Abstract
Background
Single traumatising events are associated with an elevated rate of psychological disorders in children and adolescents. To date, it remains unclear whether early psychological interventions can reduce longer term psychological maladjustment.
Objective
To systematically review the literature to determine the characteristics and efficacy of early psychological interventions in children and adolescents after a single, potentially-traumatising event.
Design
Systematic searches were conducted of all relevant bibliographic databases. Studies on early psychological interventions were included if the first session was conducted within 1 month of the event. Two independent observers assessed each study for eligibility, using pre-determined inclusion and exclusion criteria, and rated the study's methodological quality. A meta-analysis was conducted on the group effects between individuals allocated to intervention versus control groups. Hence, effect sizes (ES) and confidence intervals were computed as well as heterogeneity and analogue-to-the ANOVA analyses.
Results
Seven studies (including four randomised controlled trials) met the inclusion criteria. Depending on the specific outcome variable (e.g., dissociation, anxiety and arousal), small to large beneficial ES were noted. Although the meta-analysis revealed unexplained heterogeneity between the ES of the included studies, and although studies varied greatly with regards to their methodological quality and the interventions tested, findings suggest that early interventions should involve psycho-education, provide individual coping-skills and probably involve some kind of trauma exposure. Also, a stepped procedure that includes an initial risk screen and the provision of multiple sessions to those children at risk may be a promising strategy.
Conclusions
To date, research on the effectiveness of early interventions in children after a potentially traumatising event remains scarce. However, our review suggests that early interventions may be helpful.
Keywords: systematic review, PTSD, post-traumatic stress, crisis intervention, critical incident stress debriefing
Potentially traumatising events, ranging from car accidents to natural disasters, are frequent in children and adolescents. Approximately two-fifths to two-thirds of children and adolescents in two US studies (Copeland, Keller, Angold, & Costello, 2007; Giaconia et al., 1995) and 15%–22.5% in two European samples (Essau, Conradt, & Petermann, 1999; Perkonigg et al., 2005) had already experienced at least one potentially traumatising event in their life. Meta-analysis conducted by Kahana, Feeny, and Youngstrom (2006) revealed that up to one-fifth of children develop post-traumatic stress disorder (PTSD) after various single traumatising events. Recently, Kronenberg et al. (2010) and LeBrocque et al. (2010) examined trajectories over 3 years in children and adolescents after a hurricane, and over 2 years after accidental injuries, respectively. Both studies identified the same three trajectories, with 70%–90% of the children either resilient or recovered and exhibiting good adaptive functioning within months of the traumatising event. By contrast, the remaining 10%–30% had a chronic course, with significant symptomatology and dysfunction, including PTSD, even 2–3 years later (Kronenberg et al., 2010; Le Brocque, Hendrikz, & Kenardy, 2010).
To prevent such chronic trajectories, early interventions are needed. However, to date, very limited evidence exists to indicate how to best intervene in children in the aftermath of a single traumatic event, and no evidence-based standardised procedure is widely accepted. While systematic reviews on the efficacy of early single interventions in adults have demonstrated either no or even harmful effects (Roberts, Kitchiner, Kenardy, & Bisson, 2010a; Rose, Bisson, Churchill, & Wessely, 2009), multi-session, trauma-focused cognitive behavioural therapy (tf-CBT) interventions for individuals at high risk may be efficient (2010b). However, the evidence for children and adolescents is unclear. Therefore, the aim of this study was to conduct a systematic review of all studies on early psychological interventions in children and adolescents after a single traumatising event. The objectives were (1) to investigate the characteristics of early psychological interventions and (2) to conduct a meta-analysis on the group effects between individuals allocated to an intervention versus a control group. Based on the findings, clinical implications and recommendations for future research are given.
Methods
Data sources and search strategies
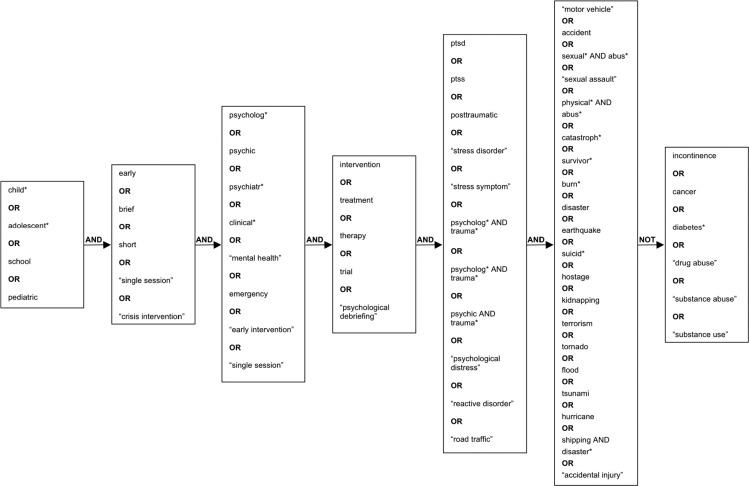
In August 2010, systematic searches using pre-defined keywords in English and German language (see Fig. 1) for empirical studies and dissertations were conducted of EMBASE, CINAHL, PsycINFO, PSYNDEX, the Cochrane database of clinical trials and systematic reviews, NDLDT, ProQuest Digital Dissertation and Dissonline.de.
Fig. 1.
Search criteria tree (English).
The Boolean operator “and” was used to link the three groups of keywords for the patient population, the intervention and the psychiatric disorder, respectively. The search terms within the groups were combined with the operator “or”. To exclude articles, the operator “not” was used. Not all databases allowed the same complexity of keyword combinations. Thus, less complex combinations were created, in accordance with the capacity of the database. Furthermore, reference lists of relevant studies and reviews were revised and authors in the field were contacted for unpublished data.
Study selection
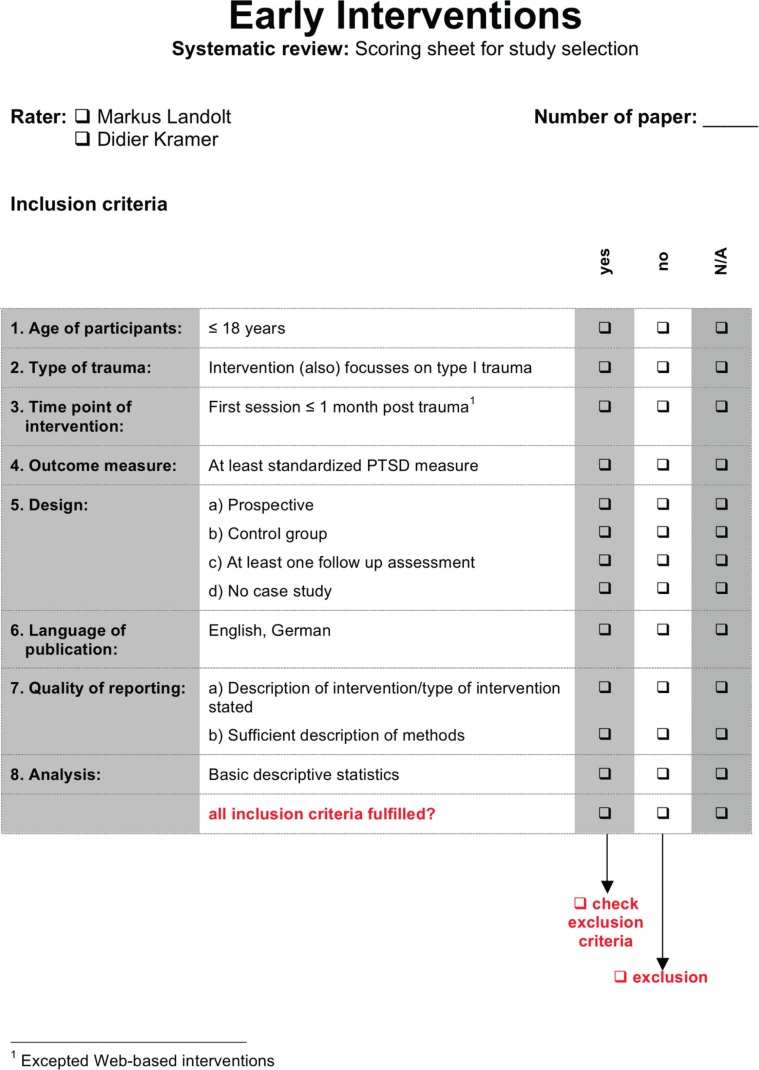
Studies were included if they met the following criteria (see Appendix 1): (1) all participants ≤18 years old; (2) experience of a single trauma; (3) first intervention session within 4 weeks after the traumatising event; (4) at least one standardised measure of PTSD or PTSS (post-traumatic stress symptoms) applied; (5) prospective study design with a control group and at least one follow-up assessment; (6) language of publication English or German; (7) details of the intervention described or general type stated; and (8) descriptive statistics available.
The corresponding authors were contacted if additional information on a given study was needed. Reasons for exclusion were documented (see Appendix 2).
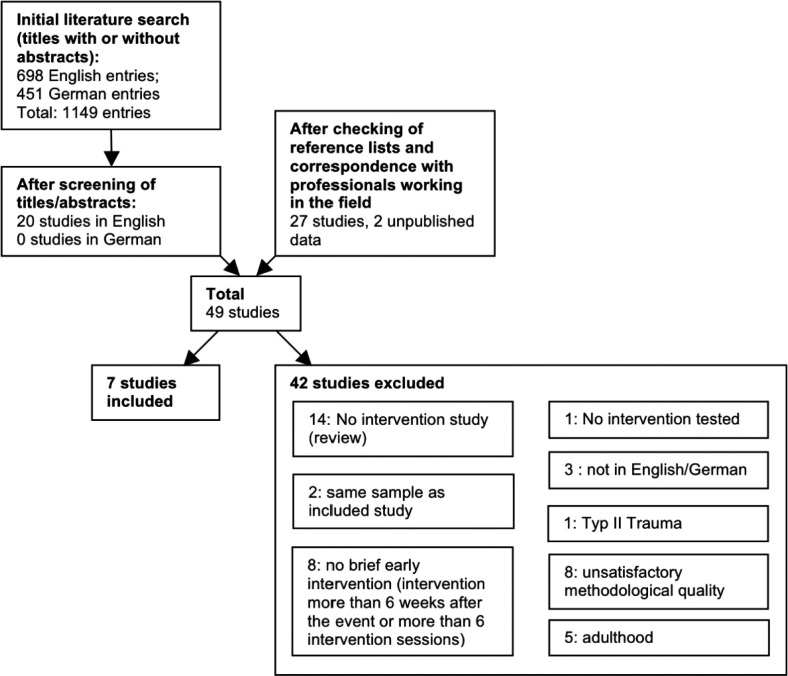
The initial literature search yielded a total of 1,149 entries. After screening titles and abstracts, 20 entries were identified to be of further interest. Examining reference lists and correspondence with professionals working in the field yielded an additional 29 studies. Hence, 49 full-text papers were reviewed. Inclusion and exclusion criteria were independently rated by the two authors, by means of a standardised checklist (see Appendix 1). Disagreements were discussed verbally until consensus was reached. Ultimately, 42 of the 49 studies were excluded, for a variety of reasons (see Fig. 2).
Fig. 2.
Flowchart of study selection.
