents also received psycho-education and advice on enhancing effective parenting and appropriate parental support, affective expression, and correcting of undesired coping behaviour of their child.
Therapists and training
Treatment was conducted by eight licensed therapists (three psychotherapists, two psychologists, and two registered psychiatric social workers). Each of the therapists treated at least one participant in each condition, and up to seven participants in total. All clinicians were trained in both treatments by the first author, a co-developer of the CBT protocol, and an expert on EMDR for children.
Treatment adherence
Several actions were taken to support and evaluate treatment adherence.
Supervision
Once a month the first author provided a full day (six contact hours) of group supervision to the clinicians on both methods. Supervision was also frequently provided by e-mail to ensure that therapists received supervision during the course of treatment with each participant.
Session checklist forms
To optimise treatment adherence, clinicians were required to follow detailed session checklist forms filling in client responses. These forms laid out each session in a step-by-step sequence of interventions, consistent with the instructions in the respective treatment manuals.
Fidelity ratings
Due to the lack of funding, taping of sessions was not possible. To evaluate treatment adherence, 25% of the completed session forms were randomly selected (blocked for equal sampling from each therapist and each treatment). The overall mean treatment integrity score (maximum was 100) was 98 for EMDR (SD=6.9) and 96 for CBT (SD=6.3). Interrater reliability was high (Cohen's kappa: .96).
Measures
Primary outcome measures
The UCLA PTSD Reaction Index (PTSD-RI) for DSM–IV has been extensively used to assess children's trauma exposure and post-traumatic stress symptoms across a variety of trauma types, age ranges, settings, and cultures (Steinberg, Brymer, Decker, & Pynoos, 2004). In the present study, child and adolescent forms were used as a self-report scale with children from the age of 6 and older. The parent version was used for all ages. The disaster-related index event was the focus of the responses. A cutoff of 38 or greater for a single incident traumatic event has been found to have the greatest sensitivity and specificity for detecting PTSD (Steinberg et al., 2004). In the present study Cronbach's alpha was .85.
The Child Report of Post-traumatic Symptoms (CROPS; Greenwald & Rubin, 1999) is a 26-item self-report questionnaire not referenced to a specific event, covering a broad spectrum of children's post-traumatic symptoms. The CROPS has shown good validity and reliability with children ages 7–17 in several settings and languages as well as sensitivity to change in post-traumatic status (Greenwald et al., 2002). We did not use the CROPS with the younger children because of concerns about item comprehension. In the present study Cronbach's alpha was .89.
The Parent Report of Post-traumatic Symptoms (PROPS, Greenwald & Rubin, 1999) is a 32-item companion measure to the CROPS, with similar validity with children ages 7–17 (Greenwald et al., 2002). We used the PROPS with all participants because the PROPS symptoms apply also to younger children and because downward age extension has been successful in clinical practice. In the present study Cronbach's alpha was .90.
Secondary outcome measures
The Birleson Depression Scale (BDS; Birleson, 1981) was used to assess the degree of depression. This self-report inventory consists of 18 items with a three point scale. The BDS has shown satisfactory internal consistency and stability (Ivarsson & Gillberg, 1997). In the present study Cronbach's alpha was .78.
The Multidimensional Anxiety Scale for Children (MASC; March, Parker, Sullivan, Stallings, & Conners, 1997) is a 39-item self-report measure of anxiety symptoms in children and adolescents, aged 7–18. The MASC demonstrated good convergent and divergent validity (March et al., 1997). In the present study, Cronbach's alpha was .88.
The Child Behaviour Check List (CBCL; Achenbach, 1991) is a widely used 118-item behaviour rating scale for children ages 4–18, where parents rate their child's behavioural problems. It has very acceptable reliability and validity. Verhulst, van der Ende, and Koot (1996) reported Cronbach's alphas of .85, .86, and .92 for internalising, externalising, and total scores, respectively.
