Abstract
BACKGROUND
To the authors’ knowledge, the effects of supraclavicular fossa radiation on the carotid artery are not well described. In the current study, the authors performed a prospective study to examine the long-term risk of carotid artery stenosis after supraclavicular irradiation for breast cancer.
METHODS
A total of 46 breast cancer patients who were treated with adjuvant radiation to the supraclavicular fossa with >8 years of follow-up underwent bilateral Doppler imaging of the carotid artery. Two independent cardiologists interpreted each ultrasound study with no knowledge of which side was treated.
RESULTS
The median follow-up from the date of diagnosis was 14.6 years and the mean patient age at the time of ultrasound was 55 years. The median prescribed dose to the supraclavicular fossa was 50 grays. Four patients were found to have clinically relevant, asymptomatic carotid stenosis, for which a cardiology referral was necessary. Only 1 of these 4 patients had stenosis involving the irradiated carotid artery only; 1 patient had bilateral stenosis and 2 patients had only contralateral stenosis. There was no difference noted with regard to isolated ipsilateral versus contralateral medial intimal thickening of the carotid artery (5 patients vs 6 patients, respectively). Furthermore, there were no differences noted with regard to ipsilateral versus contralateral peak systolic flow in the internal (83.5 vs 85.6 cm/seconds; P =.522 by the Student t test and P =.871 by the signed rank test) or common (74.4 vs 77.0 cm/seconds; P =.462 by the Student t test and P =.246 by the signed rank test) carotid artery.
CONCLUSIONS
In this prospective study of breast cancer patients with long follow-up, there was no evidence of late, clinically relevant stenosis, increased intimal thickening, or increased peak systolic carotid artery flow secondary to supraclavicular irradiation.
Keywords: breast radiation, supraclavicular, carotid artery, stenosis, late effects
Recognition that radiotherapy for breast cancer is associated with an increased risk of cardiovascular injury prompted significant research into developing treatment techniques designed to limit the radiation dose to the heart. Three-dimensional treatment planning currently allows for the careful shaping/design of radiation fields to avoid irradiating the heart and coronary arteries. As such, many have speculated that the number of cardiovascular injuries reported from trials conducted during the 1950s through 1970s will likely be significantly reduced with these newer techniques, and indeed, the most recent meta-analysis from the Early Breast Cancer Trialists’ Collaborative Group clearly demonstrates the overall survival benefit of modern radiation treatment.1 In older studies in which the dose to cardiac structures was not specifically limited, excess deaths were reported generically as cardiovascular deaths, not distinguishing between death from heart attack and death from stroke.2 Therefore, these reports did not specifically address whether incidental radiation of the carotid artery occurring when the supraclavicular fossa is treated may contribute to late toxicity and limit the effectiveness of radiotherapy.
In the current study, we invited women treated with unilateral supraclavicular radiation ≥8 years previously to undergo bilateral carotid Doppler ultrasounds to examine the impact of radiation on the flow of blood through the carotid artery. The study was designed to compare Doppler measurements on the treated side with those on the untreated side. These data are particularly important because techniques for irradiating the supraclavicular fossa have not changed dramatically over the years, and technology is available to limit the dose to the carotid artery if it was clinically warranted.
MATERIALS AND METHODS
We have recently established an up-to-date database of greater than 1500 breast cancer patients treated with mastectomy and adjuvant chemotherapy on prospective institutional clinical trials conducted between 1975 and 1994. The objective of these clinical trials was to investigate the benefits of doxorubicin-based chemotherapy. In these trials, radiation was given at the discretion of the treating physicians. The database included 470 patients who received postmastectomy radiation and 1031 patients who were treated with mastectomy and chemotherapy alone. The patients receiving radiation were treated with relatively standardized techniques and all received treatment to the supraclavicular fossa. This region was treated with megavoltage radiation to a median dose of 50 grays (Gy) in 25 daily fractions delivered over 5 weeks. The methods and dosage used to treat the supraclavicular fossa in these patients were very similar to the treatment techniques and dosages used currently (Fig. 1). With the limited information available concerning causes of nonbreast cancer-related death, we did not identify any deaths due to stroke among the 470 patients treated with radiation. We identified 180 patients treated with supraclavicular radiation who were alive at the time of the study and this cohort had a median follow-up of >8 years.
