Abstract
The relation between history of violence exposure and the development of academic and mental health problems is explored. Violence exposed children have an increased risk of developing school-related problems including: mental health problems, learning disabilities, language impairments, and other neurocognitive problems. These problems interact to create a complex web of deficits and disabilities where intervention access points are difficult to assess. Often mental health problems and academic problems develop in parallel. Timing of violence exposure and the developmental stage of the child during exposure complicate our understanding of the underlying mechanism. A model is presented that explores pathways linking violence exposure to aspects of school-related functioning, both academically and behaviorally. Early life stress, in the form of violence exposure, is related to neurocognitive deficits, including executive functioning and problems in self-regulation. Deficits in self-regulation at the level of behavior, and cognitive control and executive functioning, at the level of brain processing, are related to both academic and mental health problems, suggesting a possible psychological mechanism. Biological mechanisms are also included in the model to illustrate the contribution of the stress response, neuroendocrine system response, and neuroanatomical structural and functional impairments associated with violence exposure.
Keywords: Child maltreatment, language impairment, disability, externalizing behavior, internalizing behavior, self-regulation
Introduction1
Exposure to violence is related to problems in school functioning, including mental health, cognitive processing and language development. These problems interact to create a complex web of disabilities where intervention access points are difficult to assess. Children with histories of violence exposure are often referred for mental health services at an early age and frequently develop emotional, and behavioral disorders. The cost to both individuals and to society is large. One in eight children experiences some form of maltreatment (Finkelhor, Ormrod, Turner, & Hamby, 2005), as either abuse or the neglect of proper care. Abuse has particular repercussions for the development of school skills such as language learning, cognitive processing and self-regulation. Interpersonal violence and community violence experienced in childhood are related to myriad psychosocial problems including, attachment problems, speech, language and social interactions, delays in emotion processing, and intellectual and behavior problems (Azar & Wolfe, 2006). A better understanding of the developmental trajectory of the relation between school-related function and violence exposure, at both the level of behavior and the level of brain development, will help to guide research and intervention toward sensitive periods in development.
There are critical turning points in the parallel development of emotion regulation and academic skills in children exposed to violence that deserve further study. Violence exposure during childhood happens in concert with critical periods in language and social development, from infancy through adolescence. Violence exposure, particularly family violence, can wreak havoc on the development of neural circuits underlying basic mechanisms of affective and cognitive development (Andersen, Tomada, Vincow, Valente, Polcari, & Teicher, 2008; Choi, Jeong, Rohan, Polcari, & Teicher, 2009; Miskovic, Schmidt, Georgiades, Boyle, & Macmillan, 2010; Seckfort et al., 2008, Sheu, Polcari, Anderson, & Teicher, 2010). There is no longer any doubt that the assault of violence, both through physical or psychological trauma, can and does disrupt the process of normal child development.
Children with a history of violence exposure follow certain developmental trajectories, often withdrawing socially or behaviorally regressing, which can cause problems with peer relationships, especially in demanding social settings, such as in school. At the level of the brain, children exposed to violence may exhibit neurological changes that lead to problems of cognition in memory, executive functioning (the ability to organize and synthesize information), self-regulation, language causing learning delays or disabilities (De Bellis, Hooper, Spratt, & Woolley, 2009; De Bellis, Hooper, Woolley, & Shenk, 2009; DePrince, Weinzierl, & Combs, 2009; El-Hage, Gaillard, Isingrini, & Belzung, 2006;Seckfort et al., 2008; Watts-English, Fortson, Gibler, Hooper, & De Bellis, 2006). Integrating research from a number of fields, we review the confluence between violence exposure, mental health problems, language learning, neurocognitive development and disabilities.
Violence exposure, as used here, refers to violence in the community and family. Generally, exposure to interpersonal violence, whether witnessing violence between caregivers or direct child maltreatment, has a more negative impact on children than does exposure to community violence and is the focus of many of the studies reviewed here. The term maltreatment is understood to include both child abuse and neglect. Child abuse encompasses physical, sexual and emotional abuse of a child. Often individual studies reviewed here focus more discreetly on one of the specific aspects of maltreatment, but we use the term more broadly to refer to any subset of child abuse and neglect. The rationale for the use of the broad term, violence exposure, is two fold. First, multiple studies have shown exposure to one form of violence increases the likelihood of exposure to other forms of violence and also outcomes of violence exposure vary based on severity, developmental stage of the child, and the individual child’s developmental trajectory making violence type specific mechanisms unlikely (Andersen, Tomada, Vincow, Valente, Polcari, & Teicher, 2008; Margolin, Vickerman, Oliver & Gordis, 2010). In other words, children who experience one form of violence can have a variety of social and emotional behavioral outcomes and children who experience another form of violence may have the same diversity of outcomes. This necessitates the discussion of violence exposure more broadly.
It is also necessary to say a word about mental health problems as they relate to school function. A number of different disorders that fall under the broader umbrella of externalizing disorders (ADHD, Conduct Disorder (CD), Oppositional Defiant Disorder (ODD), and Autism) and internalizing disorders (anxiety, depression, and posttraumatic stress disorder (PTSD)) impact school function. Many children exhibit both internalizing and externalizing problems simultaneously (Graham-Bermann, Gruber, Girz & Howell, 2009; Hudziak, Achenbach, Althoff, & Pine, 2007). In addition, limited cognitive function, problems with executive functioning, diagnosed language impairments (LI), delayed language development, diagnosed learning, reading or math disorders, and school failure are within the Diagnostic and Statistical Manuel category of disorders most often diagnosed in childhood.
For purposes of this paper, we consider school related academic issues as separate from mental health in order to elucidate the transactional relation between school functioning and mental health. Theoretically, a specific learning disorder could be the cause of a specific behavioral disorder or vise versa. More likely, there is multifinality in the way that behavioral disorders transact within a particular child and family context. The purpose of this review is to examine this complex relation, to examine the role of violence in mental health and academic development and to propose a model of the role of violence in the development of both academic and mental health problems (see Graphical Abstract).
Violence Exposure and Functioning
Mental Health
Violence exposure in various forms has been related to problems in the development of psychosocial health in some children and adolescents. Although many people show great resilience after violence exposure, exposure to violence in the home and community is a precursor to the development of externalizing and internalizing mental health problems in some, with the degree of exposure determining the extent of the problem (Buckner, Beardslee, & Bassuk, 2004; Finzi-Dottan, Dekel, Lavi, & Su’ali, 2006; Lewis et al., 2010; Ozer & McDonald, 2006; Ruchkin, Henrich, Jones, Vermeiren, & Schwab-Stone, 2007). National lifetime rates of witnessing community violence as a child are around 30% (Finkelhor, Ormrod, Turner, & Hamby, 2005), but rates differ based on community. Children who experience one form of violence are much more likely to experience community violence with rates close to 100% if children report other violence exposure (Turner, Finkelhor, & Ormrod, 2010). In a population of homeless children, researchers found the rate of exposure to community violence to be over 60% (Buckner, Beardslee, & Bassuk, 2004). In urban populations rates of community violence exposure have been found to be as high as 70% (Thompson & Massat, 2005).
Although total community violence exposure predicts both internalizing and externalizing mental health problems, in the Buckner study, this was particularly salient for internalizing mental health problems where greater exposure was salient for both genders but was particularly salient for girls in the manifestation of internalizing. Of note, the authors also found self-regulatory ability to mediate this relation. Self-regulation has been found in a number of studies to be a salient mediator and at the brain level, in the form of executive function or cognitive control, is a possible mechanism for the development of both mental health and academic problems following exposure to violence.
Exposure to violence in the home, either witnessing violence between parents or experiencing direct violence, is also a precursor of the development of mental health problems (English et al., 2005; English, Marshall, & Stewart, 2003; Hanson et al., 2008; Kim & Cicchetti, 2009; Perkins, Cortina, Smith-Darden & Graham-Bermann, 2012; Ybarra, Wilkens, & Lieberman, 2007). The rate at which violence exposure is predictive differs based on gender and violence type (Hanson et al., 2008). In general, violence more than doubles the risk of development of PTSD and depression. Sexual abuse is most commonly experienced by girls and is the highest predictor of PTSD, at triple the rate, and equal to physical violence in predicting depression (Hanson et al., 2008). Among boys, sexual abuse is particularly damaging. Although boys experience sexual abuse less commonly, risk of the development of PTSD in boys is more than five times (Hanson et al., 2008).
