Abstract
OBJECTIVE
Prospective evaluation of pregnancy outcomes in women with pregestational diabetes over 6 years.
RESEARCH DESIGN AND METHODS
The ATLANTIC Diabetes in Pregnancy group provides care for women with diabetes throughout pregnancy. In 2007, the group identified that women were poorly prepared for pregnancy and outcomes were suboptimal. A change in practice occurred, offering women specialist-led, hub-and-spoke evidence-based care. We now compare outcomes from 2005 to 2007 with those from 2008 to 2010.
RESULTS
There was an increase in the numbers attending preconception care (28–52%, P = 0.01). Glycemic control before and throughout pregnancy improved. There was an overall increase in live births (74–92%, P < 0.001) and decrease in perinatal mortality rate (6.2–0.65%, P < 0.001). There was a decrease in large-for-gestational-age babies in mothers with type 1 diabetes mellitus (30–26%, P = 0.02). Elective caesarean section rates increased, while emergency section rates decreased.
CONCLUSIONS
Changing the process of clinical care delivery can improve outcomes in women with pregestational diabetes.
Pregnancy can pose significant risk to women with type 1 (T1DM) or type 2 (T2DM) diabetes mellitus (1). Optimal care has been shown to decrease these risks. The ATLANTIC Diabetes in Pregnancy (ATLANTIC DIP) group established in 2005 represents five antenatal centers in a wide geographical location along the Irish Atlantic seaboard, covering a population of 500,000. The group provides coordinated care for women with diabetes before, during, and after pregnancy. This report outlines pregnancy outcomes in women with pregestational diabetes, following changes to the process of clinical care delivery.
RESEARCH DESIGN AND METHODS
This is a prospective follow-up study designed to assess outcome after postaudit change in the process of clinical care delivery. The change resulted in the provision of dedicated combined antenatal/diabetes clinics and prepregnancy care (PPC) clinics delivered by specialist diabetes and obstetric staff. Clinical care delivery was supported by a diabetes electronic management system (DIAMOND), locally developed clinical care guidelines based on National Institute for Health and Clinical Excellence (NICE) guidelines (2), and professional and patient education materials. Pregnancy outcomes were compared before (2005–2007) and after (2008–2010) implementation of these changes. PPC involved education, contraceptive advice, provision of folic acid (5 mg) for 12 weeks, discussion of glycemic targets, initiation and/or intensification of insulin, prevention and treatment of hypoglycemia, discontinuation of teratogenic drugs, and management of blood pressure and diabetes-related complications.
All women with diabetes for >6 months before the index pregnancy were included. Five values of HbA1C were chosen to represent metabolic control; those recorded at the first obstetric visit; 12, 24, and 36 weeks’ gestation; and before delivery. Large for gestational age (LGA) was defined as birth weight >90th centile, and small for gestational age was defined as birth weight <10th centile. All congenital malformations, major and minor, were included. Preeclampsia was defined as blood pressure >140/90 mmHg with proteinuria after 20 weeks’ gestation. Maternal BMI (measured as kilograms divided by the square of height in meters) was assessed at the first obstetrical visit. Target HbA1C was <7%/53 mmol.
