Abstract
OBJECTIVE
The purpose of this study was to develop a survey of general and diabetes-specific nutrition knowledge for youth with type 1 diabetes and their parents and to assess the survey’s psychometric properties.
RESEARCH DESIGN AND METHODS
A multidisciplinary pediatric team developed the Nutrition Knowledge Survey (NKS) and administered it to youth with type 1 diabetes (n = 282, 49% females, 13.3 ± 2.9 years) and their parents (82% mothers). The NKS content domains included healthful eating, carbohydrate counting, blood glucose response to foods, and nutrition label reading. Higher NKS scores reflect greater nutrition knowledge (score range is 0–100%). In youths, glycemic control was assessed by A1C, and dietary quality was determined by the Healthy Eating Index-2005 (HEI-2005) derived from 3-day diet records. Validity was based on associations of NKS scores with A1C and dietary quality. Reliability was assessed using the Kuder-Richardson Formula 20 (KR-20) and correlations of domain scores to total score.
RESULTS
Mean NKS scores (23 items) were 56.9 ± 16.4% for youth and 73.4 ± 12.5% for parents. The KR-20 was 0.70 for youth and 0.59 for parents, representing acceptable internal consistency of the measure. In multivariate analysis, controlling for youth age, family income, parent education, diabetes duration, and insulin regimen, parent NKS scores were associated with corresponding youth A1C (β = −0.13, P = 0.03). Both parent (β = 0.20, P = 0.002) and youth (β = 0.25, P < 0.001) NKS scores were positively associated with youth HEI-2005 scores.
CONCLUSIONS
The NKS appears to be a useful measure of general and diabetes-specific nutrition knowledge for youth with type 1 diabetes and their parents.
Medical nutrition therapy, along with exercise, blood glucose monitoring, and insulin administration, is an essential component of successful diabetes management in youth with type 1 diabetes (1,2). Assessing youth and parental understanding of diabetes management tasks, including dietary management, is important because knowledge is a prerequisite for adherence, and adherence influences glycemic control (3). Few validated measures exist to assess knowledge of dietary management in youth with type 1 diabetes and their parents. Moreover, carbohydrate intake has been the major focus of nutrition education in this population due to the substantial impact of carbohydrates on glycemic excursions. However, in addition to carbohydrate counting, the American Diabetes Association also recommends consumption of an overall healthful diet for this population (1). Therefore, a nutrition measure developed for patients and families with type 1 diabetes that assesses knowledge of both general nutrition and diabetes-specific domains would be useful both clinically and as a research tool.
Previous diabetes nutrition measures have been developed for patients with type 2 diabetes (4) or have focused specifically on carbohydrate counting and insulin dosing (5). In a previous study, parental carbohydrate counting ability was assessed by comparing parents’ estimation of meal carbohydrate content with carbohydrate content calculated from dietary recalls; greater parental precision in carbohydrate counting was significantly associated with better youth glycemic control (6). In another study, higher scores on the 78-item PedsCarbQuiz, which assesses carbohydrate and insulin-dosing knowledge in youth with type 1 diabetes (5), were correlated with lower A1C values in a sample of youth with type 1 diabetes, 12 years of age and older, and their parents. Although these measures are effective in assessing carbohydrate counting skills and associations with glycemic control, they may be too resource intensive or too specific to carbohydrate estimation for an overall assessment of general nutrition knowledge in this population. A broader assessment of nutrition knowledge may be relevant not only for diabetes management, but also because nutrition plays a role in numerous relevant health outcomes, such as weight and cardiovascular risk status, for youth with type 1 diabetes (7–12).
The purpose of this study was to develop a survey of general and diabetes-specific nutrition knowledge for youth with type 1 diabetes and their parents and to assess the survey’s psychometric properties, including item difficulty, item discrimination, internal consistency, and internal reliability. We hypothesized that the measure would demonstrate acceptable internal consistency and reliability, and would be associated with glycemic control and diet quality.