Age of first exposure, frequency of exposure and exposure to multiple types of violence are important variables to consider in the development of mental health problems. In a study of children referred to child protective service for child abuse and neglect, multiple types of abuse and chronicity of abuse predicted internalizing mental health problems (English et al., 2005). In the same study, externalizing was most predicted by the earlier age of first exposure. Considering that in early childhood one of the core developmental tasks is the development of social interactions with others, it would make sense that early exposure to violence would disrupt that process and make children more vulnerable to developing externalizing behaviors. The authors examined later social competence in this population and found that chronicity of violence, physical abuse, age, and multiple types of abuse predicted deficits in social competence (English et al., 2005). Although they did not measure self-regulatory capacity directly, self-regulation of emotional response is central to social competence. There is evidence that in addition to a direct relation between abuse and mental health problems, peer-rejection and self-regulation may mediate this relation (Kim & Cicchetti, 2009; Perkins, Cortina, Smith-Darden & Graham-Bermann, 2012).
In another study, total CPS referrals also predicted child health problems, including physical disabilities, emotional disorders and learning disorders, underlying the complex relations between psychopathology and academic problems (English, Marshall, & Stewart, 2003). Finally, school-related violence, which is an often over-looked area of violence scholarship, is important in the lives of children and can be related mental health problems (Flannery, Wester, & Singer, 2004).
Academic Achievement
In terms of language and academic achievement, community and interpersonal violence exposure have been related to more negative outcomes. Children with exposure to child abuse and neglect have twice the rate of referral for special education (Jonson-Reid, Drake, Kim, Porterfield, & Han, 2004). In this prospective study of children who received Aid for Families with Dependent Children (AFDC), matched based on later substantiated maltreatment, 19% of the total sample entered special education later at a mean age of eight years old. Among the children from AFCD backgrounds without a CPS referral the rate was 14%, but was 24% for the maltreated group. Developmental risk factors as well as demographic factors, such as being male and African American, were associated with entry into special education. Developmental risk, when combined with maltreatment, increased the relation to later special education. In terms of abuse, physical abuse increased the rate for later special education by 50%. The researchers found that children with physical abuse had a heightened risk of serious emotional disturbance (SED), neglect was related to mental retardation, sexual to learning disability and mixed abuse to child delay and other health problems. Full-scale IQ deficits have also been found in children with community violence exposure (Ratner, Chiodo, Covington, Sokol, Ager, & Delaney-Black, 2006), domestic violence exposure (Ybarra, Wilkens, & Lieberman, 2007), neglect (Noble, Tottenham, & Casey, 2005), and child abuse (De Bellis, Hooper, Spratt, & Woolley, 2009; Perkins, Smith-Darden & Graham-Bermann, 2011).
Community violence and child abuse are both related to lower reading ability (De Bellis, Hooper, Spratt, & Woolley, 2009; Ratner, Chiodo, Covington, Sokol, Ager, & Delaney-Black, 2006). In a large urban sample, Ratner and colleagues found that violence victimization was related to lower overall ability and comprehension at a trend level. Interestingly, they also found that a feeling of protection at home and school was related to higher reading ability and comprehension (Ratner et al., 2006). In addition, child neglect has been related to deficits in vocabulary, language processing speed, memory and measures of attention and executive processing (De Bellis et al., 2009). For maltreated children, memory may be particularly salient in the connection between violence exposure and development of PTSD (De Bellis et al., 2009).
Potential Pathways
Violence exposures can cause neurocognitive and language processing problems through two pathways: neurological changes directly resulting from the violence exposure, and differences in exposure to interpersonal communication and language over the course of development, including number of words and type of speech (see Figure 1). In the first instance, violence exposure can be a direct cause of academic problems and disabilities through brain injury. In fact, rates of brain injury from shaken baby syndrome are over 90% (Sobsey & Nehring, 2005). Violence can also be an indirect cause of academic problems through brain changes related to learning. In the second instance, violence is related to exposure to language, which in turn is related to differences in child language acquisition (Taylor et al., 2009). Parents who communicate with their children using high amounts of negative control (use of anger, criticisms, threats, punishments, slapping and spanking), fewer questions, and more commands and prohibitions, overall, use fewer words and different types of words. Children in these dyads also use fewer words and different types of words but they also use words with fewer morphemes (the smallest part of a word that carries meaning), fewer grammatical word types, and language with fewer different functions (Taylor et al., 2009). These differences in cognitive and language processing, if not remediated early, are direct precursors of learning and cognitive disabilities (Taylor et al., 2009).
Figure 1.
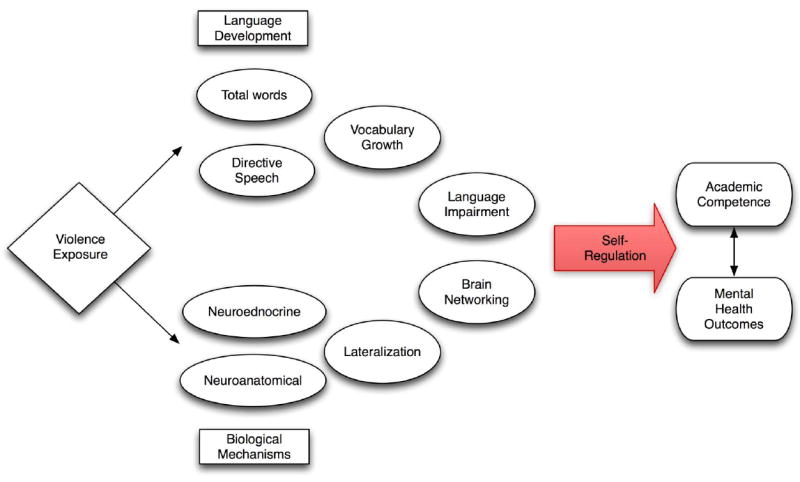
Graphical Abstract Depicting an Overview of Relations Between Violence Exposure, Academic Function and Mental Health
One core psychological construct that is linked to both biological changes resulting from violence exposure and language development is executive function deficits (or behavioral self-regulation), which may be central to the connection between academic achievement and mental health problems after violence exposure (see Figure 1). Next, we examine the evidence for these pathways in turn.
Biological Mechanisms
The study of neurobiological processes is one logical avenue of research for further understanding the underlying mechanisms that may produce the co-occurrence of mental health and academic functioning deficits after violence exposure. Childhood is a time of neural plasticity and environmental influences, including abuse and neglect, can impact the developing brain function of children (Weiss & Wagner, 1998). There are three major ways in which, theoretically, alteration of normal brain development can influence learning and behavior (see Figure 2). First, alteration of the neuroendocrine system, neuroanatomical structure (in the form of white matter and grey matter), and brain function may inhibit an individual’s ability to develop optimal functioning following exposure to violence. Second, these systems interact and associate with each other to produce cognitive functions (such as executive functioning or cognitive control) necessary for the development of self-regulation and in turn emotional or behavioral functioning. Finally, exposure to violence may influence the developing brain at a critical period making completion of certain core developmental processes difficult, delayed, or impossible. We review the evidence for neuroendocrine disruption, and neuroanatomical functional and structural changes below.
Figure 2.
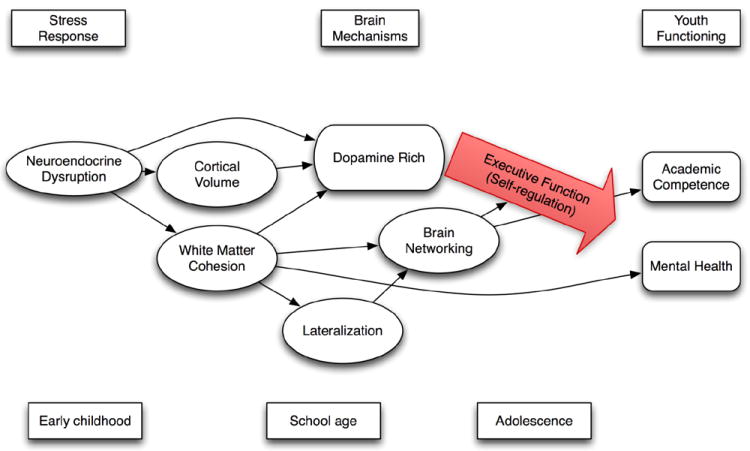
Biological Mechanisms Related to both Mental Health and School Function
Neuroendocrine Disruption
Autonomic stress response can be measured in humans by systolic and diastolic blood pressure, heart rate variability (or respiratory sinus arrhythmia, a measure of the variability of heart rate over the respiration cycle), galvanic skins response and differences in neuroendocrine expression, in particular the cortisol response. The experience of violence exposure disrupts the autonomic system including blood pressure (Murali & Chen, 2005), heart rate variability (Gordis, Feres, Olezeski, Rabkin, & Trickett, 2010; Heim et al., 2000; Murali & Chen, 2005), galvanic skin response (Gordis, Feres, Olezeski, Rabkin, & Trickett, 2010) and cortisol (Heim et al., 2000; Murali & Chen, 2005; Murray-Close, Han, Cicchetti, Crick, & Rogosch, 2008; Obradović, Bush, Stamperdahl, Adler, & Boyce, 2010). Blood pressure, heart rate variability, and galvanic skin response are physical manifestations of an internal body-brain regulation of hormones, neurotransmitters and metabolic responses. These systems interact under stress in complex ways through the regulation of neurotransmitters, which in turn regulate the release of stress hormones.