Statistical analyses
Analysis of variance and the descriptive statistics were performed with SPSS 14.0 for Windows. Pre-treatment (baseline) demographic characteristics, clinical variables, and extent of exposure to the Enschede disaster were compared between the two treatment conditions using independent t-tests for continuous variables and Chi-square tests for categorical variables. The data were analysed using analysis of variance (GLM: general linear model, repeated measures). Time (pre-treatment, post-EMDR/CBT, and follow-up) was used as a within-subject variable, and treatment (CBT or EMDR) as a between-subject variable. Two types of analyses were performed. Primary analyses were performed on the intention-to-treat sample using data from all randomised participants, while secondary analyses were performed using data from subjects who completed treatment. In the intention-to-treat analysis we replaced outcome data that were missing due to dropout using multiple imputations by fully conditional specification (Van Buuren, 2007). The imputation model was specified for 44 outcomes. Predictors in the imputation model included age, sex, treatment, treatment of parents, and ethnicity as well as other outcomes and were set up such that both relations between and within time were preserved. Five complete data sets were made by 20 Gibbs sampling iterations in Multivariate Imputation by Chained Equations (MICE; Van Buuren & Oudshoorn, 2000).
All GLM analyses were repeated for each set. Pooling of statistical parameters was done by Rubin's rules (Rubin, 1987). Pooling of ANOVA tables was done by the procedure of Li, Meng, Raghunathan, and Rubin (1991) applied to the F-statistic. Post hoc analysis also employed the effect size (ES) of the change using Cohen's d (Cohen, 1992). To correct for dependence among means in order to make direct comparisons to effect sizes from between-subjects studies, we used the correlation between the two means so that Morris and DeShon's (2002) equation can be applied. An effect size <.50 is considered small, between .50–.80 is considered moderate, and >.80 is considered large. For all statistical analyses, a p-value <.05 was considered statistically significant.
A time-to-event analysis for treatment efficiency was done for three outcomes: number of child sessions, number of parent sessions, and the sum of these two. The analysis was performed by Cox regression using the number of sessions as the outcome, dropout as the censoring indicator, and treatment group as the explanatory variable. Ties were handled by the Efron approach. Additional covariates (age, sex, and indicators of trauma severity) were included to see whether these explain any observed differences in efficiency. The covariate trauma severity was measured by the following indicators: “present in inner ring” (yes/no), “thought I would die” (yes/no), “separated from parents” (yes/no), “house damaged or lost” (yes/no). We tested for proportionality of the hazards by weighted residuals approach of Therneau and Grambsch (2000). Calculations were done with the cox.zph function in R2.11.1. None of the terms of the model was significant at the .5 level. The data thus do not contradict the assumption of proportional hazards.
Results
Descriptive statistics
In Table 3, demographic characteristics and clinical variables by treatment group are shown. Of the 52 children included in the study, 23% (n=12) fell within the age range 4–6 years, 46% (n=24) fell in the age range of 7–12 years, and 31% (n=16) were aged 13–18 years. Of the total group, 55.8% were boys. A large proportion (47%) belonged to an ethnic minority group comprising Turkish (32%) and other ethnic origins, although 83% of the children were born in the Netherlands. Most of the participants were considered to have had “severe” exposure to the fireworks disaster (see Table 2). In the brief lifetime trauma screen (UCLA), 32.7% reported no other significant history of trauma exposure, 25% reported at least one other significant past trauma event, and 42.3% reported two or more prior traumatic events. The mean number of experienced traumatic events (the firework disaster included) was 2.4 (SD=1.31). On the UCLA parent form, 17.3% of participants met full criteria of PTSD, and 59.6% met criteria for partial PTSD (i.e., criterion A met, and criteria (B+C) or (B+D) or (C+D).
Table 3.
Demographic characteristics and clinical variables by treatment group (N=52)
| Variable | CBT n=26 | EMDR n=26 | Comparison |
|---|---|---|---|
| Age | 10.0 | 10.2 | t=.24, df=1, ns |
| SD | 4.1 | 4.0 | |
| Gender | |||
| Male | 16 | 13 | χ2=.70, df=1, ns |
| Female | 10 | 13 | |
| Ethnicity | |||
| Native | 14 | 11 | χ2=.69, df=1, ns |
| Immigrant | 12 | 15 | |
| Parents in treatment | |||
| Yes | 13 | 12 | χ2=.08, df=1, ns |
| No | 13 | 14 | |
Table 2.
