Abstract
Bone marrow derived mesenchymal stromal cells (MSCs) have recently been implicated as one source of the tumor-associated stroma, which plays essential role in regulating tumor progression. In spite of the intensive research, the individual factors in MSCs controlling tumor progression have not been adequately defined. In the present study we have examined the role of galectin-1 (Gal-1), a protein highly expressed in tumors with poor prognosis, in MSCs in the course of tumor development. Co-transplantation of wild type MSCs with 4T1 mouse breast carcinoma cells enhances the incidence of palpable tumors, growth, vascularization and metastasis. It also reduces survival compared to animals treated with tumor cells alone or in combination with Gal-1 knockout MSCs. In vitro studies show that the absence of Gal-1 in MSCs does not affect the number of migrating MSCs toward the tumor cells, which is supported by the in vivo migration of intravenously injected MSCs into the tumor. Moreover, differentiation of endothelial cells into blood vessel-like structures strongly depends on the expression of Gal-1 in MSCs. Vital role of Gal-1 in MSCs has been further verified in Gal-1 knockout mice. By administering B16F10 melanoma cells into Gal-1 deficient animals, tumor growth is highly reduced compared to wild type animals. Nevertheless, co-injection of wild type but not Gal-1 deficient MSCs results in dramatic tumor growth and development.
These results confirm that galectin-1 is one of the critical factors in MSCs regulating tumor progression.
Introduction
In spite of the increasing significance [1], [2], the origin of the tumor-associated non-tumor-cell elements (tumor-associated fibroblasts and endothelium) has not been determined decisively. As it has recently been shown, one source of the tumor-associated stroma (TAS) is bone marrow-derived mesenchymal stromal cells, which migrate into the solid tumor and there contribute to the establishment of TAS [3]. Also MSCs have been implicated in formation of tumor blood vessel endothelium partially by secreting angiogenic factors such as vascular endothelial growth factor (VEGF), fibroblast growth factor (FGF), platelet-derived growth factor (PDGF), and stromal-derived factor-1 (SDF-1) [4]. Moreover, they are able to differentiate into endothelial cells as well [5].
Exogenously administered MSCs migrate and specifically localize into tumors [6]–[8]. However, the effect of transplanted MSCs in term of tumor progression is still actively debated, since both tumor-promoting and tumor-moderating functions have been indicated [9]. Tumor promotion by MSCs has been primarily attributed to their immunosuppressive function [10] and neo-vascularization promoting effect [11]. All effects of MSCs in solid tumors can be explained by two mechanisms: 1) differentiation of the multipotent MSCs into tumor-associated tissue elements such as fibroblasts [12], tumor-associated blood vessel endothelium [5] and/or smooth muscle [13] or 2) MSCs are not stably associated with these sites, rather they affect tumorigenesis via producing various angiogenic (VEGF, PDGF, FGF) [4], immunosuppressive (TGF-β1, IDO, IL-10, PGE2) [14] and metastatic (CCL5) [15], [16] factors. These possibilities are not exclusive; however providing definite answer is difficult due to the lack of MSC specific molecular markers.
Galectin-1 (Gal-1) is an immunosuppressive and pro-angiogenic member of the β-galactoside-binding lectin family, galectins. Immunosuppressive function of Gal-1 has been confirmed in a number of in vivo and in vitro studies [17]. Targeted inhibition of Gal-1 expression or function in tumor cells provokes immune response against the tumor and subsequent tumor rejection [18], [19]. Also, Gal-1 has recently been implicated in growth and metastasis of solid tumors [20]. Accordingly, high expression of Gal-1 in the tumor cells and/or in TAS indicates poor prognosis of the disease [21]. Crucial role of Gal-1 in tumor angiogenesis has also been confirmed [22], [23]. Additionally, genetically engineered carcinoma-associated fibroblasts expressing low level of Gal-1 failed to help tumor progression [24]. High level of Gal-1 expression has been detected in MSCs [25] contributing to the T-cell regulating role of MSC in vitro [26].
Here we demonstrate an important role of MSC-derived Gal-1 in regulation of tumor growth and metastasis since the absence of Gal-1 expression results in the loss of tumor promoting effect of MSCs. In vitro studies show that the absence of Gal-1 in MSCs does not affect the number of migrating MSCs toward the tumor cells which is supported by the in vivo migration of intravenously injected MSCs into the tumor. Also the in vitro differentiation of endothelial cells into blood vessel-like structures strongly depends on the expression of Gal-1 in MSCs indicating its important role in tumor neo-angiogenesis. Vital role of MSC-derived Gal-1 in tumorigenesis has been further verified in Gal-1 knockout mice. Administering B16F10 melanoma into Gal-1 deficient animals, tumor growth is highly reduced compared to wild type animals. Nevertheless, co-injection of wild type but not Gal-1 deficient MSCs results in dramatic tumor progression confirming the essential role of Gal-1 expression in MSCs.
Materials and Methods
Ethics Statement
All mouse studies were done in accordance with national and international law and regulations of animal experiments and were reviewed and approved by the Institutional Animal Care and Use Committee of Biological Research Center, Hungarian Academy of Sciences.
Cells
Mouse breast cancer cell line, 4T1 (ATCC CRL-2539, Lot No: 3306022) [27] and mouse melanoma cells, B16F10 (ATCC CRL-6475, a kind gift of Dr. R. Kiss, Free University of Brussels, Belgium) [28] were maintained in RPMI complemented with 10% FCS, mouse endothelioma cells, H5V [29] (obtained from C Vizler, Biological Research Center, Hungary) and all types of mouse MSCs (established in our laboratories) were cultured in DMEM containing 10% FCS in a humidified incubator with 5% CO2 at 37°C. All cell culture media and FCS were purchased from Invitrogen (Carlsbad, USA, www.invitrogen.com).
Isolation of MSCs from bone marrow and adipose tissue was carried out according to Peister et al. [30] with some modifications as described previously [31], [32]. Characterization of the MSC cultures was performed by cytofluorimetry (FACSCalibur, Becton Dickinson) using CD34-FITC, R-Phycoerythrin-conjugated anti-mouse CD44, CD73, CD90, Sca-1 and biotinylated CD3ε, CD45R/B220, CD11b, Ly-6G, TER-119 (BD Pharmingen, Franklin Lakes, USA, www.bd.com) followed by Streptavidin-PE (Sigma-Aldrich, St. Louis, USA www.sigmaaldrich.com). Evaluation of the data occurred with CellQuest software (Becton Dickinson).
Extra- and intracellular Gal-1 in cells was detected by cytofluorimetry in non-permeabilized and permabilized cells using goat anti-mouse Gal-1 (R&D Systems) and donkey anti-goat Ig-NL493 conjugate (R&D Systems).
Osteogenic and adipogenic differentiation was induced by culturing confluent MSCs for 2 weeks in appropriate medium as described previously [31]. Photomicrographs were taken with Olympus CKX41 inverted light microscope and Olympus Camedia C-5060 camera (Tokyo, Japan, www.olympus-global.com).
The various MSC cultures were designated in the paper as follows: bone marrow and adipose tissue MSCs isolated from wild type animals = wtMSC, and wtA-MSCs, respectively MSC from Gal-1 knockout animals = MSCGal-1−/−, and A-MSC Gal-1−/−, MSCs transfected with Gal-1 silencing or scrambled (control) RNAi constructs = siMSC or scMSC, respectively.
Silencing galectin-1 in MSCs
The method for silencing of galectin-1 gene has been previously described [33]. The following modifications have been introduced: human (hGalec120si) and mouse (mGalec340si) galectin-1 specific and scrambled (hGalec120sc and mGalec340sc) oligonucleotides were used to produce the silencing siRNA molecules (Table S1), which were designed to knock-down human (GenBank accession number BC020675.1) and mouse (GenBank accession number NM_008495.2) Gal-1.
The resulted four plasmid constructs were as follows: pSNhG120si, pSNmG340si for galectin-1 knock-down and pSNhG120sc and pSNmG340sc for control experiments, respectively. Mouse wtMSCs (106 cells) were co-nucleofected with the combination of 1+1 µg pSNGh120si and pSNmG340si for silencing or identical amounts of pSNhG120sc and pSNmG340sc plasmids for obtaining controls. Nucleofection was performed on an Amaxa Nucleofector with the A-027 program and MEF Nucleofector Kit 1 (Lonza Amaxa, Walkersville, USA, www.lonzabio.com). Clone selection lasted 11 days in DMEM, 10% FBS, 5% Horse Serum, 1× NEAA, 1× PenStrep, 1× GlutaMAX (all medium components were obtained from Invitrogen, and 1 mg/ml G418 (Sigma-Aldrich, St. Luis, USA).
Animal model
Number of mice included into each experimental group is indicated under the particular figure legend. The in vivo experiments were repeated independently three times and representative of the three experiments have been presented in the paper.
Female Balb/C and male C57BL/6 or Gal-1 knockout (strain: B6.Cg-Lgals1 tm1Rob/J, 006337, Jackson Laboratory, Bar Harbor, USA, www.jax.org) as well as X-SCID (strain: B6;129S7-Il7rtm1Imx/J, Jackson Laboratory, Bar Harbor, USA) mice (8–10 week old) were injected orthotopically with 4T1 breast carcinoma cells or subcutaneously with B16F10 melanoma cells into the right flank without or in combination with MSCGal-1−/− or MSCs expressing various amount of Gal-1 (wtMSC, scMSC or siMSC). In another model, Balb/C mice were orthotopically injected with 105 4T1 cells and when tumors became palpable, MSCs were administered intravenously as indicated. The animals were housed individually or with littermates of identical sex and had free access to food and water.
Tumors were evaluated macroscopically by the following parameters: 1) Tumor size was measured at least twice a week with a precision caliper and calculated according to the formula: d2×D×0.5 [19], where d and D are the minor and major diameters, respectively; 2) incidence of palpable tumors was determined by the daily monitoring of animals in each experimental group; 3) after euthanizing the animals, weights of the excised primary tumors and lungs were measured after 4% formaldehyde fixation (Molar Chemicals, Budapest, Hungary, www.molar.hu); 4) metastatic nodules on the surface of lungs were counted under a stereo microscope (Leitz Wetzlar, Germany, www.ernst-leitz-wetzlar.de); 5) survival of experimental animals was estimated using Kaplan-Meier plot analysis.