Within the neuroendocrine system, cortisol is particularly important as it is involved in the fight or flight response to stress (Meewisse et al., 2007). Cortisol is a glucocorticoid produced by the adrenal gland. Corticotrophin-releasing hormone, a neurotransmitter released by the hypothalamus, is activated by the stress response and begins a cascade by activating adrenocorticotropic hormone in the pituitary gland, that in turn activates the release of the stress hormone cortisol from the adrenal gland. Basal cortisol, cortical diurnal rhythms and cortical reactivity to stress have all been implicated in exposure to stress, but a thorough evaluation of the literature is beyond the scope of this paper. Exposure to violence is related to higher basal cortical levels, greater flattening of the cortisol diurnal rhythm (Cicchetti, Rogosch, Gunnar, & Toth, 2010; Murali & Chen, 2005), and a slower growth in cortisol over the course of development (Trickett, Noll, Susman, Shenk, & Putnam, 2010).
Timing of the child’s exposure to violence is particularly critical in changes in cortical response to later stress (Cicchetti, Rogosch, Gunnar, & Toth, 2010; Trickett, Noll, Susman, Shenk, & Putnam, 2010). Early abuse may be particularly damaging (Cicchetti, Rogosch, Gunnar, & Toth, 2010), but timing of abuse in relation to the development of a normative cortisol response in children is particularly difficult to study, as children often experience abuse for a number of years (Trickett, Noll, Susman, Shenk, & Putnam, 2010). Cortisol reactivity is also implicated in reduced school engagement and academic competence (Obradović, Bush, Stamperdahl, Adler, & Boyce, 2010) and the development of psychopathology (Obradović, Bush, Stamperdahl, Adler, & Boyce, 2010; Cicchetti, Rogosch, Gunnar, & Toth, 2010). The developmental stage of the child and the demands of both schooling and social development are likely to influence the behavioral outcomes of abuse at various developmental stages.
Monoamine oxidase A (MAOA) is an enzyme, controlled by the MAOA gene, implicated in the regulation the neurotransmitters serotonin (5-HT), dopamine (DA) and norepinephrine (NE) (Mead, Beauchaine, & Shannon, 2010). Maltreated children with a functional polymorphism in the MAOA gene have increased rates of mental health disorders including attention and emotional problems (Kim-Cohen et al., 2006). Neuroendocrine dysregulation in 5-HT, DA, and NE and related systems has been found in studies of children with violence exposure histories (De Bellis et al., 1999). In this seminal study, maltreated children with PTSD (n=18) were found to have higher urinary epinephrine, norepinephrine, dopamine and free cortisol. Duration of abuse was positively correlated with all four measures while NE and DA were primarily correlated with PTSD symptomatology.
The MAOA gene is also related to a number of other mental health and behavioral outcomes including aggression (Kim-Cohen et al., 2006), depression (Bremner, 2003), antisocial (Kim-Cohen et al., 2006) and self-regulatory behavioral problems (Kim-Cohen et al., 2006; Oades et al., 2008). Using data from the Environmental Longitudinal Risk study a birth cohort of 975 boys with genotyped data, Kim-Cohen and colleagues examined 62 boys with physical abuse histories compared to matched controls. They examined polymorphisms of the MAOA gene associated with high and low activity of MAOA. Exposure to physical abuse was related to higher mental health problems in both groups. In addition, they found an interaction whereby the Low MAOA polymorphisms had lower mental health problems in the unexposed group but the group exposed to physical abuse with Low MAOA, showed a steeper rise in mental health problems. This same interaction was found for attention, antisocial and emotion problems, if low activity MAOA and no exposure to physical abuse, problems were less than in the high activity MAOA group but surpassed the high activity MAOA if exposed to physical abuse (Kim-Cohen et al., 2006). This suggests that the low activity MAOA polymorphism is a phenotypic risk factor for mental health problems when exposed to the violence. In addition, this work suggests that violence exposure and genetic risk interact to create a vulnerability to different mental health problems, including both aggression and self-regulation.
Self-regulation is particularly important in that it is tied to both mental health and school function through deficits in attention and ADHD. The three primary systems that have been implicated in the development of ADHD are the noradrenergic (NA), dopaminergic (DA) and serotonergic (5-HT) systems (Halperin, Newcorn, & Sharma, 1996). The NA system is the site of function for most ADHD medications, but none of these systems is singularly implicated in ADHD. There is a distinction between children with comorbid aggression and ADHD and those with a more “pure” ADHD (Campbell, Sameroff, Lewis, & Miller, 2000; Halperin, Newcorn, & Sharma, 1996; Lahey, McBurnett, & Loeber, 2000). Reading Disordered (RD) and non-RD children with ADHD differ in their NA response, whereas children who are aggressive and have ADHD differ from pure ADHD in 5-HT response suggesting that the 5-HT system is more central to aggression whereas the NA system may be more central to RD and ADHD (Halperin, Newcorn, & Sharma, 1996).
Brain Development
Research has shown that violence exposure impacts normal brain development. Violence exposure appears to be related to dysfunctional development in brain volumes, white matter development and regional brain function. Violence exposed children have smaller brain volumes in areas related to cognition and emotion processing (Andersen, Tomada, Vincow, Valente, Polcari, & Teicher, 2008), less white matter cohesion (Choi, Jeong, Rohan, Polcari, & Teicher, 2009; Seckfort et al., 2008), dysfunction in dopamine rich brain regions (Sheu, Polcari, Anderson, & Teicher, 2010), and altered lateralization of brain function (Miskovic, Schmidt, Georgiades, Boyle, & Macmillan, 2010). Complicating the science of understanding this link, the timing, duration, and length of exposure determine at what point within normative development, violence exposure influences the brain and what structures and functions are most impacted (Andersen, Tomada, Vincow, Valente, Polcari, & Teicher, 2008). Smaller brain volumes are related to the age at which violence exposure occurs and are a sign of disrupted development. Deficit in white matter cohesion is considered a sign of dysfunctional brain networking. Dopamine rich areas are necessary for the development of self-regulatory function. Finally, altered lateralization is interpreted as a dysfunction in the development of regional functional differences. Normal developmental changes, such as in cortical thickness, are also influenced by individual factors, such as intelligence, which in turn may be influenced by violence exposure (Graham-Bermann, Howell, Miller, Kwek, & Lilly, 2010; Shaw et al., 2006).
Taken together, these findings suggest that violence exposure negatively impacts the neuroendocrine system and brain development during critical periods of the normal developmental trajectory. This disruption leads to vulnerabilities in systems necessary for cognitive and emotion processing. In particular, neuroendocrine disruption of stress related function and the combination of vulnerabilities in cognitive control and emotion brain areas, can lead to a deficit in self-regulatory processing. Adequate self-regulatory processing is a necessary component of classroom functioning and often is the first school-related psychopathology to raise the attention of schools and parents.
Language Development
The development of the relationship between language disorders and behavior problems can be seen as going through a series of stages that are reviewed in turn below. The first stage is a delay in language development in preschool with its association with attentional problems. In middle childhood, children with reading disabilities and those with a history of language delay show higher rates of internalizing problems. In adolescence, which is associated with a general trend in increased risk behavior, there is a link between unremediated reading disabilities and externalizing behavior problems (see Figure 3).
Figure 3.
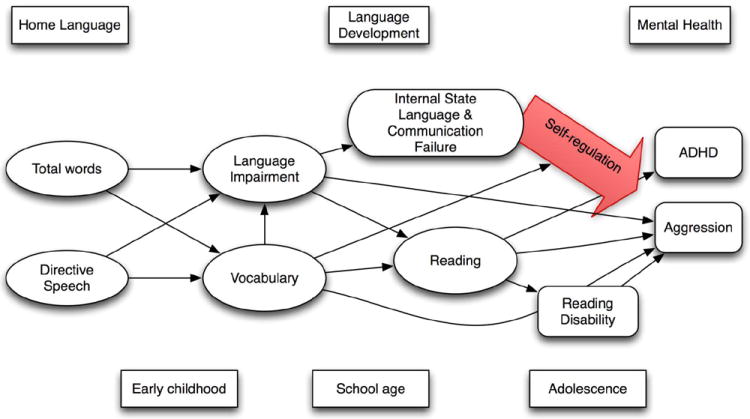
Developmental Course of Language Development as a Factor in the Development of Mental Health Problems in Children
Early Childhood Communication
One mechanism that has been posited for language disorders leading to problem behaviors is through communication failure. Children with language impairments are more likely to have difficultly with pragmatic language, such as turn taking, which would interfere with their social development and day-to-day communication with peers and teachers. Stevenson (1996) argues that this “communication failure may lead to frustration on the part of language impaired children that may lead to both externalizing and internalizing” (see Figure 3). Social cognitive deficits have also been linked to language impairment. Children with language impairments may experience a decrease in self-esteem (McGee, Share, Moffitt, Williams, & Silva, 1988) putting them at-risk of developing negative social behaviors. Children with language impairment have been shown to have a more limited understanding of emotion in social situations.
