Abstract
OBJECTIVE
To determine the association of regular exercise, BMI, and fasting glucose with the risk of type 2 diabetes and to predict the risk.
RESEARCH DESIGN AND METHODS
Korean subjects (n = 7,233; 40–79 years old) who were not diagnosed with diabetes at baseline were enrolled through the National Health Insurance Corporation. All participants underwent biennial examinations, and 1,947 of 7,233 subjects also underwent a 6-month program of moderate-intensity exercise (300 min/week) without dietary advice.
RESULTS
During follow-up (mean = 2 years), there were 303 incidents of type 2 diabetes in the nonexercise program group (n = 5,286) and 83 in the exercise program group (n = 1,947). After adjusting for confounders, the risk of type 2 diabetes was positively associated with BMI and inversely with regular exercise, especially among overweight/obese subjects. After further adjustment for BMI, the odds ratios for risk of diabetes associated without and with regular exercise were 1.00 and 0.77, respectively. Among subjects with normal fasting glucose, exercise reduced the diabetes risk; however, among those with impaired fasting glucose (IFG), the protective effect of exercise was found only among overweight/obese subjects. The overweight/obese subjects in the exercise program group exhibited improved fasting glucose compared with the nonexercise program group and showed 1.5 kg of weight loss and a 3-cm decrease in waist circumference. Among overweight/obese subjects with unchanged fasting glucose, weight loss was greater in the exercise program group.
CONCLUSIONS
Regular exercise reduces the risk of type 2 diabetes in overweight/obese individuals. Particularly, regular exercise and weight or waist circumference control are critical factors for preventing diabetes in overweight/obese individuals with IFG.
The benefits of exercise in preventing and treating type 2 diabetes are widely recognized (1). Exercise improves glycemic control, body composition, cardiorespiratory fitness, cardiovascular risk, physical functioning, and well-being in patients with type 2 diabetes or prediabetes (1–3). Regular exercise is therefore a key strategy in diabetes prevention. A number of large-scale, randomized, controlled trials have been performed to evaluate the effect of lifestyle modification in prediabetic populations (4–10), with the aim of reducing the incidence of type 2 diabetes and ameliorating risk factors associated with this disease. These lifestyle interventions, which generally included both physical activity and nutritional interventions, have been highly successful in preventing the onset of type 2 diabetes. Studies that failed to show improved glycemic control typically reported poor exercise compliance (11) or low-intensity exercise (12). However, most physical activity intervention studies focused on English speakers. Additional studies are needed to characterize ethnic and/or cultural differences in the risk of type 2 diabetes because most studies show lower physical activity levels in nonwhite compared with white populations (13). Accordingly, tailor-made interventions that take into account the different needs of various groups (e.g., language and culture) should be developed and evaluated. In this prospective cohort study, we evaluated the association of regular exercise, BMI, and glucose levels with the risk of type 2 diabetes in a Korean population. The exercise program was prescribed and delivered by qualified health professionals.
RESEARCH DESIGN AND METHODS
Study population
This 2-year, prospective cohort study included 7,233 Korean subjects (40–79 years old) who underwent biennial medical evaluations through the National Health Insurance Corporation (NHIC) (2007–2011). Major exclusion criteria included a diagnosis of diabetes or use of medications known to impair glucose tolerance. The procedure and results of screening, recruitment, and classification of the study subjects are shown in the flowchart (Supplementary Fig. 1). A total of 21,673 subjects underwent both basal and biennial medical evaluations between 2007 and 2011. Type 2 diabetes was not detected in 7,576 subjects (35.0%), and they were subdivided into the exercise (n = 2,290) and nonexercise (n = 5,286) program groups. Among the exercise program group, 1,947 subjects met the requirements of the exercise program. At any period during the 2-year study, 1,947 of the subjects participated in a 6-month exercise program provided by the Health Promotion Center of the NHIC that consisted of 300 min/week of moderate-intensity exercise without specific dietary advice. The remaining 5,286 subjects underwent the biennial examinations only. At the end of the 2-year study, participants were subdivided into groups according to fasting glucose levels: normal fasting glucose (NFG), impaired fasting glucose (IFG), and type 2 or new-onset diabetes based on the biennial medical evaluation results. New-onset diabetes was defined as diagnosed (i.e., use of antidiabetic medication) or undiagnosed (American Diabetes Association criteria of fasting glucose ≥126 mg/dL [7.0 mmol/L]). IFG was defined as a fasting glucose level of 100–126 mg/dL (5.55–6.99 mmol/L) and NFG as a fasting glucose level <100 mg/dL (5.55 mmol/L). Written informed consent was obtained from all participants before screening, consistent with the Helsinki Declaration.