RESEARCH DESIGN AND METHODS
Developing the questionnaire item pool
The survey items were developed by a multidisciplinary team consisting of pediatric endocrinologists, pediatric diabetes nurses, nutrition scientists, registered dietitians, certified diabetes educators, and behavioral scientists. Item content was designed to reflect constructs typically addressed in diabetes nutrition education and relevant to disease management and general health. The content domains of the Nutrition Knowledge Survey (NKS) included 1) healthful eating, 2) carbohydrate counting, 3) blood glucose response to foods, and 4) nutrition label reading. An initial item pool of 39 questions was generated. Items were multiple-choice with four response options.
Study participants
Eligibility criteria for youth included the diagnosis of type 1 diabetes for >1 year, 8–18 years of age, daily insulin dose ≥0.5 units/kg, and absence of any significant gastrointestinal disease that would impact dietary intake (e.g., celiac or inflammatory bowel disease). Youth with type 1 diabetes and their parents were recruited during routine clinic visits to a tertiary pediatric diabetes center in Boston, Massachusetts. Informed consent was obtained from parents and youth 18 years of age, and assent was obtained from children <18 years of age. Families received $40 compensation for their participation. The local institutional review board approved the study.
Administration and scoring
Youth and parents independently completed parallel versions of the NKS on the same day as a routine clinic appointment. The 39 items took ∼10–15 min to answer. NKS scores were calculated as the percentage of retained items answered correctly, such that scores could range from 0 to 100%, with higher percentages indicating greater nutrition knowledge.
Dietary intake and diet quality
Dietary intake of youth was assessed with 3-day diet records (typically two weekdays and one weekend day). Study staff instructed families on how to complete diet records, which were usually completed within 1 week of the study visit. Dietary data were analyzed with Nutrition Data System for Research software version 2009 developed by the Nutrition Coordinating Center at the University of Minnesota (Minneapolis, MN). The U.S. Department of Agriculture’s Healthy Eating Index-2005 (HEI-2005) was calculated to assess conformance to dietary guidelines using the method recently developed by Miller et al. (13); HEI-2005 scores range from 0 to 100, with higher scores indicating more healthful diets.
Demographic and clinical data
Demographic information including race/ethnicity, parent education level, household composition, and household income were collected by parent self-report. Details on diabetes history and current treatment regimen were abstracted from electronic health records from the same clinic visit in which the NKS was administered. A1C was assayed by high-performance liquid chromatography (Tosoh 2.2 device; Tosoh Corp., San Francisco, CA); reference range is 4–6%.
Statistical analyses
The psychometric properties of the NKS were determined. Survey items were analyzed for item difficulty by examining the percentage of participants that answered each item correctly. An item was eliminated if <20 or >90% of both youth and parents answered it correctly. Although this resulted in a greater number of items with lower difficulty and discrimination for parents than for youth, this was determined to be acceptable in order to create a parallel measure for parents and children. Item discrimination was determined by computing the index of discrimination ([upper group % correct] – [lower group % correct]), which reflects the degree to which an item differentiates between high and low scorers on the total measure. The acceptable index for item discrimination values was 25% and greater, as this indicates good item discrimination, with values of 15–24% considered marginal (14). The Kuder-Richardson Formula 20 (KR-20) was used as an overall measure of internal consistency appropriate for dichotomous responses (i.e., correct/incorrect) and scores are interpreted like a Cronbach α (indicating the degree to which the set of items measures a single construct). Higher scores indicate a more homogeneous test and greater internal consistency. Internal reliability was examined by calculating the degree to which the subtotal score of each of the four domains correlated with the total score. Multiple linear regression analysis, controlling for clinically relevant diabetes-related and demographic characteristics (youth age, family income, parent education, diabetes duration, and insulin regimen), was used to assess the relations of nutrition knowledge with A1C and dietary intake in subjects providing diet records. In the models examining youth NKS, interactions of youth age with NKS were tested to determine whether the association of youth NKS with A1C and dietary intake varied by age. Analyses were performed using SPSS version 17.0 (Chicago, IL).
