Abstract
This paper provides an introduction to Geographical Information Systems (GIS) and how they can be used. It reviews the current state of GIS use in health care before identifying the barriers to more pervasive use of GIS in health. Finally, it makes recommendations for the direction of health GIS research over the next decade and concludes with a call to action to health informatics researchers to stop ignoring a tool and methodology that has such immense potential for improving the health of our communities.
Keywords: Geographic Information Systems, Public Health Informatics, Medical Informatics, Public Health, Epidemiology
I. Introduction
Given that we know that patients tend to access health care services within their local geographic communities, the application of geographical information systems (GIS) to health service planning & provision would seem a logical progression. However, whilst the use of GIS in public health & epidemiology (for example, to map incidence and prevalence of disease) is reasonably well developed [1] the use of such technologies in understanding health service access, utilization and demand remains to be explored [2,3].
When used to the full extent of its capability, GIS can "inform and educate (professionals and the public); empower decision making at all levels; help in planning and tweaking clinically and cost-effective actions, in predicting outcomes before making any financial commitments and ascribing priorities in a climate of finite resources; change practices; and continually monitor and analyze changes, as well as sentinel events [4]." Yet, despite the incredible potential benefits of applying GIS technologies, their use in health service planning and provision remains greatly underutilized.
The aim of this paper is to provide an introduction to GIS and how it can be used, to review the current state of GIS use in health care, to identify the barriers to more pervasive use of GIS in health and to make recommendations for the direction of health GIS research over the next decade.
II. History
The concept of considering spatial data when seeking to understand the prevalence and incidence of disease is intrinsic to the fields of epidemiology and public health. The most well known use of GIS, in a rudimentary form, is that of Dr. John Snow in London, England, in 1854 when he mapped the incidences of a cholera outbreak demonstrating that a specific water pump was the cause of infection [5]. Removing the handle from that pump almost immediately reduced the number of cases of cholera; though Snow himself points out that the numbers were already diminishing when he removed the pump handle.
On a wider scale today the World Health Organization (WHO) issues disease alerts that are mapped at http://www.healthmap.org and provided in near-real time. Traditionally, such maps are used to plan service provision. In the case of the WHO, it may be where to send their expertise and resources; or at a more local level it may be where to build a new hospital.
Bizarrely, despite GIS technologies being freely available on the internet, the Canadian outbreak of severe acute respiratory syndrome (SARS) in Canada in 2003 was managed by paper charts and color-coded post-it notes. It is one thing for a developing country, such as India, to state that "without computers and the Internet, we are fighting 21st century health problems with 19th century tools [6]," but it is quite another for Toronto's Chief Medical Officer to observe the same thing [7] in a country as developed and technology literate as Canada within the last decade!
Astonishingly, it was only nine years ago (2003) that the term 'Geographical Information Systems (GIS)' was added to Medical Subject Headings (MeSH) reflecting the growing interest in the application of cartography (mapping) functions to healthcare.
III. Uses of GIS
A GIS is a "computerized system that relates and displays data collected from a geographic entity in the form of a map. The ability of GIS to overlay existing data with new information and display it in colour on a computer screen is used primarily to conduct analyses and make decisions related to geology, ecology, land use, demographics, transportation, and other domains, most of which relate to the human use of the physical environment [8]." So GIS is a modern tool that is now readily available and usable; but what can we use it for?
1. Map Where Things Are
Their most basic use is simply to map where things are. Whether that be merely to identify an individual feature is, such as the location of an emergency room, or to look at the distribution of features on a map to more clearly visualise the emergence of patterns.
2. Map Quantities
We can map quantities, such as where the most, and least, of something is to find places that meet specified criteria and take action. For example, we could look at which jurisdiction in a country has the highest percentage of children classified as obese or overweight. However, knowing which area has the greatest problem with obesity in children is helpful but not really enough to aid us in planning services.
3. Map Densities
Therefore, we need to look at further complexities such as density mapping. By mapping density we can map areas with different populations on an equivalent basis. That is, we can map areas which may vary greatly in size but have smaller numbers of people against smaller geographic areas that have larger numbers of people to see the true density of the feature we are looking at.
Although we must be careful again to truly understand what we are mapping. For example, health care maps will almost always show concentrations of disease around major urban settings. This doesn't necessarily mean that urban settings have a causal link with that disease, but more likely that families with chronically ill members will actually move into those urban settings in order to access specialized care. Consequentially, we must be cautious when drawing conclusions from density maps unless we truly understand both the source and the validity of the data being presented.
4. Find out What's Inside
With GIS we can also look at what's happening inside a specific area; such as mapping the movement of equipment, staff and patients as they move around within a hospital to help with the tracking of infection.
5. Find What's Nearby
Likewise, we can map what's occurring within a set distance of a feature. If we see increased mortality in a specific area we can look to see what might be causing that. It could be as simple as there being a palliative care facility in the area or more disturbingly, a successor to Dr. Shipman [9-11] is practicing there.