Characterization of Gal-1 expression by Western blotting and QPCR
SDS-PAGE and Western Blot analysis
Cell lysates (105 MSCs, 2×105 4T1 or B16F10 cell equivalent/sample) were analyzed by Western blotting after running the samples on a 12%–17.5% gradient SDS-polyacrylamide gel (SDS-PAGE) then electro-transferred onto nitrocellulose membrane (Whatman® Protran, Kent, UK, www.whatman.com ®). After blocking with 3% gelatin (Sigma-Aldrich, St. Luis, USA) in TBS plus 0.05% Tween® 20 (Sigma-Aldrich, St. Luis, USA), the membrane was incubated with polyclonal rabbit anti-Gal-1 and HRP conjugated anti-rabbit immunoglobulin (Dako, Glostrup, Denmark, www.dako.com). Rabbit anti-Gal-1 was produced in our laboratory (for specificity control see Fig. S3). It reacted with monomer and dimer recombinant human Gal-1, gave one reactive band in wtMSC at the proper MW and none in MSCGal-1−/−. Rabbit anti-β-actin (Abcam, Cambridge, UK, www.abcam.com) was used as loading control. Immunoreactive proteins were visualized using the ECL Plus detection system (GE Healthcare Amersham™ Waukesha, USA, www.gelifesciences.com) on Agfa X-ray film (Mortsel, Belgium www.agfa.com). Molecular mass standard proteins: Page Ruler™ Prestained Protein Ladder (Fermentas, Glen Burnie, USA, www.fermentas.com).
QPCR
Total RNA was extracted using RNeasy Plus RNA isolation kit (QIAGEN, Germantown, USA, www.qiagen.com) according to manufacturer's instruction. cDNA was obtained using GoScript™ Reverse Transcriptase (Promega Corporation, Madison, USA, www.promega.com) from 2 µg of template total RNA per reaction. QRT-PCR was performed in triplicates using TaqMan® Gene Expression Master Mix (Applied Biosystems Inc, Foster City, USA, www.appliedbiosystems.com) for Lgals1, Ptgs2, Tgfb1 and IL10 and AccuPower® 2× Greenstar qPCR Master Mix (Bioneer, Daedeok-gu, Daejeon, South Korea) for VEGFA, angiopoietin1, ORP150 and BEX2 in RotoGene3000 instrument (Corbett Life Science, Sydney, Australia). Relative quantification of gene expression was determined by comparison of threshold values. All results were normalized to GAPDH. TaqMan® Gene Expression Assays were commercially available for Lgals1 (Mm00839408_g1), Ptgs2 (Mm00478374_m1), Tgfb1 (Mm01178820_m1), IL10 (Mm00439614_m1, GAPDH (Mm99999915_g1), and QPCR primers were designed using Universal ProbeLibrary Assay Design program (Roche Applied Science, https://www.roche-applied-,science.com/sis/rtpcr/upl/index.jsp?id=UP030000) for VEGFA angipoietin1, ORP150 and BEX2. VEGFA fwd: aaaaacgaaagcgcaagaaa, rev: tttctccgctctgaacaagg; Angiopoietin fwd: cggatttctcttcccagaaac, rev: tccgacttcatattttccacaa; ORP150 fwd: tggcgtgctcagtttagaca, rev:agagtagattcttcctctgggcta; Bex2 fwd: actacgccgcaagggatag, rev: tttcacgccttgttccactt; GAPDH fwd: tttgatgttagtggggtctcg, rev: agcttgtcatcaacgggaag.
Histology and Biometrics
Paraffin embedded tissue sections: Embedding, processing and Hematoxylin and Eosin (Sigma-Aldrich, St. Luis, USA) staining was carried out as standard protocols. Microvessel density (MVD) was analyzed with morphological means and with visual inspection of areas filled with red blood cells using a microscope (Carl Zeiss Axio Imager.Z1 and Carl Zeiss AxioCam MRc5 camera, Oberkochen, Germany, www.zeiss.com) and evaluated with AxioVision software (AxioVs40 V 4.6.3.0 Carl Zeiss Imaging Solutions GmbH) based on 10 randomly selected non-overlapping fields of 3 different samples (vascularized (vasc.) area (%) = average vasc. area (µm2)/field (µm2)×100). Relative microvessel density (MVDrel) was calculated by the following equation MVDrel = MVD(4T1+MSC)/MVD4T1, where MVD(4T1+MSC) = microvessel density of tumors initiated in the presence of 4T1 breast carcinoma and MSCs, MVD4T1 = microvessel density of tumors initiated with injection of 4T1 breast carcinoma alone.
Percentage of lung metastatic area was determined by the measurement of cumulated macrometastatic areas divided with the total lung tissue area ×100.
Frozen tissue sections (7 µm thick) were prepared according to the standard protocol. To track the localization of MSCs within the frozen tissue sections MSCs were pre-labeled with CM-DiI (Invitrogen, www.invitrogen.com). The sections were counter-stained with DAPI (Vector Laboratories, Burlingame, USA, www.vectorlabs.com) and mounted in Fluoromount G (Southern Biotech). CM-DiI labeled MSCs were visualized using laser scanning confocal microscope (Olympus FV 1000, Olympus Holding Europa GmbH, Hamburg, Germany, www.olympus-europa.com).
In vitro capillary formation assay
MSCs were pre-labeled with CM-DiI according to the manufacturer's protocol. Then they were co-cultured with unlabeled mouse heart capillary endothelial cells, H5V in a ratio of 1∶1 in a 24-well plate (Orange Scientific, Braine-l'Alleud, Belgium) in the presence or absence of 30 mM sucrose (Sigma, St. Luis, USA) or thiodigalactoside (TDG, Carbosynth LTD). Separately cultured MSCs or H5V cells served as controls. Capillary formation was evaluated as follows: five randomly selected non-overlapping areas of co-cultured cells were examined by fluorescence microscope (Olympus IX81, Olympus Holding Europa GmbH, Hamburg, Germany, www.olympus-europa.com). Tubes were quantified by measuring the length of capillary-like structures with CellR Imaging Software Software (Olympus Holding Europa GmbH, Hamburg, Germany) after 3 days of cell cultures.
In vitro migration assay of MSCs
2D migration test was performed in ibiTreat Ibidi µ-Dish 35 mm,high Grid-500 culture (Ibidi, München, Germany, www.ibidi.com) dish. The two insert reservoirs were plated with 104 MSCs pre-labeled with CM-DiI and 3×104 4T1 breast carcinoma cells in 70 µl of culture medium, respectively. Proliferation of the cells was blocked with 5 mM hydroxyurea (Sigma-Aldrich, St. Luis, USA) for 8 hours. At the starting time point the inserts were removed and migration was let for 16 hours in cell culture medium containing 5 mM hydroxyurea. The migration was stopped by fixing the cells with 4% paraformaldehyde (Sigma-Aldrich, St. Luis, USA) in PBS for 4 minutes at room temperature then washed with PBS. The nuclei of the cells were stained with Hoechst33342 fluorescent dye (Sigma-Aldrich, St. Luis, USA) for 30 min at 37°C. Snapshot photographs of initial and end state was taken with fluorescent microscope (Olympus IX81). Migrating cells were counted in 5 fields of 3 independent experiments and the migration distance was analyzed by ImageJ software (free access provided by NIH).
Statistical analysis
Statistical analysis was performed using Student's t-test to evaluate the statistical significance (set at * p<0.05, ** p<0.01, *** p<0.001) between two given experimental groups.
Results
Characterization of MSCs and tumor cell lines
All types of MSCs including those of wild type (wtMSC), Gal-1 knocked down (siMSC), control cells transfected with scrambled RNA (scMSC) and Gal-1 knockout (MSCGal-1−/−) cells expressed CD44, CD73, CD90 and Sca-1 (Fig. S1) but not markers of cells of hematopoietic origin, CD34, CD45R, Ly6G, CD3, CD11b, TER119 (data not shown), and differentiated into adipogenic and osteogenic directions (Fig. S2). Western blotting analysis showed that wt and scMSCs expressed abundant, siMSCs low level and MSCGal-1−/− none of Gal-1 (Fig. S3A). Tumor cell lines, 4T1 breast carcinoma and B16F10 melanoma cells also expressed Gal-1 although Gal-1 production in B16F10 was lower than in 4T1 (Fig. S3B and C). As Gal-1 level in MSCs and tumor cell lines is critical, it was quantified using QPCR. As shown on Fig. S3C 4T1 expressed 2 fold Gal-1 as wtMSC, while B16F10 melanoma cells produced only 20% of Gal-1 in wtMSC. Another crucial point is the localization of Gal-1 in MSCs as Gal-1 may function as intra- or extracellular factor. Fig. S3D shows that Gal-1 is present in both cellular compartments, however amount of secreted Gal-1 on B16F10 cell surface is less than on 4T1 (Fig. S3D).
MSCs produce tumor growth regulating factors other than Gal-1. Therefore the major factors affecting tumor growth, COX2 (PGE2 producing enzyme), TGF-β1, angiopoietin1, IL-10 and VEGF in wtMSCs and MSCGal-1−/− were analyzed. The expressions of these factors showed that COX2, TGF-β1 and angiopoietin1 mRNAs were expressed at similar level and IL-10 was not produced in either MSC lines. VEGF expression was slightly higher in MSCGal-1−/− than in wtMSCs (Fig. S3E). Recent papers [34], [35] implicated ORP150, a major pro-angiogenic gene and BEX2 (brain-expressed X-linked gene) in Gal-1 triggered pathways of in vivo and in vitro angiogenesis in glioblastoma tumors. Due to the importance of these gene products regulating tumor vascularization and being intimate signaling target for Gal-1 in brain tumors, QPCR experiments were carried out in wtMSCs and MSCGal-1−/− cells. As showed on Fig. S3F BEX2 was not expressed in the cells irrespective their Gal-1 expression. Although ORP150 was expressed, its expression did not depend on the presence or absence of Gal-1 in MSCs.