Methodological quality rating
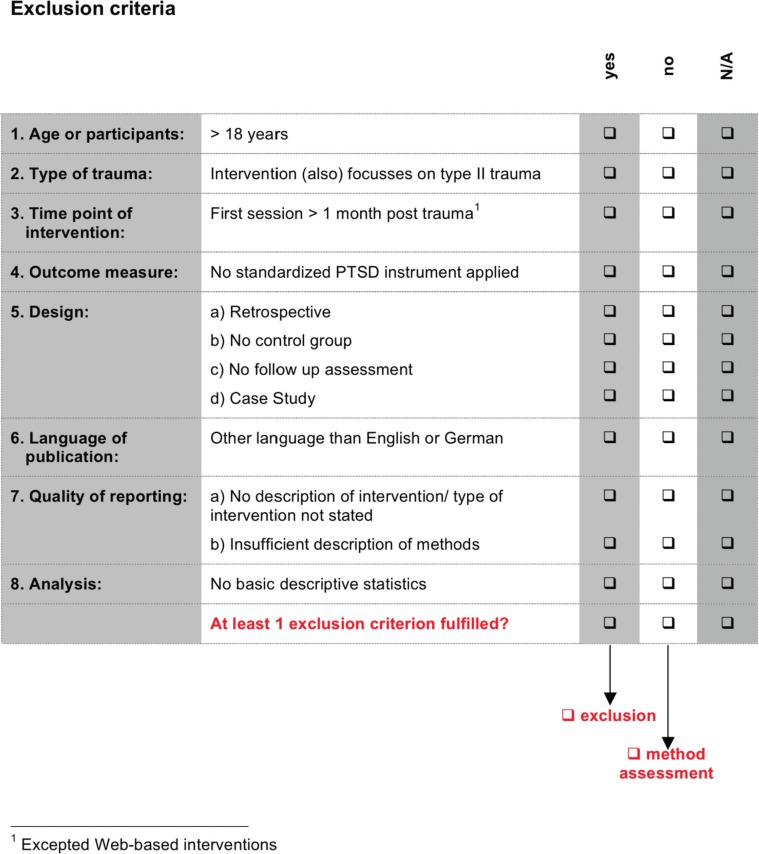
The methodological quality of each of the seven remaining studies was rated independently by the two authors using a standardised checklist with 22 items. Inter-rater reliability by Cohen was excellent, with κ=0.940 (95% CI=0.919–0.957). In any case of disagreement, consensus was achieved by discussion.
Twenty of the 22 items in the utilised checklist (see Appendix 3) were adapted from Roberts, Kitchiner, Kenardy, and Bisson (2010b). Additionally, two items were added to check for the availability of any drop-out analysis and to assess the use of both self and proxy report. Each item was assessed using either a two (0–1) or three point (0–2) scale, with higher values indicating better quality. A maximum total quality score of 42 points was possible.
Due to the specific study concept (web-based information provision), not all the criteria were applicable for two studies (Cox, Kenardy, & Hendrikz, 2010; Kenardy, Thompson, Le Brocque, & Olsson, 2008). Consequently, the percentaged portion of the applicable items that met the methodological criteria was calculated for each study with higher percentages standing for a better methodological quality. Based on the mean overall percentage rate of 66%, two study groups were defined: higher quality studies with quality ratings above the overall mean and lower quality studies with ratings below the mean.
Data extraction
Study methodology and characteristics are summarised in Table 1. Due to the inhomogeneous number, both of the follow-up assessments and data collection points among the different studies, the data were reduced to the following two time points: Follow-up #1 occurring less than 3 months from the traumatic event, and follow-up #2 three or more months post-event. This allocation ensures that, for each outcome variable and follow-up time point, the data of each study are represented only once.
Table 1.
Summary of studies included in the review
| Sample | Design | Intervention | Measures | Results | Quality Rating of Method | |||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|
|
|||||||||||||||||||
| Authors, year | Origin | Number of participants | Age range | Type of trauma | Randomisation | Double blinded | Control groups | Follow up | Type of interventions | Theoretical basis | Time to intervention post trauma | Number of treatment sessions | Setting | Lead professional | Psycho education on posttraumatic stress symptoms | Normalisation of acute stress reactions | Reconstruction of trauma event | Type of coping skills and topics addressed | Social support | Outcome variables-self | Outcome variables-proxy | Predictor variables self or proxy | Reported outcome | Percentage |
| Berkowitz et al., 2011 | USA | 106 | 7–17 | Potentially traumatic events (Motor vehicle accident; sexual abuse; witnessing violence; physical assault; injuries (e.g., sport); animal bite,; threats of violence) | Yes | No | Supportive comparison condition | 4 weeks from baseline assessment (up to 2 months) and 3 months | Caregiver-Child Intervention (CFTSI) | Cognitive and behavioural | Within 30 days | 4 | Child and caregiver separately as well as together | Master- and doctoral-level clinicians | Yes | Yes | No | Thought replacement methods for intrusive thoughts, breath retraining for anxiety, behavioual activation for depression and avoidance. Sleep disturbance, depressive withdrawal, oppositionality/ tantrums, intrusive thoughts, anxiety/ avoidance/ and phobic reactions, general overview of traumatic stress symptoms and techniques to manage them | Comparison of the measured responses in order to improve communication to enhance the emotional support provided by the caregiver | PTSD-RI, TSCC | – | THQ, PBI, PSS-Fa, BASC-2 (Baseline only), CBCL (Baseline only), PCL-C (Screening, Baseline only) | + Significant time x group effects of PTSD-(TSCC) and anxiety (TSCC)-sympotms Significant group differences in relation to re-experiencing and avoidance-symptoms (PTSD-RI) | 81% |
| Cox et al., 2010 | AUS | 56 | 7–16 | Unintentional injuries including mild traumatic brain injury | Yes | No | No intervention | 4–6 weeks and 6 months | Web-based information | Cognitive and resilience theory | 2–3 weeks | Access 2 weeks posttrauma to the third postintervention assessment after 6 months | Provision of written information for parents and child separately | No personal contact (written information provided) | Yes | Yes | Recommend that children and parents talk about and reflect upon the accident | Instructions how to emotionally support the child and how to cope with own distress, relaxation, doing pleasant activities, identifying personal strengths, reflection of the event. | Emphasize parental role for the child's recovery | TSCC-A | – | IES-R (parents) | + Significant time x group effects of anxiety (TSCC-A): Decrease in the intervention group; increase in the control group. | 82% |
| Kenardy et al., 2008 | AUS | 103 | 7–15 | Motor vehicle accidents, falls and sport injuries | No | No | Hospitalized without intervention | 1 and 6 months | Information booklet provision | Cognitive and behavioural | 72 hours | 1 | Provision of written information for parents and child separately | No personal contact (written information provided) | Yes | Yes | Recommend that children and parents talk about and reflect the accident | Time to relax for parents, accepting social support if necessary, provide emotional support to the children, children may talk about the event and event-related feelings, return to normal activities | Recommendation to accept social support if necessary | CIES, SCAS | – | IES (parents), DASS (parents) | + Significant time x group Effects in children's anxiety (SCAS) at the 1 month follow-up and the parental intrusion symptoms (CIES) and total PTSS (CIES) at the 6 months follow-up. | 61% |
| Poijula et al., 2001 | FIN | 89 | 13–17 | Adolescent suicide | No | No | No intervention | 6 months | Defusing and Psychological debriefing | Debriefing | 1 to 7 days | 1 to 2 | Group | Trained clinical psychologists | Possibly | Possibly | Possibly | not mentioned | Not mentioned | IES, HSIB | – | 39-item inventory by Dyregrov et al. (1999) | = No significant group differences in all outcome variables | 33% |
| Stallard et al., 2006 | GB | 158 | 7–18 | Road traffic accidents | Yes | Yes | Neutral nonaccident focused discussion | 8 months | Debriefing | Debriefing | 28 days | 1 | Child alone | Researcher (without any information about her clinical experience or formation) | Yes | Yes | Detailed reconstruction | Extraction and discussion of trauma-related thoughts and feelings, general advice for how to cope with thoughts and feelings. | Not mentioned | CAPS-C, CIES, BDI, R-MAS, SDQ | SDQ | – | = No significant group differences in all outcome variables | 88% |
| Yule et al., 1992 | GB | 24 | 14–16 | Shipping disaster | No | No | Unaffected age and sex matched school | 5 months | Group debriefing | Debriefing with problem-solving approach, based on cognitive behavioural methods | 10 days | 1 | Group | Clinical psychologist (eventually among others) | Possibly | Possibly | Possibly | Problem-solving approach to target anxiety, avoidance and intrusive thoughts | Not mentioned | IES, BDI, RMAS, Modified form of the Fear Survey Schedule for Children | – | – | + Significant group differences in intrusion (IES), overall PTSD symptoms (IES) and fears. | 26% |
| Zehnder et al., 2010 | CH | 99 | 7–16 | Road traffic accidents | Yes | Yes | No intervention | 2 and 6 months | Cognitive behavioural early intervention | Cognitive and behavioural | 10 days | 1 | One session with the child and at least one parent together | Clinical psychologist | Yes | Yes | Detailed reconstruction | Identification and support in modification of dysfunctional accident-related appraisals, provision of instructions on coping skills | Recommend providing parental security to the child throughout the acute period | IBS-P-KJ, IBS-A-KJ, DIKJ | CBCL | SES, life events, MISS | + Significant group subgroup (7-11y) differences in depression (DIKJ) and behaviour (CBCL) at 6 months follow up | 90% |
Note: BASC-2, Behaviour Assessment System for Children, Second Edition-Self Report; BDI, Birleson Depression Inventory; CAPS-C, post-traumatic stress disorder scale for children; CBCL, Child Behaviour Checklist; CIES, Children's Revised Impact of Event Scale; DASS, Depression & Anxiety Stress Scale; DIKJ, German version of the Children's Depression Inventory (CDI); HSIB, Hogan Sibling Inventory of Bereavement; IBS-A-KJ, Interview for ASD similarly to assess DSM-IV-TR acute stress disorder symptoms; IBS-P-KJ, German version of the Clinician-Administered PTSD Scale for Children and Adolescents (CAPS-CA); IES-R, The Impact of Events Scale-Revised; Kiddie-SADS-L, Semistructured interview for the diagnosis of DSM-IV childhoood mental disorders derived from the Kiddie-Schedule for Affective Disorders and Schizophrenia for School Age Children (Kiddie-SADS); MISS, Modified Injury Severity Scale; PBI, Parent Behaviour Inventory; PCL-C, PTSD Checklist-Civilian Version; PSS-Fa, Perceived Social Support-Familiy; PTSD-RI, UCLA Posttraumatic Stress Disorder Index; R-MAS, Revised Manifest Anxiety Scale; SCAS, Pence Child Anxiety Scale; SDQ, Strengths and Difficulties Questionnaire; SES, Socio-economic status; STAI-C, State-Trait Anxiety Inventory for Children; THQ, Trauma History Questionnaire; TSCC, Trauma Symptom Checklist for Children; TSCC-A, The Trauma Symptom Checklist for Children-A.
Data analyses
Whenever possible, between-group effect sizes (ES) and corresponding 95% confidence intervals (CI) at follow-up points 1 and 2 were calculated for the outcome measures. Given that different measures were used across the seven studies, standard mean differences (SMD) were used, defined as the difference between the mean of the intervention and the control group divided by the pooled standard deviation (SD) (Durlak, 2009). The latter was computed as per Lipsey and Wilson (2001). As SMDs based on small sample sizes are prone to a slight upward bias (Lipsey & Wilson, 2001), small sample size bias correction for d-type ES was calculated for all SMDs (Hedges, 1981). The statistical significance of each SMD was computed (Wilson, 2005).
To ensure that each study had only one effect size per outcome variable, in the Berkowitz, Stover, and Marans (2011) study, a mean effect size was computed from the two applied instruments that measured PTSS (TSCC and PTSD-RI). As Zehnder, Meuli, and Landolt (2010) reported significantly, different results for the two studied subgroups, the ES for these two sub-groups (7–11 years old and 12–16 years old) were entered separately into analysis. To respect the lower precision of effect size in studies with fewer subjects, a weighted mean effect size was calculated per outcome variable, using the inverse variance (Lipsey & Wilson, 2001; Wilson, 2005).
To test the assumption that any differences between ES are due to sampling error alone––and that the ES, therefore, estimate the same population effect size––a homogeneity analysis was conducted. If such an analysis is found to be significant (p Q<0.05), the null hypothesis of homogeneity must be rejected, meaning that any variability among the SMDs exceeds what can be expected from sampling error alone (Lipsey & Wilson, 2001). In the latter case, analogue-to-the ANOVA moderator analysis, while assuming a mixed effects model, was conducted (Lipsey & Wilson, 2001; Wilson, 2005). Study quality was chosen as a dichotomous moderator variable (higher/lower quality), whilst the intercept was deemed a random effect.