The development of self-regulation of emotion and the development of early language are bidirectional. Toddlers express emotion through facial expression and body language but are unable to express emotion through the use of language (Dale, 1996). Toddlers use language in order to communicate in unaroused states. Children progress through stages of language development that allow for increased use of internal state language, or language used to express and describe emotions. Internal state language is developed with five major influences: the maternal language used toward the child, the mother-infant attachment bond, the cognitive development of the child, sibling and peer influences and the child’s style of language learning. There are differences in the ways that boys and girls learn internal state language (Dale, 1996). Both mothers and older siblings have been found to use more internal state language with girls, with a corresponding positive impact on the use of internal state language by girls at 24 months. Children with behavioral problems experience more parental criticism and less parental warmth that may lead to delays in language development (Dale, 1996).
Language Skills
Another model posits that family environment and later hyperactive behaviors may be indirectly linked through language and non-verbal skills. Language skills at 18 months predict hyperactive behavior at 5 years (Girouard et al., 1998). Less educated parents are likely to use fewer words, less complicated syntax and fewer references to events not in the present when communicating with their children (Hart & Risley, 1995). Children in stressed homes are more likely to hear disjointed language and receive irrelevant replies (Dale, 1996). Parents with higher expressive language skills use more physical comforting with their children and more explanations for requests during child conflict situations, rather than demands (Stansbury & Zimmerman, 1999; Taylor, Donovan, Miles, & Leavitt, 2009). Expressive language is related to cognitive development, whereas the use of directive language is related to decreased development of a number of elements of language including total word usage, receptive, sematic and pragmatic language (Murray and Hornbaker, 1997; Taylor, Donovan, Miles, & Leavitt, 2009). Family environment contributes to the language skills of the child, and then, subsequently, children’s language skills promote behaviors in primary caregivers that either inhibit or disinhibit emotional regulation, which in turn can lead to externalizing behavior development.
Approximately half of all children with language delays have been reported to exhibit comorbid behavior problems, and by eight years of age language delay is related to increased behavior problems (Benasich, Curtiss, & Tallal, 1993). Children with expressive language delays are more likely to show hyperactive and under-controlled behavior, which is not the case for children with receptive language delays (Stevenson, 1996). The reverse relation has also been found. Among psychiatrically referred children, in one study, over a quarter had previously been diagnosed with Language Impairments (LI) (Cohen, 1993). Children with diagnosed LI differed from those with undiagnosed LI in having more severe expressive language delays but previously undiagnosed children were rated more aggressive and delinquent by their teachers and parents. Approximately 50% of children with ADHD also have speech/language impairments (Tannock & Schacler, 1996).
Vocabulary development is important in the understanding of both aggressive behavior and ADHD. Vocabulary development is related to aggression in 19-month-old twins (Dionne et al., 2003). In this study, aggression and vocabulary growth each have both a genetic and an environmental component. However, the percent of variance explained differed between these two phenotypes, suggesting that they differ in terms of the extent to which genetics and environment influence their development. For aggression, 58% of the variance was explained by genetic factors but for expressive vocabulary, 51% of the variance was accounted for by shared environment, suggesting that family rearing practices play an important role in vocabulary growth. Hart and Risley (1995) found that total number of words spoken in the home vary greatly and are the single strongest determinant of child vocabulary growth.
Reading Skills
Children with language impairments develop reading disabilities at higher rates than children without language impairments. Reading disorders, which by definition cannot be diagnosed until children are reading, have been implicated in the relationship with both internalizing and externalizing problems. Willcutt and Pennington (2000) found both reading disordered girls and boys showed higher rates of ADHD, ODD and CD and had higher rates of anxiety and depression. They also scored higher on Child Behavior Checklist (CBCL) internalizing and externalizing subscales. Results were particularly pronounced with boys in rates of ADHD, ODD and CD and with girls in rates of depression. It is clear there is a transactional relationship between child psychopathology and learning disorders, although the specific mechanisms at work are likely to be diverse and complex. Much less clear is the role of the context in moderating these causal relationships. For children with a history of maltreatment, the context of their maltreatment is integral to their development.
Externalizing, internalizing, and comorbid children have lower IQs (Diamond, Muller, Rondeau, & Rich, 2001; Kusche, Cook & Greenberg, 1993) and reading math and spelling achievement (Kusche et al 1993). ADHD is comorbid with CD, Major Depressive Disorder, Anxiety Disorder, and learning disabilities (LD) or special needs (Faraone, Biederman, & Keily, 1996). Externalizing and comorbid groups are significantly more likely to be represented in special education (Kusche et al 1993). Children with internalizing disorders have equal rates of oral language problems as those with externalizing problems (Donahue, Hartas, & Cole, 1999). PTSD symptomology predicts lower cognitive functioning (Diamond, Muller, Rondeau, & Rich, 2001). These studies of the correlation between psychopathology and learning problems typically do not address the directionality of effect. It may be that learning problems either pre-date psychopathology or co-occur in early childhood.
Self-regulation
Violence exposure is also to linked to increased internalizing and externalizing behavior through self-regulation. Violence exposure causes decreases in self-regulatory behavior (Kim & Cicchetti, 2009) tied to problems in executive functioning, the ability to plan, organize, and synthesize information (DePrince, Weinzierl, & Combs, 2009; Seckfort et al., 2008). In particular, the relation between self-regulation, psychopathology and academic learning may mediate the development of academic problems after violence exposure.
Mental Health and Academic Problems
One of the most stable findings in developmental psychology is that behavior disorders and other forms of psychopathology are comorbid with cognitive impairment, school failure and learning disabilities such as reading and language disorders (Benasich, Curtiss, & Tallal, 1993; Cohen, Davine, Horodezky, Lipsett, & Isaacson, 1993; Dale, 1996; Donahue et al, 1999). More recent research has shown that there is a bidirectional relation between symptoms that undermine school function and failures in functioning contributing to symptoms (Kim & Cicchetti, 2009; Masten et al., 2005). In one study, the combination of language impairment and parental distress predicted separately to both aggression and delinquency (Brownlie et al., 2004). In another, ADHD and youth with language disorders had high rates of aggression, depression and anxiety symptoms (Mcgillivray & Baker, 2008). Although these rates were subclinical, high rates of mental health symptoms, which do not rise to the level of true mental health disorders, may impact peer and teacher relationships. Both peer and teacher relationships are central to success at school, which means that failures in these relationships are likely to contribute to the circularity of the relation between school academic function and psychopathology (Kim & Cicchetti, 2009).
One interesting study examined adolescent boys exposed to terror attacks (e.g., suicide bombings and shootings) in Israel (Finzi-Dottan, Dekel, Lavi, & Su’ali, 2006). This study compared learning disability (LD) and history of prior exposure as vulnerabilities for the development of mental health problems (in the form of PTSD). Learning disability predicted both avoidance and hypervigilant symptoms in youth with LD suggesting, perhaps, that some core psychological process associated with LD leads to a failure at top-down control over emotion. Illustrating how complicated these interactions are in populations exposed to violence, past history of threatening life events, such as car accident, hospitalization and violence exposure, and parental attachment also predicted PTSD symptoms. Studies of youth with violence exposure and/or behavioral disorders may miss these developmentally complex relations by studying middle childhood or adolescence, where academic problems may have been present but undetected for much of the time prior to study.
Executive Function
Executive dysfunction has been posited as a core neurocognitive function linking psychopathology and academic problems. Executive function is the ability to plan, organize, and delay pre-potent responses in order to reach more complex goals. Failures in executive functioning have been posited as the underlying cause of attention deficit disorder. This higher order skill is seen as necessary in the development of self-regulation, a deficit seen in children with ADHD. In addition, self-regulation is skill that is integral to the development of language skills and other skills central to school success.