RESULTS
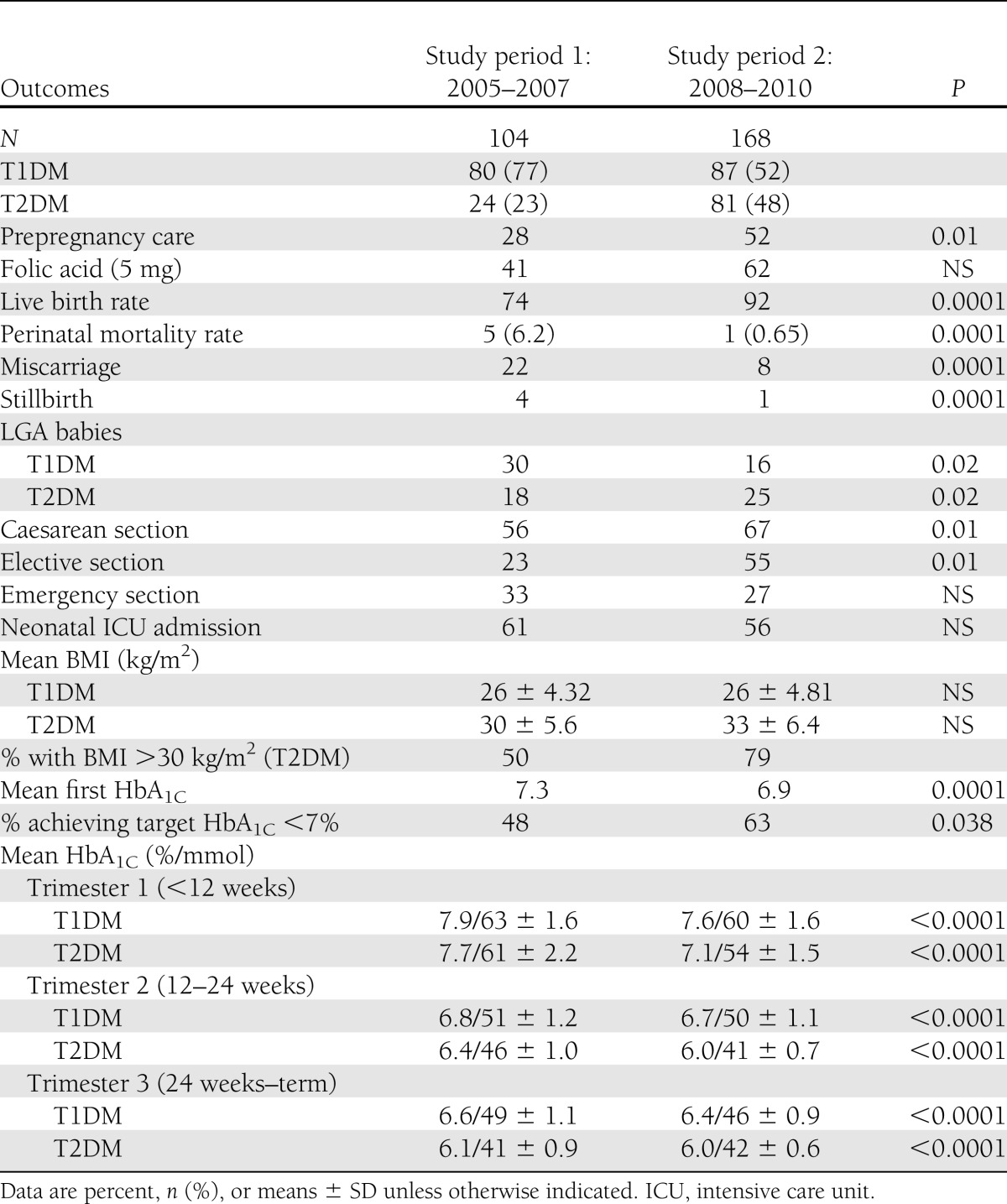
Two hundred seventy-two pregnancies were examined over a 6-year period; 61% had T1DM, and 39% had T2DM. There was an increase in the numbers of pregnancies in women with T2DM over time, in line with the increasing incidence in the background population (Table 1).
Table 1.
Pregnancy outcomes comparing period 1 (2005–2007) with period 2 (2008–2010) for ATLANTIC DIP
Between periods 1 and 2, the number of women receiving prepregnancy care increased by twofold (P = 0.01) (Table 1). There was a nonsignificant increase in the number receiving folic acid prepregnancy (P = 0.2). Overall, the first recorded HbA1C decreased from a mean of 7.3 to 6.9% (P < 0.001), and the number of women achieving HbA1C <7% at their booking visit increased significantly (P = 0.038). Glycemic control improved significantly throughout pregnancy for women with both T1DM and T2DM (Table 1).