Given that all outcome variables in the analysed studies measured symptom severity (e.g., PTSS), any negative SMD indicates improvement in the desired direction, with the intervention group superior to controls. The magnitude of the SMD was interpreted by means of Cohen's categories for ES: 0.2–0.5, small effect; 0.5–0.8, medium effect;>0.8, large effect (Cohen, 1988).
To compare the effectiveness of higher versus lower quality studies, mean SMDs and 95% CI were calculated for all seven studies together, and separately for higher and lower quality studies.
Whenever possible, the overall number and percentage of full-blown and partial PTSD diagnoses in the intervention and control groups were calculated for follow-up times 1 and 2. Furthermore, depending on sample size, chi-square analysis or Fishers’ exact test was used to assess the statistical significance of between-group differences within each separate study and across all studies when scores were combined separately for follow-up points 1 and 2.
In the present review, the terms PTSD and PTSS were differentiated from one another. PTSS was used when addressing symptom severity (i.e., continuous PTSD symptoms) and PTSD was used when addressing either the DSM disorder, as such, or the dichotomisable DSM diagnosis of partial or full-blown PTSD.
Results
Description of studies
Study methodology and characteristics are summarised in Table 1.
Origin
Four publications were conducted in Europe, two in Australia and one in the USA.
Characteristics of the examined samples
The overall sample sizes range from 24 to 158; and the age of participants ranges from 7 to 18 years. Trauma types were very heterogeneous. Four studies included only one type of trauma, such as a classmate's suicide (Poijula, Dyregrov, Wahlberg, & Jokelainen, 2001), road traffic accident (Stallard et al., 2006; Zehnder et al., 2010) or shipping disaster (Yule, 1992). Three studies examined heterogeneous samples, including physical and sexual inter-personal assault and/or various unintentional injuries (Berkowitz et al., 2011; Cox et al., 2010; Kenardy et al., 2008).
Study design
Four publications were randomised controlled trials (RCT) (Berkowitz et al., 2011; Cox et al., 2010; Stallard et al., 2006; Zehnder et al., 2010), but only two of these were double blinded (Stallard et al., 2006; Zehnder et al., 2010).
The control groups varied greatly in their quality, with most studies using a comparison group that received no intervention. Two studies (Cox et al., 2010; Zehnder et al., 2010) allocated the children randomly to either an intervention or untreated control group. Kenardy et al. (2008) created an unmatched control group consisting of all those children who were medically treated in a hospital, where children did not receive any early psychological treatment. In the study of Poijula et al. (2001), the two schools that received no intervention were declared the control group post hoc. Yule (1992) compared two girls schools, where children had been involved in a shipping disaster. One school accepted early help from the authors and the other did not. It remained unclear if and to what extent students at the latter (control) school received any help. Only two studies compared two different intervention conditions: Berkowitz et al. (2011) provided a four-session supportive comparison condition. Stallard et al. (2006) carried out a neutral, non-accident-focused discussion about daily issues, such as friends, favourite music or sports.
The time points for follow-up ranged from one (Berkowitz et al., 2011; Cox et al., 2010; Kenardy et al., 2008) to eight (Stallard et al., 2006) months. Three studies included a single follow-up assessment (Poijula et al., 2001; Stallard et al., 2006; Yule, 1992), and four studies two follow-up assessments (Berkowitz et al., 2011; Cox et al., 2010; Kenardy et al., 2008; Zehnder et al., 2010). Most studies chose a follow-up assessment 5–6 months post-trauma (Cox et al., 2010; Kenardy et al., 2008; Poijula et al., 2001; Yule, 1992; Zehnder et al., 2010).
Interventions
Theoretical background
Most of the interventions were based on elements of behavioural and cognitive therapy (Berkowitz et al., 2011; Cox et al., 2010; Kenardy et al., 2008; Zehnder et al., 2010). Three studies used the so-called “debriefing session” as the intervention (Poijula et al., 2001; Stallard et al., 2006; Yule, 1992). Yule (1992) used as their group debriefing an adopted problem-solving approach based on cognitive behavioural methods. Poijula et al. (2001) and Stallard et al. (2006) claimed that their interventions were a modified debriefing procedure adapted from Dyregrov (1991). Kenardy et al. (2008) and Cox et al. (2010) provided written psycho-educational information that was based on cognitive behavioural and cognitive and resilience theory, respectively.
Elements of the interventions
Psycho-education. The majority of the trials used psychoeducation as an important element of the intervention (Cox et al., 2010; Kenardy et al., 2008; Stallard et al., 2006; Zehnder et al., 2010).
Trauma narrative. Stallard et al. (2006) and Zehnder et al. (2010) conducted a detailed re-construction of the traumatic event by means of a trauma narrative. Notably, Zehnder et al. (2010) used child-appropriate play material to accomplish this. It is not stated explicitly whether Poijula et al. (2001) and Yule (1992) re-constructed the traumatising event with the children, although this is usually part of the debriefing procedure (e.g., Dyregrov, 1991; Mitchell & Everly, 1993). The information provided in the studies by Cox et al. (2010) and Kenardy et al. (2008) included recommendations to children and parents to talk about the accident. However, no guided re-construction was conducted. Berkowitz et al. (2011) did not re-construct the traumatic event with the child.
Coping skills. All interventions except for that of Poijula et al. (2001) provided information and instructions on how to cope with specific trauma-related stressors. Most of them identified dysfunctional trauma-related cognitions and/or feelings in children and/or parents that were processed with cognitive-behavioural methods (Berkowitz et al., 2011; Cox et al., 2010; Stallard et al., 2006; Zehnder et al., 2010). Poijula et al. (2001) and Yule (1992) may have such techniques as well because it is part of the original debriefing procedure. However, this is not explicitly mentioned in their publications. Berkowitz et al. (2011) subsumed the coping skills within the wrap-up of the family intervention. They divided stress reactions into five areas, and corresponding skills were discussed with each child and the parents. Unfortunately, very few details on the coping skill interventions are provided in the manual (Berkowitz & Marans, 2008). One further study also suggested using relaxation techniques (Cox et al., 2010). Two authors recommended that the child should return to normal activities (Kenardy et al., 2008; Zehnder et al., 2010). Comparable to this, Cox et al. (2010) suggested that children should do pleasant things. The authors also reminded the child of his/her personal resources (Cox et al., 2010). Albeit the discussion of coping skills was usually directly addressed to the child, Cox et al. (2010) and Kenardy et al. (2008) provided coping skills for parental distress.
Social support. The main aim of the intervention by Berkowitz et al. (2011) was to improve the communication between the child and parents. Three other studies also picked social support as the central issue. Cox et al. (2010) emphasised the parent's role in the child's recovery, whereas Kenardy et al. (2008) suggested that parents accept external social support, if necessary. Zehnder et al. (2010) recommended that the parents and child seek social support to cope with acute stress reactions, whereas the parents additionally were instructed how to support their child in general.
Age
All interventions focused on children 6–18 years old; the vast majority of the studies provided interventions that were not adapted to the child's developmental stage. Only the intervention offered by Cox et al. (2010) and Kenardy et al. (2008) addressed two different age groups. The wording of the information provided was adjusted to the child's cognitive ability and reading skills.
Time line for treatment
The first intervention session was held from 1 day to 1 month posttrauma. Stallard et al. (2006) and Berkowitz et al. (2011) started their intervention not later than day 28 and 30, respectively. No information regarding the mean duration or SD for this sizeable time span is available. However, the four sessions of Berkowitz et al. (2010) were completed within 28.9 days (SD=12.87 days).
Number of sessions
Three of the five studies in which a face-to-face intervention was provided consisted of a single session (Stallard et al., 2006; Yule, 1992; Zehnder et al., 2010). Poijula et al. (2001) provided one or two and Berkowitz et al. (2011) four sessions. It remains unclear how many of the individuals in the former study received two sessions. For the web-based intervention offered by Cox et al (2010), the number of website accesses by the participants was not registered. However, the participants had access to the information 2 weeks post-trauma until the third assessment time point after 6 months (Cox et al., 2010). The information brochure handed out by Kenardy et al. (2008) was read by 97% of the parents and by 83% of the children in the intervention group. It was not recorded whether the leaflet was read more than once.
Setting
The family members attending the intervention sessions varied between studies. Berkowitz et al. (2011) conducted their sessions with the child and the caregiver separately as well as together. Zehnder et al. (2010) held a single conjoint session with the child and at least one parent. The written information used in the studies of Cox et al (2010) and Kenardy et al. (2008) was provided to parents and children separately, without face-to-face contact. The two studies with several children involved in the same disaster used a group format (Poijula et al., 2001; Yule, 1992). Stallard et al. (2006) used an individual format with the child alone participating in the intervention.
Lead professional
The intervention usually was provided by clinically experienced professionals, such as master- or doctoral-level psychologists (Berkowitz et al., 2011; Poijula et al., 2001; Yule, 1992; Zehnder et al., 2010). Only the intervention in Stallard et al. (2006) was provided by a researcher, whose clinical experience and education are not stated. The psycho-educational intervention offered by Cox et al. (2010) and Kenardy et al. (2008) was not delivered personally, but in written form.
Methodological quality assessment
The study quality ranged from 26% to 90% (see Table 1). Four studies reached higher quality with percentages above the mean of 66% (Berkowitz et al., 2011; 81%; Cox et al., 2010; 82%; Stallard et al., 2006; 88%; Zehnder et al., 2010; 90%) and three studies were of lower quality with ratings below this mean (Kenardy et al., 2008; 61%; Poijula et al., 2001; 33%; Yule, 1992; 26%).
Although all seven studies used reliable and valid measures of change with good psychometric properties, few studies assessed parameters using multi-modal measures (Berkowitz et al., 2011; Stallard et al., 2006; Zehnder et al., 2010) and by involving different informants (Zehnder et al., 2010). Potential confounders were controlled in just three studies (Berkowitz et al., 2011; Stallard et al., 2006; Zehnder et al., 2010). There was no clearly defined population and an inadequate randomisation, primarily in the three studies with the lowest quality scores (Kenardy et al., 2008; Poijula et al., 2001; Yule, 1992). These studies also used qualitatively poor control groups. Only two studies were double blinded (Stallard et al., 2006; Zehnder et al., 2010). An a priori power calculation to estimate the required sample size was conducted for only two studies (Cox et al., 2010; Zehnder et al., 2010). Only Berkowitz et al. (2011) checked treatment fidelity independently.