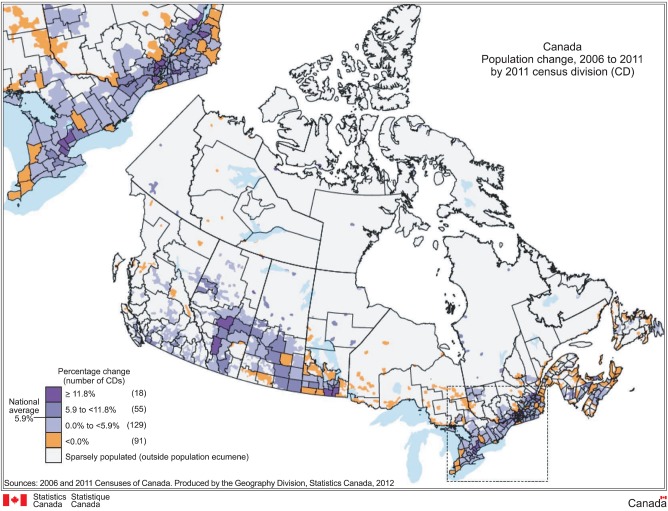
6. Map Change
We can map the change in an area (Figure 1) to anticipate future conditions, decide on a course of action, or to evaluate the results of an action or policy. For example, we can study how emergency patterns change from day to day to help decide where ambulances should be stationed.
Figure 1.
Mapping Change of Canada Population, 2006-2011.
We do have to be concerned with the validity of the data we're mapping. Sometimes what appears to be an increase in incidence of a disease over time is simply due to an increase in reporting of that disease [12].
IV. Current State of GIS Use in Health
In 1996 Clarke et al. [13] recognised that whilst GIS had been in development for over 30 years, it was only then that such systems had become readily usable for those not extensively trained in their use. Their review article 'On epidemiology and geographic information systems: a review and discussion of future directions [13]' specifically addressed the disciplinary crossover between GIS and public health and epidemiology.
They provided an overview of GIS functionality in terms of data storage, data capture, data retrieval and data display. They also identified a number of applications of GIS in health such as the surveillance and monitoring of water-borne diseases, environmental health, modeling exposure to electro-magnetic fields, predicting child pedestrian injuries and the analysis of disease policy and planning [13] as well as making the case for further use of GIS in public health. Fast forward 15 years to 2011, and the same points are still echoed in several more recent reviews [3,14,15].
1. So How is GIS Being Used in Health?
In 2003, McLafferty [14] summarized the current uses of GIS as being able to be categorized into four distinct areas: 1) analysing need for health care; 2) analysing access to health care, a) measuring access, b) evaluating inequalities in access; 3) geographic variation in utilization; and 4) GIS & health care delivery, a) locating health services, b) spatial decision support systems, and c) GIS & disasters.
She stated that at that time, GIS-based research on service performance and effectiveness was in its infancy and that whilst efforts were underway to integrate GIS with spatial decision support systems they were still in the stages of early evolution.
In 2008, Graves [15] looked specifically at the use of GIS in evaluating health care access or health outcomes. She conducted an integrative literature review in this area that presented the results from nine articles. She found that GIS had been used in a wide variety of health applications, and that GIS had been shown to be effective in relating health outcomes to the level of access to health care.
Like McLafferty before her, she identified several areas in which GIS in health was in its infancy, but felt that there was "sufficient research to support the use of GIS as an effective technology for the study of healthcare access and outcomes [Para] [15]."
In 2011, Nykiforuk and Flaman [3] continued the debate by reviewing once again GIS for health promotion and public health. They identified four predominant themes from a systematic review which was comprised of 621 journal articles and book chapters: 1) disease surveillance, a) disease mapping, b) disease modeling; 2) risk analysis; 3) health access and planning; and 4) community health profiling.
2. Disease Surveillance
Disease surveillance is an epidemiological practice that monitors the spread of disease in order to establish patterns of progression. A key component of modern disease surveillance is disease case reporting. Interestingly in these days of advanced technologies disease progression can sometimes be tracked by individuals' internet search engine usage more quickly than through traditional reporting mechanisms [16]. By tracking the location of individuals seeking information about the flu Google was able to estimate flu activity by region in the USA about two weeks later than traditional methods of Centre for Disease Control & Prevention (CDC) flu outbreak reporting.
Examples of the diseases currently been surveilled in both developed [17,18] and undeveloped countries using GIS are tropical diseases [19], parasites [20,21], rabies epidemic [22], maleria [23-27], HIV/AIDS in India [28] & South Africa [29], cancer [30,31], communicable diseases [32,33], cholera [34], and sleeping sickness [35].
3. Risk Analysis
Traditionally the use of GIS for risk analyses has been linked with environmental exposures and mitigating risks consequential to exposures. Additionally, it is often integrated with disease modeling to effectively demonstrate how humans interact with their environment and how that interaction affects their health [36].
Current examples of health GIS use in risk analysis include flood management [37], air pollution [33,38-44], soil-borne infections [45], arsenic poisoning from ground water [46], climate change [47,48], ecosystem decline [49], pesticide exposure [50,51], and other environmental exposure assessments [52,53].