RESULTS
Participants
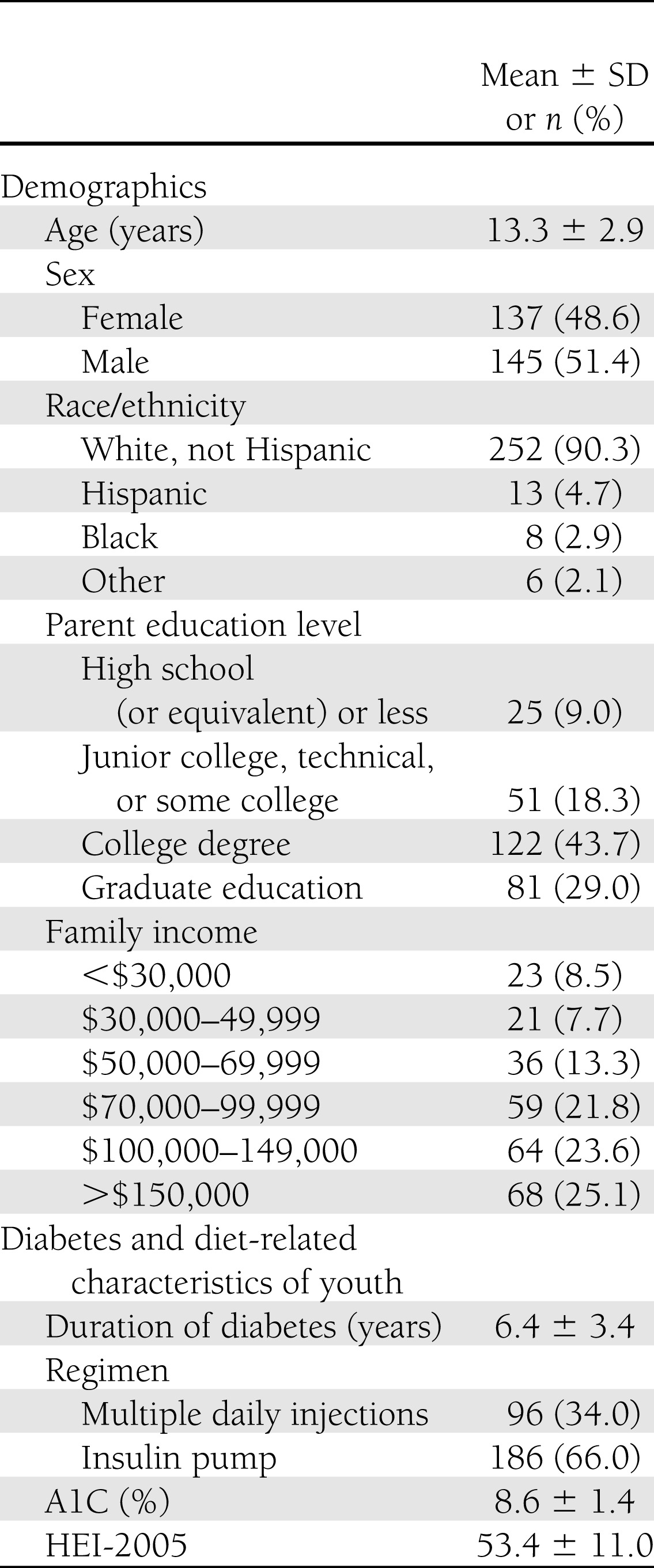
Two hundred eighty-two youths and their parents (82% mothers) completed the measure. The mean duration of diabetes for youth was 6.4 ± 3.4 years, mean A1C was 8.6 ± 1.4%, and 66% of youths received insulin pump therapy. Sample characteristics are presented in Table 1. Of the 282 youths, 252 (89%) completed 3-day diet records. Parent NKS scores were significantly higher for youths with completed diet records (74.1 ± 11.6% vs. 68.0 ± 17.5%, P = 0.01); there were no differences in youth NKS scores between those who did and did not complete diet records.