Effectiveness of interventions
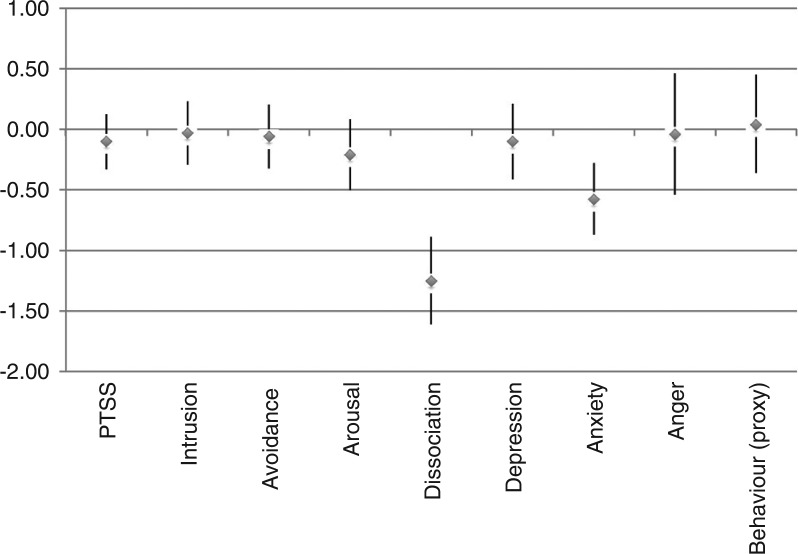
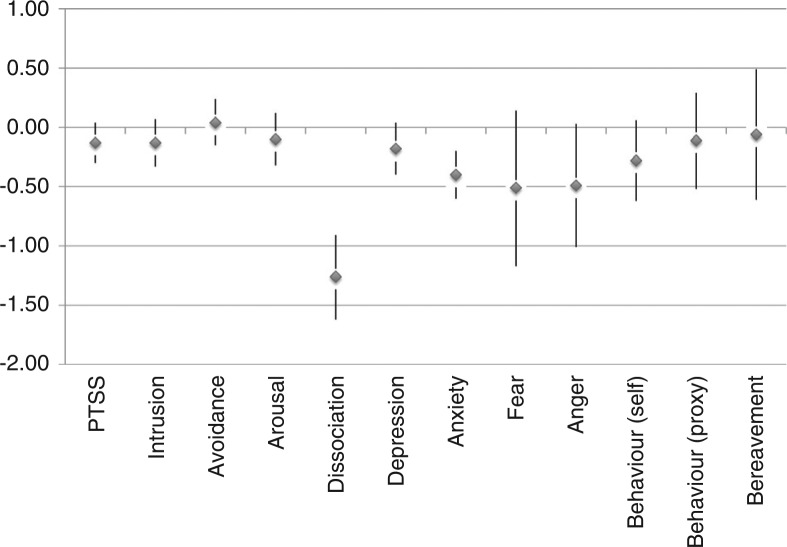
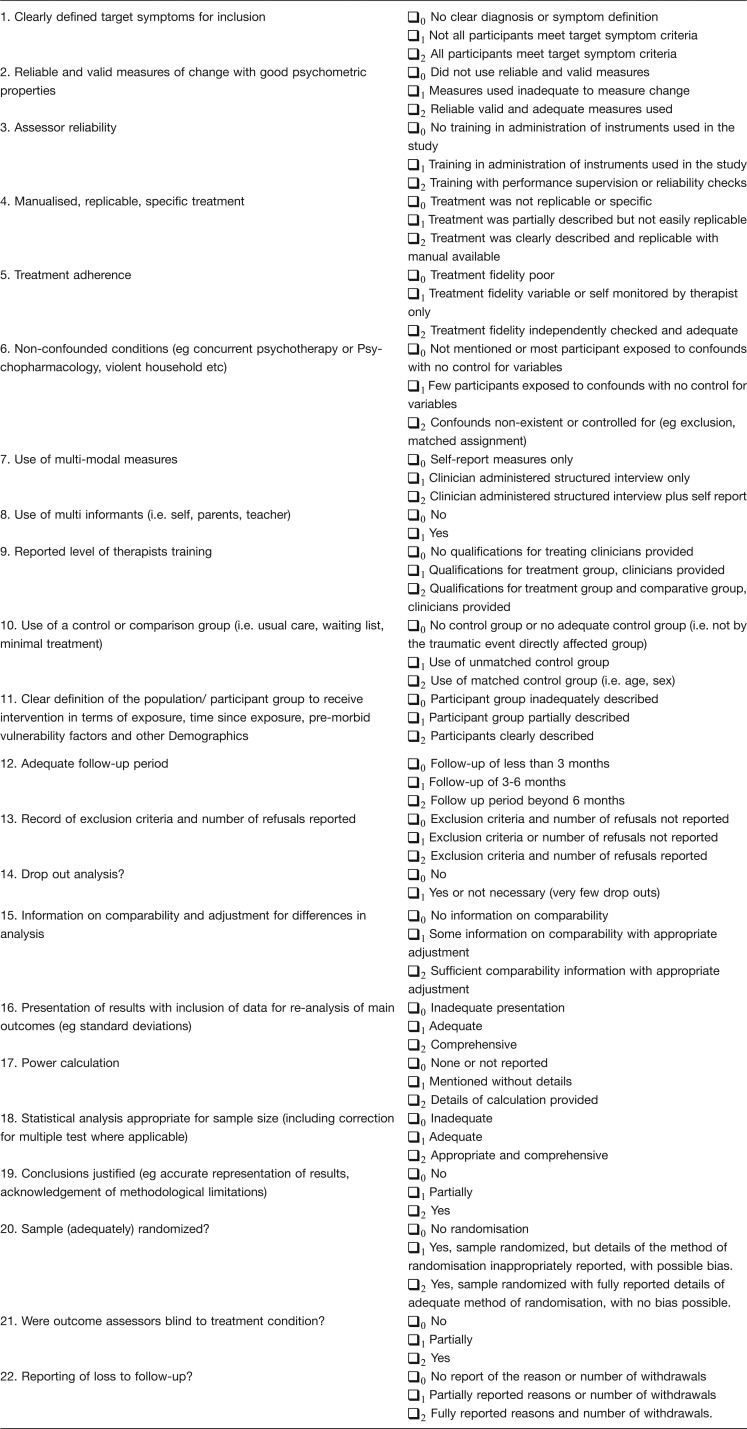
Table 2 shows the between-group SMDs and 95% CI for all available outcome variables at the follow-up time points 1 and 2. For each follow-up, only studies with available data for the respective time point were listed. Fig. 3 and Fig. 4 visually illustrate the distribution of the mean SMDs and the corresponding 95% CI. The incident rates of PTSD are presented in Table 3, including the test of between-group significance.
Table 2.
Between-group standardised mean differences (SMDs)
| f/u 1 (<3 to 8 months) | Post-traumatic stress symptoms | Intrusion | Avoidance | ||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Authors, year | f/u time point | n (Intervention) | n (Control) | SMD | CI | p | Measure | n (Intervention) | n (Control) | SMD | CI | p | Measure | n (Intervention) | n (Control) | SMD | CI | p | Measure | ||||||
| Berkowitz et al. (2011) | Up to 2 months | 48 | 48 | −0.71 | −1.12 | to | −0.30 | n.s. | TSCC,PTSD-RI | 42 | 42 | −0.41 | −0.84 | to | .03 | n.s. | PTSD-RI | 42 | 42 | −50 | −93 | to | −0.06 | <.05 | PTSD-RI |
| Cox et al. (2010) | 4–6 weeks | 30 | 32 | 0.11 | −0.39 | to | 0.60 | n.s. | TSCC-A | to | to | ||||||||||||||
| Kenardy et al. (2010) | 1 month | 16 | 36 | 0.24 | −0.35 | to | 0.83 | n.s. | CIES | 17 | 37 | 0.15 | −0.43 | to | 0.72 | n.s. | CIES | 16 | 36 | 0.18 | −0.41 | to | 0.77 | n.s. | CIES |
| Zehnder et al. (2010) (Subgroup 7–11 years) | 2 months | 22 | 28 | 0.27 | −0.29 | To | 0.83 | n.s. | CAPS-CA | 22 | 28 | 0.36 | −0.20 | to | 0.92 | n.s. | CAPS | 22 | 27 | 0.22 | −0.35 | to | 0.78 | n.s. | CAPS |
| Zehnder et al. (2010) (Subgroup 12–16 years) | 2 months | 27 | 22 | .05 | −0.51 | to | 0.62 | n.s. | CAPS-CA | 27 | 22 | 0.06 | −0.51 | to | 0.62 | n.s. | CAPS | 27 | 22 | 0.18 | −0.39 | to | 0.74 | n.s. | CAPS |
| Total | 143 | 166 | −10 | −0.33 | to | 0.12 | n.s. | Q:sign | 108 | 129 | −0.03 | −0.29 | to | 0.23 | n.s. | Q: n.s. | 107 | 127 | −0.06 | −0.32 | to | 0.20 | n.s. | Q: n.s. | |
|
| |||||||||||||||||||||||||
| f/u 1 (<3 to 8 months) | Arousal | Dissociation | Depression | ||||||||||||||||||||||
| Authors, year | f/u time point | n (Intervention) | n (Control) | SMD | CI | p | Measure | n (Intervention) | n (Control) | SMD | CI | p | Measure | n (Intervention) | n (Control) | SMD | CI | p | Measure | ||||||
|
| |||||||||||||||||||||||||
| Berkowitz et al. (2011) | Up to 2 months | 42 | 42 | −0.48 | −0.91 | to | −0.04 | <.05 | PTSD-RI | 53 | 53 | −2.57 | −3.08 | to | −2.05 | <.01 | TSCC | ||||||||
| Cox et al. (2010) | 4–6 weeks | 30 | 32 | −0.01 | −0.51 | to | 0.49 | n.s | TSCC-A | 30 | 32 | 0.09 | −0.40 | to | 0.59 | n.s. | TSCC-A | ||||||||
| 2008) | 1 month | ||||||||||||||||||||||||
| Zehnder et al. (2008) (Subgroup 7–11 years) | 2 months | 22 | 28 | 0.08 | −0.48 | to | 0.64 | n.s. | CAPS | 22 | 28 | −0.53 | −1.10 | to | 0.03 | n.s. | CDI | ||||||||
| Zehnder et al. (2010) (Subgroup 12–16 years) | 2 months | 27 | 22 | −0.05 | −0.62 | to | 0.51 | n.s. | CAPS | 27 | 22 | 0.09 | −0.48 | to | 0.65 | n.s. | CDI | ||||||||
| Total | 91 | 92 | −0.21 | −0.50 | to | 0.08 | n.s. | Q: n.s. | 83 | 85 | −1.25 | −1.61 | to | −0.89 | <0.001 | Q: sign | 79 | 82 | −0.10 | −0.41 | to | 0.21 | n.s. | Q: n.s. | |
|
| |||||||||||||||||||||||||
| f/u 1 (<3 to 8 months) | Anxiety | Anger | Behaviour (Proxy reported) | ||||||||||||||||||||||
| Authors, year | f/u time point | n (Intervention) | n (Control) | SMD | CI | p | Measure | n (Intervention) | n (Control) | SMD | CI | p | Measure | n (Intervention) | n (Control) | SMD | CI | p | Measure | ||||||
|
| |||||||||||||||||||||||||
| Berkowitz et al. (2011) | Up to 2 months | 53 | 53 | −3.44 | −4.04 | to | −2.84 | <.01 | TSCC | ||||||||||||||||
| Cox et al. (2010) | 4–6 weeks | 30 | 32 | 0.32 | −0.18 | to | 0.82 | n.s. | TSCC-A | 30 | 32 | −0.04 | −0.54 | to | 0.46 | n.s. | TSCC-A | ||||||||
| Kenardy et al. (2008) | 1 month | 28 | 56 | 0.35 | −0.11 | to | 0.80 | n.s. | SCAS | ||||||||||||||||
| Zehnder et al. (2010) (Subgroup 7–11 years) | 2 months | 22 | 28 | −0.46 | to | 0.10 | n.s. | CBCL | |||||||||||||||||
| Zehnder et al. (2010) (Subgroup 12–16 years) | 2 months | 27 | 22 | 0.57 | −0.01 | to | 1.14 | n.s. | CBCL | ||||||||||||||||
| Total | 111 | 141 | −0.58 | −0.87 | to | −0.28 | <.001 | Q: Sign | 30 | 32 | −0.04 | −0.54 | to | 0.46 | n.s. | Q: – | 49 | 50 | 0.04 | −0.36 | to | 0.45 | n.s. | Q: Sign | |
|
| |||||||||||||||||||||||||
| f/u 2 (<3 to 8 months) | Post-traumatic stress symptoms | Intrusion | Avoidance | ||||||||||||||||||||||
| Authors, year | f/u time point | n (Intervention) | n (Control) | SMD | CI | p | Measure | n (Intervention) | n (Control) | SMD | CI | P | Measure | n (Intervention) | n (Control) | SMD | CI | P | Measure | ||||||
|
| |||||||||||||||||||||||||
| Berkowitz et al. (2011) | 3 months | 48 | 47 | −0.72 | −1.14 | to | −0.31 | <.01 | TSCC, PTSD-RI | 42 | 41 | −0.64 | −1.08 | to | −0.20 | <.01 | PTSD-RI | 42 | 41 | −0.47 | −0.90 | to | −0.03 | <0.05 | PTSD-RI |
| Cox et al. (2010) | 6 months | 31 | 28 | −0.13 | −0.64 | to | 0.38 | n.s. | TSCC-A | ||||||||||||||||
| Kenardy et al. (2008) | 6 months | 17 | 37 | 0.87 | 0.27 | to | 1.47 | <.01 | CIES | 16 | 36 | 0.65 | 0.05 | to | 1.25 | <.05 | CIES | 17 | 37 | 0.81 | 0.22 | to | 1.14 | <0.01 | CIES |
| 2001) | 6 months | 55 | 32 | 0.00 | −0.44 | to | 0.44 | n.s. | IES | to | |||||||||||||||
| 2006) | 8 months | 70 | 62 | −0.08 | −0.42 | to | 0.26 | n.s. | CIES | 70 | 62 | −0.05 | −0.39 | to | 0.30 | n.s. | CIES | 70 | 62 | 0.01 | −0.33 | to | 0.35 | n.s. | CIES |
| Yule et al. (1992) | 5 months | 24 | 15 | −1.00 | −1.68 | to | −0.31 | <.01 | IES | 24 | 15 | −0.97 | −165 | to | −0.29 | <.01 | IES | 24 | 15 | −0.60 | 1.26 | to | 0.05 | n.s. | IES |
| Zehnder et al. (2010) (Subgroup 7–11 years) | 6 months | 22 | 28 | −0.01 | −0.57 | to | 0.55 | n.s. | CAPS-CA | 22 | 28 | −0.07 | −0.63 | to | 0.49 | n.s. | CAPS | 22 | 27 | 0.08 | −0.48 | to | 0.65 | n.s. | CAPS |
| Zehnder et al. (2010) (Subgroup 12–16 years) | 6 months | 27 | 22 | 0.22 | −0.35 | to | 0.78 | n.s. | CAPS-CA | 27 | 22 | 0.33 | −0.24 | to | 0.89 | n.s. | CAPS | 27 | 22 | 0.09 | −0.47 | to | 0.66 | n.s. | CAPS |
| Total | 294 | 271 | −0.13 | −0.30 | to | 0.04 | n.s. | Q: Sign | 201 | 204 | −0.13 | −0.33 | to | 0.07 | n.s. | Q: Sign | 202 | 204 | −0.04 | −0.23 | to | 0.16 | n.s. | Q: Sign | |
|
| |||||||||||||||||||||||||
| f/u 2 (<3 to 8 months) | Arousal | Dissociation | Depression | ||||||||||||||||||||||
| Authors, year | f/u time point | n (Intervention) | n (Control) | SMD | CI | p | Measure | n (Intervention) | n (Control) | SMD | CI | P | Measure | n (Intervention) | n (Control) | SMD | CI | P | Measure | ||||||
|
| |||||||||||||||||||||||||
| Berkowitz et al. (2011) | 3 months | 42 | 40 | −0.36 | −0.79 | to | 0.08 | n.s. | PTSD-RI | 53 | 53 | −2.22 | −2.71 | to | −1.74 | <.01 | TSCC | ||||||||
| Cox et al. (2010) | 6 months | 31 | 28 | −0.19 | −0.70 | to | 0.32 | n.s. | TSCC-A | 31 | 28 | −0.15 | −0.66 | to | 0.37 | n.s. | TSCC-A | ||||||||
| Kenardy et al. (2008) | 6 months | ||||||||||||||||||||||||
| Poijula et al. (2001) | 6 months | ||||||||||||||||||||||||