Exercise program
The exercise program was prescribed and delivered by qualified health professionals. All subjects who volunteered to participate in the exercise program were screened for eligibility through questionnaires and the basic medical examination before enrollment. Based on the screening result, eligible participants underwent a physical fitness test that included a hand-grip strength measurement and sit-up test for muscular strength, a standing on one leg with eyes closed test for balance, and the use of a cycle ergometer for testing cardiorespiratory endurance. After the baseline anthropometric and fitness measurement, the exercise physiologist prescribed a personalized program (i.e., exercise type, intensity, and frequency) to each person. Intensity of aerobic exercise ranged between an initial exercise intensity of 65% heart rate maximum to, and upward of, 85% heart rate maximum. Intensity of resistance exercise was 50% of one repetitive maximum value and trained in one set (12–15 repetitions). Exercise frequency was three times per week for 6 months. The programs were performed for 6 months and consisted of warm-up (10–15 min), aerobic (25–30 min; e.g., treadmill or cycling), resistance (10–15 min; e.g., bench press, arm curl, bent-knee sit-up, etc.), and cool-down (10–15 min; general relaxation and stretching) exercises.
Data collection: anthropometric and biochemical parameters
The NHIC biennial examinations performed by the medical staff at local hospitals follow a standard procedure. Participants were asked 1) to describe health habits, including cigarette smoking and alcohol consumption and 2) whether they were treated for diabetes, and the date of diagnosis if they answered yes. Anthropometric and biochemical measurements included BMI, waist circumference, and blood pressure. Serum glucose and lipid profiles (triglycerides and total, LDL, and HDL cholesterol) were measured after fasting.
Statistical analyses
Each participant’s fasting glucose status was classified as NFG, IFG, or type 2 diabetes based on results of the biennial examinations. At the end of the study, any changes from baseline were categorized as improvement (IFG to NFG), no change (NFG to NFG and IFG to IFG), or deterioration (NFG to IFG and NFG/IFG to diabetes); the last two categories (i.e., NFG/IFG to diabetes) were combined because of small numbers in the NFG-to-diabetes category (14).
Statistical analyses were performed using SPSS version 12.0 for Windows (SPSS Inc., Chicago, IL). Frequency was analyzed by χ2 test. Differences in clinical variables between groups (exercise vs. nonexercise program group) were evaluated by independent Student t test, and a general linear model test was used to adjust for baseline values or smoking/drinking status and antihypertensive drug use. A paired Student t test was used to evaluate the effects of the exercise program. After adjusting for confounding factors, the association of type 2 diabetes with exercise, BMI, and fasting glucose concentrations was evaluated using a logistic regression model to estimate odds ratios (ORs) (95% CIs). Logistic regression analysis was used to determine the relationship between IFG and type 2 diabetes status and participation in an exercise program. Continuous variables were expressed as mean ± SE, and categorical variables were expressed as absolute numbers and percentages. A two-tailed value of P < 0.05 was considered significant.