Extent of exposure to Enschede disaster by treatment group (N=52)
| Variable | CBT n=26 | EMDR n=26 | Comparison |
|---|---|---|---|
| Present in inner ring | 17 | 20 | χ2=2.35, df=1, ns |
| Thought that he/she was going to die | 17 | 17 | χ2 =.00, df=1, ns |
| Separated from one of parents | 23 | 21 | χ2=.27, df=1, ns |
| Home damaged or lost | 17 | 14 | χ2=1.47, df=3, ns |
| Parent severely injured | 0 | 3 | χ2=3.18, df=1, ns |
| Injured her/himself | 2 | 5 | χ2=1.65, df=1, ns |
| Family member died | 1 | 1 | χ2=.01, df=1, ns |
| Number of trauma's (Enschede disaster included) | 2.8 | 2.3 | F=3.01, df=50, ns |
Pre-treatment differences
Pre-treatment assessment showed no differences between both treatment groups (intention to treat) on any of the demographic variable (see Table 2) and outcome measures except for the UCLA parent version (t=2.5, df=50, p=.02). Because data were collected over a 3-year period, which equated a range of participants receiving treatment 1–4 years post-disaster, time since disaster in relation to impact of treatment and/or severity of symptoms at pre-treatment was examined. The relation between “time since disaster” and “severity of symptoms” was positive on all measures, indicating that the longer after the disaster children were referred for treatment, the more severe the symptoms were. However, none of the regression weights were significantly different from zero. In addition, the regression weight relating “time since disaster” and “impact of treatment” was not significant.
Dropout analysis
Of the 52 initial participants 14 (27%) dropped out: 8 (30.8%) from the EMDR group and 6 (23.1%) from the CBT group. The dropout rate was not significantly different across both groups (χ2=.39, df=1, p=.53). Thirty-eight children completed both the treatment and the follow-up (18 EMDR, 20 CBT). Of them, 21 were boys (55.3%). The main reason given for dropping out was that the parents were overburdened (57%). Other reasons for dropping out were: refusing to talk (7%), language problems (7%), and a new trauma rising to the forefront (14%). One adolescent refused treatment from a therapist not belonging to his own culture (7%) and one child showed spontaneous recovery before treatment started (7%). Dropout occurred in the very beginning before treatment was started and seemed to be unrelated to the treatment condition. For this group that did not receive the allocated treatment, it was attempted to conduct the assessments post-treatment and at follow-up, albeit without success. Comparison between the 14 dropouts and the 38 completers regarding presentation at time of initial assessment yielded no significant differences on any of the demographic characteristics or number of traumatic experiences (UCLA parent version, trauma screen). On the symptom scales, only the mean score of the PROPS was marginally significantly higher for the dropout group than for the treatment completers (t=2.09, df=48, p=.04).
Intention-to-treat analysis regarding change over time and intervention effects
Repeated measures analysis of variance of treatment outcome after treatment (n=52) and at follow-up (n=52) indicated a significant time effect (all p-values <.001) and no interaction effect between time and treatment condition for all measures (p-values between .11 and .51). This indicates that both CBT and EMDR were effective and that neither was significantly more effective than the other in reducing symptoms of PTSD, anxiety, depression, or behavioural problems. Findings remained the same when the analysis was repeated for native and immigrant children separately. Table 4 shows means and standard deviations for both treatment groups pre-treatment, post-treatment, and follow-up on all measures. At post-test, 0% met criteria of full PTSD and partial PTSD. At follow-up there was a slight increase: 5.8% met full criteria of PTSD and 0% met criteria for partial PTSD. The fraction of missing information of the estimates in Table 4 varied between 0 and .05. Since all are well below .10, the choice for m=5 multiple imputations was adequate (Schafer, 1997, p. 198–200).
Table 4.