My Place History [54] developed by ESRI [55], the leading developer of GIS, provides a good example of how environmental exposures during your lifetime increases your risks of developing different diseases over time. The instigator of My Place History, Bill Davenhall [54] experienced a "personal health train wreck" and consequently ESRI developed a GIS tool allowing individuals in the USA to examine the environmental factors that may contribute to their disease.
4. Health Access and Planning
GIS use in health access and planning usually relates directly to analyzing market segmentation and network analysis. That is, developing an understanding of the physical location of health services and the distance and ability to travel between them. This is an area where GIS has been used extensively in both developed developing countries.
Health GIS is also being used in projects depicting key indicators of drug policy development over time [56], general access & quality of services studies [57,58], developing a model for determining the appropriate means of trauma transport [59], understanding the relationship that proximity to primary care clinics has on health outcomes in an urban setting [60], nursing workforce distribution planning [61], travel related health [62], the provision of vision services [63], sledding injuries [64], trauma management [65], injury research [66] and modeling ambulance response times [67].
5. Community Health Profiling
The mapping of community characteristics, such as ethnic identification, socio-economic status, gender, health behaviours, mortality and morbidity, together combine to provide profiles of population groups which allows for the explanation of general relationships between health and setting.
Current examples include supporting Hispanic community transitions [68], assessing community primary care needs [69], community development [70], community pharmacy populations [71], and developing an understanding of the spiritual dimension of health for communities [72].
However, community profiling must be undertaken with great care as whilst it can help us better understand the multi-level links between people and their environment the data linkages that such profiles are developed from are frequently not as valid as would be desired.
To extend our scope beyond that of GIS use in public health and epidemiology we can identify two additional areas in which GIS is being used in health. The first is a refinement of community profiling pertaining to the built environment, neighbourhoods and their impact on health.
6. Built Environment & Neighbourhoods
A neighbourhood [73] is a geographically localized community within a larger city, town or suburb. Consequently, measures such as walkability [74-76], needs for school transport [77], the food environment [78], opportunities for physical activity [79], environmental barriers [80] and alcohol use related to where alcohol is available for purchase [81] may be different in neighbourhoods that have the same built environment; where the built environment is the surroundings that have been made by humans. The second is an extension to disease surveillance: crisis management.
7. Crisis Management
While not used extensively in this area yet health GIS is being used in combination with a sensor web, citizen sensing and social web technologies to monitor public and environmental crises [82]. It is also being used to manage and plan for disasters & humanitarian emergencies [83,84].
V. Barriers to GIS Use in Health
The one consistent message throughout all the published work to date on health GIS is that the potential for benefit is vast but that several barriers still remain to pervasive use. Clarke et al. [13] suggestion in 1996 that GIS was being seen as a new "widget" yet to come into play was continued by McLafferty [14] in 2003 when she stated that researchers tended to view GIS as a mapping tool and didn't fully understand the potential applications.
Further, McLafferty [14] argued that adoption of GIS in health was uneven due to structural barriers such as the lack of available spatial data and privacy & confidentiality restrictions that limit access to data about health status and outcomes, especially at an individual level or for small areas. She further stated that public data, even when it was available, often couldn't be linked due to differences in the structure and level of granularity [14].
Additionally, due to the known limitations of indicators such as mortality and morbidity, over the years researchers have turned more to qualitative methods and blended methods to help develop our understanding of health care access, use and provision. Unfortunately, GIS wasn't able to fully integrate that data for analysis, beyond simply placing it at a discrete geographic location as of 2003. In fact, it still remains an issue today in 2012.
McLafferty [14] further recognized that there was a distinct lack of knowledge around how people acquire knowledge from a GIS and interpret it for their own use and decision making. In the same time period as McLafferty, Higgs and colleagues studied the use of GIS in the English National Health Service (NHS) [85,86] and reported that little use was found, especially in service planning, and that national guidance was needed for departments to be able to actively utilize the tools available.
VI. Conclusion
Having identified the barriers to the use of GIS in health a number of authors have made recommendations as to how we should best develop the use of GIS in health. These can be summarized as follows:
Integrate instruction on GIS into public health curricula [13]
Develop formal links between the interdisciplinary research communities working with GIS in health [3,13]
Seize the opportunity to set the public health agenda and influence the use of such technologies to improve public health [13,87,88]
Link information by place/location across sectors such as health, education, social services, and the justice system that together provide care [14,89]
Develop analytic techniques that take account of qualitative data in GIS [14]
Develop our understanding of the human dimension of using GIS in health [14]
Undertake studies that provide a greater understanding of patterns of geography, health care access and provision of services [15]
Develop further understanding of the relationship between specific populations and their unique geographical contexts [15]
Communicate with, and involve, stakeholders in the development and display of knowledge in mapped formats [3].