RESULTS
Clinical characteristics at baseline and 2-year follow-up
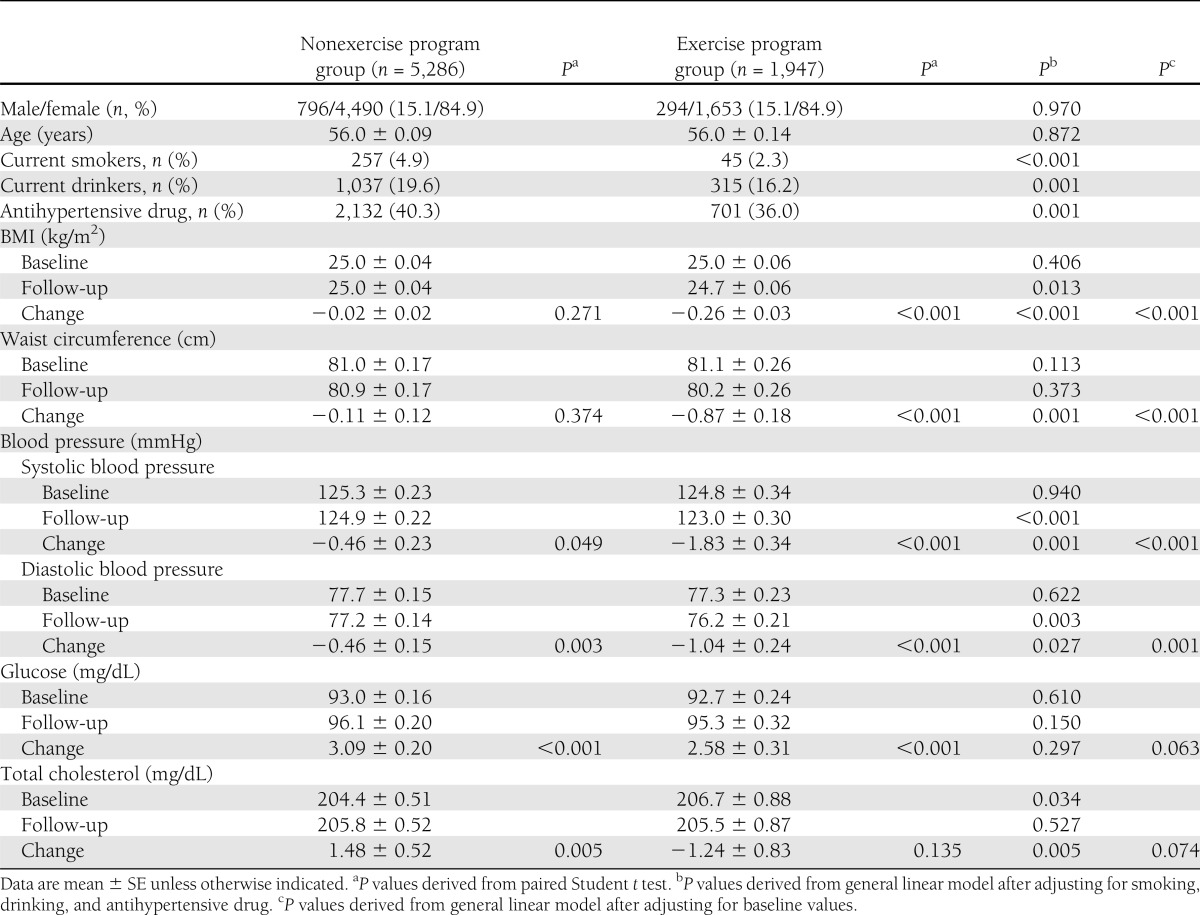
We measured compliance to the exercise program and only included subjects that attended at least 60 of the intervention periods (72 times/6 months). All subjects who were affiliated with the exercise program group underwent a 6-month program of moderate-intensity exercise (300 min/week) without dietary advice. Almost all of the basal physical fitness test characteristics in the exercise program group (hand-grip strength measurement, sit-up test, standing on one leg with eyes closed test, and trunk flexion forward test) were improved at the end of the 2-year study (Supplementary Table 1). Clinical characteristics of participants at baseline and at the 2-year follow-up are shown in Table 1. No significant differences were found between the two groups (exercise vs. nonexercise program group) in sex distribution, age, BMI, blood pressure, and serum glucose at baseline. However, the exercise program group had lower proportions of current smokers, current drinkers, and antihypertensive drug users compared with the nonexercise program group. Mean total cholesterol level at baseline was slightly but significantly higher in the exercise program group after adjusting for smoking, drinking, and antihypertensive drug use.
Table 1.