Means and SDs of measures for EMDR (n=26) and CBT (n=26) groups at pre-test, post-test, and follow-up, including corresponding effect sizes for the intention-to-treat sample
| Variable | Pre-test T1 | Post-test T2 | Follow-up T3 | Effect size T1–T2 | Effect size T1–T3 |
|---|---|---|---|---|---|
| PROPS | |||||
| EMDR | 30.5 (11.5) | 17.7 (9.6) | 19.2 (13.1) | 1.08 | 1.01 |
| CBT | 34.7 (12.8) | 19.5 (11.7) | 21.3 (13.3) | 1.40 | 1.20 |
| CROPS* | |||||
| EMDR | 23.3 (9.9) | 12.0 (9.1) | 11.2 (8.0) | 1.02 | 1.10 |
| CBT | 22.7 (9.6) | 12.3 (8.1) | 11.9 (8.3) | 1.16 | .98 |
| UCLA Ch/Ad Total* | |||||
| EMDR | 31.4 (12.3) | 16.1 (9.1) | 14.2 (9.0) | 1.23 | 1.44 |
| CBT | 30.5 (10.4) | 16.9 (9.6) | 16.7 (9.3) | 1.06 | 1.27 |
| UCLA Par. Total | |||||
| EMDR | 31.3 (10.5) | 20.2 (9.6) | 15.6 (10.4) | 1.00 | 1.62 |
| CBT | 38.5 (8.2) | 22.8 (10.5) | 24.6 (11.9) | 1.38 | 1.07 |
| Birleson* | |||||
| EMDR | 13.5 (5.5) | 7.8 (5.2) | 6.5 (5.3) | .92 | 1.04 |
| CBT | 14.2 (6.3) | 7.6 (5.0) | 8.6 (6.0) | 1.09 | .80 |
| MASC Total* | |||||
| EMDR | 53.8 (17.7) | 33.1 (14.9) | 33.3 (17.4) | 1.12 | 1.02 |
| CBT | 47.6 (16.8) | 33.8 (18.9) | 31.6 (18.4) | .62 | .85 |
| CBCL Total | |||||
| EMDR | 56.3 (29.1) | 36.7 (24.5) | .88 | ||
| CBT | 56.3 (23.5) | 41.8 (25.0) | .87 | ||
UCLA Par. Total means UCLA Parent version Total, UCLA Ch/Ad Total means UCLA Child/Adolescent version.
Lower n as children under 7 years did not complete these self-report measures: EMDR (n=21), CBT (n=19).
Effect sizes
Table 4 also shows the effect sizes related to the various measures for the intention-to-treat sample concerning pre-treatment versus post-treatment and pre-treatment versus follow-up. Large effect sizes were found for both treatments on all but one outcome measures, which ranged for T1–T2 in the EMDR condition between .92 and 1.23 and in the CBT condition between .62 and 1.40. Effect sizes calculated for T1–T3 ranged in the EMDR condition between .88 and 1.62 and in the CBT condition between .80 and 1.27.
Completer analysis
Among participants providing outcome data, 20 in the CBT group and 18 in the EMDR group completed treatment. Results were similar to the results of the intention-to-treat analysis showing that both treatment groups improved significantly on all measures (all p-values <.001). No interaction effect between time and treatment condition emerged (p-values between .09 and .69).
Efficiency
In order to assess whether one of the treatment methods produced greater treatment gains with fewer appointments, the mean amount of sessions per group was calculated. The mean number of child sessions needed was 3.17 (SD=.86, range 2–5) in the EMDR group and 4.00 (SD=1.03, range 2–7) in the CBT group (t=2.7, df=36, p=.011). Prior to session 4, 20% of the children in the CBT group and 66.6% in the EMDR group were asymptomatic. The time-to-event analysis showed that EMDR was more efficient than CBT in both the plain analysis (hazard ratio [HR]: .34 [.17–.67] 95% CI) and after correction for age, sex, and trauma severity (HR .33 [.15–.73]). The mean number of parent sessions was 3.11 (SD=1.53, range 0–5) for EMDR and 3.55 (SD=1.32, range 0–7) for CBT (not significant). The time-to-event analysis yielded a similar result (HR: .77 [.40–1.46]). The mean number of child and parent sessions summed together (EMDR 6.28, CBT 7.55) showed a significant difference in favour of the EMDR group (t=2.16, df=36, p=.038). The corresponding plain time-to-event analysis produced a hazard ratio of .43 [.22–.85]. The ratio changed to .50 [.22–1.12]) after correcting for age, sex, and trauma.