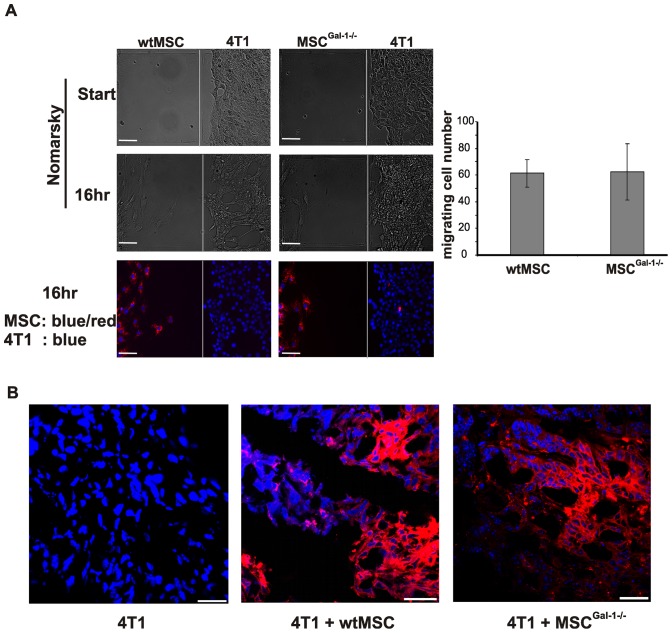
Role of MSC-derived Gal-1 in MSC localization in the tumor tissue
To determine whether Gal-1 expression in MSCs contributed to the localization and survival of MSCs within the tumor environment, first an in vitro migration assay was carried out (Fig. 1A). Neither absence of Gal-1 in MSCGal-1−/− (Fig. 1A) nor reduction of Gal-1 in siMSCs (data not shown) affected the number of the migrating cells (Fig. 1A graph). There was no migration observed when MSCs were cultured alone in the migration plate (data not shown). Accordingly, in vivo migration of intravenously injected MSCs (expressing fluorescence protein, Venus) into pre-existing tumor bearing mice was not influenced by expression of Gal-1 when measured on the 7th day following MSC injection (data not shown). Analysis of the frozen tumor tissue sections obtained from animals co-injected with 4T1 breast carcinoma cells and fluorescent dye labeled wtMSCs or MSCGal-1−/− showed no difference between the localization of the different MSCs (Fig. 1B). The siMSCs and scMSCs persisted in the tumor similarly to wtMSCs (data not shown).
Figure 1. Galectin-1 expression in MSCs does not affect their localization within the tumor.
(A) Migration of CM-DiI labelled wtMSCs and MSCGal-1−/− (red) toward 4T1 tumor cells in vitro was followed for 16 h in Ibidi dish. All nuclei were visualized with Hoechst33342 (blue), and images were taken with fluorescent microscope. MSCs migrating to the cell free zone were counted and the average of 3 independent experiments was presented on the diagram (right panel). (B) Female Balb/C mice were challenged by 4T1 cells alone (103 cells) (left) or in combination with 105 wtMSC (middle) or MSCGal-1−/− (right) pre-labeled with CM/DiI (red). Cryosections of primary tumors were counter-stained with DAPI (blue) and analyzed with a confocal microscope. Representative images of 60 sections obtained from 3 independent experiments are shown. Scale bar: 30 µm.
Gal-1-dependent enhancement of tumor growth
In vitro analysis of tumor cell growth in the presence of wt or MSCGal-1−/− was carried out. Neither supernatant of MSCs nor their direct interaction with tumor cells in co-culture affected growth of 4T1 or B16F10 tumor cells regardless of their Gal-1 expression (data not shown) indicating that MSCs did not directly act on tumor cell proliferation.
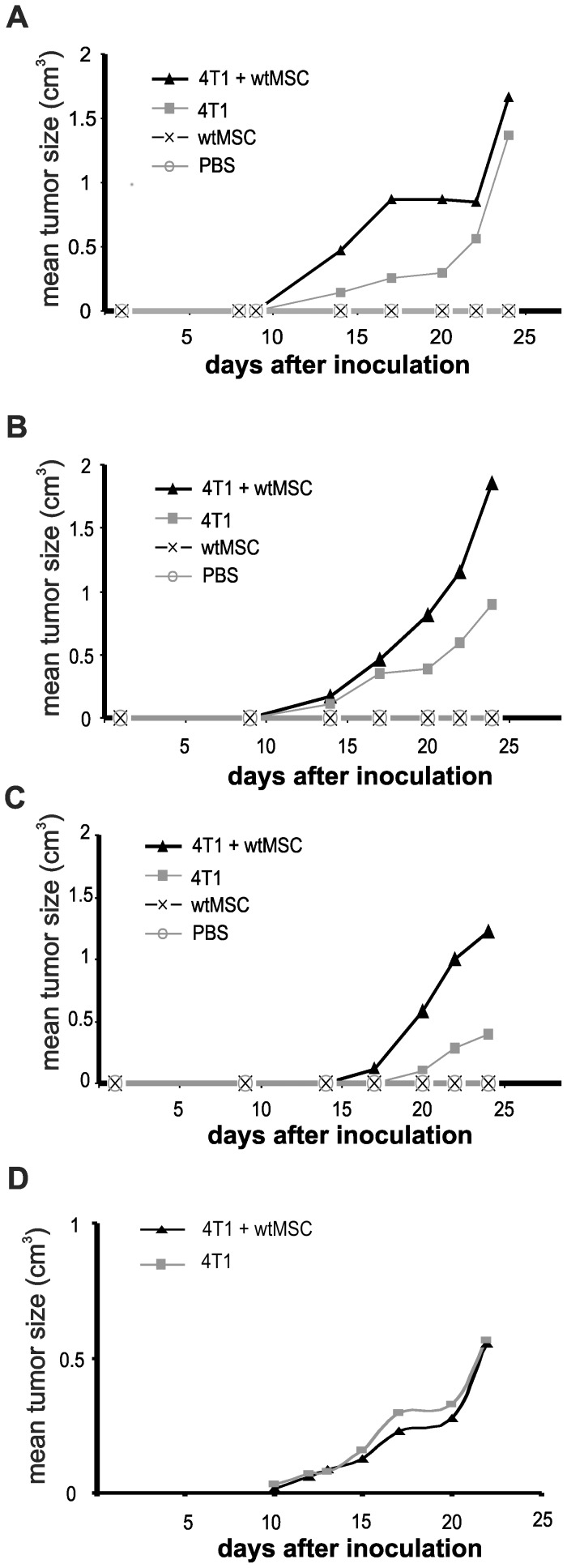
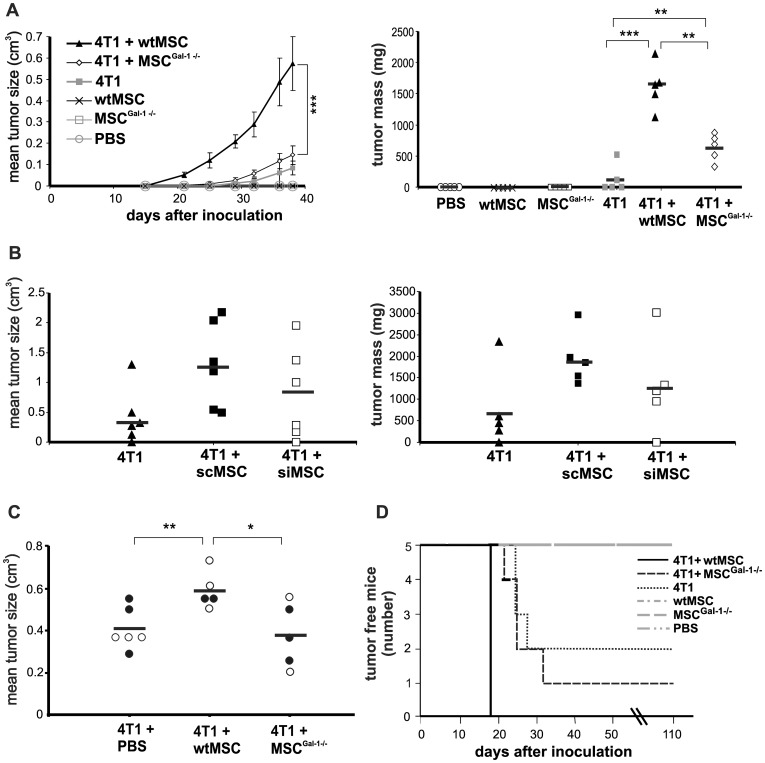
Balb/C mice were injected with syngeneic 4T1 breast carcinoma cells with or without wtMSCs or MSCsGal-1−/−. MSC-tumor cell ratio varied as 1∶1, 10∶1 and 100∶1. MSC number was kept at 105 and tumor cell number was changed. In all variations wt MSCs supported tumor growth. In contrast, when MSC number was decreased to 104, in spite of the MSC-tumor cell ratio remained at 1∶1, MSC failed to affect tumor growth (Fig. 2). This result indicated that MSC number used to modulate tumor growth was a crucial point when playing role in early tumor development. Tumor cells and MSCs were applied in 1∶100 ratio in the further experiments, since it was the most effective combination in this setup. Tumor volume and weights were increased >5-fold (Fig. 3A left) and >7-fold (Fig. 3A right), respectively by wtMSCs on the 40th day and the tumors were palpable much earlier (20th versus 32nd day) compared to that of induced by tumor cells alone. In contrast to wild type MSCs, co-injection of Gal-1 deficient MSC did not affect tumor development either in size, timing (Fig. 3A, left) or weight (Fig. 3A, right). Co-injection of siMSCs expressing low but detectable amount of Gal-1 (Fig. S3A) resulted in a reduction of tumor growth compared to the effect of control scMSCs (Fig. 3B). This result was reproducible but not significant indicating that low amount of Gal-1 in MSCs was sufficient to exert some tumor promoting effect. MSCs alone did not generate tumor development in 110 days follow up (Fig. 3A and Fig. 3D).
Figure 2. Tumor promoting activity of MSCs depends on the number of MSCs and ratio of MSCs/tumor cells injected.