Participant characteristics at baseline and at the end of the 2-year study
At the end of the 2-year study, the nonexercise program group showed significantly increased fasting glucose and total cholesterol levels, but decreased blood pressure. The exercise program group also showed significantly increased fasting glucose levels, but decreased BMI, waist circumference, and blood pressure. After adjusting for baseline values, changes in BMI, waist circumference, and blood pressure were significantly lower in the exercise program group compared with the nonexercise program group. At the 2-year follow-up, BMI and blood pressure were lower in the exercise program group than the nonexercise program group after adjusting for smoking, drinking, and antihypertensive drug use (Table 1).
Association between type 2 diabetes and exercise, BMI, and fasting glucose
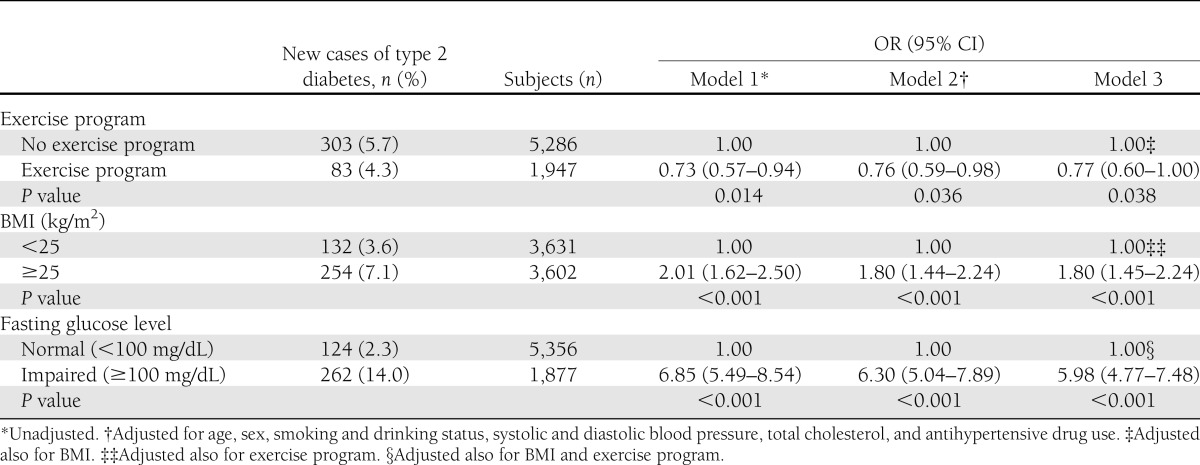
During a mean follow-up period of 2 years, there were 303 incident cases of type 2 diabetes in the nonexercise program group and 83 in the exercise program group (Table 2). The risk of type 2 diabetes after adjusting for confounding factors (age, sex, smoking/drinking status, systolic and diastolic blood pressure, total cholesterol, and antihypertensive drug use) significantly decreased with regular exercise. After further adjustment for BMI, the ORs for risk of diabetes associated without and with regular exercise were 1.00 and 0.77, respectively (P = 0.038 for trend). Overweight/obesity was associated with a 1.80-fold increased risk for type 2 diabetes compared with normal weight after adjusting for confounding factors and exercise (P < 0.001 for trend). Subjects with IFG showed a 5.98-fold higher risk of developing type 2 diabetes than subjects with NFG after adjustment for all covariates (P < 0.001 for trend).
Table 2.
Association between type 2 diabetes and exercise, BMI, and fasting glucose concentration
In subgroup analyses based on BMI (<25 and ≥25 kg/m2) (Supplementary Fig. 2A), the inverse association between exercise and risk of type 2 diabetes was stronger for overweight/obese subjects. The inverse association between exercise and risk for type 2 diabetes persisted in subgroup analyses based on glucose levels (NFG and IFG) (Supplementary Fig. 2B). The positive association between BMI and risk of type 2 diabetes was confirmed in subjects with NFG and IFG (Supplementary Fig. 2C).
The joint association of exercise, BMI, and glucose levels with the risk of type 2 diabetes after adjusting for confounding factors is shown in Supplementary Fig. 3. Among subjects with NFG, BMI was positively associated with the protective effect of exercise. However, among those with IFG, the protective effect of exercise was only found in overweight/obese subjects. Compared with normal-weight subjects with NFG in the exercise program group, overweight/obese subjects with IFG in the nonexercise program group showed a 16.3-fold higher risk of developing type 2 diabetes. The relative effect of obesity and exercise on diabetes risk was larger among subjects with NFG, but the absolute effect was larger among subjects with IFG.