FIGURE 1.
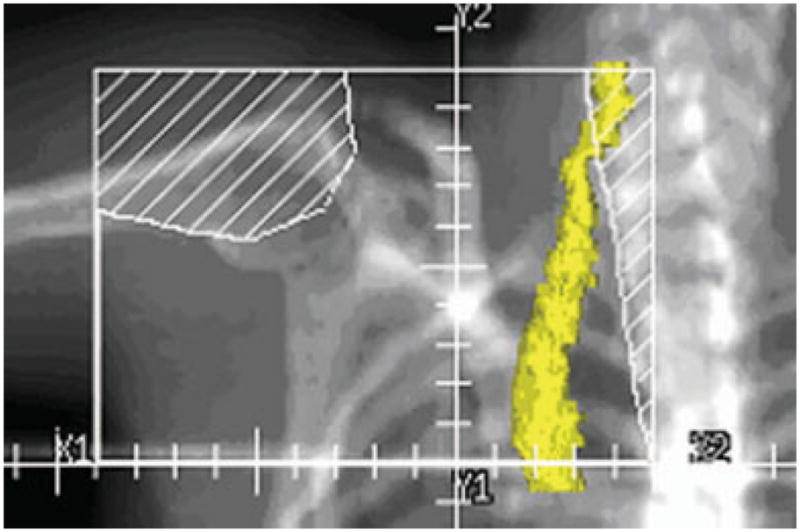
Representative supraclavicular field. The ipsilateral common carotid artery (yellow) often is partially within the radiation field (45 Gray to ~50% of the volume in this example). The internal carotid artery (superior to the field border) is unlikely to receive the radiation dose in patients without positive supraclavicular lymph nodes.
After obtaining approval from the Institutional Surveillance Committee, the identified patients with a minimum follow-up of 8 years after receiving radiotherapy to the supraclavicular fossa were contacted by mail and invited to participate in this study. To minimize bias, we began by recruiting consecutive patients, beginning with those with the longest follow-up. After informed consent was obtained, each participant filled out a case report form that included the following information: age, weight, menopausal status, history of cerebrovascular events, hypertension, diabetes, coronary artery disease, smoking history, and medications. Participants then underwent a physical examination and had 10 cc of blood drawn for a cholesterol panel and c-reactive protein and homocysteine levels and 10 cc of blood drawn to store serum and DNA for future studies. The rationale for studying the cholesterol panel and c-reactive protein and homocysteine levels was that all these factors have been previously described to correlate with the risk of atherosclerotic disease.
All participants underwent a bilateral Doppler ultrasound of the carotid artery performed in the Department of Cardiology and interpreted by 2 independent cardiologists who were blinded to the side treated with supraclavicular radiation. Determination of the need for cardiology referral based on the degree of stenosis was made by the interpreting cardiologist and explicitly reported on a unique reporting form for each case. Each participant served as their own control (irradiated carotid artery vs unirradiated carotid artery), thereby eliminating the numerous potential confounding variables that can affect rates of cardiovascular disease. Patients with clinically significant lesions were referred to the cardiology department and treated in accordance with the standard of care for such lesions.
Statistical Analysis
Paired analyses were used to control for variability in baseline risk factors for carotid artery disease between patients. The planned accrual was 100 patients. Approximately half of the accrual goal was met after 2 mailings. The study was closed after the accrual of 46 patients. Given the event rate of approximately 10%, the study is underpowered to demonstrate a difference, with a P value < .05 (1-sided assuming radiotherapy would increase the risk of clinically significant stenosis). The numeric flow data from the carotid artery screening studies were analyzed using the Student t test and signed rank comparisons.