Despite the exponential growth in the evidence for the use of GIS in health it remains a discipline slow to grow and mature. In contrast the use of GIS in other domains, such as business, marketing, environmental assessments, and education, is now considered to be an inherent component.
The barriers to the discipline of health GIS developing further are not to be underestimated. Take for example, a study designed to examine childhood obesity. At the heart of the study is the need to explore the relationships between where children live, study and play. One would need to look at walkability factors, distances between appropriate and inappropriate food sources, play areas, parks and exercise facilities, schools, homes and their families' work places. Right there, unless we collect primary data from individuals with consent we're stymied. Location is personally identifiable information so under all privacy legislation, despite the fact that the child's address and registered school is held in a variety of databases (education, health or otherwise), it can't be accessed or used by those wishing to undertake this work; even though the information could be readily anonymised once the first step in the analysis was completed. This demonstrates the importance of the recommendations above.
Only when communities of researchers work in partnership with each other and with stakeholders will such issues be addressed, and only then can new methodologies be developed that protect the identity of the individual while allowing for such relationships to be explored.
Cost and ease of use are no longer barriers. There are free online tools such as GRASS, uDig GIS, TNTLite, SPRING, Flowmap, and Diva-GIS. ESRI [55] makes key components of their software available free and there are millions of maps available freely online that can be downloaded and worked with for personal use. Likewise these tools and systems are becoming easier to use daily. The issue is not in using the tools but in understanding what they represent when knowledge is presented in this way. Google maps have opened the eyes of the public to the potential of mapping and spatial-temporal analytics. It is time for the health community to work together to unleash the potential of GIS for the benefit of all.
In conclusion, health GIS remains underutilized 15 years after it was first identified as having immense potential benefits and having matured enough as a technology that researchers could use readily and easily. If, as healthcare informatics researchers, we are truly concerned with improving the health of our communities, this is a tool we should no longer be ignoring.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Cooper MM. The Dartmouth Atlas of Health Care: what is it telling us? Health Syst Rev. 1996;29:44–45. 47. [PubMed] [Google Scholar]
- 2.Joyce K. "To me it's just another tool to help understand the evidence": public health decision-makers' perceptions of the value of geographical information systems (GIS) Health Place. 2009;15:801–810. doi: 10.1016/j.healthplace.2009.01.004. [DOI] [PubMed] [Google Scholar]
- 3.Nykiforuk CI, Flaman LM. Geographic information systems (GIS) for health promotion and public health: a review. Health Promot Pract. 2011;12:63–73. doi: 10.1177/1524839909334624. [DOI] [PubMed] [Google Scholar]
- 4.Boulos MN. Towards evidence-based, GIS-driven national spatial health information infrastructure and surveillance services in the United Kingdom. Int J Health Geogr. 2004;3:1. doi: 10.1186/1476-072X-3-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Snow J. On the mode of communication of cholera. London, UK: John Churchill; 1849. [Google Scholar]
- 6.World Health Organization. The world health report 2003: shaping the future. Geneva, Switzerland: World Health Organization; 2003. [Google Scholar]
- 7.Menezes JP. Going public [Internet] Scarborough, Canada: IT World Canada; 2004. [cited at 2012 Jun 11]. Available from: http://www.itworldcanada.com/news/going-public/116928-pg3. [Google Scholar]
- 8.DeMers MN. GIS [Internet] London, UK: Encyclopaedia Britannica; c2012. [cited at 2012 Jun 11]. Available from: http://www.britannica.com/EBchecked/topic/1033394/GIS. [Google Scholar]
- 9.Kaplan R. Murder by medical malice: the love-hate relationship between Dr Harold Shipman and his patients. S Afr Med J. 2000;90:598–601. [PubMed] [Google Scholar]