Table 1.
Sample characteristics of study participants (n = 282)
Item and scale properties
The initial survey consisted of 39 items. Ten items were eliminated because either <20 or >90% of both youth and parents answered them correctly. Four items were eliminated because their index of discrimination was <25% for both parents and youth; however, one item with a marginal discrimination index value (question 23) (Table 2) was retained for greater conceptual comprehensiveness of the carbohydrate-counting questions. Two items were eliminated due to redundancy with other survey items. The final resulting NKS consists of 23 items (Supplementary Data). The Flesh-Kincaid grade level of the measure, as automated in Microsoft Word 2007 (Microsoft Corp., Redmond, WA), was 8.4.
Table 2.
Item difficulty and item discrimination of each question on the NKS
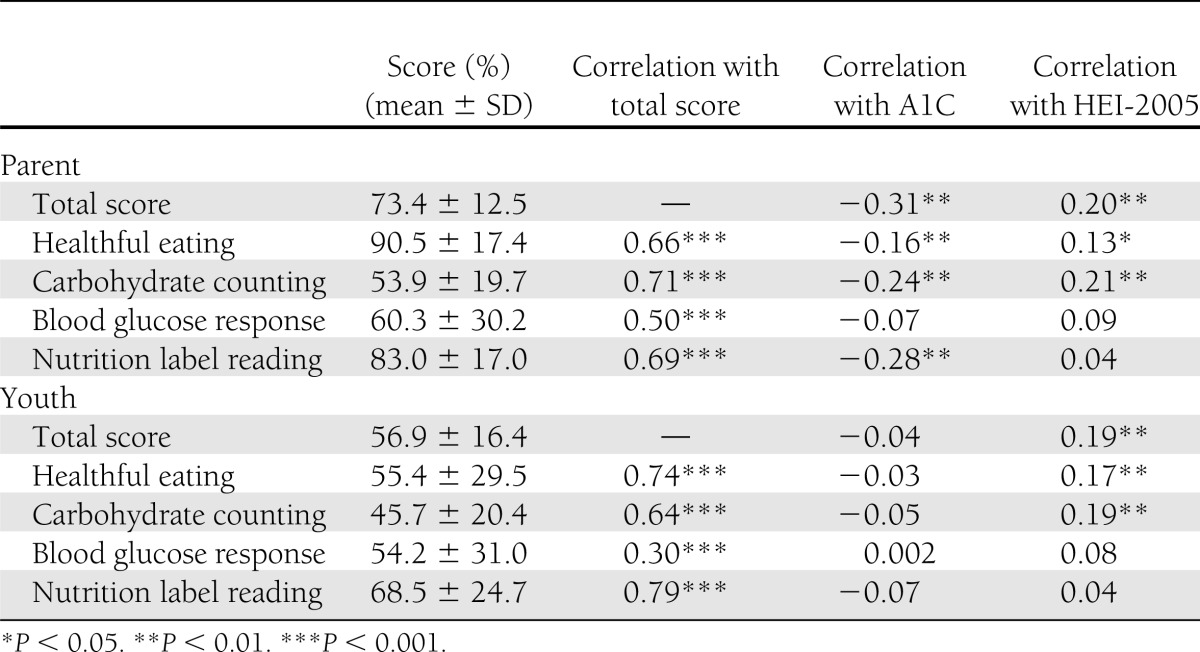
The item difficulty and item discrimination of each retained NKS question are presented in Table 2. Item difficulty ranged from 19 to 86% for youth and 23 to 96% for parents. Item discrimination was good for the majority of items. The KR-20 was 0.70 for youth and 0.59 for parents. Scores for each of the four domains in the survey were positively correlated with the total NKS score for both parents and youth (P < 0.001, all correlations) (Table 3).
Table 3.