Executive dysfunction has been implicated in the relationship between learning problems and aggression as well. In an early study, Nigg et al. (1999) found that children with lower scores on the Stroop test had later externalizing problems. Séguin, Boulerice, Harden, Tremblay, and Pihl (1999) found that children who showed stable aggression over a six year period performed less well than both unstable aggressive children (those who showed aggression at some assessment periods but not others) and nonaggressive children on tasks of general memory IQ, and frontal lobe tests.
Violence Exposure and Neurocognition
Violence exposed children exhibit neurological changes that might contribute to trouble with learning. A burgeoning literature is showing that family trauma exposure and early life stress are related to poorer executive function (DePrince, Weinzierl, & Combs, 2009; Seckfort, et al., 2008). Several studies by De Bellis have shown that children with abuse and neglect histories have deficits in executive functioning (Beers & De Bellis, 2002; De Bellis, Hooper, Spratt, & Woolley, 2009). De Bellis postulates that neuroendocrine changes in response to stress from abuse and neglect negatively impact the frontal lobe of the brain, causing inattention and other problems associated with executive functioning (De Bellis, 2001; De Bellis, Hooper, Sapia, Vasterling, & Brewin, 2005; Watts-English, Fortson, Gibler, Hooper, & DeBellis, 2006). Violence exposure also has deleterious effects on memory (De Bellis et al, 2009; De Bellis, Hooper, Woolley, & Shenk, 2009; El-Hage, Gaillard, Isingrini & Belzung, 2006) and on performance speed (El-Hage et al, 2006), both skills necessary for successful school functioning.
Childhood executive functioning deficits have been posited as the basis for problems with self-regulation. Students who have difficulty with self-regulation are often removed from normative learning situations, through removal from the regular classrooms, putting them at greater risk of the development of cognitive and language problems. At home, children who lack self-regulation hear more directive language, a correlate with delayed language development (Taylor, Donovan, Miles, & Leavitt, 2009). At school, children are removed from more inclusive environments, also a risk factor for the development of academic skills. In turn, cognitive delays and language processing problems likely play a role in the development of executive function and self-regulation skills. This circular relationship between executive functioning and self-regulation, and language and cognitive processing is difficult to disentangle. However, each type of delay has been connected with internalizing mental health problems. Executive function deficits, self-regulation problems, language processing and cognitive development delays each hamper the child’s ability to understand and respond to social cues, which results in withdrawal or acting out in social situations.
Conclusions
The research literature has repeatedly documented a connection between violence exposure and later psychopathology. Previous studies have documented that different types of violence exposure have different outcomes for children. Sexual abuse is particularly damaging in terms of mental health, most specifically in relation to the development of PTSD (Hanson et al., 2008). In terms of educational outcomes, physical abuse is most likely to contribute to special education diagnosis, primarily in the diagnosis of serious emotional disturbance. Sexual abuse was most likely to be related to LD (Jonson-Reid, Drake, Kim, Porterfield, & Han, 2004). This might suggest that PTSD in school is less recognized and has a less marked impact on school-related behavior. It is also possible that the path for sexual abuse might be from abuse to up-regulation of emotion to failure to concentrate, whereas for physical abuse the path might be from abuse to failure to down-regulate to emotional dysregulation and concurrent academic problems.
Differential pathways based on type of violence have yet to be established. However, the emergence of both externalizing and internalizing adjustment problems can be a critical turning point in the development of violence-exposed children. Most vulnerable to these deleterious effects are those functions that are concurrently developing at the time of violence exposure (Andersen, Tomada, Vincow, Valente, Polcari, & Teicher, 2008). During early childhood, self-regulatory processing and language development can be most impaired in children with mental health problems related to violence exposure. Academic and social functioning can be affected by later exposure. At each stage of development, academic function and social function can work together to impact mental health either positively or negatively.
Social functioning difficulties have implications for school related functioning. Both internalizing and externalizing behavior problems remove students from social learning situations that promote language and cognitive growth. Removal from positive school and family educational settings limits the youth’s ability to learn more complex language patterns, organizational skills and self monitoring behaviors as the demands of social and school environment change. The combination of social withdrawal and behavioral problems that lead to smaller, socially removed classroom environments, allow for fewer opportunities to develop self-regulatory skills and social skills necessary for healthy peer-to-peer and adult-to-child relationships.
The reverse is also true. Cognitive processing problems, language delays, and disabilities are often associated with internalizing and externalizing problems. Children with weak language skills may develop, or continue to develop, externalizing problems, internalizing problems, or both through a number of mechanisms. Language impaired children have more difficulty understanding emotions of others and social situations. This may lead to communication failure with other children or adults, which in turn leads to frustration. These children may develop low self-esteem and resort to aggression or withdrawal from others as a result. In early childhood, children with language impairment may appear to be hyperactive or inattentive. In later childhood, language impairment can lead to reading disability, which is associated with both internalizing and externalizing behavior in childhood. In adolescence, children with continued reading disabilities are more likely to show externalizing problems.
There is evidence from cognitive neuroscience that violence exposure causes neurobiological changes that have implications for learning, executive functioning and self-regulation. Findings from neurobiology show that the experience of violence alters the neurochemistry of an individual in ways that may impact learning or may mimic or create learning disabilities. Cascading stress hormones also influence self-regulatory capacity. Children who have experienced violence exhibit abnormalities in a variety of brain regions in cortical thickness, white matter structure and function. It is reasonable to hypothesize that these neurological differences could result in difficulties in school. The frontal region is utilized in planning, setting goals, organizing, and prioritizing information. The temporal lobe is the site of the Wernicke’s area, an important site for language comprehension, and the auditory cortex where auditory stimuli are processed. The amygdala is part of the limbic system and has a role in the processing of emotion. Finally, the corpus callosum is necessary for the transfers and integration of information from both halves of the brain. These areas are at-risk for change due to violence exposure.
It is unlikely that different experiences with violence exposure, which are likely to differentially influence the neurobiology of individuals, would have singular or simple patterns of influence on the learning styles of students. However, it is clear that brain abnormalities are likely to impact sensory processing and integration in a number of distinct ways depending on the individual. In it also clear that repeated maltreatment and traumatic events have a compounding effect on the brain (van der Kolk, 1997, 2003; Van Voorhees & Scarpa, 2004).
We have argued here that cognitive processing and learning problems may be at the center between the known relation between violence exposure and psychopathology. Children with Conduct Disorder can be discriminated from controls by measuring language skills, punishment by parents, ADHD symptoms and oppositional symptoms (Toupin et al., 2000). Children with ADHD show deficits in pragmatic speech and with interpretations of social situations. Pragmatic speech seems to be positively influenced by the use of stimulant medication prescribed for ADHD. The influence of executive function is bidirectional. Executive function influences the development of pragmatic language and social communication and these factors in turn influence the development of executive function (Tannock & Schacler, 1996).
Clinical and Research Implications
Targeted interventions directed at executive function and remediating disability would be essential for assisting children with a history of violence exposure regardless of whether or not their functioning on any of those dimensions rises to the level of a diagnosable disability. Development of cognitive and learning skills is central to the known relation between maltreatment and internalizing and externalizing problems. This would suggest that screening for cognitive deficits and learning problems should be provided to children with histories of violence exposure before they present with problems that reach a clinical cut off in special education or in the realm of mental health.
Future research should focus on the interrelations between executive function, self-regulation, disability and other cognitive processing deficits. Within the cognitive literature, the directions are unclear. Executive function has been posited as a mediator between language and cognitive processing and behavior. This line of research would help to determine cognitive interventions that could moderate the role of cognitive impairments in the development of violence. Another important future direction for research is in determining the extent of neurobiological changes due to timing, duration and extent of exposure to violence and the implications of these changes on the development of language and cognitive processing.
Finally, research might focus on intervention programs that can target specific language and cognitive deficits that have been found to result from the maltreatment of children. Early intervention with at-risk families and their children that focuses on screening for language and cognitive development problems should be incorporated into programs for children at risk of and exposed to violence and those at risk of developing psychopathology. Children who are showing early language and cognitive delays would benefit from programs that provide targeted instruction on infant-caregiver interaction in terms of language and language-rich environments for children.
Acknowledgments
The authors would like to thank the following people for assistance in the preparation of this manuscript. Arnold Sameroff and the Development of Psychopathology and Mental Health certificate program at the University of Michigan. Dr. Sameroff read versions of this manuscript for his class on the development of psychopathology and the program as a whole trained Dr. Perkins in thinking developmentally about psychopathology and the role of both contextual and environmental influences. In particular, Toni Antonucci and Catherine Lord were instrumental in that instruction. We would like to thank Dr. Gregory Dalack and the Department of Psychiatry for providing support and protected time to complete this work. Finally Dr. Perkins would like to thank her former students who inspired her academic career.