RESULTS
Study Population
A total of 180 patients were invited to participate through a mailing, 25% of whom agreed to participate. Therefore, 92 ultrasounds were performed on 46 patients. The median follow-up from the date of the original diagnosis in the studied patients was 14.6 years. The mean age of the study population at the time of ultrasound was 55 years. The median dose to the supraclavicular fossa was 50 Gy. One patient reported a history of myocardial infarction (not requiring cardiology referral) and no patients reported a history of stroke. One patient reported a history of transient ischemic attack (not requiring a cardiology referral), and 5 patients reported a diagnosis of type 2 diabetes insipidus (1 patient in the referral group). The mean total cholesterol level was 202 mg/dL (normal value, 120–200 mg/dL), the high density lipoprotein was 57 mg/dL (normal < 55 mg/dL), low density lipoprotein was 116 mg/dL (normal, 74–186 mg/dL), homocysteine was 9.5 mg/L (normal, 5–13 mg/L; repeat values > 10 mg/L are considered abnormal), and the mean smoking pack-years was 7.7 years. Raw data for the entire cohort are presented in Table 1.
TABLE 1.
Patient and Serum Data for All Patients in the Study*
| HTN | BB | ASA | CHOL | TG | HDL | CRP | HCSY | Pack-Year | OCP | HRT | TAM |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Yes | Yes | Yes | 245 | 196 | 55 | 1.79 | 13.9 | 5 | No | No | No |
| Yes | Yes | Yes | 235 | 222 | 44 | 0.27 | 0 | No | No | No | |
| Yes | Yes | Yes | 190 | 133 | 53 | 0.1 | 11.2 | 0 | No | No | Yes |
| No | No | No | 215 | 204 | 31 | 0.89 | 11.1 | 0 | No | No | |
| Yes | Yes | Yes | 151 | 83 | 77 | 0.52 | 9.8 | 0 | Yes | Yes | No |
| Yes | No | Yes | 196 | 365 | 34 | 9.34 | 11.4 | 30 | Yes | Yes | Yes |
| Yes | No | No | 206 | 221 | 70 | 0.62 | 19.7 | 0 | No | No | No |
| Yes | No | Yes | 180 | 148 | 54 | 0.23 | 14.4 | 0 | Yes | Yes | No |
| Yes | No | Yes | 217 | 222 | 46 | 0.13 | 7.0 | 0 | Yes | No | No |
| No | Yes | Yes | 217 | 206 | 62 | 0.22 | 6.1 | 8 | No | No | Yes |
| No | Yes | No | 177 | 67 | 61 | < 0.10 | 5.6 | 0 | Yes | No | No |
| No | Yes | No | 217 | 66 | 60 | < 0.10 | 6.5 | 0 | No | No | No |
| No | No | No | 218 | 69 | 45 | 11.59 | 11.8 | 0 | Yes | No | Yes |
| No | No | Yes | 122 | 118 | 44 | 1.78 | 14.6 | 0 | Yes | No | No |
| No | No | No | 173 | 94 | 59 | 1.17 | 5.3 | 0 | Yes | No | No |
| No | No | No | 197 | 116 | 53 | 1 | 11.0 | 13 | Yes | No | Yes |
| No | No | No | 192 | 68 | 63 | 0.95 | 4.6 | 24 | Yes | No | No |
| No | No | No | 180 | 196 | 38 | 0.92 | 6.9 | 0 | Yes | No | |
| No | No | No | 185 | 114 | 61 | 0.69 | 8.1 | 15 | Yes | No | No |
| No | No | Yes | 193 | 83 | 75 | 0.61 | 9.2 | 4 | Yes | Yes | No |
| No | No | No | 212 | 131 | 43 | 0.59 | 10.4 | 30 | Yes | No | No |
| No | No | Yes | 254 | 158 | 56 | 0.57 | 9.1 | 90 | Yes | Yes | No |
| No | No | No | 217 | 126 | 79 | 0.43 | 9.3 | 10 | Yes | No | No |
| No | No | No | 181 | 72 | 59 | 0.42 | 10.1 | 0 | Yes | No | No |
| No | No | No | 285 | 239 | 42 | 0.4 | 7.0 | 0 | No | No | No |
| No | No | No | 176 | 202 | 58 | 0.38 | 2 | Yes | No | No | |
| No | No | No | 147 | 131 | 50 | 0.34 | 7.3 | 0 | No | No | No |
| No | No | No | 187 | 82 | 49 | 0.27 | 9.2 | 0 | Yes | No | No |