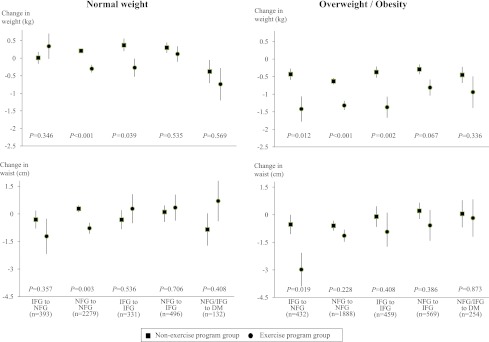
Mean changes in body weight and waist circumference according to fasting glucose level change, exercise, and BMI
Among overweight/obese subjects, significantly fewer subjects showed improved fasting glucose (from IFG to NFG) during the 2-year study in the exercise program group, although body weight fell by about 1.5 kg and waist circumference by 3 cm (Fig. 1). Among overweight/obese subjects whose fasting glucose status did not change, weight loss was greater in the exercise program group. Among normal-weight subjects with unchanged NFG status, reductions in body weight and waist circumference were significantly greater in the exercise program group.
Figure 1.
Mean changes in body weight and waist circumference according to participation in the 6-month exercise program, BMI (normal weight vs. overweight/obese), and changes in fasting glucose. Data are expressed as mean ± SE. DM, type 2 diabetes. (A high-quality color representation of this figure is available in the online issue.)
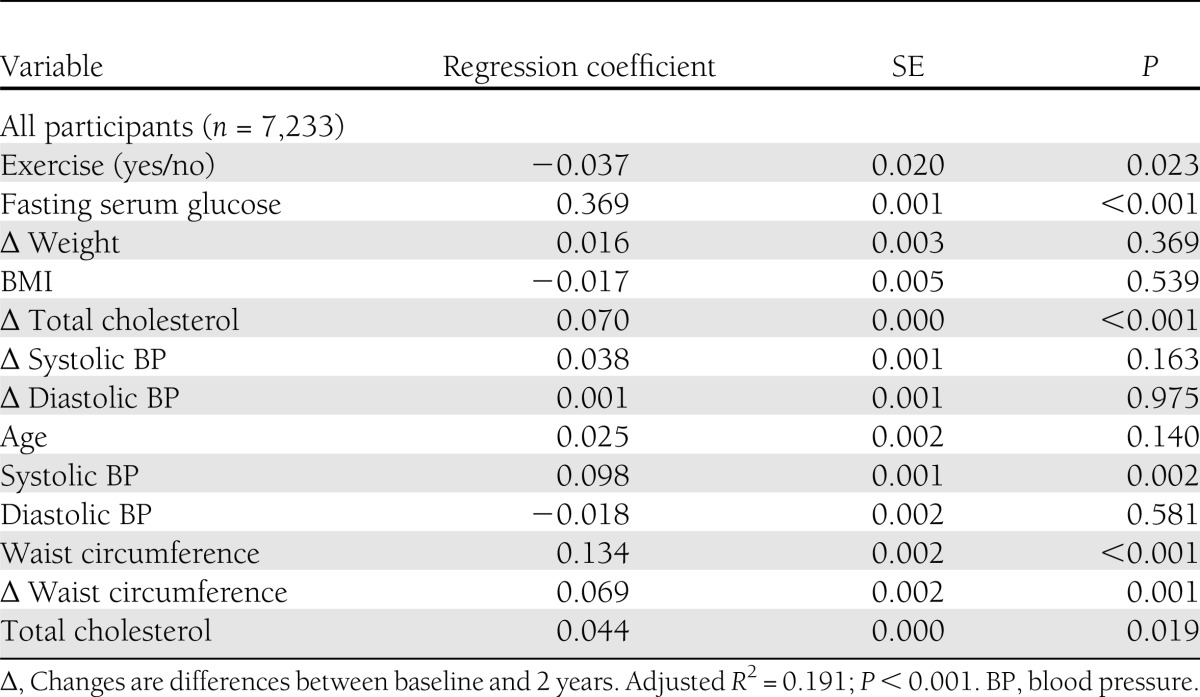
Regular exercise as an independent predictor of IFG and type 2 diabetes
Based on these results, we performed logistic regression analysis to determine independent predictors of IFG and type 2 diabetes (Table 3). Age, baseline BMI, △ weight, baseline waist circumference, △ waist circumference, exercise, baseline glucose level, baseline blood pressure (diastolic and systolic), △ blood pressure (diastolic and systolic), baseline total cholesterol, and △ total cholesterol were evaluated. Regular exercise was found to be an independent predictor of IFG and type 2 diabetes (β = −0.037 ± 0.020; P = 0.023) together with known risk factors for IFG and metabolic syndrome (baseline waist circumference, P < 0.001; △ waist circumference, P = 0.001; baseline glucose level, P < 0.001; baseline systolic blood pressure, P = 0.002; baseline total cholesterol, P = 0.019; and △ total cholesterol, P < 0.001).