- 10.Baker R. Implications of Harold Shipman for general practice. Postgrad Med J. 2004;80:303–306. doi: 10.1136/pgmj.2003.013110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Baker R, Hurwitz B. Intentionally harmful violations and patient safety: the example of Harold Shipman. J R Soc Med. 2009;102:223–227. doi: 10.1258/jrsm.2009.09k028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shaw NT. Electronic patient records in primary care: study has serious flaw. BMJ. 2003;327:622. doi: 10.1136/bmj.327.7415.622-b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Clarke KC, McLafferty SL, Tempalski BJ. On epidemiology and geographic information systems: a review and discussion of future directions. Emerg Infect Dis. 1996;2:85–92. doi: 10.3201/eid0202.960202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McLafferty SL. GIS and health care. Annu Rev Public Health. 2003;24:25–42. doi: 10.1146/annurev.publhealth.24.012902.141012. [DOI] [PubMed] [Google Scholar]
- 15.Graves BA. Integrative literature review: a review of literature related to geographical information systems, healthcare access, and health outcomes. Perspect Health Inf Manag. 2008;5:11. [PMC free article] [PubMed] [Google Scholar]
- 16.Dugas AF, Hsieh YH, Levin SR, Pines JM, Mareiniss DP, Mohareb A, Gaydos CA, Perl TM, Rothman RE. Google Flu Trends: correlation with emergency department influenza rates and crowding metrics. Clin Infect Dis. 2012;54:463–469. doi: 10.1093/cid/cir883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Duncombe J, Clements A, Hu W, Weinstein P, Ritchie S, Espino FE. Geographical information systems for dengue surveillance. Am J Trop Med Hyg. 2012;86:753–755. doi: 10.4269/ajtmh.2012.11-0650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Horst MA, Coco AS. Observing the spread of common illnesses through a community: using geographic information systems (GIS) for surveillance. J Am Board Fam Med. 2010;23:32–41. doi: 10.3122/jabfm.2010.01.090137. [DOI] [PubMed] [Google Scholar]
- 19.Khan OA, Davenhall W, Ali M, Castillo-Salgado C, Vazquez-Prokopec G, Kitron U, Soares Magalhaes RJ, Clements AC. Geographical information systems and tropical medicine. Ann Trop Med Parasitol. 2010;104:303–318. doi: 10.1179/136485910X12743554759867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Simoonga C, Utzinger J, Brooker S, Vounatsou P, Appleton CC, Stensgaard AS, Olsen A, Kristensen TK. Remote sensing, geographical information system and spatial analysis for schistosomiasis epidemiology and ecology in Africa. Parasitology. 2009;136:1683–1693. doi: 10.1017/S0031182009006222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Daniel M, Kolar J, Zeman P. GIS tools for tick and tick-borne disease occurrence. Parasitology. 2004;129(Suppl):S329–S352. doi: 10.1017/s0031182004006080. [DOI] [PubMed] [Google Scholar]
- 22.Mungrue K, Mahabir R. The rabies epidemic in Trinidad of 1923 to 1937: an evaluation with a geographic information system. Wilderness Environ Med. 2011;22:28–36. doi: 10.1016/j.wem.2010.11.001. [DOI] [PubMed] [Google Scholar]
- 23.Kelly GC, Hii J, Batarii W, Donald W, Hale E, Nausien J, Pontifex S, Vallely A, Tanner M, Clements A. Modern geographical reconnaissance of target populations in malaria elimination zones. Malar J. 2010;9:289. doi: 10.1186/1475-2875-9-289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sipe NG, Dale P. Challenges in using geographic information systems (GIS) to understand and control malaria in Indonesia. Malar J. 2003;2:36. doi: 10.1186/1475-2875-2-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Singer BH, de Castro MC. Agricultural colonization and malaria on the Amazon frontier. Ann N Y Acad Sci. 2001;954:184–222. doi: 10.1111/j.1749-6632.2001.tb02753.x. [DOI] [PubMed] [Google Scholar]
- 26.Ghebreyesus TA, Witten KH, Getachew A, O'Neill K, Bosman A, Teklehaimanot A. Community-based malaria control in Tigray, northern Ethiopia. Parassitologia. 1999;41:367–371. [PubMed] [Google Scholar]
- 27.Najera JA. Prevention and control of malaria epidemics. Parassitologia. 1999;41:339–347. [PubMed] [Google Scholar]
- 28.Kandwal R, Garg PK, Garg RD. Health GIS and HIV/AIDS studies: perspective and retrospective. J Biomed Inform. 2009;42:748–755. doi: 10.1016/j.jbi.2009.04.008. [DOI] [PubMed] [Google Scholar]
- 29.Vanmeulebrouk B, Rivett U, Ricketts A, Loudon M. Open source GIS for HIV/AIDS management. Int J Health Geogr. 2008;7:53. doi: 10.1186/1476-072X-7-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Aneja S, Gross CP, Soulos PR, Yu JB. Geographical information systems: applications and limitations in oncology research. Oncology (Williston Park) 2011;25:1221–1225. [PubMed] [Google Scholar]