Footnotes
Abbreviations: 5-HT = serotonin, ADHD = Attention Deficit Hyperactivity Disorder, AFDC = Aid for Families with Dependent Children, CD = Conduct Disorder, CPS = Child Protective Service, DA = dopamine, LD = Learning Disability, LI = Language Impairment, MAOA = monoamine oxidase A, NE = norephinephrine, ODD = Oppositional Defiant Disorder, PTSD = Posttraumatic Stress Disorder.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Andersen S, Tomada A, Vincow E, Valente E, Polcari A, Teicher M. Preliminary evidence for sensitive periods in the effect of childhood sexual abuse on regional brain development. The Journal of Neuropsychiatry and Clinical Neurosciences. 2008;20(3):292–301. doi: 10.1176/appi.neuropsych.20.3.292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Azar ST, Wolfe DA. Child Physical Abuse and Neglect. In: Mash EJ, Barkley RA, editors. Treatment of Childhood Disorders. 3. New York: The Guilford Press; 2006. pp. 595–646. [Google Scholar]
- Beers SR, De Bellis MD. Neuropsychological function in children with maltreatment-related posttraumatic stress disorder. American Journal of Psychiatry. 2002;159(3):483–486. doi: 10.1176/appi.ajp.159.3.483. [DOI] [PubMed] [Google Scholar]
- Benasich AA, Curtiss S, Tallal P. Language, learning, and behavioral disturbances in childhood: A longitudinal perspective. Journal of the American Academy of Child & Adolescent Psychiatry. 1993;32(3):585–594. doi: 10.1097/00004583-199305000-00015. [DOI] [PubMed] [Google Scholar]
- Bremner JD. Long-term effects of childhood abuse on brain and neurobiology. Child and Adolescent Psychiatric Clinics of North America. 2003;12(2):271–92. doi: 10.1016/s1056-4993(02)00098-6. [DOI] [PubMed] [Google Scholar]
- Brownlie E, Beitchman J, Escobar M, Young A, Atkinson L, Johnson C, et al. Early language impairment and young adult delinquent and aggressive behavior. Journal of Abnormal Child Psychology. 2004;32(4):453–67. doi: 10.1023/b:jacp.0000030297.91759.74. [DOI] [PubMed] [Google Scholar]
- Buckner J, Beardslee W, Bassuk E. Exposure to violence and low-income children’s mental health: direct, moderated, and mediated relations. American Journal of Orthopsychiatry. 2004;74(4):413–23. doi: 10.1037/0002-9432.74.4.413. [DOI] [PubMed] [Google Scholar]
- Campbell SM, Sameroff AJ, Lewis M, Miller SM. Handbook of developmental psychopathology. 2. Kluwer Academic Publishers; 2000. Attention-deficit/hyperactivity disorder: A developmental view; pp. 383–401. [Google Scholar]
- Choi J, Jeong B, Rohan M, Polcari A, Teicher M. Preliminary Evidence for White Matter Tract Abnormalities in Young Adults Exposed to Parental Verbal Abuse. Biological Psychiatry. 2009;65(3):227–234. doi: 10.1016/j.biopsych.2008.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cicchetti D, Rogosch F. The impact of child maltreatment and psychopathology on neuroendocrine functioning. Development & Psychopathology. 2001;13(4):783–804. [PubMed] [Google Scholar]
- Cicchetti D, Rogosch F, Gunnar M, Toth S. The differential impacts of early physical and sexual abuse and internalizing problems on daytime cortisol rhythm in school-aged children. Child Development. 2010;81(1):252–69. doi: 10.1111/j.1467-8624.2009.01393.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen NJ, Davine M, Horodezky N, Lipsett L, Isaacson L. Unsuspected language impairment in psychiatrically disturbed children: prevalence and language and behavioral characteristics. Journal of the American Academy of Child and Adolescent Psychiatry. 1993;32(3):595–603. doi: 10.1097/00004583-199305000-00016. [DOI] [PubMed] [Google Scholar]
- Dale P. Language and emotion: a developmental perspective. In: Beitchman JH, Cohen NJ, Konstantareas MM, Tannock R, editors. Language, Learning, and Behavior Disorders: Developmental, Biological, and Clinical Perspectives. New York, NY, US: Cambridge University Press; 1996. pp. xv–582. [Google Scholar]
- De Bellis MD. Developmental traumatology: The psychobiological development of maltreated children and its implications for research, treatment, and policy. Development and Psychopathology. 2001;13(3):539–564. doi: 10.1017/s0954579401003078. [DOI] [PubMed] [Google Scholar]
- De Bellis, et al. A.E. Bennett Research Award Developmental traumatology Part I: Biological stress systems. Biological Psychiatry. 1999;45(10):1259–70. doi: 10.1016/s0006-3223(99)00044-x. [DOI] [PubMed] [Google Scholar]
- De Bellis MD, Hooper SR, Sapia JL, Vasterling JJ, Brewin CR. Neuropsychology of PTSD: Biological, cognitive, and clinical perspectives. Guilford Press; 2005. Early Trauma Exposure and the Brain; pp. 153–177. [Google Scholar]
- De Bellis MD, Hooper SR, Spratt EG, Woolley DP. Neuropsychological findings in childhood neglect and their relationships to pediatric PTSD. Journal of the International Neuropsychological Society. 2009;15(06):868. doi: 10.1017/S1355617709990464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Bellis M, Hooper S, Woolley D, Shenk C. Demographic, Maltreatment, and Neurobiological Correlates of PTSD Symptoms in Children and Adolescents. Journal of Pediatric Psychology. 2009 Dec 11;:1–8. doi: 10.1093/jpepsy/jsp116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DePrince A, Weinzierl K, Combs M. Executive function performance and trauma exposure in a community sample of children. Child Abuse & Neglect. 2009;33(2009):353–361. doi: 10.1016/j.chiabu.2008.08.002. [DOI] [PubMed] [Google Scholar]
- Diamond T, Muller RT, Rondeau LA, Rich JG. Advances in Psychology Research. V. Huntington, NY, US: Nova Science Publishers, Inc; 2001. The relationships among PTSD symtomatology and cognitive functioning in adult survivors of child maltreatment; pp. 253–279. [Google Scholar]
- Dionne G, Tremblay RE, Boivin M, Laplante D, Perusse D. Physical aggression and expressive vocabulary in 19-month-old twins. Developmental Psychology. 2003;39(2):261–272. doi: 10.1037//0012-1649.39.2.261. [DOI] [PubMed] [Google Scholar]
- Donahue M, Hartas D, Cole D. Research on Interactions Among Oral Language and Emotional/Behavioral Disorders. In: Rogers-Adkinson DL, Griffith PL, editors. Communication Disorders and Children with Psychiatric and Behavioral Disorders. San Diego: Singular Publishing Group; 1999. p. 466. [Google Scholar]
- El-Hage W, Gaillard P, Isingrini M, Belzung C. Trauma-related deficits in working memory. Cognitive Neuropsychiatry. 2006;11(1):33–46. doi: 10.1080/13546800444000164. [DOI] [PubMed] [Google Scholar]
- English DJ, Upadhyaya MP, Litrownik AJ, Marshall JM, Runyan DK, Graham JC, Dubowitz H. Maltreatment’s wake: the relationship of maltreatment dimensions to child outcomes. Child Abuse & Neglect. 2005;29(5):597–619. doi: 10.1016/j.chiabu.2004.12.008. [DOI] [PubMed] [Google Scholar]
- English DJ, Marshall DB, Stewart AJ. Effects of family violence on child behavior and health during early childhood. Journal of Family Violence. 2003;18(1):43–57. [Google Scholar]
- Faraone SV, Biederman J, Keily K. Cognitive functioning, learning disability, and school failure in attention deficit hyperactivity disorder: A family study perspective. In: Beitchman JH, Cohen NJ, Konstantareas MM, Tannock R, editors. Language, Learning, and Behavior Disorders: Developmental, Biological, and Clinical Perspectives. New York, NY, US: Cambridge University Press; 1996. pp. xv–582. [Google Scholar]
- Finkelhor D, Ormrod R, Turner H, Hamby SL. The victimization of children and youth: A comprehensive, national survey. Child Maltreatment. 2005;10(1):5–25. doi: 10.1177/1077559504271287. [DOI] [PubMed] [Google Scholar]
- Finzi-Dottan R, Dekel R, Lavi T, Su’ali T. Posttraumatic stress disorder reactions among children with learning disabilities exposed to terror attacks. Comprehensive Psychiatry. 2006;47(2):144–151. doi: 10.1016/j.comppsych.2005.05.001. [DOI] [PubMed] [Google Scholar]
- Flannery D, Wester K, Singer M. Impact of exposure to violence in school on child and adolescent mental health and behavior. Journal of Community Psychology. 2004;32(5):559–573. [Google Scholar]