Parent and youth NKS total and domain scores and correlations with youth A1C and HEI-2005 scores
The mean NKS scores based on the reduced item pool were 73.4 ± 12.5% (range 30–96) for parents and 56.9 ± 16.4% (range 13–91) for youth (P < 0.001). Youth ≥13 years of age had higher scores than those <13 years of age (62.9 ± 14.1 vs. 49.4 ± 16.0%, P < 0.001). Parent and youth NKS scores were modestly correlated (r = 0.25, P < 0.001), and youth NKS scores were moderately correlated with youth age (r = 0.44, P < 0.001).
Association with demographic characteristics
Youth, but not parent, NKS scores showed a small correlation with diabetes duration (r = 0.12, P = 0.04). Parents of youths using an insulin pump showed higher NKS scores than parents of youths using multiple daily injections (75.2 vs. 70.0%, P = 0.001). The higher NKS scores in youths using insulin pump therapy approached statistical significance compared with youths using multiple daily injections (58.2 vs. 54.2%, respectively, P = 0.07). Parents with a college degree or greater had higher NKS scores than parents with less education (76.0 vs. 69.1%, P < 0.001); this association was also seen among their corresponding children’s scores (58.5 vs. 54.3%, P = 0.04). Household income was modestly associated with parent (r = 0.23, P < 0.001), but not youth, NKS scores.
Validity
Correlations of NKS total and domain scores with youth A1C and HEI-2005 are shown in Table 3. Parent, but not youth, NKS scores were inversely associated with youth A1C (r = −0.31, P < 0.01, and r = −0.04, NS, respectively); both parent and youth NKS were positively associated with HEI-2005. In multivariate analysis, parent NKS score remained inversely associated with youth A1C (β = −0.13, P = 0.03; model r2 = 0.23) after controlling for youth age, family income, parent education, diabetes duration, and insulin regimen. Both parent (β = 0.20, P = 0.002; model r2 = 0.07) and youth (β = 0.25, P < 0.001; model r2 = 0.08) NKS scores remained associated with HEI-2005 scores after controlling for youth age, family income, parent education, diabetes duration, and insulin regimen. There were no significant interactions of youth age with youth NKS scores for associations with either A1C or HEI-2005.
CONCLUSIONS
Despite modern approaches to intensive insulin therapy for the management of type 1 diabetes, dietary management remains at the cornerstone of diabetes treatment (1,15). Previous research supports the relevance of dietary adherence to diabetes outcomes (16–19). The NKS is a brief, reliable, and easy-to-use measure of nutrition knowledge for youth with type 1 diabetes and their families. The NKS was designed for clinical and research use as a measure of nutrition knowledge.
The NKS is one of the first measures specifically developed for youth with type 1 diabetes and their parents that assesses both general nutrition (e.g., healthful choices and label reading) and diabetes-specific (e.g., carbohydrate counting and glycemic response to foods) nutrition knowledge. Previous nutrition measures for youth with type 1 diabetes have focused primarily on carbohydrate counting (5). Those measures were used to inform the development of the current measure; however, the NKS was developed to be a broader measure that assesses various aspects of nutrition, which are important for optimal diabetes management. Notably, our findings indicate that both general and diabetes-specific dimensions of parents’ nutrition knowledge were associated with glycemic control.
The advantages of the NKS are that it is a brief, self-administered measure that can be completed in ∼10 min. The reading level is somewhat higher than that of the youngest participants; however, reading level is based on the number of syllables in the words used. A nutrition knowledge measure for this population requires the use of multisyllable terms such as carbohydrate (used repeatedly in the measure), insulin, vitamins, etc. Due to diabetes education provided to these youth, they very likely understood these terms. When the measure was tested in a relatively large sample of youth with type 1 diabetes managed with modern intensive insulin therapy and their parents, it demonstrated acceptable internal consistency and external validity. Greater nutrition knowledge of parents was associated with both better glycemic control and higher diet quality in youths. In addition, greater youth nutrition knowledge was associated with higher diet quality; however, the association of youth nutrition knowledge with glycemic control was not significant. The mean youth age was 13 years; therefore, it is likely that parents were primarily responsible for food-related decisions, including grocery shopping, meal preparation, and carbohydrate counting. Notably, parent NKS was significantly higher than youth NKS. Associations of higher NKS with higher parent education, older youth age, insulin pump use, and diabetes duration further support the validity of the measure because these factors likely relate to greater exposure to nutrition education. The majority of parents who completed the NKS were mothers so it was not possible to determine whether mothers’ and fathers’ nutrition knowledge scores would have different relationships with youth A1C; this would be an interesting question to examine in future research.