Table 3.
Results of logistic regression analysis for IFG and diabetes status as dependent variables
CONCLUSIONS
In this 2-year study, a 6-month exercise program consisting of 300 min/week of moderate-intensity exercise without dietary changes resulted in a 23% reduction in the incidence of type 2 diabetes. This inverse association between exercise and risk of type 2 diabetes was stronger among overweight/obese subjects than normal-weight subjects. In addition, the exercise program group showed improved fasting glucose levels (from IFG to NFG: normal-weight subjects in the exercise program group, 46.0%; overweight/obese subjects in the exercise program group, 54.0%). Improved fasting glucose was associated with reductions in waist circumference and BMI; this reduction was significantly greater in the exercise program group, suggesting that regular exercise indirectly reduces the risk of type 2 diabetes through decreased body weight or improved body fat distribution in overweight/obese subjects. Exercise has been shown to facilitate weight loss (15) but more strongly influences abdominal adiposity (16). The overweight/obese subjects in the exercise program group whose fasting glucose values improved or remained the same showed a greater reduction in body weight. This result is consistent with previous reports showing that being overweight or physically inactive increases the risk of type 2 diabetes (6), demonstrating the need for appropriate exercise interventions for this group.
A number of studies have demonstrated the benefits of exercise on glucose regulation. The U.S. Diabetes Prevention Program reported a 58% reduction in the incidence of type 2 diabetes with an average of 2.8 years (range, 1.8–4.6) of lifestyle intervention that prescribed 150 min/week of moderate-intensity exercise and a dietary program designed to induce a 7% weight loss (6). A similar risk reduction of 58% was associated with lifestyle changes in the Finnish Diabetes Prevention Study (5); and in Asian Indians with impaired glucose tolerance, lifestyle modifications, including 210 min/week of brisk walking and dietary modifications (i.e., reduction in total calorie intake and total fat intake, avoidance of simple sugars and refined carbohydrates, and inclusion of fiber-rich food), resulted in a 28.5% reduced risk of incident diabetes (7). Hu et al. (17) also reported an inverse association between physical activity and the risk of type 2 diabetes for nonobese subjects with normal glucose regulation, as well as subjects who were either obese or showed impaired glucose regulation (mean follow-up = 9.4 years). However, several studies reported that glycemic control did not improve with lifestyle modification and drug therapy (11,12). Krousel-Wood et al. (11) reported that exercise interventions have the potential to reduce BMI in patients with diabetes but not reduce HbA1c. Khan et al. (12) reported that exercise in conjunction with oral drug therapy prescribed for the individual with type 2 diabetes did not directly modify HbAlc levels. These discrepant results might be partly due to differences in the duration of follow-up, prescribed nutritional therapy, and prescribed exercise volume and/or intensity. In the current study, an exercise program (without nutrition intervention) was prescribed and monitored by a qualified health care professional. A strong inverse association between exercise and risk of type 2 diabetes was found among overweight/obese subjects.