- Girouard PC, Baillargeon RH, Tremblay RE, Glorieux J, Lefebvre F, Robaey P. Developmental pathways leading to externalizing behaviors in 5 year olds born before 29 weeks of gestation. Journal of Developmental & Behavioral Pediatrics. 1998;19(4):244–253. doi: 10.1097/00004703-199808000-00002. [DOI] [PubMed] [Google Scholar]
- Gordis EB, Feres N, Olezeski CL, Rabkin AN, Trickett PK. Skin conductance reactivity and respiratory sinus arrhythmia among maltreated and comparison youth: relations with aggressive behavior. Journal of Pediatric Psychology. 2010;35(5):547–558. doi: 10.1093/jpepsy/jsp113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graham-Bermann SA, Gruber G, Girz L, Howell KH. Factors discriminating among profiles of resilient coping and psychopathology in children exposed to domestic violence. Child Abuse & Neglect. 2009;33(9):648–660. doi: 10.1016/j.chiabu.2009.01.002. [DOI] [PubMed] [Google Scholar]
- Graham-Bermann SA, Howell KH, Miller LE, Kwek J, Lilly M. Traumatic events and maternal education as predictors of verbal ability for preschool children exposed to intimate partner violence (IPV) Journal of Family Violence. 2010;25(4):383–392. [Google Scholar]
- Halperin JM, Newcorn JH, Sharma V. Neurochemical correlates of academic achievement deficits and aggressive behavior in children with ADHD. In: Beitchman JH, Cohen NJ, Konstantareas MM, Tannock R, editors. Language, Learning, and Behavior Disorders: Developmental, Biological, and Clinical Perspectives. New York, NY, US: Cambridge University Press; 1996. pp. xv–582. [Google Scholar]
- Hanson R, Borntrager C, Self-Brown S, Kilpatrick D, Saunders B, Resnick H, et al. Relations among gender, violence exposure, and mental health: the national survey of adolescents. American Journal of Orthopsychiatry. 2008;78(3):313–21. doi: 10.1037/a0014056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hart B, Risley TR. Meaningful Differences in the Everyday Experience of Young American Children. Baltimore, MD, US: Paul H Brookes Publishing Co; 1995. [Google Scholar]
- Heim, et al. Pituitary-adrenal and autonomic responses to stress in women after sexual and physical abuse in childhood. JAMA: Journal of the American Medical Association. 2000;284(5):592–597. doi: 10.1001/jama.284.5.592. [DOI] [PubMed] [Google Scholar]
- Hudziak J, Achenbach T, Althoff R, Pine D. A dimensional approach to developmental psychopathology. International Journal of Methods in Psychiatric Research. 2007;16(Supplement 1):S16–23. doi: 10.1002/mpr.217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jonson-Reid M, Drake B, Kim J, Porterfield S, Han L. A prospective analysis of the relationship between reported child maltreatment and special education eligibility among poor children. Child Maltreatment. 2004;9(4):382–394. doi: 10.1177/1077559504269192. [DOI] [PubMed] [Google Scholar]
- Kearney C, Wechsler A, Kaur H, Lemos-Miller A. Posttraumatic stress disorder in maltreated youth: A review of contemporary research and thought. Clinical Child and Family Psychology Review. 2010;13(1):46–76. doi: 10.1007/s10567-009-0061-4. [DOI] [PubMed] [Google Scholar]
- Kim J, Cicchetti D. Longitudinal pathways linking child maltreatment, emotion regulation, peer relations, and psychopathology. Journal of Child Psychology and Psychiatry. 2009;51(6):706–716. doi: 10.1111/j.1469-7610.2009.02202.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim-Cohen J, Caspi A, Taylor A, Williams B, Newcombe R, Craig IW, Moffitt TE. MAOA, maltreatment, and gene–environment interaction predicting children’s mental health: new evidence and a meta-analysis. Molecular Psychiatry. 2006;11(10):903–913. doi: 10.1038/sj.mp.4001851. [DOI] [PubMed] [Google Scholar]
- Kusche CA, Cook ET, Greenberg MT. Neuropsychological and cognitive functioning in children with anxiety, externalizing, and comorbid psychopathology. Journal of Clinical Child Psychology: Special Issue: The Neuropsychological Basis of Disorders Affecting Children and Adolescents. 1993;22(2):172–195. [Google Scholar]
- Lahey BB, McBurnett K, Loeber R. Handbook of Developmental Psychopathology. 2. New York, NY, US: Kluwer Academic/Plenum Publishers; 2000. Are attention-deficit/hyperactivity disorder and oppositional defiant disorder developmental precursors to conduct disorder? pp. 431–446. [Google Scholar]
- Lewis, et al. Witnessed violence and youth behavior problems: A multi-informant study. American Journal of Orthopsychiatry. 2010;80(4):443–450. doi: 10.1111/j.1939-0025.2010.01047.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Margolin G, Vickerman KA, Oliver PH, Gordis EB. Violence exposure in multiple interpersonal domains: Cumulative and differential effects. Journal of Adolescent Health. 2010;47(2):198–205. doi: 10.1016/j.jadohealth.2010.01.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masten A, Roisman G, Long J, Burt K, Obradovic J, Riley J, et al. Developmental cascades: linking academic achievement and externalizing and internalizing symptoms over 20 years. Developmental Psychology. 2005;41(5):733–46. doi: 10.1037/0012-1649.41.5.733. [DOI] [PubMed] [Google Scholar]
- McGee R, Share D, Moffitt TE, Williams S, Silva PA. Individual Differences in Children and Adolescents. New Brunswick, NJ, US: Transaction Publishers; 1988. Reading disability, behaviour problems and juvenile delinquency; pp. 158–172. [Google Scholar]
- McGillivray J, Baker K. Effects of comorbid ADHD with learning disabilities on anxiety, depression, and aggression in adults. Journal of Attention Disorders. 2008;12(6):525–531. doi: 10.1177/1087054708320438. [DOI] [PubMed] [Google Scholar]
- Mead HK, Beauchaine TP, Shannon KE. Neurobiological adaptations to violence across development. Development and Psychopathology. 2010;22(01):1–22. doi: 10.1017/S0954579409990228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meewisse M, Reitsma JB, De Vries G, Gersons BP, Olff M. Cortisol and post-traumatic stress disorder in adults: Systematic review and meta-analysis. The British Journal of Psychiatry. 2007;191(5):387–392. doi: 10.1192/bjp.bp.106.024877. [DOI] [PubMed] [Google Scholar]
- Miskovic V, Schmidt L, Georgiades K, Boyle M, Macmillan H. Adolescent females exposed to child maltreatment exhibit atypical EEG coherence and psychiatric impairment: Linking early adversity, the brain, and psychopathology. Development and Psychopathology. 2010;22(02):419–432. doi: 10.1017/S0954579410000155. [DOI] [PubMed] [Google Scholar]
- Murali R, Chen E. Exposure to violence and cardiovascular and neuroendocrine measures in adolescents. Annals of Behavioral Medicine. 2005;30(2):155–63. doi: 10.1207/s15324796abm3002_8. [DOI] [PubMed] [Google Scholar]
- Murray AD, Hornbaker AV. Maternal directive and facilitative interaction styles: associations with language and cognitive development of low risk and high risk toddlers. Development and Psychopathology. 1997;9(3):507–16. doi: 10.1017/s0954579497001272. [DOI] [PubMed] [Google Scholar]
- Murray-Close D, Han G, Cicchetti D, Crick NR, Rogosch FA. Neuroendocrine regulation and physical and relational aggression: The moderating roles of child maltreatment and gender. Developmental Psychology. 2008;44(4):1160–1176. doi: 10.1037/a0012564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Scientific Council on the Developing Child and the National Forum on Early Childhood Policy and Programs. The Foundations of Lifelong Health Are Built in Early Childhood. 2010:1–32. [Google Scholar]
- Nigg JT, Quamma JP, Greenberg MT, Kusche CA. A two-year longitudinal study of neuropsychological and cognitive performance in relation to behavioral problems and competencies in elementary school children. Journal of Abnormal Child Psychology. 1999;27(1):51–63. doi: 10.1023/a:1022614407893. [DOI] [PubMed] [Google Scholar]
- Noble K, Tottenham N, Casey B. Neuroscience perspectives on disparities in school readiness and cognitive achievement. The Future of children / Center for the Future of Children, the David and Lucile Packard Foundation. 2005;15(1):71–89. doi: 10.1353/foc.2005.0006. [DOI] [PubMed] [Google Scholar]