There were several limitations with the current study. The NKS was evaluated in a relatively homogenous sample of youth (e.g., good control and majority on insulin pumps) receiving care at a single diabetes clinic. Although the sample in this study was a convenience sample, the racial distribution reflects the demographics of type 1 diabetes. However, parents were predominantly college educated, and there were few low-income families. In the future, it would be useful to test the measure in a more diverse group of youth from several diabetes centers to determine the measure’s performance in a more heterogeneous sample. Although the measure demonstrated the hypothesized relations with A1C and HEI-2005, there was no gold standard of general and diabetes nutrition knowledge against which to test the measure. It would be useful, however, to determine the association of the carbohydrate-counting domain of the NKS with the PedsCarbQuiz in future research. Another limitation of the study was the possibility of reporting bias in the food records, which is a concern in all diet studies. However, the mean HEI-2005 in this sample was similar to that observed in a representative sample of U.S. youth (20).
In conclusion, the NKS is a brief, self-administered measure developed to assess both general and diabetes-specific nutrition knowledge in youth with type 1 diabetes and their parents. Our findings provide strong evidence of preliminary validity of the measure to assess nutrition knowledge, suggesting potential utility in both clinical and research settings. Future research to determine the measure’s utility should include assessing the sensitivity of the measure to change in response to nutrition counseling.
Supplementary Material
Acknowledgments
This research was supported by the intramural research program of the National Institutes of Health, Eunice Kennedy Shriver National Institute of Child Health and Human Development (Contract HH-SN-267200703434C).
No potential conflicts of interest relevant to this article were reported.
A.J.R. analyzed data and wrote the manuscript. T.R.N. analyzed data, contributed to the discussion, and reviewed and edited the manuscript. S.N.M. and L.M.L. collected data, contributed to the discussion, and reviewed and edited the manuscript. L.A.H. reviewed and edited the manuscript. D.L.H. contributed to the discussion and reviewed and edited the manuscript. T.R.N. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Data from this study were presented at the 70th Scientific Sessions of the American Diabetes Association, Orlando, Florida, 25–29 June 2010.
Footnotes
This article contains Supplementary Data online at http://care.diabetesjournals.org/lookup/suppl/doi:10.2337/dc11-2371/-/DC1.