| No | No | No | 216 | 338 | 56 | 0.25 | 9.9 | 0 | Yes | No | Yes |
| No | No | No | 193 | 176 | 59 | 0.24 | 7.4 | 0 | Yes | No | No |
| No | No | No | 276 | 180 | 63 | 0.21 | 10.7 | 0 | No | Yes | No |
| No | No | No | 217 | 417 | 33 | 0.16 | 7.3 | 0 | Yes | No | No |
| No | No | No | 192 | 189 | 50 | 0.13 | 14.5 | 20 | No | Yes | Yes |
| No | No | No | 231 | 71 | 57 | 0.11 | 12.4 | 25 | Yes | No | No |
| No | No | No | 199 | 55 | 55 | < 0.10 | 11.7 | 0 | Yes | No | Yes |
| No | No | No | 274 | 88 | 65 | < 0.10 | 6.6 | 0 | No | No | No |
| No | No | Yes | 192 | 76 | 89 | < 0.1 | 6.6 | 0 | Yes | Yes | No |
| No | No | No | 187 | 59 | 85 | < 0.1 | 7.8 | 0 | Yes | No | No |
| No | No | No | 218 | 67 | 84 | < .10 | 11.3 | 26 | Yes | No | Yes |
| No | No | Yes | 207 | 213 | 47 | < .10 | 10.2 | 0 | Yes | Yes | Yes |
| No | No | Yes | 147 | 74 | 46 | < .10 | 12.8 | 3 | Yes | No | Yes |
| No | No | Yes | 167 | 92 | 51 | < .10 | 7.3 | 2 | Yes | No | No |
| No | No | No | 213 | 82 | 86 | < .10 | 7.6 | 0 | Yes | No | Yes |
| No | No | No | 223 | 102 | 62 | < .10 | 8.7 | 25 | Yes | No | No |
| No | No | No | 187 | 123 | 46 | < .10 | 7.0 | 23 | Yes | No | No |
| No | No | No | 171 | 81 | 64 | < .10 | 0 | No | No | No |
HTN indicates hypertension; BB, beta blockers; ASA, history of daily aspirin use; CHOL, cholesterol; TG, triglyceride; HDL, high-density lipoprotein; CRP, c-reactive protein; HCSY, homocysteine; OCP, ; HRT, hormone replacement therapy; TAM, tamoxifen.
The first 4 rows (shown in bold) represent patients who required a cardiology referral based on Doppler imaging. Values highlighted in blue are abnormal based on the normal range of the performing laboratory.
Results of the Carotid Study
Four patients were found to have clinically relevant, asymptomatic carotid artery stenosis, for which a cardiology referral was necessary. Only 1 of these 4 patients had a stenosis involving only the irradiated carotid artery. One patient had bilateral stenosis of both carotid arteries that was equal in magnitude and 2 patients had only a contralateral stenosis (Fig. 2). There was no difference noted with regard to the incidence of isolated ipsilateral versus contralateral medial intimal thickening of the carotid artery (5 patients vs 6 patients, respectively). Furthermore, there were no differences noted with regard to ipsilateral versus contralateral peak systolic flow in the internal (83.5 vs 85.6 cm/seconds; P =.522 by the Student t test and P =.871 by the signed rank test) or common (74.4 vs 77.0 cm/seconds; P =.462 by the Student t test and P =.246 by the signed rank test) carotid arteries (Fig. 3). Factors found to be significant predictors of a cardiology referral were hypertension (75% among the referral group and 12% among the nonreferral group; P =.001) and medications associated with a diagnosis of hypertension including beta blockers (75% vs 10%; P <.0001) and aspirin (75% vs 29%; P =.058). Dyslipidemia, an abnormal c-reactive protein level, and an elevated homocysteine level did not appear to be correlated with referral to the cardiology department based on Doppler imaging results. No patient requiring a cardiology referral had a history of hormone replacement therapy or oral contraceptive use.
FIGURE 2.