| Stallard et al. (2006) | 8 months | 70 | 62 | −0.05 | −0.39 | to | 0.29 | n.s. | CIES | 70 | 62 | −0.16 | −0.51 | to | 0.18 | n.s. | BDI | ||||||||
| Yule et al. (1992) | 5 months | 24 | 15 | −0.26 | −0.91 | to | 039 | n.s. | BDI | ||||||||||||||||
| Zehnder et al. (2010) (Subgroup 7–11 years) | 6 months | 22 | 28 | −0.04 | −0.60 | to | 0.52 | n.s. | CAPS | 22 | 28 | −0.69 | −1.26 | to | −0.11 | <0.5 | CDI | ||||||||
| Zehnder et al. (2010) (Subgroup 12–16 years) | 6 months | 27 | 22 | 0.15 | −0.41 | to | 0.72 | n.s. | CAPS | 27 | 22 | 0.26 | −0.30 | to | 0.83 | n.s. | CDI | ||||||||
| Total | 161 | 152 | −0.10 | −0.32 | to | 0.12 | n.s. | Q: n.s. | 84 | 81 | −1.26 | −1.62 | to | −0.91 | <.001 | Q: Sign | 174 | 155 | −0.18 | −0.40 | to | 0.04 | n.s. | Q: n.s. | |
|
| |||||||||||||||||||||||||
| f/u 2 (<3 to 8 months) | Anxiety | Fear | Anger | ||||||||||||||||||||||
| Authors, year | f/u time point | n (Intervention) | n (Control) | SMD | CI | p | Measure | n (Intervention) | n (Control) | SMD | CI | P | Measure | n (Intervention) | n (Control) | SMD | CI | P | Measure | ||||||
|
| |||||||||||||||||||||||||
| Berkowitz et al. (2011) | 3 months | 53 | 53 | −1.59 | −2.03 | to | −1.15 | <.01 | TSCC | ||||||||||||||||
| Cox et al. (2010) | 6 months | 31 | 28 | −0.21 | −0.72 | to | 0.30 | n.s. | TSCC-A | 31 | 28 | −0.49 | −1.01 | to | 0.03 | n.s. | TSCC-A | ||||||||
| Kenardy et al. (2008) | 6 months | 28 | 56 | 0.03 | −0.43 | to | 0.48 | n.s. | SCAS | ||||||||||||||||
| Poijula et al. (2001) | 6 months | ||||||||||||||||||||||||
| Stallard et al. (2006) | 8 months | 70 | 62 | −0.08 | −0.42 | to | 0.27 | n.s. | R-MAS | ||||||||||||||||
| Yule et al. (1992) | 5 months | 24 | 15 | −0.09 | −0.73 | to | 0.56 | n.s | R-MAS | 24 | 15 | −0.51 | −1.17 | to | 0.14 | n.s. | Fear survey schedule for children | ||||||||
| Zehnder et al. (2010) (Subgroup 7–11 years) | 6 months | ||||||||||||||||||||||||
| Zehnder et al. (2010) (Subgroup 12–16 years) | 6 months | ||||||||||||||||||||||||
| Total | 206 | 214 | −0.40 | −0.60 | to | −0.20 | <.001 | Sign | 24 | 15 | −0.51 | −1.17 | to | 0.14 | n.s. | – | 31 | 28 | −0.49 | −1.01 | to | 0.03 | n.s. | − | |
|
| |||||||||||||||||||||||||
| f/u 2 (<3 to 8 months) | Behaviour (self-reported) | Behaviour (proxy reported) | Bereavement | ||||||||||||||||||||||
| Authors, year | f/u time point | n (Intervention) | n (Control) | SMD | CI | p | Measure | n (Intervention) | n (Control) | SMD | CI | P | Measure | n (Intervention) | n (Control) | SMD | CI | P | Measure | ||||||
|
| |||||||||||||||||||||||||
| Berkowitz et al. (2011) | 3 months | ||||||||||||||||||||||||
| Cox et al. (2010) | 6 months | ||||||||||||||||||||||||
| Kenardy et al. (2008) | 6 months | ||||||||||||||||||||||||
| Poijula et al. (2001) | 6 months | 43 | 18 | −0.06 | −0.6 | to | 0.49 | n.s. | HSIB | ||||||||||||||||
| Stallard et al. (2006) | 8 months | 70 | 62 | −0.28 | −0.62 | to | 0.06 | n.s. | SDO | ||||||||||||||||
| Yule et al. (1992) | 5 months | ||||||||||||||||||||||||
| Zehnder et al. (2010) (Subgroup 7–11 y) | 6 months | 22 | 28 | −0.69 | −1.27 | to | −0.12 | <.05 | CBCL | ||||||||||||||||
| Zehnder et al. (2010) (Subgroup 12–16 y) | 6 months | 27 | 22 | 0.46 | −0.11 | to | 1.03 | n.s. | CNCL | ||||||||||||||||
| Total | 70 | 62 | −0.28 | −0.62 | to | 0.06 | n.s. | Q: – | 49 | 50 | −0.11 | −0.52 | to | 0.29 | n.s. | Q: Sign | 43 | 18 | −0.06 | −0.61 | to | 0.49 | n.s. | Q: – | |
BDI, Birleson Depression Inventory; CAPS-CA, post-traumatic stress disorder scale for children and adolescents; CBCL, Child Behaviour Checklist; CDI, Children's depression inventory; CIES, Children's Revised Impact of Event Scale; DIKJ, German version of the Children's depression inventory (CDI); HSIB, Hogan Sibling Inventory of Bereavement; IBS-P-KJ, German version of the Clinician-Administered PTSD Scale for Children and Adolescents (CAPS-CA); IES, The Impact of Events Scale.
Fig. 3.
Mean SMD and 95% CI at follow-up 1.
Fig. 4.
Mean SMD and 95% CI at follow-up 2.
Table 3.
Rates of incident post-traumatic stress disorder (PTSD)
| Study | PTSD diagnosis | n (EG) | n (CG) | n | Time point after accident | Intervention group (%) | Control group (%) | Total (%) | Test of between-group significance | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Full | 53 | 53 | 106 | 1 month (Baseline) | 23 | 43.4 | 21 | 39.6 | 44 | 41.5 | χ2=0.155; df =1; p (2-tail)=0.693 (n.s.) | |
| Berkowitz et al. (2010) | Partial | 53 | 53 | 106 | 1 month (Baseline) | 14 | 26.4 | 10 | 18.9 | 24 | 22.6 | χ2=0.862; df =1; p (2-tail)=0.353 (n.s.) |
| Full | 30 | 58 | 88 | 1 month | 0 | 0.0 | 2 | 3.4 | 2 | 2.3 | Fishers’ exact: p (2-tail)=0.545 (n.s.) | |
| Kenardy et al. (2008) | Partial | 30 | 58 | 88 | 1 month | 3 | 10.0 | 8 | 13.8 | 11 | 12.5 | Fishers’ exact: p (2-tail)=0.743 (n.s.) |
| Full | 82 | 76 | 158 | 4 weeks | 19 | 23.2 | 27 | 35.5 | 46 | 29.1 | χ2=2.918; df =1; p (2-tail)=0.088 (n.s.) | |
| Stallard et al. (2006) | Partial | – | – | – | – | – | – | – | – | – | – | – |
| Full | 49 | 50 | 99 | 2 months | 6 | 12.2 | 1 | 2.0 | 7 | 7.1 | Fishers’ exact: p (2-tail)=0.059 (n.s.) | |
| Zehnder et al. (2010) | Partial | 49 | 50 | 99 | 2 months | 2 | 4.1 | 5 | 10.0 | 7 | 7.1 | Fishers’ exact: p (2-tail)=0.436 (n.s.) |
| Full | 214 | 237 | 451 | 1–2 months | 48 | 22.4 | 51 | 21.5 | 99 | 22.0 | χ2=0.054; df =1; p (2-tail)=0.815 (n.s.) | |
| Total | Partial | 132 | 161 | 293 | 1–2 months | 19 | 14.4 | 23 | 14.3 | 42 | 14.3 | χ2=0.001; df =1; p (2-tail)=1.000 (n.s.) |
| Study | PTSD diagnosis | n (EG) | n (CG) | n | Time point after accident | Intervention group (%) | Control group (%) | Total (%) | Test of between-group significance | |||
| Full | 53 | 53 | 106 | 3 months | 7 | 13.2 | 15 | 28.3 | 22 | 20.8 | χ2=3.671; df =1; p (2-tail)=0.055 (n.s.) | |
| Berkowitz et al. (2010) | Partial | 53 | 53 | 106 | 3 months | 10 | 18.9 | 15 | 28.3 | 25 | 23.6 | χ2=1.309; df=1; p (2-tail)=0.253 (n.s.) |
| Full | 24 | 50 | 74 | 6 months | 0 | 0.0 | 1 | 2.0 | 1 | 1.4 | Fishers' exact: p (2-tail)=1.000 (n.s.) | |
| Kenardy et al. (2008) | Partial | 24 | 50 | 74 | 6 months | 3 | 12.5 | 13 | 26.0 | 16 | 21.6 | Fishers’ exact: p (2-tail)=0.238 (n.s.) |
| Full | 70 | 62 | 132 | 8 months | 10 | 14.3 | 7 | 11.3 | 17 | 12.9 | χ2=0.263; df =1; p (2-tail)=0.608 (n.s.) | |
| Stallard et al. (2006) | Partial | – | – | – | – | – | – | – | – | – | – | – |
| Full | 49 | 50 | 99 | 6 months | 4 | 8.2 | 0 | 0.0 | 4 | 4.0 | Fishers’ exact: p (2-tail)=0.056 (n.s.) | |
| Zehnder et al. (2010) | Partial | 49 | 50 | 99 | 6 months | 4 | 8.2 | 5 | 10.0 | 9 | 9.1 | Fishers’ exact: p (2-tail)=1.000 (n.s.) |
| Full | 196 | 215 | 411 | 3– months | 21 | 10.7 | 23 | 10.7 | 44 | 10.7 | χ2=0.000; df =1; p (2-tail)=1.000 (n.s.) | |
| Total | Partial | 126 | 153 | 279 | 3–7 months | 17 | 13.5 | 33 | 21.6 | 50 | 17.9 | χ2=3.064; df =1; p (2-tail)=0.080 (n.s.) |
For between-group comparisons, heterogeneity analyses revealed significant heterogeneity for the included SMDs in terms of PTSS, dissociation, anxiety and proxy-reported behaviour at follow-up points 1 and 2 and for avoidance at follow-up 2 (see Q in Table 2). Applying analogue-to-the ANOVA moderator analysis, no significant differences between the SMDs of lower and higher quality studies could be identified for any outcome variable. Therefore, these results are not presented.