Different numbers of 4T1 breast carcinoma cells (A: 105; B and D: 104; C:103) were injected with or without 105 (A–C) or 104 (D) MSCs into Balb/C female mice and tumor size was regularly measured with a special caliper. n = 5.
Figure 3. Deficiency of Gal-1 in knockout MSCs diminishes the tumor promoting effect of MSCs.
Female Balb/C mice were challenged by orthotopic inoculation of 103 4T1 cells alone or in combination with 105 wtMSCs or MSCGal-1−/− (A) or scMSCs or siMSCs (B). C) Tumor bearing (initiated by injection of 105 4T1 cells) mice were injected intravenously once with 106 (open circles) or twice with 3×105 (black circles) wtMSCs or MSCGal-1−/−. Tumor size (A left panel) was monitored daily or on the 40th (B left panel) or 20th day (C) after tumor initiation. Tumor mass was determined by measuring the formaldehyde fixed primary tumors isolated from sacrificed mice (A and B, right panels). Control mice were injected with PBS or MSCs without tumor cells. Data represent the mean ± SD. Significance on A left graph was calculated only for data on day 38. Number of animals in the experimental groups: A left panel: n = 5, A right panel: n = 5, B left panel: n = 6, B right panel: n = 5, C n = 5–6. ** p<0.01, *** p<0.001. D) Tumor incidence of mice challenged with 103 4T1 cells alone or in the combination with 105 wtMSCs or MSCGal-1−/− was evaluated using Kaplan-Meier analysis. Control mice were injected with PBS, wtMSC or MSCGal-1−/−. Mice were considered as tumor bearing when the tumor was palpable. Tumor free animals were surveyed up to 110 days. n = 5.
Whether MSC and MSC-derived Gal-1 affected growth of pre-existing tumors, mice carrying palpable breast tumor were transplanted with a single or a couple of injection with 106 or 3×105 MSCs, respectively. As Fig. 3C shows, injection of wtMSCs resulted in significantly higher tumor growth as compared to mice untreated with MSCs or treated with Gal-1 knockout MSCs indicating that Gal-1 in MSCs contribute to the MSCs' tumor-promoting activity in pre-existing tumors as well.
Analysis of incidence of palpable tumor showed that all mice, co-administered with 4T1 and wtMSC, developed tumors within 18 days (Fig. 3D). Nevertheless, injection of 4T1 alone or in combination with MSCsGal-1−/− showed delayed tumor growth occurring between 21–32 days after initiation of the tumor (Fig. 3D). Examination of the survival of the animals in the different groups (Fig. S4) was carried out on limited number of mice due to sparing suffering of animals. Since one of five mice injected with 4T1 and wtMSC deceased as early as 38 days following tumor initiation, one mouse of each group was sacrificed before tumor-caused death for further analysis at the same time. Evaluation of the remaining animals' survival showed good correlation with the results of tumor incidence since all mice injected with 4T1 and wtMSC died within 45 days while those obtaining 4T1 or 4T1 and MSCsGal-1−/died between 45 and 85 days after tumor initiation. Moreover 1 and 2 animals survived over 110 days in the groups injected with 4T1 and MSCsGal-1−/− and 4T1 alone, respectively.
To see whether MSC-derived Gal-1 enhanced tumor growth by contributing to establishment of tumor immuno-privilege similarly to tumor-cell derived Gal-1 did [18], [19], B16F10 melanoma cells were co-injected with wtMSCs or MSCGal-1−/− into X-SCID immuno-compromised mice. Gal-1 deficient MSCs failed to support tumor growth while wtMSCs effectively enhanced tumor size compared to tumor cells injected without MSCs (Fig. S5). These results indicated that MSC-derived Gal-1 did not act via the immune response when supported tumor growth.
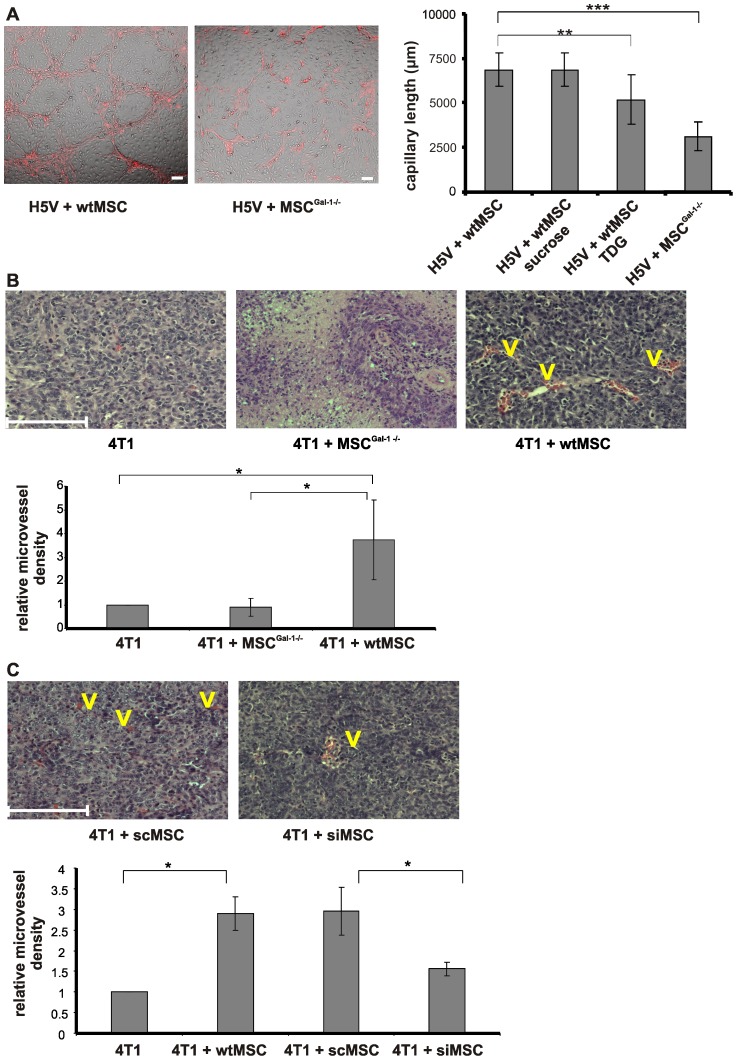
MSC-induced elevation of microvessel density of primary tumors requires Gal-1 expression by MSCs
To find out whether Gal-1 was implicated in MSC-regulated tumor vascularization, an in vitro capillary assay was carried out. As shown on Fig. 4A, the absence of Gal-1 in MSCs resulted in diminished blood vessel-like structure formation when co-cultured with H5V murine endothelial cells as compared to the effect of wtMSCs. Neither MSCs nor H5V cells formed vessel-like structures alone (data not shown). Competition of Gal-1 effect with lactose analogue, thiodigalactoside (TDG), but not sucrose (control disaccharide) also resulted in significant reduction of capillary formation (Fig. 4A) confirming not only the role of Gal-1 in vessel-like structure formation, but also the function of Gal-1 localized extracellularly. Accordingly, breast carcinoma was vascularized similarly when tumor cells were applied alone or together with MSCGal-1−/−. In contrast, wtMSCs dramatically increased the vascularization of the tumor (Fig. 4B). Interestingly, the vascularized area within the tumor showed significant decline when siMSCs were co-injected (Fig. 4C), supporting the reproducible but not significant decrease in the macroscopic parameters of the primary tumors (Fig. 3B). These results and the similar expression of other pro-angiogenic factors (VEGF, angiopoietin1 and ORP150, Fig. S3E and F) strongly indicated that Gal-1 in MSCs played an essential role in generating new capillary networks of the tumors. MSCs isolated from other source such as adipose tissue supported tumor vascularization on Gal-1 specific fashion (Fig. S6) similarly to bone marrow derived MSCs (Fig. 4).
Figure 4. MSC-derived Gal-1 influences the capillary formation of H5V endothelioma in vitro and increases the microvessel density of 4T1 tumors in vivo.
(A) In vitro capillary assay. CM-DiI labeled wtMSCs or MSCGal-1−/− (red) were incubated with mouse heart capillary endothelial cells (H5V) in a ratio of 1∶1 for 3 days (left) in the presence or absence of 30 mM sucrose or TDG. Tubes were quantified in parallel samples by measuring the length of capillary-like structures in five random areas of co-cultured cells (right). **p<0.001, ***p<0.0001. (B and C) In vivo analysis of microvessel density in tumors. Female Balb/C mice were challenged by 4T1 (103 cells) alone (B, left) or in combination with 105 MSCGal-1−/− (B, middle), wtMSC (B, right), scMSC (C, left) and siMSc (C, right). The presented microscopic pictures are representative of 3 experiments. Morphometric measurement of vascularized (V) areas (B and C lower panels) was performed on paraffin-embedded primary tumor tissue sections as described in Materials and methods. Scale bar is 100 µm. *p<0.05.