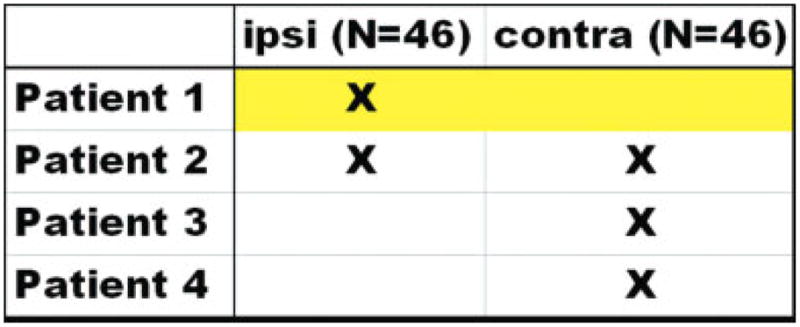
Of the 4 patients requiring a cardiology referral for significant stenosis, only 1 patient (highlighted in yellow) was found to have a stenosis on the treated side alone ipsi indicates ipsilateral; contra, contralateral.
FIGURE 3.
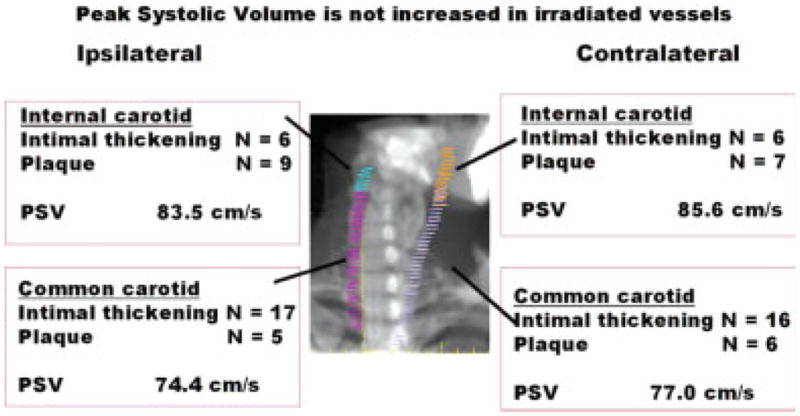
The number, type, and location of lesions identified by ultrasound. For peak systolic volume (PSV) (ipsilateral vs contralateral), the P value was not found to be significant for each vessel using the Student t test and the signed rank test.
DISCUSSION
It is estimated that nearly 100,000 women each year receive radiotherapy for breast cancer, and many of these patients require irradiation of the supraclavicular fossa as a component of treatment. For the majority of women with lymph node-positive disease, treatment of this region is indicated to reduce the risk of disease recurrence in the undissected axilla (level III) and supraclavicular lymph nodes. An unfortunate consequence of treatment of the supraclavicular fossa is irradiation of the ipsilateral carotid artery. The fact that the contralateral carotid artery is not exposed to radiation provided us with a unique opportunity to quantify the risks of carotid artery radiation. Using the contralateral carotid artery of each patient as a control provided us with a way to adjust for known and unknown factors influencing the risk of carotid artery disease. We found that, at the doses used for breast cancer, there was no evidence of an increase in clinically relevant stenosis related to supraclavicular irradiation delivered >8 years earlier, and that supra-clavicular radiation did not increase the incidence of the classic radiation-induced vascular injury, medial intimal thickening of in-field vessels.
One rationale for studying carotid injury after radiotherapy for breast cancer comes from a meta-analysis of the data from 40 mature randomized trials that investigated the use of radiotherapy for breast cancer.2 The analysis specifically implicated cardiovascular events as a significant cause of non-breast cancer death among breast cancer patients treated with radiation (P =.0007). These observed cardiovascular injuries developed many years after the initial radiation treatment. Specifically, the ratio of annual nonbreast cancer-related death rates between the unirradiated and irradiated groups was not significantly different up to 9 years after treatment. However, after ≥10 years, the ratio was 30% higher in those patients treated with radiotherapy.2
The Early Breast Cancer Trialists’ Collaborative Group meta-analysis has recently been updated. Although investigation of the impact of changes in technique on long-term outcomes over time was not explicitly the objective of this study, improvements in radiation technique appear to have improved the balance between a decreased rate of breast cancer deaths and radiation-related cardiac disease.1 In addition, the incidence of stroke was reported for what to our knowledge is the first time in this study. Although the ratio of rates of stroke in the radiated and unirradiated groups indicated a slightly higher risk of stroke among patients who received radiation, this difference was not found to be statistically significant (ratio of rates 1.12; P = 0.3).