The mean overall ES for the outcome measures ranged from 0.04 to −1.26. Notably, none of the means indicated any harmful overall effects. The CI of the averaged mean SMDs mostly included zero and, therefore, did not reach significance. However, the vast majority of the CI were negative, indicating a trend towards a beneficial effect.
Dissociation, arousal and anxiety exhibited the largest overall effects, ranging from small (−0.21) to large (−1.26). Out of all the outcome variables, only dissociation and anxiety achieved statistical significance, implying positive interventional effects. It is noteworthy that the study by Berkowitz et al. (2011) contributed most to the beneficial effects of early intervention for dissociation and anxiety. Even though fear, anger and self-reported behaviour also revealed positive, but small effects, these SMDs were based on a single study and, as such, cannot be interpreted as mean overall effects.
Although the overall intervention effects for depression and proxy-reported behaviour were negligible, the single ES identified by Zehnder et al. (2010) suggest that their intervention was more helpful for younger (7–11 years of age) versus older children (12–16 years of age). By contrast, for PTSS, at follow-up 2, the data from Kenardy et al. (2008) suggest an unfavourable effect. Notably, these highly positive SMDs (i.e., PTSS at follow-up 2: SMD=0.87, 95% CI=0.27 to 1.47; p<0.01) are due to different levels at baseline. However, in both the control and intervention group, PTSS decreased over time, with the control group recovering more quickly (Kenardy et al., 2008). Only four authors provided data for full-blown and partial PTSD (Berkowitz et al., 2011; Kenardy et al., 2008; Stallard et al., 2006; Zehnder et al., 2010). There were no significant overall between-group effects (see Table 3).
Taken together, dissociation and anxiety are the areas for which the greatest and most significant mean intervention effects were observed. In general, the overall SMDs at both follow-up time points indicate beneficial but generally small effects of early interventions, ranging from 0.04 to −1.26, with the majority between −0.10 and −0.60. The 95% CI vary widely, ranging from negative to positive. However, most of the 95% CI lie in the negative range. Heterogeneity analysis revealed that the degree of variety between the single ES, which were averaged into these mean SMDs, might not estimate the same population mean ES. In the same way, the analogue-to-the ANOVA analysis could not uncover the source of this variability such as random effects or a moderator-like study quality.
Discussion
Type of intervention
Theoretical base
There is little variety regarding the theoretical base of the studies we analysed, as half of the studies were categorised as either “behavioural and cognitive” (Berkowitz et al., 2011; Cox et al., 2010; Kenardy et al., 2008; Zehnder et al., 2010) or an adapted debriefing procedure (Poijula et al., 2001; Stallard et al., 2006; Yule, 1992). Due to the very superficial description of the theoretical backgrounds, the studies cannot be compared in this regard.
Content
While some interventions included narrative exposure as an important component (Cox et al., 2010; Yule, 1992; Zehnder et al., 2010), the study by Berkowitz et al. (2011) did not. Beneficial effects were reported for both types of studies. Therefore, it is unclear to what extent a trauma narrative should be part of early intervention.
Presumably, all studies provided psycho-education. However, Cox et al. (2010) and Kenardy et al. (2008) were the only investigators whose intervention focused exclusively on information provision. Because both studies reported a significant reduction in anxiety, psycho-education seems to be an effective component of early interventions.
The vast majority of studies included individually provided coping skills, although most authors failed to report how they were taught. With respect to specific kinds of coping skills, such as general versus symptom specific coping skills, no pattern of effectiveness could be found among the studies. Hence, it remains unclear to what extent coping-skill-directed interventions are helpful for a traumatised child's recovery.
Setting
The greater proportion of interventions addressed both the child and the caregiver. All yielded beneficial effects for at least some outcome variables (Berkowitz et al., 2011; Cox et al., 2010; Kenardy et al., 2008) or sub-groups (Zehnder et al., 2010). Berkowitz et al. (2011) even declared improved communication between the parents and child as the core aim of their intervention. Notably, they achieved the greatest treatment effects. Among the three interventions that did not involve parents, one did yield beneficial effects (Yule, 1992), but two studies failed to do so (Poijula et al., 2001; Stallard et al., 2006). Moreover, the Yule (1992) study was the methodologically weakest study of the three. Taken together, our review suggests that involving parents may enhance the efficacy of early interventions.
With regards to when to offer some intervention, our review revealed great variability, with some interventions provided within the first few hours after trauma and others not starting for almost 1 month. No clear association between the time of initiation and effectiveness of interventions emerged.
The vast majority of studies provided a single session. In line with what is known from early psychological interventions in adults (Roberts et al., 2010b), Berkowitz's (2011) study with four sessions suggests that more sessions may increase the benefits of a particular intervention. However, this conclusion must be interpreted with caution because only one study systematically offered multiple sessions.
None of the studies included children <7 years old, although it is known that pre-school children may suffer from clinically significant PTSS after single trauma (Meiser-Stedman, Smith, Glucksman, Yule, & Dalgleish, 2008). Zehnder et al. (2010) were the only authors who reported an influence of the child's age on the effectiveness of their intervention and found it more helpful for younger children (7–11 years).
Although the information booklets of Cox et al. (2010) and Kenardy et al. (2008) used age-appropriate wording, both studies did not provide any data on this issue. In summary, there is tentative evidence for the need of more developmentally appropriate provision of early interventions.
In almost all studies, the intervention was provided to all children, irrespective of their early symptomatology. Interestingly, the study that identified the largest ES used a stepped procedure, beginning with risk screening and subsequently providing the intervention only to children deemed at appreciable risk for long-lasting PTSS (Berkowitz et al., 2011). This finding is consistent with previous studies in adults that found a stepped procedure in the early aftermath of trauma to be effective (Roberts et al., 2010b).
Effects
Of the seven studies we analysed, five identified beneficial between-group treatment effects for at least one outcome variable (Berkowitz et al., 2011; Cox et al., 2010; Kenardy et al., 2008; Yule, 1992; Zehnder et al., 2010). Notably, no study reported harmful effects. The overall between-group ES underlined these results by revealing promising beneficial tendencies with regards to dissociation, anxiety and, to some extent, arousal.
Conversely, intervention effects regarding PTSS and PTSD were small and non-significant. Therefore, early psychological interventions may not have any influence on post-traumatic stress symptoms after traumatising events. Notably, while the overall intervention effects for PTSS across all studies were small, two studies revealed medium-to-large beneficial effects (Berkowitz et al., 2011; Yule, 1992). Berkowitz et al. used a stepped procedure that may have enhanced the intervention's effects on PTSS. Meanwhile, the results of Yule (1992) must be interpreted with caution, as this study was rated lowest in quality.
The reported ES in the present review are comparable to those that were uncovered by a systematic review on the efficacy of individual trauma-focused CBT (tf-CBT) in traumatised children and adolescents (Wethington et al., 2008: ES for PTSS=0.34). Notably, only about half of the 11 studies that were analysed were randomised and controlled. Since the publication of that review, three new RCTs on this topic have been published (Cohen, Mannarino, & Iyengar, 2011; Scheeringa, Weems, Cohen, Amaya-Jackson, & Guthrie, 2011; Smith et al., 2007). The ES in these studies were considerably greater (e.g., Scheeringa et al., 2011: ES for PTSS=1.07; Smith et al., 2007: ES for PTSS=1.59). Thus, based on the current literature, established trauma therapy, such as tf-CBT, clearly seems to be more effective than early interventions.
Heterogeneity analyses revealed significant results for the SMDs for every outcome variable. Therefore, differences between the studies might extend beyond sampling error. Our initial hypothesis that study quality may explain these heterogeneities could not be confirmed by moderator analysis. Therefore, the mean SMDs presented in this review generally should be interpreted with caution.
Overall, the present meta-analysis yielded encouraging results with regards to the beneficial effects of early interventions after a single traumatic event. However, because of certain limitations in our results, we are currently not able to provide definitive answers regarding the efficacy of early psychological intervention in children and adolescents after such events. For instance, the CI of ES were wide, the methodological quality of the studies varied considerably and the significant heterogeneity that exists between the ES of single studies remains unexplained.
Methodological shortcomings of the analysed studies
The mean overall quality of the included studies was satisfactory with a large variation between studies. Most studies had methodological shortcomings. For instance, although psychometrically sound measures were used, the vast majority were self-report questionnaires. Only three studies conducted clinical interviews (Berkowitz et al., 2011; Stallard et al., 2006; Zehnder et al., 2010). Furthermore, different informants were rarely involved. Although assessors usually were trained, supplementary supervision to ensure treatment fidelity was only provided by Stallard et al. (2006). Independence of the outcome assessors by blinding was not often guaranteed. Taken together, these limitations could significantly impact the accuracy of outcome analyses. The three lower-quality studies also lacked control against possible confounders, clearly defined sample populations, adequate randomisation and appropriate control groups.
Shortcomings of this systematic review
Although each area was assessed by different measures (e.g., CDI and TSCC for depression), a single mean SMD was calculated for each area. It must be taken into consideration that, even though different measures presume to assess the same concept, they do not necessarily achieve the same result. For instance, in the present review, Berkowitz et al. (2011) assessed PTSS by means of the PTSD-RI and TSCC. The semi-structured PTSD-RI interview revealed lower SMDs than the self-reported TSCC, despite the fact that the two measures were applied to the same children.
Another common problem in research field is that of non-participants. Neither intervention studies nor systematic quality assessments are able to assess the reasons why people choose not to participate in an intervention study. For instance, one important reason for non-participation might be avoidance that, inevitably, would lead to meaningful bias.
Implications
Implications for clinical practice
Because the reviewed studies used different types of intervention, it is difficult to provide evidence-based clinical recommendations at this point. However, our findings suggest that early interventions in traumatised children should probably include age-appropriate psycho-education, the provision of individual coping skills, parental involvement and, possibly, some form of trauma exposure (trauma narrative). Furthermore, the number of sessions may play an important role in the intervention's efficacy, with more sessions being more helpful than fewer. Finally, given that most children recover without professional help (Le Brocque et al., 2010), a stepped procedure should be considered, starting by screening children to assess their risk of long-term morbidity and to provide interventions to only those children who are at risk for long-term psychological problems.