References
- 1.Bantle JP, Wylie-Rosett J, Albright AL, et al. American Diabetes Association Nutrition recommendations and interventions for diabetes: a position statement of the American Diabetes Association. Diabetes Care 2008;31(Suppl. 1):S61–S78 [DOI] [PubMed] [Google Scholar]
- 2.Johnson CC, Nicklas TA, Arbeit ML, Franklin FA, Berenson GS. A comprehensive model for maintenance of family health behaviors: the “Heart Smart” family health promotion program. Fam Community Health 1988;11:1–7 [Google Scholar]
- 3.Hood KK, Peterson CM, Rohan JM, Drotar D. Association between adherence and glycemic control in pediatric type 1 diabetes: a meta-analysis. Pediatrics 2009;124:e1171–e1179 [DOI] [PubMed] [Google Scholar]
- 4.Miller CK, Achterberg CL. Reliability and validity of a nutrition and food-label knowledge test for women with type 2 diabetes mellitus. J Nutr Educ 2000;32:43–48 [Google Scholar]
- 5.Koontz MB, Cuttler L, Palmert MR, et al. Development and validation of a questionnaire to assess carbohydrate and insulin-dosing knowledge in youth with type 1 diabetes. Diabetes Care 2010;33:457–462 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mehta SN, Quinn N, Volkening LK, Laffel LMB. Impact of carbohydrate counting on glycemic control in children with type 1 diabetes. Diabetes Care 2009;32:1014–1016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jones KL. Role of obesity in complicating and confusing the diagnosis and treatment of diabetes in children. Pediatrics 2008;121:361–368 [DOI] [PubMed] [Google Scholar]
- 8.Krishnan S, Short KR. Prevalence and significance of cardiometabolic risk factors in children with type 1 diabetes. J Cardiometab Syndr 2009;4:50–56 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Libman IM, Pietropaolo M, Arslanian SA, LaPorte RE, Becker DJ. Changing prevalence of overweight children and adolescents at onset of insulin-treated diabetes. Diabetes Care 2003;26:2871–2875 [DOI] [PubMed] [Google Scholar]
- 10.Mangge H, Schauenstein K, Stroedter L, Griesl A, Maerz W, Borkenstein M. Low grade inflammation in juvenile obesity and type 1 diabetes associated with early signs of atherosclerosis. Exp Clin Endocrinol Diabetes 2004;112:378–382 [DOI] [PubMed] [Google Scholar]
- 11.Szadkowska A, Pietrzak I, Szlawska J, Kozera A, Gadzicka A, Młynarski W. Abdominal obesity, metabolic syndrome in type 1 diabetic children and adolescents. Pediatr Endocrinol Diabetes Metab 2009;15:233–239 [PubMed] [Google Scholar]
- 12.Wadwa RP. Cardiovascular disease risk in youth with diabetes mellitus. Rev Endocr Metab Disord 2006;7:197–204 [DOI] [PubMed] [Google Scholar]
- 13.Miller PE, Mitchell DC, Harala PL, Pettit JM, Smiciklas-Wright H, Hartman TJ. Development and evaluation of a method for calculating the Healthy Eating Index-2005 using the Nutrition Data System for Research. Public Health Nutr 2011;14:306–313 [DOI] [PubMed] [Google Scholar]
- 14.Moussa MA, Ouda BA, Nemeth A. Analysis of multiple-choice items. Comput Methods Programs Biomed 1991;34:283–289 [DOI] [PubMed] [Google Scholar]
- 15.Smart C, Aslander-van Vliet E, Waldron S. Nutritional management in children and adolescents with diabetes. Pediatr Diabetes 2009;10(Suppl. 12):100–117 [DOI] [PubMed] [Google Scholar]
- 16.Anderson EJ, Richardson M, Castle G, et al. The DCCT Research Group Nutrition interventions for intensive therapy in the Diabetes Control and Complications Trial. J Am Diet Assoc 1993;93:768–772 [DOI] [PubMed] [Google Scholar]
- 17.Delahanty LM, Halford BN. The role of diet behaviors in achieving improved glycemic control in intensively treated patients in the Diabetes Control and Complications Trial. Diabetes Care 1993;16:1453–1458 [DOI] [PubMed] [Google Scholar]
- 18.Delahanty LM. Clinical significance of medical nutrition therapy in achieving diabetes outcomes and the importance of the process. J Am Diet Assoc 1998;98:28–30 [DOI] [PubMed] [Google Scholar]
- 19.Mehta SN, Volkening LK, Anderson BJ, et al. Family Management of Childhood Diabetes Study Steering Committee Dietary behaviors predict glycemic control in youth with type 1 diabetes. Diabetes Care 2008;31:1318–1320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fungwe T, Guenther PM, Juan WY, Hiza H, Lino M. The Quality of Children's Diets in 2003-04 As Measured by the Healthy Eating Index-2005. Nutrition Insight 43 Washington D.C., U.S. Department of Agriculture, Center for Nutrition Policy and Promotion, 2009 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.