Several previous studies reported that impaired glucose regulation appears to best predict future diabetes (18–21). Lifestyle changes have been shown to be effective in preventing both diabetes and obesity in high-risk adults with impaired glucose tolerance (4–6). Compared with normal-weight subjects with NFG who participated in the regular exercise program in the current study, the risk of developing type 2 diabetes for overweight/obese subjects with IFG was 16.3-fold higher in the nonexercise program group and 10.8-fold higher in the exercise program group. This finding that regular exercise reduces the risk of diabetes among obese individuals with IFG is consistent with results of previous clinical trials (4–6).
The strength of the current study was that the exercise program was prescribed and monitored by a qualified health care professional, whereas previous studies often used self-reports of physical activity, which are less accurate and usually result in bias. The limitation of the current study was the lack of randomization of participants to groups (exercise vs. nonexercise program group). In addition, we did not perform the 2-h oral glucose tolerance test on the biennial medical evaluations and during the supervised exercise program study; therefore, the criteria for diabetes (i.e., patient history or fasting glucose levels) may have included some cases of asymptomatic diabetes at baseline or misclassified the glucose status. Misclassification of diabetes would weaken the association between exercise and BMI and the risk of type 2 diabetes. Despite these limitations, the current study shows that regular exercise can reduce the risk of type 2 diabetes in individuals who are overweight or obese, even without dietary changes. The findings indicate that regular exercise and reductions in weight or waist circumference are critical factors in diabetes prevention among overweight or obese individuals with IFG.
Supplementary Material
Acknowledgments
This work was supported by the Korean NHIC and the Midcareer Researcher Program through National Research Foundation of Korea, Republic of Korea (M10642120002-06N4212-00210 and 2012-0005604).
No potential conflicts of interest relevant to this article were reported.
J.S.C., R.K., J.H.K., J.K.P., O.Y.K., M.K., J.W.P., J.Y.J, and J.H.L. analyzed data, developed the study protocol and design, and read, commented on, and contributed to the submitted manuscript. J.H.L. provided the research funding, developed the study protocol and design, and wrote the manuscript. J.H.L. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
The authors thank the research volunteers who participated in the studies described in this article.
Footnotes
This article contains Supplementary Data online at http://care.diabetesjournals.org/lookup/suppl/doi:10.2337/dc11-2074/-/DC1.
J.S.C. and R.K. contributed equally to this work as primary authors.
References
- 1.Haskell WL, Lee IM, Pate RR, et al. American College of Sports Medicine. American Heart Association Physical activity and public health: updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Circulation 2007;116:1081–1093 [DOI] [PubMed] [Google Scholar]
- 2.Marwick TH, Hordern MD, Miller T, et al. Council on Clinical Cardiology, American Heart Association Exercise, Cardiac Rehabilitation, and Prevention Committee. Council on Cardiovascular Disease in the Young. Council on Cardiovascular Nursing. Council on Nutrition, Physical Activity, and Metabolism. Interdisciplinary Council on Quality of Care and Outcomes Research Exercise training for type 2 diabetes mellitus: impact on cardiovascular risk: a scientific statement from the American Heart Association. Circulation 2009;119:3244–3262 [DOI] [PubMed] [Google Scholar]
- 3.Snowling NJ, Hopkins WG. Effects of different modes of exercise training on glucose control and risk factors for complications in type 2 diabetic patients: a meta-analysis. Diabetes Care 2006;29:2518–2527 [DOI] [PubMed] [Google Scholar]
- 4.Pan XR, Li GW, Hu YH, et al. Effects of diet and exercise in preventing NIDDM in people with impaired glucose tolerance. The Da Qing IGT and Diabetes Study. Diabetes Care 1997;20:537–544 [DOI] [PubMed] [Google Scholar]