Gal-1 in MSCs is an important factor in promotion of tumor metastasis
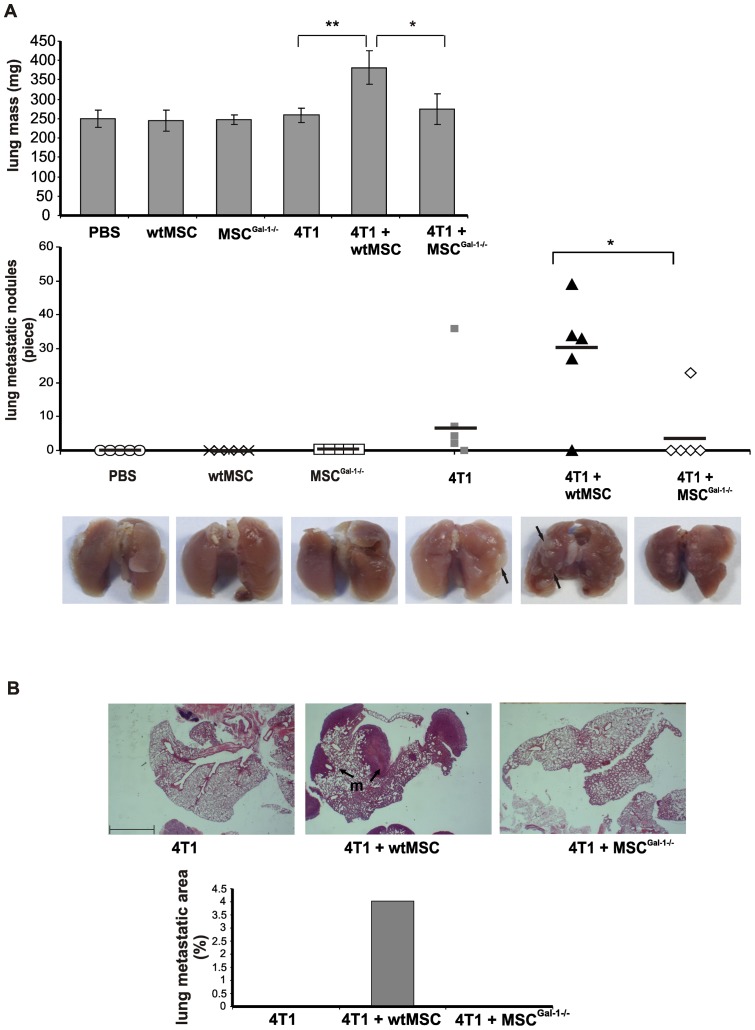
To determine the role of Gal-1 expression in MSCs regarding the frequency of lung metastasis, the lungs of differently treated animals were macroscopically surveyed (Fig. 5A) after sacrificing them. Average lung weights were around 250 mg in all experimental groups, except those from mice co-injected with 4T1 and wtMSCs which was significantly higher. Moreover, co-transplantation of wtMSCs resulted in a significant elevation of the number of lung metastatic nodules compared to that induced with MSCGal-1−/− or tumor cells alone.
Figure 5. MSC-derived Gal-1 promotes tumor metastasis.
Lungs were isolated from mice treated as described under Fig. 3. and fixed with formaldehyde. The lungs were weighed (A upper panel) and the metastatic nodules (marked with black arrows) were counted (A lower panel). * p<0.05, ** p<0.01, n = 5. Control mice were injected with either PBS, wtMSC or MSCGal-1−/−. (B) Micro-metastases were evaluated on paraffin-embedded, haematoxylin-eosin-stained lung sections. Metastases (m) are delineated by black arrows. Percentage of lung metastatic area (lower graph) was determined as described in Materials and methods. Scale bar: 1 mm.
Accordingly, histochemical analysis of the lung tissues showed that the ratio of the metastatic area versus the whole lung section isolated from wtMSCs co-injected animals were much higher than in lungs of animals transplanted with tumor cells alone or in combination with MSCGal-1−/− (Fig. 5B). These results implied that Gal-1 expression in MSCs efficiently contributed to promotion of metastasis.
Tumorigenic effect of endogenous Gal-1 versus MSC-derived Gal-1
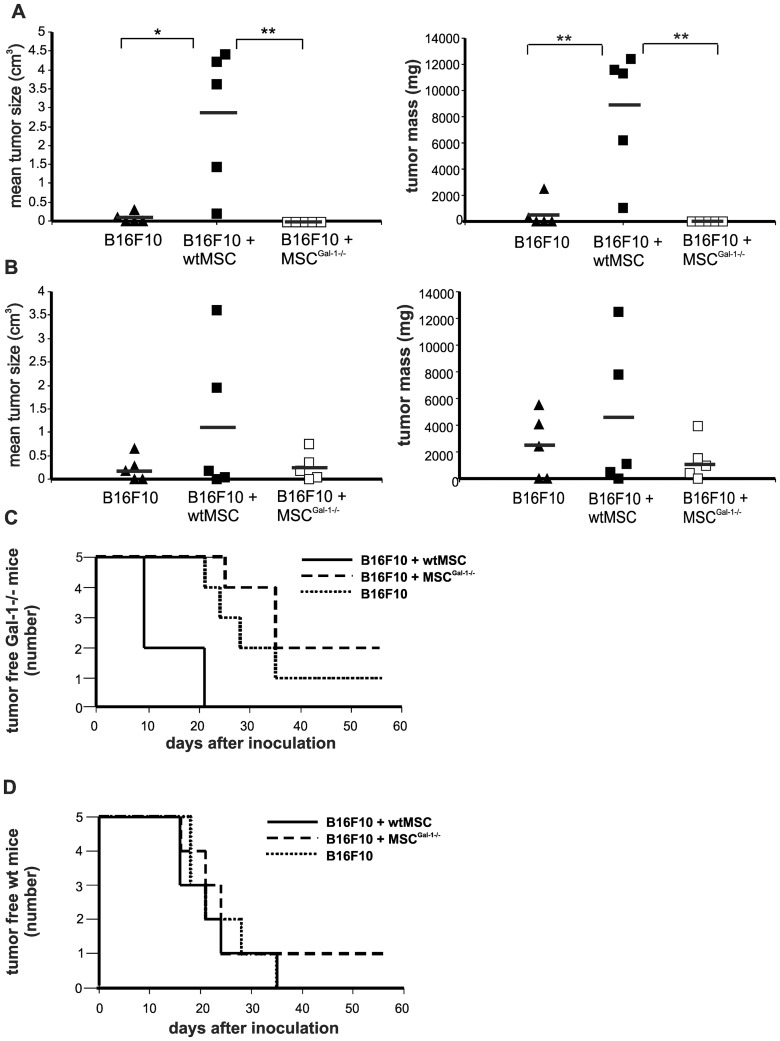
To find out whether endogenous Gal-1 affected tumor growth we changed breast carcinoma to melanoma model to be able to use syngeneic tumor conditions. Wild type (wt) C57BL/6 or Gal-1 knockout (Gal-1−/−) B6.Cg-Lgals1 tm1Rob/J mice were treated with syngeneic B16F10 melanoma cells with or without wtMSCs or MSCsGal-1−/− (Fig. 6). Hardly detectable tumors were observed when Gal-1−/− mice were injected with melanoma cells alone (Fig. 6A) compared to those in wt animals (Fig. 6B) on the 24th day of injection. Co-transplantation of wtMSCs with melanoma cells accelerated tumor development in wild type mice although the enhancement was not statistically significant (Fig. 6B) in contrast to growth promoting effect of wtMSCs on the growth of breast carcinoma (Fig. 3A). The difference between the two tumor types could be attributed to the extremely high aggressiveness of melanoma. More importantly wtMSCs significantly and dramatically supported melanoma growth in Gal-1−/− mice (Fig. 6A and C). In contrast, transplantation of tumor cells together with MSCsGal-1−/− did not promote tumor appearance until the 23rd day in Gal-1 knockout mice (Fig. 6A). The presence of Gal-1 in MSCs seemed to be essential to support tumor development in knockout mice and Gal-1 expression in tumor cells was not sufficient to entirely by-pass the endogenous Gal-1 deficiency. Accordingly, tumor growth was urged in Gal-1−/− mice injected with tumor together with wtMSCs, resulting in no tumor free animals within 21 days after transplantation. Those Gal-1 knockout animals which were injected with tumor cells alone or in the presence of Gal-1 deficient MSCs showed a delayed tumor growth as the first animals developed visible tumors on the 21st and 25th day and even after 60 days of observation one and two animals remained tumor free, respectively (Fig. 6C). Co-application of wtMSCs in wt mice hardly influenced the appearance of the tumor (Fig. 6D) indicating the aggressive growth of the melanoma.
Figure 6. MSC-derived Gal-1 is sufficient to induce early tumor development in Gal-1 knockout mice.
Five hundred B16F10 melanoma cells were subcutaneously injected alone or together with 105 wtMSCs or MSCGal-1−/− into Gal-1 knockout (B6.Cg-Lgals1 tm1Rob/J) (A and C) or wild type C57BL/6 (B and D) mice. Tumor size (cm3) and tumor mass (mg) were measured on day 23 (left) and on day 24 (right), respectively (A and B). * p<0.05, ** p<0.01, n = 5. Kaplan-Meier analysis was carried out to evaluate the development of palpable tumors in Gal-1 knockout (C) and wt (D) mice.
Discussion
Recently the stromal elements of solid tumors have obtained extensive attention since they serve as critical niche of the tumor tissue. Two elements of the tumor stroma, the tumor-associated fibroblasts (TAF) and myofibroblasts partially derive from bone marrow MSCs [3]. During tumor development, MSCs are mobilized into the circulation, migrate toward and engraft into the tumor microenvironment [36], [37]. In the tumors, MSCs favor tumorigenesis and tumor growth by differentiating into TAFs [12], [38], promoting neo-angiogenesis [11], [39] and establishing cancer stem cell niches with immunosuppressive effect [10], [14].
Opposite effects of exogenously administered MSCs on tumor progression have been recently demonstrated since MSCs supported or suppressed tumor growth [9]. Our findings are in accordance to those describing that MSCs promote tumor growth. Co-injection of MSCs with 4T1 breast carcinoma cells results in dramatic elevation of tumor size, weight, and tumor incidence while survival of the animals decrease. Moreover, transplantation of MSCs into pre-existing tumor bearing mice supports tumor growth on a fashion partially dependent of Gal-1 expression. In contrast, in melanoma model MSCs do not cause significant difference in tumor incidence compared to melanoma cells injected in the absence of MSCs demonstrating the high aggressiveness of the melanoma.
Tumor modulating effects of MSCs are attributed to numerous factors released into the tumor microenvironment [4]. One of the factors which MSCs produce and secrete is Gal-1 [25] however its function in tumor growth has not been revealed. Here we have identified Gal-1 as a novel, crucial factor in tumorigenic effect of MSCs. Tumor growth supporting function of Gal-1 knockout MSCs is significantly weaker compared to that of wild type MSCs.