There was a significant improvement in pregnancy outcomes. The live birth rate increased from 74 to 92% (P < 0.0001), and miscarriages and stillbirths decreased between the study periods (Table 1). Overall, perinatal mortality fell from 5 (6.2%) to 1 (0.65%). Congenital malformations were unchanged; however, there were no malformations recorded in women attending PPC. Preeclampsia rates were unchanged (11.5%). There was a significant decrease in number of babies born LGA in women with T1DM (P = 0.02). Conversely, however, there was a significant increase in babies born LGA in women with T2DM (P = 0.02). There was no change in numbers born small for gestational age. Caesarean section rates increased overall, with an increase in elective rates from and a nonsignificant reduction in emergency section rate (Table 1). In addition, there was a nonsignificant reduction in the number of babies admitted to neonatal intensive care.
Mean booking BMI was unchanged (mean 26 kg/m2) in women with T1DM. In comparison, mean BMI of women with T2DM increased from 30 to 34 kg/m2 between the two time intervals (P = 0.034). More women with T2DM were obese (BMI >30 kg/m2) in time period 2 compared with time period 1 (P = 0.04).
CONCLUSIONS
Pregestational diabetes occurs in approximately 1 in 250 pregnancies, and prevalence is increasing (3) worldwide. Pregnancies in women with pregestational diabetes are associated with increased maternal and neonatal morbidity and mortality, as has been demonstrated by studies including the Confidential Enquiry into Maternal and Child Health (CEMACH) diabetes report (3) and by this study group (1).
Maternal complications include higher rates of caesarean delivery (3), worsening of preexisting retinopathy (5) and nephropathy (6), and higher rates of hypertension and preeclampsia (3). Fetal/neonatal complications include higher perinatal mortality rates (2), more LGA babies associated with shoulder dystocia and caesarean delivery (7), and more congenital malformations (2,8) and premature delivery (9).
PPC (10) including optimization of glycemic control is associated with an improvement in these outcomes. Early pregnancy glycemic control, more so than late, decreases the risk of delivering a macrosomic infant (11). Glycemic control also decreases the risk of miscarriage and malformation (12). Animal studies have shown that folic acid use decreases the incidence of fetal malformation (13).
ATLANTIC DIP aims to provide coordinated, specialist-delivered, evidence-based care to women before, during, and after pregnancy. In 2007, outcomes were compared with that of the background population and were found to be suboptimal, with stillbirth 5 times, perinatal mortality 3.5 times, and congenital anomalies twice that of the background population (1). These results are similar to those reported by previous population-based studies (3,14). In addition, women were poorly prepared for pregnancy, with only 28% of women attending PPC, 43% taking folic acid prior to pregnancy, and one-half entering pregnancy with an HbA1C <7% (1). These results are similar to those reported by previous population-based studies (3,14). There have been few similar studies, but previous intensive pregnancy care programs have been shown to be similarly effective (15).
Following these results, ATLANTIC DIP concentrated on changing the process of clinical care delivery and developed combined antenatal/diabetes clinics and dedicated PPC clinics, electronic data collection, clinical care guidelines, and professional and patient education materials, aiming to “close the audit loop.” We have now subsequently compared outcomes and found that more women are attending PPC, with better glycemic control resulting in a decrease in miscarriage and stillbirth rates and an increase in take-home-baby rate. There have been few similar studies, but intensive pregnancy care programs have been shown to be similarly effective (15). T2DM in pregnancy is becoming more common, and these women are becoming more obese and delivering more macrosomic babies. Further work is required for optimization of this cohort of women.
Acknowledgments
No potential conflicts of interest relevant to this article were reported.
L.A.O. was the main author of the manuscript. G.A. was the statistician and data analyst and was involved in the production of the results. B.K. and L.C. contributed to data collection and the production of the results. F.D. was the chairperson of the group, edited data, and contributed to discussion. F.D. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Parts of this study were presented in poster form at the 72nd Scientific Sessions of the American Diabetes Association, Philadelphia, Pennsylvania, 8–12 June 2012.