Discussion
To our knowledge this was the first randomised controlled study for children's disaster-related post-traumatic stress symptoms comparing two active treatments among children in a broad age range and from a wide diversity of ethnic populations. Apparently both CBT and EMDR are capable of substantially reducing children's symptoms of post-traumatic stress, anxiety, depression, and behavioural problems presenting in a community mental health setting. The post-treatment gains of both treatments were maintained at 3-months follow-up, while no side effects were reported. These findings are especially promising considering that the children and parents in the present study received together only six to eight sessions of 60 min each, indicating that brief treatment in this context can be highly beneficial. The results bode well in the light of the large treatment needs among traumatised children worldwide and are consistent with data on adult studies on CBT and EMDR, in that both methods were efficacious and that the effect sizes were substantial (Bisson et al., 2007; Seidler & Wagner, 2006). Although no significant differences between the treatments were found, this does not mean that differences can be excluded since the study may be underpowered.
The finding that treatment gains of EMDR were reached in fewer sessions than those of CBT is in line with some previous randomised controlled studies comparing CBT and EMDR (Jaberghaderi et al., 2004; Power et al., 2002). However, it is possible that this finding of difference in efficiency was an artefact of slight differences across conditions in the treatment fidelity and of the research design. In this study, the session durations were roughly similar across treatment conditions, but the number of min per session was not precisely tracked. It is therefore conceivable that the mean duration of the CBT sessions might have been shorter than that of the EMDR sessions.
A number of other limitations must be recognised when considering the present findings. First, the relatively small number of participants may have resulted in a lack of sufficient power and sensitivity to detect small differences between the groups. Second, the study lacked a no-treatment control group. Third, follow-up assessments were undertaken at only 3 months post-treatment, thereby limiting conclusions regarding the sustainability of the treatment gains over a longer time period. Finally, in this unfunded field study the fidelity ratings were based on session checklists with no systematic review of session recordings to verify the therapists’ documentation. Therefore, the current findings must be interpreted with due caution.
Methodological strengths of our trial include the inclusion of two active trauma treatments, validated measures with clearly defined target symptoms, multiple sources to detect the impact of treatment on multiple symptom domains, random assignment to treatment condition, the same therapists for both treatment conditions cancelling possible therapist effects, blind evaluation, detailed manual-guided treatment protocols, expert therapist training, supervision and therapist checklist forms to support treatment adherence, (limited) assessment and confirmation of treatment fidelity, and field conditions and inclusion criteria supporting ecological validity.
Conclusions
The present results provide support for the effectiveness of both EMDR and CBT among a heterogeneous, multicultural sample of children and adolescents with disaster-related symptoms indicating the feasibility of implementing these treatments for children. A difference is found between EMDR and CBT for efficiency. More research is needed to confirm EMDR's efficiency advantage and to address the issue of comparative efficacy between these treatments for psychological trauma.
Acknowledgements
We are grateful to all children, parents, and therapists of Mediant, who took part in the study. Moreover, we gratefully acknowledge Mrs. E. Vroom, research nurse, whose great effort contributed to completing data acquisition.
For the abstract or full text in other languages, please see Supplementary files under Reading Tools online
Conflict of interest and funding
There is no conflict of interest in the present study for any of the authors.
References
- Achenbach T. M. Manual for the child behavior checklist/4-18 & 1991 profile. Burlington, VT: Department of Psychiatry, University of Vermont; 1991. [Google Scholar]