- 31.Bell BS, Hoskins RE, Pickle LW, Wartenberg D. Current practices in spatial analysis of cancer data: mapping health statistics to inform policymakers and the public. Int J Health Geogr. 2006;5:49. doi: 10.1186/1476-072X-5-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Flahault A, Blanchon T, Dorléans Y, Toubiana L, Vibert JF, Valleron AJ. Virtual surveillance of communicable diseases: a 20-year experience in France. Stat Methods Med Res. 2006;15:413–421. doi: 10.1177/0962280206071639. [DOI] [PubMed] [Google Scholar]
- 33.Rogers DJ, Randolph SE. Studying the global distribution of infectious diseases using GIS and RS. Nat Rev Microbiol. 2003;1:231–237. doi: 10.1038/nrmicro776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Nyamogoba HD, Obala AA, Kakai R. Combating cholera epidemics by targeting reservoirs of infection and transmission routes: a review. East Afr Med J. 2002;79:150–155. doi: 10.4314/eamj.v79i3.8896. [DOI] [PubMed] [Google Scholar]
- 35.Cattand P, Jannin J, Lucas P. Sleeping sickness surveillance: an essential step towards elimination. Trop Med Int Health. 2001;6:348–361. doi: 10.1046/j.1365-3156.2001.00669.x. [DOI] [PubMed] [Google Scholar]
- 36.Tatem AJ, Adamo S, Bharti N, Burgert CR, Castro M, Dorelien A, Fink G, Linard C, Mendelsohn J, Montana L, Montgomery MR, Nelson A, Noor AM, Pindolia D, Yetman G, Balk D. Mapping populations at risk: improving spatial demographic data for infectious disease modeling and metric derivation. Popul Health Metr. 2012;10:8. doi: 10.1186/1478-7954-10-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Taylor J, Lai KM, Davies M, Clifton D, Ridley I, Biddulph P. Flood management: prediction of microbial contamination in large-scale floods in urban environments. Environ Int. 2011;37:1019–1029. doi: 10.1016/j.envint.2011.03.015. [DOI] [PubMed] [Google Scholar]
- 38.Levy JI, Clougherty JE, Baxter LK, Houseman EA, Paciorek CJ HEI Health Review Committee. Evaluating heterogeneity in indoor and outdoor air pollution using land-use regression and constrained factor analysis. Res Rep Health Eff Inst. 2010;(152):5–80. [PubMed] [Google Scholar]
- 39.Zou B, Wilson JG, Zhan FB, Zeng Y. Air pollution exposure assessment methods utilized in epidemiological studies. J Environ Monit. 2009;11:475–490. doi: 10.1039/b813889c. [DOI] [PubMed] [Google Scholar]
- 40.Zhou Y, Levy JI. Factors influencing the spatial extent of mobile source air pollution impacts: a meta-analysis. BMC Public Health. 2007;7:89. doi: 10.1186/1471-2458-7-89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mindell J, Barrowcliffe R. Linking environmental effects to health impacts: a computer modelling approach for air pollution. J Epidemiol Community Health. 2005;59:1092–1098. doi: 10.1136/jech.2005.036897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Scoggins A. Does air pollution pose a public health problem for New Zealand? Aust N Z J Public Health. 2004;28:16–19. doi: 10.1111/j.1467-842x.2004.tb00626.x. [DOI] [PubMed] [Google Scholar]
- 43.Bytnerowicz A, Badea O, Barbu I, Fleischer P, Fraczek W, Gancz V, Godzik B, Grodzinska K, Grodzki W, Karnosky D, Koren M, Krywult M, Krzan Z, Longauer R, Mankovska B, Manning WJ, McManus M, Musselman RC, Novotny J, Popescu F, Postelnicu D, Prus-Głowacki W, Skawinski P, Skiba S, Szaro R, Tamas S, Vasile C. New international long-term ecological research on air pollution effects on the Carpathian Mountain forests, Central Europe. Environ Int. 2003;29:367–376. doi: 10.1016/S0160-4120(02)00172-1. [DOI] [PubMed] [Google Scholar]
- 44.Dent AL, Fowler DA, Kaplan BM, Zarus GM, Henriques WD. Using GIS to study the health impact of air emissions. Drug Chem Toxicol. 2000;23:161–178. doi: 10.1081/dct-100100109. [DOI] [PubMed] [Google Scholar]
- 45.Jex AR, Lim YA, Bethony JM, Hotez PJ, Young ND, Gasser RB. Soil-transmitted helminths of humans in Southeast Asia - towards integrated control. Adv Parasitol. 2011;74:231–265. doi: 10.1016/B978-0-12-385897-9.00004-5. [DOI] [PubMed] [Google Scholar]
- 46.Khan NI, Owens G, Bruce D, Naidu R. Human arsenic exposure and risk assessment at the landscape level: a review. Environ Geochem Health. 2009;31(Suppl 1):143–166. doi: 10.1007/s10653-008-9240-3. [DOI] [PubMed] [Google Scholar]
- 47.Luber G, McGeehin M. Climate change and extreme heat events. Am J Prev Med. 2008;35:429–435. doi: 10.1016/j.amepre.2008.08.021. [DOI] [PubMed] [Google Scholar]
- 48.Maynard NG, Conway GA. A view from above: use of satellite imagery to enhance our understanding of potential impacts of climate change on human health in the Arctic. Alaska Med. 2007;49:38–43. [PubMed] [Google Scholar]
- 49.Twumasi YA, Merem EC. Using remote sensing and GIS in the analysis of ecosystem decline along the River Niger Basin: the case of Mali and Niger. Int J Environ Res Public Health. 2007;4:173–184. doi: 10.3390/ijerph2007040013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Fenske RA. State-of-the-art measurement of agricultural pesticide exposures. Scand J Work Environ Health. 2005;31(Suppl 1):67–73. [PubMed] [Google Scholar]