MSCs are mobilized into the circulation upon hypoxia [40], a general feature of solid tumors, and attracted into the tumor by factors induced by hypoxia-induced factor1α (HIF1α), including VEGF, and SDF-1α [41]. Within the tumor, MSCs support tumor progression by enhancing neo-angiogenesis [42], contributing to the tumor immunoprivilege [10] and promoting metastasis [15]. Expression of Gal-1 is also regulated by hypoxia [43] and may serve as a mediator for all mentioned mechanisms including angiogenesis [22], [34]. We show that MSC-derived Gal-1 is implicated in formation of vessel-like structures in vitro since deficiency of Gal-1 expression in MSCs results in highly decreased tube formation in co-culture with H5V endothelial cells. In vivo data support these findings since wtMSCs increase microvessel density 4-fold, while MSCGal-1−/− does not affect it compared to the tumor triggered with breast cancer cells alone. This robust pro-angiogenic effect of MSC-derived Gal-1 becomes also obvious when siMSCs are applied together with breast carcinoma cells. Low amount of Gal-1 in the siMSCs is sufficient to partially sustain the overall tumor growth and a reduced tumor vascularization. It is of note, that tumor promoting effect of MSCs with reduced Gal-1 expression is between wtMSCs and Gal-1 deficient MSCGal-1−/−. Our in vitro and in vivo results are supported by the data published by Burns et al [44]. These authors have shown that immortalized human MSCs recruit endothelial cells and decellularized matrix produced by MSCs promote vascularization on a Gal-1 dependent manner.
Mesenchymal stromal cells enhance tumor metastasis in breast carcinoma models implicating the role of pro-angiogenic CCL5 [15]. Gal-1 also increases the metastatic potential of tumor cells since Gal-1 expression in breast cancer-associated stroma cells shows significant correlation between tumor invasiveness and lymph node metastases [45]. As it is shown here, Gal-1 in MSCs also contributes to breast cancer metastasis. While wtMSCs significantly enhance metastasis, MSCGal-1−/− do not modulate these parameters compared to those induced by breast cancer cells alone. In an other aspect, Tsunoda et al. describe the effect of infiltrating T-cells to tumor stroma and eventually to neo-angiogenesis [46]. We transplanted X-SCID mice, in which the immunological aspect of the tumor growth regulation was excluded, with B16F10 melanoma and wt or Gal-1 KO MSCs. Absence of Gal-1 in MSCs resulted in the failure of tumor promotion by MSCs indicating that MSCs' tumor supporting effect did not directly depend on the regulation of tumor specific immune response or tumor infiltrating immune cells.
Galectin-1 expression in the tumor cells substitutes endogenous Gal-1 in some extent as demonstrated in Gal-1 knockout mice [23], [47]. Tumor cells producing Gal-1 allows more effective tumor angiogenesis compared to that of Gal-1 non-expressing tumor cells [22] in mice lacking endogenous Gal-1. Other authors argue that tumor cell-derived Gal-1 contributes to tumor growth and metastasis by regulating immunosuppression [47] even in Gal-1 knockout mice. In spite of the different emphasis, these papers and our results agree that Gal-1 expression within the tumor tissue strongly affect tumor growth and metastasis. Accordingly, we have found that Gal-1 expressing melanoma grows in Gal-1 knockout mice, although tumor development is impaired as compared to that of wild type animals. However, co-injection of wtMSCs but not MSCGal-1−/− with melanoma cells into Gal-1 knockout mice results in exaggerated tumor growth comparable to that in wild type animals treated with melanoma and wtMSC. These results show that simultaneous expression of Gal-1 in the tumor cells and exogenously transplanted MSCs completely restores the tumor-growth deficiency in Gal-1 knockout animals. In this scenario we hypothesize, that endogenous stromal elements deficient in Gal-1 expression may fail to support the vascularization, a prerequisite step of tumor establishment indicating a crucial role for endogenous stroma in tumor development. This theory is experimentally supported as in vitro formation of blood vessel-like structures is reduced in the absence of Gal-1 in MSCs. The importance of endogenous Gal-1 in tumor-promotion is substantiated with results obtained using Gal-1 knockout mice; while injection of tumor cells alone or in combination with MSCGal-1−/− results in highly delayed tumor appearance in Gal-1 knockout animals, co-transplantation of wtMSCs by-passes the absence of endogenous Gal-1. Our unpublished results (Krenács et al.) and other reported data [45], [48], [49] show that high Gal-1 expression in the stromal elements of breast and prostate carcinoma as well as gastric adenocarcinoma well correlates with the invasiveness and bad prognosis of the cancer disease. Accordingly, the results presented here support the theory that Gal-1 expression in MSCs is determining in assisting effective tumor growth since exogenously added wild type but not Gal-1 knockout MSC is able to overcome the delayed tumor growth in the absence of endogenous Gal-1 in the stromal elements of Gal-1 knockout mice.
Identification of individual factors playing role of MSC-mediated tumor promotion gains special interest as using MSCs in cell-mediated tumor therapy (reviewed by Dwyer [50]) is a novel and promising tool in cancer treatment. However, due to the frequently existing differences between mouse and human cell functions, the role of human MSC-derived Gal-1 in human tumor progression requires further validation.
Supporting Information
Characterization of MSCs. wtMSC, MSCGal-1−/−, scMSCs or siMSCs were labeled with R-Phycoerythrin conjugated monoclonal antibodies against CD44, CD73, CD90 and Sca-1(black lines) and analyzed with cytofluorimetry. Gray areas depict negative controls.
(TIF)
Adipogenic and osteogenic differentiation of MSCs. Wild type MSCs, MSCGal-1−/−, scMSCs, siMSC were cultured in adipogenic (left panel) or osteogenic (right panel) medium. Lipid droplets and calcium deposits in the extracellular matrix were stained with Oil Red O and Alizarin Red S, respectively, and then analyzed with inverted light microscope. Scale bar: 50 µm.
(TIF)
Expression of Gal-1 and pro-tumorogenic factors in MSCs and tumor cell lines. Total cellular Gal-1 amounts in cell lysates prepared from wtMSCs, MSCGal-1−/−, scMSCs and siMSCs (A) or from tumor cells, 4T1 breast carcinoma and B16F10 melanoma (B) were analyzed with Western blotting. Recombinant human Gal-1 (B) was used as a positive control. Gal-1 was developed with rabbit anti-Gal-1 followed by anti-rabbit Ig–HRP and ECL Plus. Rabbit anti-β-actin was used as loading control. (C) Gal-1 expression was compared in the used MSC and tumor cell lines analyzing the Gal-1 mRNA amount using QPCR. (D) Extracellular (wtMSCs: upper left, 4T1: lower left and B1610: lower right) and total (wtMSCs: upper right) Gal-1 was examined in wtMSCs with cytofluorimetry in unpermeabilized and permeabilized cells, respectively using goat anti-mouse Gal-1 and donkey anti-goat Ig-NL493. The cell were analyzed with cytofluorimetry. Expressions of COX2, TGF-β1, IL-10, VEGFA, angiopoietin1(E) and ORP150 and BEX2 (F) genes were analyzed with QPCR in wtMSCs and MSCGal-1−/−.
(TIF)
Wild type but not Gal-1−/− MSCs reduce survival of mice with breast carcinoma. Survival of mice challenged with 103 4T1 cells alone or in combination with 105 wtMSCs or MSCGal-1−/− was evaluated using Kaplan-Meier analysis. Surviving of animals was surveyed up to 110 days. Number of animals in the experimental groups were: 4T1+wtMSC n = 5, 4T1+MSCGal-1−/− n = 4, 4T1 n = 4, wtMSC n = 4, MSCGal-1−/− n = 4, PBS n = 4.
(TIF)
wtMSCs but not MSCGal-1−/− enhances the tumor growth in immune deficient X-SCID mice. Five hundred B16F10 melanoma cells were injected subcutaneously alone or together with 105 wtMSCs or MSCGal-1−/− into male X-SCID mice (n = 4 per group). Tumor size was monitored and calculated as described under Figure 3.
(TIF)
Adipose tissue-derived MSCs increase the microvessel density of 4T1 tumors on a Gal-1 dependent fashion. Female Balb/C mice were challenged by 4T1 (103 cells) alone or in combination with 105 A-MSCGal-1−/− or wtA-MSC. Morphometric measurement of vascularized areas was performed on paraffin-embedded primary tumor tissue sections as described in Materials and methods.
(TIF)
List of siRNA oligonucleotides. Numbers in the name of oligonucleotides indicate the starting position of the 19 nucleotide long RNAi sequence in the human (hGalec) and murine galectin-1 (mGalec) mRNA and the appropriate scrambled controls.
(TIF)
Acknowledgments
We are grateful to Dr. Robert Kiss for the kind gift of B16F10 cell line, Andrea Gercsó for the excellent technical assistance, Mária Tóth and Márta Börcsök for the preparation of photographs and figures, Dr. Ferhan Ayaydin, Dr. Csaba Vizler, Dr. Éva Fekete and Nikolett Bódi for help and advice in microscopy, animal experiments and histochemistry, respectively and Balázs Odrovics (X-SCID mice), Erika Veres and the staff in the animal house for their kind helps.
Footnotes
Competing Interests: The authors have declared that no competing interests exist.