- Adler-Nevo G., Manassis K. Psychosocial treatment of pediatric posttraumatic stress disorder: The neglected field of single-incident trauma. Depression and Anxiety. 2005;22:177–189. doi: 10.1002/da.20123. [DOI] [PubMed] [Google Scholar]
- Birleson P. The validity of depressive disorder in childhood and the development of a self-rating scale: A research report. Journal of Child Psychology and Psychiatry. 1981;22:73–88. doi: 10.1111/j.1469-7610.1981.tb00533.x. [DOI] [PubMed] [Google Scholar]
- Bisson J. I., Ehlers A., Matthews R., Pilling S., Richards D., Turner S. Psychological treatments for chronic post-traumatic stress disorder. Systematic review and meta-analysis. British Journal of Psychiatry. 2007;190:97–104. doi: 10.1192/bjp.bp.106.021402. [DOI] [PubMed] [Google Scholar]
- Catani C., Kohiladevy M., Ruf M., Schauer E., Elbert T., Neuner F. Treating children traumatized by war and tsunami: A comparison between exposure therapy and meditation-relaxation in North-East Sri Lanka. BMC Psychiatry. 2009;9:22. doi: 10.1186/1471-244X-9-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chemtob C. M., Nakashima J., Carlson J. G. Brief treatment for elementary school children with disaster-related posttraumatic stress disorder: A field study. Journal of Clinical Psychology. 2002;58:99–112. doi: 10.1002/jclp.1131. [DOI] [PubMed] [Google Scholar]
- Chemtob C. M., Nakashima J. P., Hamada R. S. Psychosocial intervention for postdisaster trauma symptoms in elementary school children: A controlled community field study. Archives of Pediatrics & Adolescent Medicine. 2002;156:211–216. doi: 10.1001/archpedi.156.3.211. [DOI] [PubMed] [Google Scholar]
- Cohen J. A power primer. Psychological Bulletin. 1992;112:155–159. doi: 10.1037//0033-2909.112.1.155. [DOI] [PubMed] [Google Scholar]
- Cohen J. A., Mannarino A. P., Gibson L. E., Cozza S. J., Brymer M. J., Murray L. Interventions for children and adolescents following disasters. In: Ritchie E., Watson P., Friedman M., editors. Interventions following mass violence and disasters, strategies for mental health practice. New York: Guilford Press; 2006. pp. 227–256. [Google Scholar]
- Committee Oosting. De vuurwerkramp eindrapport (The Netherlands); Rotterdam: Phoenix and den Oudsten; 2001. [The firework disaster. Final report] [Google Scholar]
- Eland J., de Roos C., Kleber R. Ontwikkelingsonderzoek naar een opvangprotocol voor kinderen na acute traumatisering [Feasibility study of the ‘opvangprotocol’ for acutely traumatised children] Utrecht: Institute of Psychotrauma; 1999. [Google Scholar]
- Eland J., de Roos C., Kleber R. Kind en trauma, een opvangprogramma. 2nd ed. The Netherlands: Harcourt Assessment B.V; 2002. [Google Scholar]
- Goenjian A. K., Molina L., Steinberg A. M., Fairbanks L. A., Alvarez M. L., Goenjian H. A., et al. Posttraumatic stress and depressive reactions among Nicaraguan adolescents after hurricane Mitch. American Journal of Psychiatry. 2001;158:788–794. doi: 10.1176/appi.ajp.158.5.788. [DOI] [PubMed] [Google Scholar]
- Goenjian A. K., Walling D., Steinberg A. M., Karayan I., Najarian L. M., Pynoos R. A prospective study of posttraumatic stress and depressive reactions among treated and untreated adolescents 5 years after a catastrophic disaster. American Journal of Psychiatry. 2005;162:2302–2308. doi: 10.1176/appi.ajp.162.12.2302. [DOI] [PubMed] [Google Scholar]
- Greenwald R. Eye movement desensitization and reprocessing (EMDR) in child and adolescent psychotherapy. Northvale, NJ: Jason Aronson; 1999. [Google Scholar]
- Greenwald R., Rubin A. Brief assessment of children's post-traumatic symptoms: Development and preliminary validation of parent and child scales. Research on Social Work Practice. 1999;9:61–75. [Google Scholar]
- Greenwald R., Rubin A., Jurkovic G. J., Wiedemann J., Russell A. M., O'Connor M. B., et al. Psychometrics of the CROPS & PROPS in multiple cultures/translations; 2002. Nov, Presented at the annual meeting of the International Society for Traumatic Stress Studies, Baltimore, MD. [Google Scholar]
- Ivarsson T., Gillberg C. Depressive symptoms in Swedish adolescents: Normative data using the Birleson Depression Self-Rating Scale (DSRS) Journal of Affective Disorders. 1997;4:59–68. doi: 10.1016/s0165-0327(96)00098-5. [DOI] [PubMed] [Google Scholar]