- 51.Kamińska IA, Ołdak A, Turski WA. Geographical information system (GIS) as a tool for monitoring and analysing pesticide pollution and its impact on public health. Ann Agric Environ Med. 2004;11:181–184. [PubMed] [Google Scholar]
- 52.Nuckols JR, Ward MH, Jarup L. Using geographic information systems for exposure assessment in environmental epidemiology studies. Environ Health Perspect. 2004;112:1007–1015. doi: 10.1289/ehp.6738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Jarup L. Health and environment information systems for exposure and disease mapping, and risk assessment. Environ Health Perspect. 2004;112:995–997. doi: 10.1289/ehp.6736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Davenhall B. Can geographic information make you healthy? Redlands, CA: ESRI; c2012. [cited at 2012 Jun 11]. Available from: http://www.esri.com/industries/health/geomedicine/index.html. [Google Scholar]
- 55.ESRI [Internet] Redlands, CA: ESRI; c2012. [cited at 2012 Jun 11]. Available from: http://www.esri.com/ [Google Scholar]
- 56.Macgregor S, Thickett A. Partnerships and communities in English drug policy: the challenge of deprivation. Int J Drug Policy. 2011;22:478–490. doi: 10.1016/j.drugpo.2011.06.003. [DOI] [PubMed] [Google Scholar]
- 57.Clark RA, Driscoll A. Access and quality of heart failure management programs in Australia. Aust Crit Care. 2009;22:111–116. doi: 10.1016/j.aucc.2009.06.003. [DOI] [PubMed] [Google Scholar]
- 58.Parker EB, Campbell JL. Measuring access to primary medical care: some examples of the use of geographical information systems. Health Place. 1998;4:183–193. doi: 10.1016/s1353-8292(98)00010-0. [DOI] [PubMed] [Google Scholar]
- 59.Lerner EB, Billittier AJ, 4th, Sikora J, Moscati RM. Use of a geographic information system to determine appropriate means of trauma patient transport. Acad Emerg Med. 1999;6:1127–1133. doi: 10.1111/j.1553-2712.1999.tb00115.x. [DOI] [PubMed] [Google Scholar]
- 60.Baumgardner DJ, Halsmer SE, Steber DL, Shah DS, Mundt MP. Does proximity to clinic affect immunization rates and blood pressure. Int J Psychiatry Med. 2006;36:199–209. doi: 10.2190/9N36-W446-194L-9KHW. [DOI] [PubMed] [Google Scholar]
- 61.Courtney KL. Visualizing nursing workforce distribution: policy evaluation using geographic information systems. Int J Med Inform. 2005;74:980–988. doi: 10.1016/j.ijmedinf.2005.07.012. [DOI] [PubMed] [Google Scholar]
- 62.Bauer IL, Puotinen M. Geographic information systems and travel health. J Travel Med. 2002;9:308–314. doi: 10.2310/7060.2002.30170. [DOI] [PubMed] [Google Scholar]
- 63.Culham LE, Ryan B, Jackson AJ, Hill AR, Jones B, Miles C, Young JA, Bunce C, Bird AC. Low vision services for vision rehabilitation in the United Kingdom. Br J Ophthalmol. 2002;86:743–747. doi: 10.1136/bjo.86.7.743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Juang D, Feliz A, Miller KA, Gaines BA. Sledding injuries: a rationale for helmet usage. J Trauma. 2010;69:S206–S208. doi: 10.1097/TA.0b013e3181f1e81f. [DOI] [PubMed] [Google Scholar]
- 65.Schuurman N, Hameed SM, Fiedler R, Bell N, Simons RK. The spatial epidemiology of trauma: the potential of geographic information science to organize data and reveal patterns of injury and services. Can J Surg. 2008;51:389–395. [PMC free article] [PubMed] [Google Scholar]
- 66.Edelman LS. Using geographic information systems in injury research. J Nurs Scholarsh. 2007;39:306–311. doi: 10.1111/j.1547-5069.2007.00185.x. [DOI] [PubMed] [Google Scholar]
- 67.Peleg K, Pliskin JS. A geographic information system simulation model of EMS: reducing ambulance response time. Am J Emerg Med. 2004;22:164–170. doi: 10.1016/j.ajem.2004.02.003. [DOI] [PubMed] [Google Scholar]
- 68.Dulin MF, Ludden TM, Tapp H, Smith HA, de Hernandez BU, Blackwell J, Furuseth OJ. Geographic information systems (GIS) demonstrating primary care needs for a transitioning hispanic community. J Am Board Fam Med. 2010;23:109–120. doi: 10.3122/jabfm.2010.01.090136. [DOI] [PubMed] [Google Scholar]
- 69.Dulin MF, Ludden TM, Tapp H, Blackwell J, de Hernandez BU, Smith HA, Furuseth OJ. Using Geographic information systems (GIS) to understand a community's primary care needs. J Am Board Fam Med. 2010;23:13–21. doi: 10.3122/jabfm.2010.01.090135. [DOI] [PubMed] [Google Scholar]
- 70.Quon Huber MS, Van Egeren LA, Pierce SJ, Foster-Fishman PG. GIS applications for community-based research and action: mapping change in a community-building initiative. J Prev Interv Community. 2009;37:5–20. doi: 10.1080/10852350802498367. [DOI] [PubMed] [Google Scholar]