- 5.Tuomilehto J, Lindström J, Eriksson JG, et al. Finnish Diabetes Prevention Study Group Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med 2001;344:1343–1350 [DOI] [PubMed] [Google Scholar]
- 6.Knowler WC, Barrett-Connor E, Fowler SE, et al. Diabetes Prevention Program Research Group Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med 2002;346:393–403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ramachandran A, Snehalatha C, Mary S, Mukesh B, Bhaskar AD, Vijay V, Indian Diabetes Prevention Programme (IDPP) The Indian Diabetes Prevention Programme shows that lifestyle modification and metformin prevent type 2 diabetes in Asian Indian subjects with impaired glucose tolerance (IDPP-1). Diabetologia 2006;49:289–297 [DOI] [PubMed] [Google Scholar]
- 8.Kosaka K, Noda M, Kuzuya T. Prevention of type 2 diabetes by lifestyle intervention: a Japanese trial in IGT males. Diabetes Res Clin Pract 2005;67:152–162 [DOI] [PubMed] [Google Scholar]
- 9.Lindström J, Ilanne-Parikka P, Peltonen M, et al. Finnish Diabetes Prevention Study Group Sustained reduction in the incidence of type 2 diabetes by lifestyle intervention: follow-up of the Finnish Diabetes Prevention Study. Lancet 2006;368:1673–1679 [DOI] [PubMed] [Google Scholar]
- 10.Li G, Zhang P, Wang J, et al. The long-term effect of lifestyle interventions to prevent diabetes in the China Da Qing Diabetes Prevention Study: a 20-year follow-up study. Lancet 2008;371:1783–1789 [DOI] [PubMed] [Google Scholar]
- 11.Krousel-Wood MA, Berger L, Jiang X, Blonde L, Myers L, Webber L. Does home-based exercise improve body mass index in patients with type 2 diabetes? Results of a feasibility trial. Diabetes Res Clin Pract 2008;79:230–236 [DOI] [PubMed] [Google Scholar]
- 12.Khan S, Rupp J. The effect of exercise conditioning, diet, and drug therapy on glycosylated hemoglobin levels in type 2 (NIDDM) diabetics. J Sports Med Phys Fitness 1995;35:281–288 [PubMed] [Google Scholar]
- 13.Barnett AH, Dixon AN, Bellary S, et al. Type 2 diabetes and cardiovascular risk in the UK south Asian community. Diabetologia 2006;49:2234–2246 [DOI] [PubMed] [Google Scholar]
- 14.Goldberg RB, Temprosa M, Haffner S, et al. Diabetes Prevention Program Research Group Effect of progression from impaired glucose tolerance to diabetes on cardiovascular risk factors and its amelioration by lifestyle and metformin intervention: the Diabetes Prevention Program randomized trial by the Diabetes Prevention Program Research Group. Diabetes Care 2009;32:726–732 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Blair SN. Evidence for success of exercise in weight loss and control. Ann Intern Med 1993;119:702–706 [DOI] [PubMed] [Google Scholar]
- 16.Mourier A, Gautier JF, De Kerviler E, et al. Mobilization of visceral adipose tissue related to the improvement in insulin sensitivity in response to physical training in NIDDM. Effects of branched-chain amino acid supplements. Diabetes Care 1997;20:385–391 [DOI] [PubMed] [Google Scholar]
- 17.Hu G, Lindström J, Valle TT, et al. Physical activity, body mass index, and risk of type 2 diabetes in patients with normal or impaired glucose regulation. Arch Intern Med 2004;164:892–896 [DOI] [PubMed] [Google Scholar]
- 18.Shaw JE, Zimmet PZ, de Courten M, et al. Impaired fasting glucose or impaired glucose tolerance. What best predicts future diabetes in Mauritius? Diabetes Care 1999;22:399–402 [DOI] [PubMed] [Google Scholar]
- 19.Vaccaro O, Ruffa G, Imperatore G, Iovino V, Rivellese AA, Riccardi G. Risk of diabetes in the new diagnostic category of impaired fasting glucose: a prospective analysis. Diabetes Care 1999;22:1490–1493 [DOI] [PubMed] [Google Scholar]
- 20.Gabir MM, Hanson RL, Dabelea D, et al. The 1997 American Diabetes Association and 1999 World Health Organization criteria for hyperglycemia in the diagnosis and prediction of diabetes. Diabetes Care 2000;23:1108–1112 [DOI] [PubMed] [Google Scholar]
- 21.de Vegt F, Dekker JM, Jager A, et al. Relation of impaired fasting and postload glucose with incident type 2 diabetes in a Dutch population: the Hoorn Study. JAMA 2001;285:2109–2113 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.