- Jaberghaderi N., Greenwald R., Rubin A., Zand S. H., Dolatabadi S. A comparison of CBF-BT and EMDR for sexually-abused Iranian girls. Clinical Psychology and Psychotherapy. 2004;11:358–368. [Google Scholar]
- Jaycox L. H., Cohen J. A., Mannarino A. P., Walker D. W., Langley A. K., Gegenheimer K. L., et al. Children's mental health care following hurricane Katrina: A field trial of trauma-focused psychotherapies. Journal of Traumatic Stress. 2010;23(2):223–231. doi: 10.1002/jts.20518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- La Greca A. Interventions for PTSD in children and adolescents following natural disasters and acts of terrorism. In: Steele R.G., Elkin T. D., Roberts M.C., editors. Handbook of evidence-based therapies for children and adolescents. New York, NY: Springer; 2008. pp. 121–145. [Google Scholar]
- Li K. H., Meng X. L., Raghunathan T. E., Rubin D. B. Significance levels from repeated p-values with multiply-imputed data. Statistica Sinica. 1991;1:65–92. [Google Scholar]
- March J. S., Parker J. D., Sullivan K., Stallings P., Conners C. K. The Multidimensional Anxiety Scale for Children (MASC): Factor structure, reliability, and validity. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:554–565. doi: 10.1097/00004583-199704000-00019. [DOI] [PubMed] [Google Scholar]
- Morris S. B., DeShon R. P. Combining effect size estimates in meta-analysis with repeated measures and independent-groups designs. Psychological Methods. 2002;7:105–125. doi: 10.1037/1082-989x.7.1.105. [DOI] [PubMed] [Google Scholar]
- Power K., McGoldrick T., Brown K., Buchanan R., Sharp D., Swanson V., et al. A controlled comparison of eye movement desensitization and reprocessing versus exposure plus cognitive restructuring versus waiting list in the treatment of post-traumatic stress disorder. Clinical Psychology and Psychotherapy. 2002;9:299–318. [Google Scholar]
- Rubin D. B. Multiple imputation for nonresponse in surveys. New York, NY: Wiley; 1987. [Google Scholar]
- Salloum A., Overstreet S. Evaluation of individual and group grief and trauma interventions for children post disaster. Journal of Clinical Child & Adolescent Psychology. 2008;37:495–507. doi: 10.1080/15374410802148194. [DOI] [PubMed] [Google Scholar]
- Schafer J. L. Analysis of incomplete multivariate data. London: Chapman & Hall; 1997. [Google Scholar]
- Seidler G. H., Wagner F. E. Comparing the efficacy of EMDR and trauma-focused cognitive-behavioral therapy in the treatment of PTSD: A meta-analytic study. Psychological Medicine. 2006;36:1515–1522. doi: 10.1017/S0033291706007963. [DOI] [PubMed] [Google Scholar]
- Shapiro F. Eye movement desensitization and reprocessing basic principles protocols, and procedures. New York, NY: Guilford Press; 2001. [Google Scholar]
- Stallard P. Psychological interventions for post-traumatic reactions in children and young people: A review of randomised controlled trials. Clinical Psychology Review. 2006;26:895–911. doi: 10.1016/j.cpr.2005.09.005. [DOI] [PubMed] [Google Scholar]
- Steinberg A. M., Brymer M. J., Decker K. B., Pynoos R. S. The university of California at Los Angeles Post-traumatic Stress Disorder Reaction Index. Current Psychiatry Reports. 2004;6:96–100. doi: 10.1007/s11920-004-0048-2. [DOI] [PubMed] [Google Scholar]
- Therneau T. M., Grambsch P. M. Modeling survival data: Extending the Cox model. New York, NY: Springer; 2000. [Google Scholar]
- Tinker R., Wilson S. Through the eyes of a child: EMDR with children. New York, NY: Norton; 1999. [Google Scholar]
- Van Buuren S. Multiple imputation of discrete and continuous data by fully conditional specification. Statistical Methods in Medical Research. 2007;16(3):219–242. doi: 10.1177/0962280206074463. [DOI] [PubMed] [Google Scholar]
- Van Buuren S., Oudshoorn C. G. M. Multivariate imputation by chained equations: MICE V1.0 User's manual. TNO Report PG/VGZ/00.038. Leiden: TNO Preventie en Gezondheid; 2000. [Google Scholar]
- Verhulst F. C., van der Ende J., Koot H. M. Handleiding voor CBCL/4-18. [Manual for the CBCL 14-18]. Rotterdam: EUR/AZR/Sophia Kinderziekenhuis, afdeling Kinder en Jeugdpsyhiatrie; 1996. [Google Scholar]
- Yule W., Bolton D., Udwin O., Boyle S., O'Ryan D., Nurrish J. The long-term psychological effects of a disaster experienced in adolescence: I: The incidence and course of PTSD. Journal of Child Psychology and Psychiatry. 2000;41:503–511. [PubMed] [Google Scholar]