- Oades R, Lasky-Su J, Christiansen H, Faraone S, Sonuga-Barke E, Banaschewski T, et al. The influence of serotonin- and other genes on impulsive behavioral aggression and cognitive impulsivity in children with attention-deficit/hyperactivity disorder (ADHD): Findings from a family-based association test (FBAT) analysis. Behavioral and Brain Functions. 2008;4(48):48. doi: 10.1186/1744-9081-4-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Obradović J, Boyce W. Individual differences in behavioral, physiological, and genetic sensitivities to contexts: implications for development and adaptation. Developmental Neuroscience. 2009;31(4):300–8. doi: 10.1159/000216541. [DOI] [PubMed] [Google Scholar]
- Obradovic J, Burt K, Masten A. Pathways of adaptation from adolescence to young adulthood: antecedents and correlates. Annals of the New York Academy of Sciences. 2006;1094:340–4. doi: 10.1196/annals.1376.046. [DOI] [PubMed] [Google Scholar]
- Obradović J, Bush N, Stamperdahl J, Adler N, Boyce W. Biological sensitivity to context: the interactive effects of stress reactivity and family adversity on socioemotional behavior and school readiness. Child Development. 2010;81(1):270–89. doi: 10.1111/j.1467-8624.2009.01394.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ozer E. The impact of violence on urban adolescents: Longitudinal effects of perceived school connection and family support. Journal of Adolescent Research. 2005;20(2):167. [Google Scholar]
- Ozer E, McDonald K. Exposure to Violence and Mental Health Among Chinese American Urban Adolescents. Journal of Adolescent Health. 2006;39(1):73–79. doi: 10.1016/j.jadohealth.2005.09.015. [DOI] [PubMed] [Google Scholar]
- Perkins SC, Cortina K, Smith-Darden J, Graham-Bermann S. The mediating role of disability and self-regulation between violence exposure and mental health functioning in incarcerated adolescents. Journal of Interpersonal Violence. 2012;27(7) doi: 10.1177/0886260511425240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perkins SC, Smith-Darden J, Graham-Bermann S. The relation of violence exposure and ethnicity to intelligence and verbal-performance discrepancies in incarcerated male adolescents. Violence and Victims. 2011;26(4):496–512. doi: 10.1891/0886-6708.26.4.496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Posner M, Rothbart M. Influencing brain networks: implications for education. Trends in Cognitive Sciences. 2005;9(3):99–103. doi: 10.1016/j.tics.2005.01.007. [DOI] [PubMed] [Google Scholar]
- Ruchkin V, Henrich C, Jones S, Vermeiren R, Schwab-Stone M. Violence exposure and psychopathology in urban youth: The mediating role of posttraumatic stress. Journal of Abnormal Child Psychology. 2007;35(4):578–593. doi: 10.1007/s10802-007-9114-7. [DOI] [PubMed] [Google Scholar]
- Ratner H, Chiodo L, Covington C, Sokol R, Ager J, Delaney-Black V. Violence exposure, IQ, academic performance, and children’s perception of safety. Merrill-Palmer Quarterly. 2006;52:264–287. [Google Scholar]
- Seckfort D, Paul R, Grieve S, Vandenberg B, Bryant R, Williams L, et al. Early life stress on brain structure and function across the lifespan: A preliminary study. Brain Imaging and Behavior. 2008;2(1):49–58. [Google Scholar]
- Seguin JR, Boulerice B, Harden PW, Tremblay RE, Pihl RO. Executive functions and physical aggression after controlling for attention deficit hyperactivity disorder, general memory and IQ. Journal of Child Psychology & Psychiatry & Allied Disciplines. 1999;40(8):1197–1208. [PubMed] [Google Scholar]
- Shaw P, Greenstein D, Lerch J, Clasen L, Lenroot R, Gogtay N, et al. Intellectual ability and cortical development in children and adolescents. Nature. 2006;440(7084):676–679. doi: 10.1038/nature04513. [DOI] [PubMed] [Google Scholar]
- Sheu Y-S, Polcari A, Anderson C, Teicher M. Harsh corporal punishment is associated with increased T2 relaxation time in dopamine-rich regions. NeuroImage. 2010 Jul 14;:1–8. doi: 10.1016/j.neuroimage.2010.06.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobsey R, Nehring WM. Health promotion for persons with intellectual and developmental disabilities. American Association on Mental Retardation; 2005. Violence; pp. 205–234. [Google Scholar]
- Stansbury K, Zimmermann LK. Relations among child language skills, maternal socializations of emotion regulation, and child behavior problems. Child Psychiatry & Human Development. 1999;30(2):121–142. doi: 10.1023/a:1021954402840. [DOI] [PubMed] [Google Scholar]
- Stevenson J. Developmental changes in the mechanisms linking language disabilities and behavior disorders. In: Beitchman JH, Cohen NJ, Konstantareas MM, Tannock R, editors. Language, Learning, and Behavior Disorders: Developmental, Biological, and Clinical Perspectives. New York, NY, US: Cambridge University Press; 1996. pp. xv–582. [Google Scholar]
- Tannock R, Schachar R. Executive dysfunction as an underlying mechanism of behavior and language problems in attention deficit hyperactivity disorder. In: Beitchman JH, Cohen NJ, Konstantareas MM, Tannock R, editors. Language, Learning, and Behavior Disorders: Developmental, Biological, and Clinical Perspectives. New York, NY, US: Cambridge University Press; 1996. pp. xv–582. [Google Scholar]
- Taylor N, Donovan W, Miles S, Leavitt L. Maternal control strategies, maternal language usage and children’s language usage at two years. Journal of Child Language. 2009;36(02):381–404. doi: 10.1017/S0305000908008969. [DOI] [PubMed] [Google Scholar]
- Teicher MH. Scars that won’t heal: the neurobiology of child abuse. Scientific American. 2002;286(3):68–75. doi: 10.1038/scientificamerican0302-68. [DOI] [PubMed] [Google Scholar]
- Thompson T, Massat CR. Experiences of violence, post-traumatic stress, academic achievement and behavior problems of urban African-American children. Child and Adolescent Social Work Journal. 2005;22(5-6):367–393. [Google Scholar]
- Toupin J, Dery M, Pauze R, Mercier H, Fortin L. Journal of Child Psychology & Psychiatry & Allied Disciplines. 3. Vol. 41. US Cambridge University Press; 2000. Cognitive and familial contributions to conduct disorder in children; pp. 2333–2344. [PubMed] [Google Scholar]
- Trickett PK, Noll JG, Susman EJ, Shenk CE, Putnam FW. Attenuation of cortisol across development for victims of sexual abuse. Development and Psychopathology. 2010;22(01):165. doi: 10.1017/S0954579409990332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turner HA, Finkelhor D, Ormrod R. Poly-victimization in a national sample of children and youth. American Journal of Preventive Medicine. 2010;38(3):323–330. doi: 10.1016/j.amepre.2009.11.012. [DOI] [PubMed] [Google Scholar]
- van der Kolk BA. The psychobiology of posttraumatic stress disorder. Journal of Clinical Psychiatry. 1997;58(Supplement 9):16–24. [PubMed] [Google Scholar]
- van der Kolk BA. The neurobiology of childhood trauma and abuse. Child and Adolescent Psychiatry Clinics of North America. 2003;12(2):293–317. ix. doi: 10.1016/s1056-4993(03)00003-8. [DOI] [PubMed] [Google Scholar]
- Van Voorhees E, Scarpa A. The effects of child maltreatment on the hypothalamic-pituitary-adrenal axis. Trauma, Violence & Abuse. 2004;5(4):333–352. doi: 10.1177/1524838004269486. [DOI] [PubMed] [Google Scholar]
- Watts-English T, Fortson BL, Gibler N, Hooper SR, DeBellis MD. The psychobiology of maltreatment in childhood. Journal of Social Issues. 2006;62(4):717–736. [Google Scholar]
- Weiss MJS, Wagner SH. What explains the negative consequences of adverse childhood experiences on adult health? Insights from cognitive and neuroscience research. American Journal of Preventive Medicine. 1998;14(4):356–360. doi: 10.1016/s0749-3797(98)00011-7. [DOI] [PubMed] [Google Scholar]
- Willcutt EG, Pennington BF. Psychiatric comorbidity in children and adolescents with reading disability. Journal of Child Psychology & Psychiatry & Allied Disciplines. 2000;41(8):1039–1048. [PubMed] [Google Scholar]
- Ybarra G, Wilkens S, Lieberman A. The influence of domestic violence on preschooler behavior and functioning. Journal of Family Violence. 2007;22(1):33–42. [Google Scholar]