Implications for future research
Several issues should be incorporated into future research. To increase methodological quality, randomised controlled trials should be conducted, incorporating sample sizes pre-determined via a priori power analysis and including an adequate follow-up period with at least two data collection points. To better address a child's emotional and cognitive developmental stage, age-appropriate interventions should be developed and evaluated, specifically for pre-schoolers. Although the range of different types of trauma within any one sample should be minimised, across studies, investigated traumas should include different trauma types such as inter-personal physical and sexual assault and natural disasters. To improve intervention efficacy and for economic reasons, a stepped procedure should be used that includes initial screening to identify children at high risk. The intervention should be theory based and thoroughly manualised. Additionally, treatment fidelity should be monitored by an independent professional. Both descriptive data and inferential analysis are warranted (e.g., provision of means, SDs and ES with 95% CI). One should assess a variety of clinical outcomes besides PTSD, as some symptoms (e.g., depression) often co-exist in individuals after a traumatising event. Standardised and well-validated outcome measures should be both self- and proxy reported. Furthermore, control variables should be assessed––such as parental well-being and the child's pre-trauma psychological state––as they may strongly influence the development of long-term psychological maladjustment. Because most previous studies applied several interventional elements at the same time, the efficacy of single elements cannot be examined separately. Therefore, future studies also should try to disentangle the specific effects of different interventional components such as psycho-education, trauma narratives, coping skills training and the treatment of parental stress reactions.
Acknowledgements
This research was supported by a grant from the Anna Muller Grocholski Foundation. We would like to thank Professor David B. Wilson for his support regarding the meta-analytic statistics.
Appendix 1: Scoring sheet for study selection
Continuation of scoring sheet for study selection
Appendix 2: Reasons for articles to be excluded
| Study | Reason for exclusion |
|---|---|
| Austin et al., 1999 | Review |
| Bisson et al., 2004 | Adulthood |
| Brill et al., 2001 | Review |
| Bronchard et al., 2001 | Review |
| Bryant et al., 1998 | Adulthood |
| Bryant et al., 2005 | Adulthood |
| Brymer et al., 2009 | Review |
| Caffo & Belaise, 2003 | Review |
| Casswell, 1997 | Unsatisfactory methodological quality |
| Catani et al., 2009 | Typ II Trauma |
| Chapman et al., 2001 | Unsatisfactory methodological quality |
| Chemtob et al., 2002 | no brief early intervention (intervention more than 6 weeks after the event or more than 6 intervention sessions) |
| Cohen et al., 2010 | Review |
| Cohen, J., 2003 | Review |
| Espie, 2009 | no brief early intervention (intervention more than 6 weeks after the event or more than 6 intervention sessions) |
| Foa et al, 2006 | Adulthood |
| Fremont, 2004 | Review |
| Galante & Foa, 1986 | no brief early intervention (intervention more than 6 weeks after the event or more than 6 intervention sessions) |
| Giannopoulou et al., 2006 | no brief early intervention (intervention more than 6 weeks after the event or more than 6 intervention sessions) |
| Gidron et al., 2001 | Adulthood |
| Goenjian et al., 1997 | no brief early intervention (intervention more than 6 weeks after the event or more than 6 intervention sessions) |
| Grant et al., 1997 | No Intervention |
| Hoagwood, 2007 | no brief early intervention (intervention more than 6 weeks after the event or more than 6 intervention sessions) |
| Klingmann, 1987 | Unsatisfactory methodological quality |
| La Greca & Silverman, 2009 | Review |
| Litz & Maguen, 2007 | Review |
| Math et al, 2008 | no brief early intervention (intervention more than 6 weeks after the event or more than 6 intervention sessions) |
| Nagao et al., 1995 | not in english |
| Nagao et al., 2001 | not in english |
| Okuno et al, 2001 | not in english |
| Poijula et al., submitted | Unsatisfactory methodological quality |
| Poijula et al., 2001b | same sample as included study |
| Pynoos & Eth, 1986 | Unsatisfactory methodological quality |
| Pynoos & Nader, 1988 | Review |
| Rivlin, E., 1988 | Review |
| Roberts et al, 2009 | Review |
| Salcioglu & Basoglu, 2008 | No brief early intervention (intervention more than 6 weeks after the event or more than 6 intervention sessions) |
| Schreier et al., 2005 | Unsatisfactory methodological quality |
| Silverman et al., 2008 | Review |
| Stuber et al., 2002 | Unsatisfactory methodological quality |
| Vila et al., 1999 | Unsatisfactory methodological quality |
| Yule & Udwin, 1991 | Same sample as included study |
Appendix 3: Adapted quality assessment tool
For the abstract or full text in other languages, please see Supplementary files under Reading Tools online
Conflict of interest and funding
There is no conflict of interest in the present study for any of the authors.
References
*Studies included in this review
- Berkowitz S. J., Marans S. R. The Child and Family Traumatic Stress Intervention, version 5. unbublished; 2008. [Google Scholar]
- * Berkowitz S. J., Stover C. S., Marans S. R. The child and family traumatic stress intervention: Secondary prevention for youth at risk of developing PTSD. Journal of Child Psychology and Psychiatry. 2011;52(6):676–685. doi: 10.1111/j.1469-7610.2010.02321.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioural sciences. 2nd ed. Hillsdale, NJ: Lawrence Erlbaum Associates; 1988. [Google Scholar]
- Cohen J. A., Mannarino A. P., Iyengar S. Community treatment of posttraumatic stress disorder for children exposed to intimate partner violence: A randomized controlled trial. Archives of Pediatrics & Adolescent Medicine. 2011;165(1):16–21. doi: 10.1001/archpediatrics.2010.247. [DOI] [PubMed] [Google Scholar]
- Copeland W. E., Keller G., Angold A., Costello E. J. Traumatic events and posttraumatic stress in childhood. Archives of General Psychiatry. 2007;64:577–584. doi: 10.1001/archpsyc.64.5.577. [DOI] [PubMed] [Google Scholar]
- * Cox C. M., Kenardy J. A., Hendrikz J. K. A randomized controlled trial of a web-based early intervention for children and their parents following unintentional injury. Journal of Pediatric Psychology. 2010;35(6):581–592. doi: 10.1093/jpepsy/jsp095. [DOI] [PubMed] [Google Scholar]
- Durlak J. A. How to select, calculate, and interpret effect sizes. Journal of Pediatric Psychology. 2009;34(9):917–928. doi: 10.1093/jpepsy/jsp004. [DOI] [PubMed] [Google Scholar]
- Dyregrov A. Grief in children: A handbook for adults. London: Jessica Kingsley; 1991. [Google Scholar]
- Essau C. A., Conradt J., Petermann F. Häufigkeit der posttraumatischen Belastungsstörung bei Jugendlichen: Ergebnisse der Bremer Jugendstudie. [Frequency of posttraumatic stress disorder in adolescents: Results of the Bremen Youth Study] Zeitschrift für Kinder- und Jugendpsychiatrie und Psychotherapie. 1999;27:37–45. doi: 10.1024//1422-4917.27.1.37. [DOI] [PubMed] [Google Scholar]
- Giaconia R. M., Reinherz H. Z., Silverman A. B., Pakiz B., Frost A. K., Cohen E. Traumas and posttraumatic stress disorder in a community population of older adolescent. Journal of the American Academy of Child and Adolescent Psychiatry. 1995;34:1369–1380. doi: 10.1097/00004583-199510000-00023. [DOI] [PubMed] [Google Scholar]
- Hedges L. V. Distribution theory for glass's estimator of effect size and related estimators. Journal of Educational Statistics. 1981;6:107–128. [Google Scholar]
- Kahana S. Y., Feeny N. C., Youngstrom E. A. Posttraumatic stress in youth experiencing illnesses and injuries: An exploratory meta-analysis. Traumatology. 2006;12:148–161. [Google Scholar]
- *Kenardy J. A., Thompson K., Le Brocque R., Olsson K. Information-provision intervention for children and their parents following pediatric accidental injury. European Child & Adolescent Psychiatry. 2008;17(5):316–325. doi: 10.1007/s00787-007-0673-5. [DOI] [PubMed] [Google Scholar]
- Kronenberg M. E., Hansel T. C., Brennan A. M., Osofsky H. J., Osofsky J. D., Lawrason B. Children of Katrina: Lessons learned about postdisaster symptoms and recovery patterns. Child Development. 2010;81(4):1241–1259. doi: 10.1111/j.1467-8624.2010.01465.x. [DOI] [PubMed] [Google Scholar]
- Le Brocque R. M., Hendrikz J., Kenardy J. A. The course of posttraumatic stress in children: Examination of recovery trajectories following traumatic injury. [Research Support, Non-U.S. Govt] Journal of Pediatric Psychology. 2010;35(6):637–645. doi: 10.1093/jpepsy/jsp050. Epub 2009 Jun 2017. [DOI] [PubMed] [Google Scholar]
- Lipsey M. W., Wilson D. B. Practical meta-analysis. Thousand Oaks: Sage; 2001. [Google Scholar]
- Meiser-Stedman R., Smith P., Glucksman E., Yule W., Dalgleish T. The posttraumatic stress disorder diagnosis in preschool- and elementary school-age children exposed to motor vehicle accidents. American Journal of Psychiatry. 2008;165:1326–1337. doi: 10.1176/appi.ajp.2008.07081282. [DOI] [PubMed] [Google Scholar]
- Mitchell J. T., Everly G. S. Critical incident stress debriefing: An operations manual for the prevention of trauma among emergency service and disaster workers. Baltimore: Chevron Publishing; 1993. [Google Scholar]
- Perkonigg A., Pfister H., Stein M. B., Höfler M., Lieb R., Maercker A., et al. Longitudinal course of posttraumatic stress disorder and posttraumatic stress disorder symptoms in a community sample of adolescents and young adults. American Journal of Psychiatry. 2005;162:1320–1327. doi: 10.1176/appi.ajp.162.7.1320. [DOI] [PubMed] [Google Scholar]
- * Poijula S., Dyregrov A., Wahlberg K. E., Jokelainen J. Reactions to adolescent suicide and crisis intervention in three secondary schools. International Journal of Emergency Mental Health. 2001;3(2):97–106. [PubMed] [Google Scholar]
- Roberts N. P., Kitchiner N. J., Kenardy J., Bisson J. Multiple session early psychological interventions for the prevention of post-traumatic stress disorder. Cochrane Database of Systematic Reviews, 4. 2010. http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=19588408. CD006869. Retrieved from. [DOI] [PubMed]
- Roberts N. P., Kitchiner N. J., Kenardy J., Bisson J. I. Early psychological interventions to treat acute traumatic stress symptoms. Cochrane Database of Systematic Reviews, 4. 2010. http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=20238359. doi:10.1002/14651858.CD007944.pub2. CD007944. Retrieved from. [DOI] [PMC free article] [PubMed]
- Rose S. C., Bisson J., Churchill R., Wessely S. Psychological debriefing for preventing post traumatic stress disorder (PTSD); Cochrane Database of Systematic Reviews, 1; 2009. CD000560. Retrieved from doi:10.1002/14651858.CD000560. [Google Scholar]
- Scheeringa M. S., Weems C. F., Cohen J. A., Amaya-Jackson L., Guthrie D. Trauma-focused cognitive-behavioral therapy for posttraumatic stress disorder in three-through six year-old children: a randomized clinical trial. Journal of child psychology and psychiatry and allied disciplines. 2011;52(8):853–860. doi: 10.1111/j.1469-7610.2010.02354.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith P., Yule W., Perrin S., Tranah T., Dalgleish T., Clark D. M. Cognitive-behavioural therapy for PTSD in children and adolescents: A preliminary randomized controlled trial. Journal of American Academy of Child and Adolescent Psychiatry. 2007;46(8):1051–1061. doi: 10.1097/CHI.0b013e318067e288. [DOI] [PubMed] [Google Scholar]