Funding: This work was supported by the Bástyai-Holczer Foundation and by grants from the Hungarian Scientific Research Fund: OTKA PD 75938 (http://www.otka.hu/), NKTH-OTKA CK 78007 (http://www.otka.hu/), NKTH-OTKA CK 78188 (http://www.otka.hu/), and OTKA K 69047 (http://www.otka.hu/). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Bergfeld SA, DeClerck YA. Bone marrow-derived mesenchymal stem cells and the tumor microenvironment. Cancer Metastasis Rev. 2010;29:249–261. doi: 10.1007/s10555-010-9222-7. doi: 10.1007/s10555-010-9222-7. [DOI] [PubMed] [Google Scholar]
- 2.Pietras K, Ostman A. Hallmarks of cancer: interactions with the tumor stroma. Exp Cell Res. 2010;316:1324–1331. doi: 10.1016/j.yexcr.2010.02.045. doi: 10.1016/j.yexcr.2010.02.045. [DOI] [PubMed] [Google Scholar]
- 3.Quante M, Tu SP, Tomita H, Gonda T, Wang SSW, et al. Bone marrow-derived myofibroblasts contribute to the mesenchymal stem cell niche and promote tumor growth. Cancer Cell. 2011;19:257–272. doi: 10.1016/j.ccr.2011.01.020. doi: 10.1016/j.ccr.2011.01.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Roorda BD, ter Elst A, Kamps WA, de Bont ESJM. Bone marrow-derived cells and tumor growth: contribution of bone marrow-derived cells to tumor micro-environments with special focus on mesenchymal stem cells. Crit Rev Oncol Hematol. 2009;69:187–198. doi: 10.1016/j.critrevonc.2008.06.004. doi: 10.1016/j.critrevonc.2008.06.004. [DOI] [PubMed] [Google Scholar]
- 5.Oswald J, Boxberger S, Jørgensen B, Feldmann S, Ehninger G, et al. Mesenchymal stem cells can be differentiated into endothelial cells in vitro. Stem Cells. 2004;22:377–384. doi: 10.1634/stemcells.22-3-377. doi: 10.1634/stemcells.22-3-377. [DOI] [PubMed] [Google Scholar]
- 6.Klopp AH, Spaeth EL, Dembinski JL, Woodward WA, Munshi A, et al. Tumor irradiation increases the recruitment of circulating mesenchymal stem cells into the tumor microenvironment. Cancer Res. 2007;67:11687–11695. doi: 10.1158/0008-5472.CAN-07-1406. doi: 10.1158/0008-5472.CAN-07-1406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang H, Cao F, De A, Cao Y, Contag C, et al. Trafficking mesenchymal stem cell engraftment and differentiation in tumor-bearing mice by bioluminescence imaging. Stem Cells. 2009;27:1548–1558. doi: 10.1002/stem.81. doi: 10.1002/stem.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kidd S, Spaeth E, Dembinski JL, Dietrich M, Watson K, et al. Direct evidence of mesenchymal stem cell tropism for tumor and wounding microenvironments using in vivo bioluminescent imaging. Stem Cells. 2009;27:2614–2623. doi: 10.1002/stem.187. doi: 10.1002/stem.187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Klopp AH, Gupta A, Spaeth E, Andreeff M, Marini F 3rd. Concise review: Dissecting a discrepancy in the literature: do mesenchymal stem cells support or suppress tumor growth? Stem Cells. 2011;29:11–19. doi: 10.1002/stem.559. doi: 10.1002/stem.559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Djouad F, Plence P, Bony C, Tropel P, Apparailly F, et al. Immunosuppressive effect of mesenchymal stem cells favors tumor growth in allogeneic animals. Blood. 2003;102:3837–3844. doi: 10.1182/blood-2003-04-1193. doi: 10.1182/blood-2003-04-1193. [DOI] [PubMed] [Google Scholar]
- 11.Sun B, Zhang S, Ni C, Zhang D, Liu Y, et al. Correlation between melanoma angiogenesis and the mesenchymal stem cells and endothelial progenitor cells derived from bone marrow. Stem Cells Dev. 2005;14:292–298. doi: 10.1089/scd.2005.14.292. doi: 10.1089/scd.2005.14.292. [DOI] [PubMed] [Google Scholar]
- 12.Spaeth EL, Dembinski JL, Sasser AK, Watson K, Klopp A, et al. Mesenchymal stem cell transition to tumor-associated fibroblasts contributes to fibrovascular network expansion and tumor progression. PLoS ONE. 2009;4:e4992. doi: 10.1371/journal.pone.0004992. doi: 10.1371/journal.pone.0004992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gong Z, Niklason LE. Use of human mesenchymal stem cells as alternative source of smooth muscle cells in vessel engineering. Methods Mol Biol. 2011;698:279–294. doi: 10.1007/978-1-60761-999-4_21. doi: 10.1007/978-1-60761-999-4_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nauta AJ, Fibbe WE. Immunomodulatory properties of mesenchymal stromal cells. Blood. 2007;110:3499–3506. doi: 10.1182/blood-2007-02-069716. doi: 10.1182/blood-2007-02-069716. [DOI] [PubMed] [Google Scholar]
- 15.Karnoub AE, Dash AB, Vo AP, Sullivan A, Brooks MW, et al. Mesenchymal stem cells within tumour stroma promote breast cancer metastasis. Nature. 2007;449:557–563. doi: 10.1038/nature06188. doi: 10.1038/nature06188. [DOI] [PubMed] [Google Scholar]
- 16.Hartmann MC, Dwyer RM, Costello M, Potter SM, Curran C, et al. Relationship between CCL5 and transforming growth factor-β1 (TGFβ1) in breast cancer. Eur J Cancer. 2011;47:1669–1675. doi: 10.1016/j.ejca.2011.05.001. doi: 10.1016/j.ejca.2011.05.001. [DOI] [PubMed] [Google Scholar]
- 17.Rabinovich GA, Ilarregui JM. Conveying glycan information into T-cell homeostatic programs: a challenging role for galectin-1 in inflammatory and tumor microenvironments. Immunol Rev. 2009;230:144–159. doi: 10.1111/j.1600-065X.2009.00787.x. doi: 10.1111/j.1600-065X.2009.00787.x. [DOI] [PubMed] [Google Scholar]
- 18.Stannard KA, Collins PM, Ito K, Sullivan EM, Scott SA, et al. Galectin inhibitory disaccharides promote tumour immunity in a breast cancer model. Cancer Lett. 2010;299:95–110. doi: 10.1016/j.canlet.2010.08.005. doi: 10.1016/j.canlet.2010.08.005. [DOI] [PubMed] [Google Scholar]
- 19.Rubinstein N, Alvarez M, Zwirner NW, Toscano MA, Ilarregui JM, et al. Targeted inhibition of galectin-1 gene expression in tumor cells results in heightened T cell-mediated rejection; A potential mechanism of tumor-immune privilege. Cancer Cell. 2004;5:241–251. doi: 10.1016/s1535-6108(04)00024-8. [DOI] [PubMed] [Google Scholar]
- 20.Rabinovich GA. Galectin-1 as a potential cancer target. Br J Cancer. 2005;92:1188–1192. doi: 10.1038/sj.bjc.6602493. doi: 10.1038/sj.bjc.6602493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Camby I, Le Mercier M, Lefranc F, Kiss R. Galectin-1: a small protein with major functions. Glycobiology. 2006;16:137R–157R. doi: 10.1093/glycob/cwl025. doi: 10.1093/glycob/cwl025. [DOI] [PubMed] [Google Scholar]
- 22.Thijssen VLJL, Postel R, Brandwijk RJMGE, Dings RPM, Nesmelova I, et al. Galectin-1 is essential in tumor angiogenesis and is a target for antiangiogenesis therapy. Proc Natl Acad Sci USA. 2006;103:15975–15980. doi: 10.1073/pnas.0603883103. doi: 10.1073/pnas.0603883103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Thijssen VL, Barkan B, Shoji H, Aries IM, Mathieu V, et al. Tumor cells secrete galectin-1 to enhance endothelial cell activity. Cancer Res. 2010;70:6216–6224. doi: 10.1158/0008-5472.CAN-09-4150. doi: 10.1158/0008-5472.CAN-09-4150. [DOI] [PubMed] [Google Scholar]
- 24.Wu M-H, Hong H-C, Hong T-M, Chiang W-F, Jin Y-T, et al. Targeting galectin-1 in carcinoma-associated fibroblasts inhibits oral squamous cell carcinoma metastasis by downregulating MCP-1/CCL2 expression. Clin Cancer Res. 2011;17:1306–1316. doi: 10.1158/1078-0432.CCR-10-1824. doi: 10.1158/1078-0432.CCR-10-1824. [DOI] [PubMed] [Google Scholar]
- 25.Silva WA, Jr, Covas DT, Panepucci RA, Proto-Siqueira R, Siufi JLC, et al. The profile of gene expression of human marrow mesenchymal stem cells. Stem Cells. 2003;21:661–669. doi: 10.1634/stemcells.21-6-661. doi: 10.1634/stemcells.21-6-661. [DOI] [PubMed] [Google Scholar]
- 26.Gieseke F, Böhringer J, Bussolari R, Dominici M, Handgretinger R, et al. Human multipotent mesenchymal stromal cells use galectin-1 to inhibit immune effector cells. Blood. 2010;116:3770–3779. doi: 10.1182/blood-2010-02-270777. doi: 10.1182/blood-2010-02-270777. [DOI] [PubMed] [Google Scholar]
- 27.Aslakson CJ, Miller FR. Selective events in the metastatic process defined by analysis of the sequential dissemination of subpopulations of a mouse mammary tumor. Cancer Res. 1992;52:1399–1405. [PubMed] [Google Scholar]
- 28.Fidler IJ. Biological behavior of malignant melanoma cells correlated to their survival in vivo. Cancer Res. 1975;35:218–224. [PubMed] [Google Scholar]
- 29.Garlanda C, Parravicini C, Sironi M, De Rossi M, Wainstok de Calmanovici R, et al. Progressive growth in immunodeficient mice and host cell recruitment by mouse endothelial cells transformed by polyoma middle-sized T antigen: implications for the pathogenesis of opportunistic vascular tumors. Proc Natl Acad Sci USA. 1994;91:7291–7295. doi: 10.1073/pnas.91.15.7291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Peister A, Mellad JA, Larson BL, Hall BM, Gibson LF, et al. Adult stem cells from bone marrow (MSCs) isolated from different strains of inbred mice vary in surface epitopes, rates of proliferation, and differentiation potential. Blood. 2004;103:1662–1668. doi: 10.1182/blood-2003-09-3070. doi: 10.1182/blood-2003-09-3070. [DOI] [PubMed] [Google Scholar]