Although the data regarding radiation-related death from stroke reported by the Early Breast Cancer Trialists’ Collaborative Group is reassuring, the authors state that examination of late radiation effects in this study was only semiquantitative and, even with the availability of individual patient data, the reporting of very late events can often be variable. In addition, because these data included many women with early-stage disease who were treated with breast conservation therapy, it is likely that many of the women in the radiotherapy group did not receive any dose to the supraclavicular fossa. In the current study, we explicitly examined not only the clinical endpoint of stroke but also the initiating events of medial intimal thickening and the disruption of carotid artery flow in vessels ipsilateral to supraclavicular radiation and found no evidence of any radiation-induced clinical alteration of the vessels. The radiation-induced morphologic and pathologic changes in large vessels have been examined and reported in both human and large animal studies and are indistinguishable from atherosclerotic changes characterized by medial intimal thickening.3,4 This study is unique in that it allows for the specific assessment of this characteristic change. We reported no difference with regard to intimal medial thickening and found no evidence of altered carotid artery flow that was correlated with radiation to the supraclavicular fossa.
With regard to the intended endpoint to compare rates of clinically relevant stenosis in irradiated versus unirradiated carotid arteries, the current study is limited by its failure to meet the accrual, making it underpowered to demonstrate equivalence. In addition, it should be noted that, as in any mailing survey, a self-selection bias exists that may further influence the results. This study likely evaluated the carotid artery flow of patients with minimal cardiovascular morbidity because patients with significant morbidity may have been less likely to respond to the invitation. Indeed, only 1 respondent reported a history of transient ischemic attack and only 1 patient had a history of myocardial infarction. Nevertheless, fewer events in the radiated group as well as the similar findings regarding medial thickening and quantitative measures of carotid artery flow between both groups are reassuring. The current study data are consistent with 3 recent reports confirming the lack of correlation between supraclavicular radiation and stroke. In a study of 820 breast cancer patients who were treated with radiation as a component of breast conservation therapy, the authors found no evidence that radiation to the supraclavicular fossa was associated with an increased risk of experiencing a cerebrovascular accident.5 This cohort had a median age of 56 years and included 40 patients who were aged <35 years, accounting for the overall low rate of cerebrovascular accidents reported for the entire cohort: 2.7% at 10 years. Age was found to be the only predictor for cerebrovascular accident on multivariate analysis. In a similar Surveillance, Epidemiology, and End Results (SEER)-based analysis of 5752 breast cancer patients aged >66 years, we reported no increase in the rate of hospitalization for stroke among the 471 patients with ≥4 positive lymph nodes (surrogate for supraclavicular radiation, 10.5%) compared with the 5281 patients with no positive lymph nodes (surrogate for no supraclavicular radiation, 10%)6 The median follow-up in this study was 90 months. A third retrospective study from the Netherlands Cancer Institute examined the rates of transient ischemic attack and stroke among women treated for early-stage breast cancer and again reported no increased risk of stroke among women who received radiotherapy specifically to the supraclavicular fossa (hazards ratio of 1.0).7 This report had what to our knowledge was the longest follow-up period published to date at 18 years and included only those women who survived for >10 years after treatment. An increased risk of stroke was associated with hormonal therapy, hypertension, and hypercholesterolemia (hazards ratios of 1.9, 2.1, and 1.6, respectively).
Both prospective and retrospective data have implicated radiation in increasing the risk of carotid stenosis after radiotherapy for head and neck cancer.8–11 These data highlight the importance of dose and volume (both of which are greater in the treatment of head and neck cancer) in determining late radiation effects. The total dose to the supraclavicular fossa for breast cancer patients is generally prescribed to ≤50 Gy, and the position of the carotid artery at the edge of the field means that it will generally receive significantly less than the prescription dose, in some cases 50% less. In addition, contrary to typical radiation treatment for head and neck malignancies, the full length of the carotid artery rarely would be included in the typical supraclavicular field. Special situations in breast cancer (ie, the presence of persistent macroscopic disease in the lymph nodes) in which the supraclavicular fossa is treated to a larger volume and higher total dose are not addressed in the current study or, to our knowledge, the published literature to date. However, from the data presented herein in conjunction with the previously mentioned studies of radiation to the carotid artery in patients being treated for breast cancer, it can be concluded that the techniques currently used to irradiate the supraclavicular fossa do not increase the likelihood of carotid pathology or clinical consequences thereof, and that the development of more costly alternative techniques to limit the radiation dose to the carotid artery during standard adjuvant breast cancer irradiation does not appear to be warranted. Additional studies are needed to specifically evaluate those women with an increased baseline risk of cardiovascular disease and women treated with definitive radiation doses to the supraclavicular region.