The authors acknowledge the ATLANTIC DIP collaborators.
References
- 1.Dunne FP, Avalos G, Durkan M, et al. ; ATLANTIC DIP collaborators. ATLANTIC DIP: pregnancy outcome for women with pregestational diabetes along the Irish Atlantic seaboard. Diabetes Care 2009;32:1205–1206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.National Institute for Health and Clinical Excellence. Diabetes in pregnancy; management of diabetes and its complications from pre-conception to the post-natal period, clinical guideline 63 [article online], 2008. Available from www.nice.org.uk/nicemedia/pdf/CG063Guidance.pdf Accessed 29 October 2011
- 3.Confidential Enquiry into Maternal and Child Health. Diabetes in Pregnancy: Are We Providing the Best Care? London, CEMACH, 2007 [Google Scholar]
- 4.Persson M, Norman M, Hanson U. Obstetric and perinatal outcomes in type 1 diabetic pregnancies: A large, population-based study. Diabetes Care 2009;32:2005–2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Star J, Carpenter MW. The effect of pregnancy on the natural history of diabetic retinopathy and nephropathy. Clin Perinatol 1998;25:887–916 [PubMed] [Google Scholar]
- 6.Reece EA, Coustan DR, Hayslett JP, et al. Diabetic nephropathy: pregnancy performance and fetomaternal outcome. Am J Obstet Gynecol 1988;159:56–66 [DOI] [PubMed] [Google Scholar]
- 7.Boulet SL, Alexander GR, Salihu HM. Secular trends in cesarean delivery rates among macrosomic deliveries in the United States, 1989 to 2002. J Perinatol 2005;25:569–576 [DOI] [PubMed] [Google Scholar]
- 8.Greene MF. Spontaneous abortions and major malformations in women with diabetes mellitus. Semin Reprod Endocrinol 1999;17:127–136 [DOI] [PubMed] [Google Scholar]
- 9.Carter MF, Fowler S, Holden A, Xenakis E, Dudley D. The late preterm birth rate and its association with comorbidities in a population-based study. Am J Perinatol 2011;28:703–707 [DOI] [PubMed] [Google Scholar]
- 10.Pearson DW, Kernaghan D, Lee R, Penney GC, Scottish Diabetes in Pregnancy Study Group The relationship between pre-pregnancy care and early pregnancy loss, major congenital anomaly or perinatal death in type I diabetes mellitus. BJOG 2007;114:104–107 [DOI] [PubMed] [Google Scholar]
- 11.Rey E, Attié C, Bonin A. The effects of first-trimester diabetes control on the incidence of macrosomia. Am J Obstet Gynecol 1999;181:202–206 [DOI] [PubMed] [Google Scholar]
- 12.Ylinen K, Aula P, Stenman UH, Kesäniemi-Kuokkanen T, Teramo K. Risk of minor and major fetal malformations in diabetics with high haemoglobin A1c values in early pregnancy. Br Med J (Clin Res Ed) 1984;289:345–346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Oyama K, Sugimura Y, Murase T, et al. Folic acid prevents congenital malformations in the offspring of diabetic mice. Endocr J 2009;56:29–37 [DOI] [PubMed] [Google Scholar]
- 14.Jensen DM, Damm P, Moelsted-Pedersen L, et al. Outcomes in type 1 diabetic pregnancies: a nationwide, population-based study. Diabetes Care 2004;27:2819–2823 [DOI] [PubMed] [Google Scholar]
- 15.Murphy HR, Roland JM, Skinner TC, et al. Effectiveness of a regional prepregnancy care program in women with type 1 and type 2 diabetes: benefits beyond glycemic control. Diabetes Care 2010;33:2514–2520 [DOI] [PMC free article] [PubMed] [Google Scholar]