- 71.Ryan K, Norris P, Becket G. Capturing data on medicines usage: the potential of community pharmacy databases. N Z Med J. 2005;118:U1677. [PubMed] [Google Scholar]
- 72.Boulos MN. Geographic information systems and the spiritual dimension of health: a short position paper. Int J Health Geogr. 2003;2:6. doi: 10.1186/1476-072X-2-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Cutchin MP, Eschbach K, Mair CA, Ju H, Goodwin JS. The socio-spatial neighborhood estimation method: an approach to operationalizing the neighborhood concept. Health Place. 2011;17:1113–1121. doi: 10.1016/j.healthplace.2011.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Gray JA, Zimmerman JL, Rimmer JH. Built environment instruments for walkability, bikeability, and recreation: disability and universal design relevant? Disabil Health J. 2012;5:87–101. doi: 10.1016/j.dhjo.2011.12.002. [DOI] [PubMed] [Google Scholar]
- 75.Butler EN, Ambs AM, Reedy J, Bowles HR. Identifying GIS measures of the physical activity built environment through a review of the literature. J Phys Act Health. 2011;8(Suppl 1):S91–S97. doi: 10.1123/jpah.8.s1.s91. [DOI] [PubMed] [Google Scholar]
- 76.Brownson RC, Hoehner CM, Day K, Forsyth A, Sallis JF. Measuring the built environment for physical activity: state of the science. Am J Prev Med. 2009;36:S99–S123. doi: 10.1016/j.amepre.2009.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Wong BY, Faulkner G, Buliung R. GIS measured environmental correlates of active school transport: a systematic review of 14 studies. Int J Behav Nutr Phys Act. 2011;8:39. doi: 10.1186/1479-5868-8-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Charreire H, Casey R, Salze P, Simon C, Chaix B, Banos A, Badariotti D, Weber C, Oppert JM. Measuring the food environment using geographical information systems: a methodological review. Public Health Nutr. 2010;13:1773–1785. doi: 10.1017/S1368980010000753. [DOI] [PubMed] [Google Scholar]
- 79.Duncan MJ, Badland HM, Mummery WK. Applying GPS to enhance understanding of transport-related physical activity. J Sci Med Sport. 2009;12:549–556. doi: 10.1016/j.jsams.2008.10.010. [DOI] [PubMed] [Google Scholar]
- 80.Hammel J, Jones R, Smith J, Sanford J, Bodine C, Johnson M. Environmental barriers and supports to the health, function, and participation of people with developmental and intellectual disabilities: report from the State of the Science in Aging with Developmental Disabilities Conference. Disabil Health J. 2008;1:143–149. doi: 10.1016/j.dhjo.2008.05.001. [DOI] [PubMed] [Google Scholar]
- 81.Wieczorek WF, Hanson CE. New modeling methods: geographic information systems and spatial analysis. Alcohol Health Res World. 1997;21:331–339. [PMC free article] [PubMed] [Google Scholar]
- 82.Kamel Boulos MN, Resch B, Crowley DN, Breslin JG, Sohn G, Burtner R, Pike WA, Jezierski E, Chuang KY. Crowdsourcing, citizen sensing and sensor web technologies for public and environmental health surveillance and crisis management: trends, OGC standards and application examples. Int J Health Geogr. 2011;10:67. doi: 10.1186/1476-072X-10-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Mathew D. Information technology and public health management of disasters - a model for South Asian countries. Prehosp Disaster Med. 2005;20:54–60. doi: 10.1017/s1049023x00002156. [DOI] [PubMed] [Google Scholar]
- 84.Kaiser R, Spiegel PB, Henderson AK, Gerber ML. The application of geographic information systems and global positioning systems in humanitarian emergencies: lessons learned, programme implications and future research. Disasters. 2003;27:127–140. doi: 10.1111/1467-7717.00224. [DOI] [PubMed] [Google Scholar]
- 85.Higgs G, Smith DP, Gould MI. Findings from a survey on GIS use in the UK National Health Service: organisational challenges and opportunities. Health Policy. 2005;72:105–117. doi: 10.1016/j.healthpol.2004.06.011. [DOI] [PubMed] [Google Scholar]
- 86.Higgs G, Gould M. Is there a role for GIS in the 'new NHS'? Health Place. 2001;7:247–259. doi: 10.1016/s1353-8292(01)00014-4. [DOI] [PubMed] [Google Scholar]
- 87.Croner CM. Public health, GIS, and the internet. Annu Rev Public Health. 2003;24:57–82. doi: 10.1146/annurev.publhealth.24.012902.140835. [DOI] [PubMed] [Google Scholar]
- 88.Rushton G. Public health, GIS, and spatial analytic tools. Annu Rev Public Health. 2003;24:43–56. doi: 10.1146/annurev.publhealth.24.012902.140843. [DOI] [PubMed] [Google Scholar]
- 89.Cromley EK. GIS and disease. Annu Rev Public Health. 2003;24:7–24. doi: 10.1146/annurev.publhealth.24.012902.141019. [DOI] [PubMed] [Google Scholar]