Acknowledgments
Supported in part by National Cancer Institute Grants CA16672 and T32CA77050.
Footnotes
Presented at the American Society for Therapeutic Radiology and Oncology Annual Meeting, October 16–20, 2005, Denver, Colorado.
References
- 1.Clarke M, Collins R, Darby S, et al. Effects of radiotherapy and of differences in the extent of surgery for early breast cancer on local recurrence and 15-year survival: an overview of the randomised trials. Lancet. 2006;366:2087–2106. doi: 10.1016/S0140-6736(05)67887-7. [DOI] [PubMed] [Google Scholar]
- 2.Favourable and unfavourable effects on long-term survival of radiotherapy for early breast cancer: an overview of the randomised trials. Early Breast Cancer Trialists’ Collaborative Group. Lancet. 2000;355:1757–1770. [PubMed] [Google Scholar]
- 3.Moss WT. The heart and blood vessels. In: Brand WN, Battifora H, editors. Radiation Oncology, Rationale, Technique, Results. St. Louis: CV Mosby Co; 1973. pp. 248–256. [Google Scholar]
- 4.Fonkalsrud EW, Sanchez M, Zerubavel R, Mahoney A. Serial changes in arterial structure following radiation therapy. Surg Gynecol Obstet. 1977;145:395–400. [PubMed] [Google Scholar]
- 5.Jagsi R, Griffith KA, Koelling T, Roberts R, Pierce LJ. Stroke rates and risk factors in patients treated with radiation therapy for early-stage breast cancer. J Clin Oncol. 2006;24:2779–2785. doi: 10.1200/JCO.2005.04.0014. [DOI] [PubMed] [Google Scholar]
- 6.Woodward WA, Giordano SH, Duan Z, Hortobagyi GN, Buchholz TA. Supraclavicular radiation for breast cancer does not increase the 10-year risk of stroke. Cancer. 2006;106:2556–2562. doi: 10.1002/cncr.21943. [DOI] [PubMed] [Google Scholar]
- 7.Hooning MJ, Dorresteijn LD, Aleman BM, et al. Decreased risk of stroke among 10-year survivors of breast cancer. J Clin Oncol. 2006;24:5388–5394. doi: 10.1200/JCO.2006.06.5516. [DOI] [PubMed] [Google Scholar]
- 8.Dorresteijn LD, Kappelle AC, Boogerd W, et al. Increased risk of ischemic stroke after radiotherapy on the neck in patients younger than 60 years. J Clin Oncol. 2002;20:282–288. doi: 10.1200/JCO.2002.20.1.282. [DOI] [PubMed] [Google Scholar]
- 9.Lam WW, Leung SF, So NM, et al. Incidence of carotid stenosis in nasopharyngeal carcinoma patients after radiotherapy. Cancer. 2001;92:2357–2363. doi: 10.1002/1097-0142(20011101)92:9<2357::aid-cncr1583>3.0.co;2-k. [DOI] [PubMed] [Google Scholar]
- 10.Conomy JP, Kellermeyer RW. Delayed cerebrovascular consequences of therapeutic radiation. A clinicopathologic study of a stroke associated with radiation-related carotid arteriopathy. Cancer. 1975;36:1702–1708. doi: 10.1002/1097-0142(197511)36:5<1702::aid-cncr2820360525>3.0.co;2-v. [DOI] [PubMed] [Google Scholar]
- 11.Elerding SC, Fernandez RN, Grotta JC, Lindberg RD, Causay LC, McMurtrey MJ. Carotid artery disease following external cervical irradiation. Ann Surg. 1981;194:609–615. doi: 10.1097/00000658-198111000-00009. [DOI] [PMC free article] [PubMed] [Google Scholar]