- 31.Urbán VS, Kiss J, Kovács J, Gócza E, Vas V, et al. Mesenchymal stem cells cooperate with bone marrow cells in therapy of diabetes. Stem Cells. 2008;26:244–253. doi: 10.1634/stemcells.2007-0267. doi: 10.1634/stemcells.2007-0267. [DOI] [PubMed] [Google Scholar]
- 32.Hegyi B, Kudlik G, Monostori E, Uher F. Activated T-cells and pro-inflammatory cytokines differentially regulate prostaglandin E2 secretion by mesenchymal stem cells. Biochem Biophys Res Commun. 2012;419:215–220. doi: 10.1016/j.bbrc.2012.01.150. doi: 10.1016/j.bbrc.2012.01.150. [DOI] [PubMed] [Google Scholar]
- 33.Kovács-Sólyom F, Blaskó A, Fajka-Boja R, Katona RL, Végh L, et al. Mechanism of tumor cell-induced T-cell apoptosis mediated by galectin-1. Immunol Lett. 2010;127:108–118. doi: 10.1016/j.imlet.2009.10.003. doi: 10.1016/j.imlet.2009.10.003. [DOI] [PubMed] [Google Scholar]
- 34.Le Mercier M, Mathieu V, Haibe-Kains B, Bontempi G, Mijatovic T, et al. Knocking down galectin 1 in human hs683 glioblastoma cells impairs both angiogenesis and endoplasmic reticulum stress responses. J Neuropathol Exp Neurol. 2008;67:456–469. doi: 10.1097/NEN.0b013e318170f892. doi: 10.1097/NEN.0b013e318170f892. [DOI] [PubMed] [Google Scholar]
- 35.Le Mercier M, Fortin S, Mathieu V, Roland I, Spiegl-Kreinecker S, et al. Galectin 1 proangiogenic and promigratory effects in the Hs683 oligodendroglioma model are partly mediated through the control of BEX2 expression. Neoplasia. 2009;11:485–496. doi: 10.1593/neo.81526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Placencio VR, Li X, Sherrill TP, Fritz G, Bhowmick NA. Bone marrow derived mesenchymal stem cells incorporate into the prostate during regrowth. PLoS ONE. 2010;5:e12920. doi: 10.1371/journal.pone.0012920. doi: 10.1371/journal.pone.0012920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Goldstein RH, Reagan MR, Anderson K, Kaplan DL, Rosenblatt M. Human bone marrow-derived MSCs can home to orthotopic breast cancer tumors and promote bone metastasis. Cancer Res. 2010;70:10044–10050. doi: 10.1158/0008-5472.CAN-10-1254. doi: 10.1158/0008-5472.CAN-10-1254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Direkze NC, Hodivala-Dilke K, Jeffery R, Hunt T, Poulsom R, et al. Bone marrow contribution to tumor-associated myofibroblasts and fibroblasts. Cancer Res. 2004;64:8492–8495. doi: 10.1158/0008-5472.CAN-04-1708. doi: 10.1158/0008-5472.CAN-04-1708. [DOI] [PubMed] [Google Scholar]
- 39.Peters BA, Diaz LA, Polyak K, Meszler L, Romans K, et al. Contribution of bone marrow-derived endothelial cells to human tumor vasculature. Nat Med. 2005;11:261–262. doi: 10.1038/nm1200. doi: 10.1038/nm1200. [DOI] [PubMed] [Google Scholar]
- 40.Rochefort GY, Delorme B, Lopez A, Hérault O, Bonnet P, et al. Multipotential mesenchymal stem cells are mobilized into peripheral blood by hypoxia. Stem Cells. 2006;24:2202–2208. doi: 10.1634/stemcells.2006-0164. doi: 10.1634/stemcells.2006-0164. [DOI] [PubMed] [Google Scholar]
- 41.Liu L, Yu Q, Lin J, Lai X, Cao W, et al. Hypoxia-Inducible Factor-1α Is Essential for Hypoxia-Induced Mesenchymal Stem Cell Mobilization into the Peripheral Blood. Stem Cells Dev. 2011. Available: http://www.ncbi.nlm.nih.gov/pubmed/21275821. Accessed 17 August 2011. [DOI] [PubMed]
- 42.Suzuki K, Sun R, Origuchi M, Kanehira M, Takahata T, et al. Mesenchymal stromal cells promote tumor growth through the enhancement of neovascularization. Mol Med. 2011;17:579–587. doi: 10.2119/molmed.2010.00157. doi: 10.2119/molmed.2010.00157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zhao X-Y, Chen T-T, Xia L, Guo M, Xu Y, et al. Hypoxia inducible factor-1 mediates expression of galectin-1: the potential role in migration/invasion of colorectal cancer cells. Carcinogenesis. 2010;31:1367–1375. doi: 10.1093/carcin/bgq116. doi: 10.1093/carcin/bgq116. [DOI] [PubMed] [Google Scholar]
- 44.Burns JS, Kristiansen M, Kristensen LP, Larsen KH, Nielsen MO, et al. Decellularized matrix from tumorigenic human mesenchymal stem cells promotes neovascularization with galectin-1 dependent endothelial interaction. PLoS ONE. 2011;6:e21888. doi: 10.1371/journal.pone.0021888. doi: 10.1371/journal.pone.0021888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Jung E-J, Moon H-G, Cho BI, Jeong C-Y, Joo Y-T, et al. Galectin-1 expression in cancer-associated stromal cells correlates tumor invasiveness and tumor progression in breast cancer. Int J Cancer. 2007;120:2331–2338. doi: 10.1002/ijc.22434. doi: 10.1002/ijc.22434. [DOI] [PubMed] [Google Scholar]
- 46.Tsunoda S, Sakurai H, Saito Y, Ueno Y, Koizumi K, et al. Massive T-lymphocyte infiltration into the host stroma is essential for fibroblast growth factor-2-promoted growth and metastasis of mammary tumors via neovascular stability. Am J Pathol. 2009;174:671–683. doi: 10.2353/ajpath.2009.080471. doi: 10.2353/ajpath.2009.080471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Banh A, Zhang J, Cao H, Bouley DM, Kwok S, et al. Tumor Galectin-1 Mediates Tumor Growth and Metastasis through Regulation of T-Cell Apoptosis. Cancer Res. 2011;71:4423–4431. doi: 10.1158/0008-5472.CAN-10-4157. doi: 10.1158/0008-5472.CAN-10-4157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.van den Brûle FA, Waltregny D, Castronovo V. AID-PATH730>3.0.CO;2-2. 2001.
- 49.Bektas S, Bahadir B, Ucan BH, Ozdamar SO. CD24 and galectin-1 expressions in gastric adenocarcinoma and clinicopathologic significance. Pathol Oncol Res. 2010;16:569–577. doi: 10.1007/s12253-010-9248-8. doi: 10.1007/s12253-010-9248-8. [DOI] [PubMed] [Google Scholar]
- 50.Dwyer RM, Khan S, Barry FP, O'Brien T, Kerin MJ. Advances in mesenchymal stem cell-mediated gene therapy for cancer. Stem Cell Res Ther. 2010;1:25. doi: 10.1186/scrt25. doi: 10.1186/scrt25. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Characterization of MSCs. wtMSC, MSCGal-1−/−, scMSCs or siMSCs were labeled with R-Phycoerythrin conjugated monoclonal antibodies against CD44, CD73, CD90 and Sca-1(black lines) and analyzed with cytofluorimetry. Gray areas depict negative controls.
(TIF)
Adipogenic and osteogenic differentiation of MSCs. Wild type MSCs, MSCGal-1−/−, scMSCs, siMSC were cultured in adipogenic (left panel) or osteogenic (right panel) medium. Lipid droplets and calcium deposits in the extracellular matrix were stained with Oil Red O and Alizarin Red S, respectively, and then analyzed with inverted light microscope. Scale bar: 50 µm.
(TIF)
Expression of Gal-1 and pro-tumorogenic factors in MSCs and tumor cell lines. Total cellular Gal-1 amounts in cell lysates prepared from wtMSCs, MSCGal-1−/−, scMSCs and siMSCs (A) or from tumor cells, 4T1 breast carcinoma and B16F10 melanoma (B) were analyzed with Western blotting. Recombinant human Gal-1 (B) was used as a positive control. Gal-1 was developed with rabbit anti-Gal-1 followed by anti-rabbit Ig–HRP and ECL Plus. Rabbit anti-β-actin was used as loading control. (C) Gal-1 expression was compared in the used MSC and tumor cell lines analyzing the Gal-1 mRNA amount using QPCR. (D) Extracellular (wtMSCs: upper left, 4T1: lower left and B1610: lower right) and total (wtMSCs: upper right) Gal-1 was examined in wtMSCs with cytofluorimetry in unpermeabilized and permeabilized cells, respectively using goat anti-mouse Gal-1 and donkey anti-goat Ig-NL493. The cell were analyzed with cytofluorimetry. Expressions of COX2, TGF-β1, IL-10, VEGFA, angiopoietin1(E) and ORP150 and BEX2 (F) genes were analyzed with QPCR in wtMSCs and MSCGal-1−/−.
(TIF)
Wild type but not Gal-1−/− MSCs reduce survival of mice with breast carcinoma. Survival of mice challenged with 103 4T1 cells alone or in combination with 105 wtMSCs or MSCGal-1−/− was evaluated using Kaplan-Meier analysis. Surviving of animals was surveyed up to 110 days. Number of animals in the experimental groups were: 4T1+wtMSC n = 5, 4T1+MSCGal-1−/− n = 4, 4T1 n = 4, wtMSC n = 4, MSCGal-1−/− n = 4, PBS n = 4.
(TIF)
wtMSCs but not MSCGal-1−/− enhances the tumor growth in immune deficient X-SCID mice. Five hundred B16F10 melanoma cells were injected subcutaneously alone or together with 105 wtMSCs or MSCGal-1−/− into male X-SCID mice (n = 4 per group). Tumor size was monitored and calculated as described under Figure 3.
(TIF)
Adipose tissue-derived MSCs increase the microvessel density of 4T1 tumors on a Gal-1 dependent fashion. Female Balb/C mice were challenged by 4T1 (103 cells) alone or in combination with 105 A-MSCGal-1−/− or wtA-MSC. Morphometric measurement of vascularized areas was performed on paraffin-embedded primary tumor tissue sections as described in Materials and methods.
(TIF)
List of siRNA oligonucleotides. Numbers in the name of oligonucleotides indicate the starting position of the 19 nucleotide long RNAi sequence in the human (hGalec) and murine galectin-1 (mGalec) mRNA and the appropriate scrambled controls.
(TIF)