- *Stallard P., Velleman R., Salter E., Howse I., Yule W., Taylor G. A randomised controlled trial to determine the effectiveness of an early psychological intervention with children involved in road traffic accidents. Journal of child psychology and psychiatry and allied disciplines. 2006;47(2):127–134. doi: 10.1111/j.1469-7610.2005.01459.x. [DOI] [PubMed] [Google Scholar]
- Wethington H. R., Hahn R. A., Fuqua-Whitley D. S., Sipe T. A., Crosby A. E., Johnson R. L., et al. The effectiveness of interventions to reduce psychological harm from traumatic events among children and adolescents: A systematic review. American Journal of Preventive Medicine. 2008;35(3):287–313. doi: 10.1016/j.amepre.2008.06.024. [DOI] [PubMed] [Google Scholar]
- Wilson D. B. Meta-analysis macros for SAS, SPSS, and Stata; 2005. Retrieved on August 15, 2011 from. Producer. [Google Scholar]
- * Yule W. Post-traumatic stress disorder in child survivors of shipping disasters: The sinking of the Jupiter. Psychotherapy and Psychosomatics. 1992;57(4):200–205. doi: 10.1159/000288599. [DOI] [PubMed] [Google Scholar]
- *Zehnder D., Meuli M., Landolt M. A. Effectiveness of a single-session early psychological intervention for children after road traffic accidents: a randomised controlled trial. Child Adolesc Psychiatry Ment Health, 4. 2010. http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=20181120. (7). Retrieved from. [DOI] [PMC free article] [PubMed]
References
References to studies excluded from this review
- Austin L. S., Godleski L. S. Therapeutic approaches for survivors of disaster. Psychiatric Clinics of North America. 1999;22(4):897–910. doi: 10.1016/s0193-953x(05)70132-5. [DOI] [PubMed] [Google Scholar]
- Bisson J. I., Shepherd J. P., Joy D., Probert R., Newcombe R. G. Early cognitive-behavioural therapy for post-traumatic stress symptoms after physical injury. Randomised controlled trial. British Journal of Psychiatry. 2004;184:63–69. doi: 10.1192/bjp.184.1.63. [DOI] [PubMed] [Google Scholar]
- Brill C., Fiorentino N., Grant J. Covictimization and inner city youth: A review. International Journal of Emergency Mental Health. 2001;3(4):229–239. [PubMed] [Google Scholar]
- Bronchard M., Robin M., Mauriac F., Waddington A., Noirot M. N., Devynck C. A review of treatment strategies for teen-age and adult rape victims seen rapidly after the assault. Encephale. 2001;27(1):1–7. [PubMed] [Google Scholar]
- Bryant R. A., Harvey A. G., Dang S. T., Sackville T., Basten C. Treatment of acute stress disorder: A comparison of cognitive-behavioural therapy and supportive counseling. Journal of Consulting & Clinical Psychology. 1998;66(5):862–866. doi: 10.1037//0022-006x.66.5.862. [DOI] [PubMed] [Google Scholar]
- Bryant R. A., Moulds M. L., Guthrie R. M., Nixon R. D. The additive benefit of hypnosis and cognitive-behavioural therapy in treating acute stress disorder. Journal of Consulting & Clinical Psychology. 2005;73(2):334–340. doi: 10.1037/0022-006X.73.2.334. [DOI] [PubMed] [Google Scholar]
- Brymer M. J., Steinberg A. M., Vernberg E. M., Layne C. M., Watson P. J., Jacobs A. K. Acute Interventions for Children and Adolescents. In: Foa E. B., Keane T. M., Friedman M. J., Cohen J. A., editors. Effective treatment for PTSD. 2nd ed. New York: Guilford press; 2009. pp. 106–116. [Google Scholar]
- Caffo E., Belaise C. Psychological aspects of traumatic injury in children and adolescents. Child and Adolescent Psychiatric Clinics of North America. 2003;12(3):493–535. doi: 10.1016/s1056-4993(03)00004-x. [DOI] [PubMed] [Google Scholar]
- Casswell G. Learning from the aftermath: The response of mental health workers to a school bus crash. Clinical Child Psychology and Psychiatry. 1997;2:517–523. [Google Scholar]
- Catani C., Kohiladevy M., Ruf M., Schauer E., Elbert T., Neuner F. Treating children traumatized by war and Tsunami: a comparison between exposure therapy and meditation-relaxation in North-East Sri Lanka. BMC Psychiatry. 2009;9(22) doi: 10.1186/1471-244X-9-22. http://www.ncbi.nlm.nih.gov/pubmed/19439099. Retrieved from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chapman L., Morabito D., Ladakakos C., Schreier H., Knudson M. The effectiveness of art therapy interventions in educing Post Traumatic Stress Disorder (PTSD) symptoms in pediatric trauma patients. Art Therapy: Journal of the American Art Therapy Association. 2001;18(2):100–104. [Google Scholar]
- Chemtob C. M., Nakashima J. P., Carlson J. G. Brief treatment for elementary school children with disaster-related posttraumatic stress disorder: A field study. Journal of Clinical Psychology. 2002;58:99–112. doi: 10.1002/jclp.1131. [DOI] [PubMed] [Google Scholar]
- Cohen J. A. Treating acute posttraumatic reactions in children and adolescents. Biological Psychiatry. 2003;53(9):827–833. doi: 10.1016/s0006-3223(02)01868-1. [DOI] [PubMed] [Google Scholar]
- Cohen J. A., Bukstein O., Walter H., Benson S. R., Chrisman A., Farchione T. R. Practice parameter for the assessment and treatment of children and adolescents with posttraumatic stress disorder. Journal of the American Academy of Child & Adolescent Psychiatry. 2010;49(4):414–430. [PubMed] [Google Scholar]
- Espie E., Gaboulaud V., Baubet T., Casas G., Mouchenik Y., Yun O., Grais R. F., Moro M. R. Trauma-related psychological disorders among Palestinian children and adults in Gaza and West Bank, 2005–2008. International Journal of Mental Health, 3. 2009 doi: 10.1186/1752-4458-3-21. Art. No: 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foa E. B., Zoellner L. A., Feeny N. C. An evaluation of three brief programs for facilitating recovery after assault. Journal of Traumatic Stress. 2006;19(1):29–43. doi: 10.1002/jts.20096. [DOI] [PubMed] [Google Scholar]
- Fremont W. P. Childhood reactions to terrorism-induced trauma: A review of the past 10 years. Journal of the American Academy of Child & Adolescent Psychiatry. 2004;43(4):381–392. doi: 10.1097/00004583-200404000-00004. [DOI] [PubMed] [Google Scholar]
- Galante R., Foa D. An epidemiological study of psychic trauma and treatment effectiveness for children after a natural disaster. Journal of the American Academy of Child and Adolescent Psychiatry. 1986;25:357–363. [Google Scholar]
- Giannopoulou I., Dikaiakou A., Yule W. Cognitive-behavioural group intervention for PTSD symptoms in children following the Athens 1999 earthquake: A pilot study. Clinical Child Psychology and Psychiatry. 2006;11(4):543–553. doi: 10.1177/1359104506067876. [DOI] [PubMed] [Google Scholar]
- Gidron Y., Gal R., Freedman S., Twiser I., Lauden A., Snir Y. Translating research findings to PTSD prevention: Results of a randomized-controlled pilot study. Journal of Traumatic Stress. 2001;14(4):773–780. doi: 10.1023/A:1013046322993. [DOI] [PubMed] [Google Scholar]
- Goenjian A. K., Karayan I., Pynoos R. S., Minassian D., Najarian L. M., Steinberg A. M. Outcome of psychotherapy among early adolescents after trauma. American Journal of Psychiatry. 1997;154:536–542. doi: 10.1176/ajp.154.4.536. [DOI] [PubMed] [Google Scholar]
- Grant S. M., Hardin S. B., Pesut D. J., Hardin T. Psychological evaluations, referrals, and follow-up of adolescents after their exposure to Hurricane Hugo. Journal of child and Adolescent Psychiatric Nursing. 1997;10(1):7–16. doi: 10.1111/j.1744-6171.1997.tb00207.x. [DOI] [PubMed] [Google Scholar]
- Hoagwood K. E. Implementing CBT for traumatized children and adolescents after September 11: Lessons learned from the Child and Adolescent Trauma Treatments and Services (CATS) project. Journal of Clinical Child and Adolescent Psychology. 2007;36(4):581–592. doi: 10.1080/15374410701662725. [DOI] [PubMed] [Google Scholar]
- Klingman A. A school-based emergency crisis intervention in a mass school disaster. Professional Psychology: Research and Practice. 1987;18:604–612. [Google Scholar]
- La Greca A. M., Silverman W. K. Treatment and prevention of posttraumatic stress reactions in children and adolescents exposed to disasters and terrorism: What is the evidence? Child Development Perspectives. 2009;3(1):4–10. [Google Scholar]
- Math S. B., Tandon S., Girimaji S. C., Benegal V., Kumar U., Hamza A. Psychological impact of the tsunami on children and adolescents from the andaman and nicobar islands. The Primary Care Companion to the Journal of Clinical Psychiatry. 2008;10(1):31–37. doi: 10.4088/pcc.v10n0106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagao K., Okuno M., Shindou E. Mental symptoms induced by a massive outbreak of infectious disease (Enterhemorragic Escherichia Coli 0157) in elementary school children: II. Six cases of delayed and reactivated stress-related disorders, including PTSD. Japanese Journal of Child and Adolescent Psychiatry. 2001;42(4):315–322. [Google Scholar]
- Nagao K., Okuyama M., Miyamoto S., Haba T. Treating early mental health and post-traumatic symptoms of children in the Hanshin-Awaji earthquake. Acta Paediatrica Japonica. 1995;37(6):745–754. doi: 10.1111/j.1442-200x.1995.tb03418.x. [DOI] [PubMed] [Google Scholar]
- Poijula S., Kemppainen P., Wahlberg K. E., Hakko H. Early Crisis Intervention and Screening in School for Suicide-Bereaved Schoolmates; submitted. [Google Scholar]
- Poijula S., Wahlberg K. E., Dyregrov A. Adolescent suicide and suicide contagion in three secondary schools. International Journal of Emergency Mental Health. 2001;3(3):163–168. [PubMed] [Google Scholar]
- Pynoos R. S., Eth S. Witness to violence: The child interview. Journal of the American Academy of Child and Adolescent Psychiatry. 1986;25:306–319. [Google Scholar]
- Pynoos R. S., Nader K. Psychological first aid and treatment approach to children exposed to community violence: Research implications. Journal of Traumatic Stress. 1988;1(4):445–473. [Google Scholar]
- Rivlin E. The psychological trauma and management of severe burns in children and adolescents. British Journal of Hospital Medicine. 1988;40(3):210–215. [PubMed] [Google Scholar]
- Roberts N. P., Kitchiner N. J., Kenardy J., Bisson J. Multiple session early psychological interventions for the prevention of post-traumatic stress disorder. Cochrane Database of Systematic Reviews. 2010;(3) doi: 10.1002/14651858.CD006869.pub2. CD006869. [DOI] [PubMed] [Google Scholar]
- Salcioglu E., Basoglu M. Psychological effects of earthquakes in children: Prospects for brief behavioural treatment. World Journal of Pediatrics. 2008;4(3):165–172. doi: 10.1007/s12519-008-0032-8. [DOI] [PubMed] [Google Scholar]
- Schreier H., Ladakakos C., Morabito D., Chapman L., Knudson M. M. Posttraumatic stress symptoms in children after mild to moderate pediatric trauma: A longitudinal examination of symptom prevalence, correlates, and parent-child symptom reporting. Journal of Trauma. 2005;58(2):353–363. doi: 10.1097/01.ta.0000152537.15672.b7. [DOI] [PubMed] [Google Scholar]
- Silverman W. K., Ortiz C. D., Viswesvaran C., Burns B. J., Kolko D. J., Putnam F. W. Evidence-based psychosocial treatments for children and adolescents exposed to traumatic events. Journal of Clinical Child and Adolescent Psychology. 2008;37(1):156–183. doi: 10.1080/15374410701818293. [DOI] [PubMed] [Google Scholar]
- Stuber J., Fairbrother G., Galea S., Pfefferbaum B., Wilson-Genderson M., Vlahov D. Determinants of counseling for children in Manhattan after the September 11 attacks. Psychiatric Services. 2002;53(7):815–822. doi: 10.1176/appi.ps.53.7.815. [DOI] [PubMed] [Google Scholar]
- Vila G., Porche L.-M., Mouren-Simeoni M.-C. An 18-month longitudinal study of posttraumatic disorders in children who were taken hostage in their school. Psychosomatic Medicine. 1999;61(6):746–754. doi: 10.1097/00006842-199911000-00005. [DOI] [PubMed] [Google Scholar]
- Yule W., Udwin O. Screening child survivors for post-traumatic stress disorder: Experiences from the Jupiter sinking. British Journal of Clinical Psychology. 1991;30:131–138. doi: 10.1111/j.2044-8260.1991.tb00928.x. [DOI] [PubMed] [Google Scholar]