Abstract
Little is known about whether early symptom presentation differs in toddlers with ASD from ethnic minority versus non-minority backgrounds. Within a treatment study for toddlers with ASD, we compared 19 minority to 65 Caucasian children and their parents on variables obtained from the Mullen Scales of Early Learning, Autism Diagnostic Observation Schedule, and Communication and Symbolic Behavior Scales Caregiver Questionnaire. The majority of parents were from the upper classes irrespective of ethnic membership. Minority children had lower language and communication scores than non-minority children. Findings indicate that subtle communication delays may be undetected or presumed unremarkable by parents of minority toddlers, and that more significant delays are needed to prompt the search for intervention services.
Keywords: autism spectrum disorder, toddlers, early symptoms, minority
Autism spectrum disorders (ASD) are a set of neurodevelopmental disorders marked by impairments in social interaction, communication, and repetitive and stereotypical behavior, with onset of developmental disruption before age three (DSM IV-TR, APA, 2000). ASD affects 1 in 110 children in the United States (CDC, 2010), and there is no medical cure. Yet developmental and behavioral interventions have been shown to improve communication, social, play, and behavioral functioning in children ASD. Although early detection of ASD is possible as early as 14 months of age (Landa, Holman, & Garrett-Mayer, 2007) and is crucial for accessing early intervention services, diagnosis often occurs after the third birthday (Mandell, Novak, & Zubritsky, 2005). Particularly troublesome is the more considerable delay in diagnosis of ASD in children from minority groups relative to children from non-minority groups (Mandell, Listerud, Levy, & Pinto-Martin, 2002; Mandell et al., 2005).
While the prevalence of ASD does not differ across racial and ethnic groups (Fombonne, 2003), a limited number of studies have shown that children of African American, Hispanic, and Asian descent are less likely to receive early diagnosis of autism than Caucasian children (Mandell et al., 2002; Mandell et al., 2009; CDC, 2006). In addition, when minority children eventually diagnosed with ASD see health-care professionals, they are more likely to receive a diagnosis other than autism. For example, Mandell et al. (2007) reported that African-American children with ASD were usually diagnosed with ADHD, conduct disorder, or adjustment disorder on their first specialty health-care visit. In another study, Begeer, Bouk, Boussaid, Terwogt, & Koot (2009) examined why non-European minorities in the Netherlands were proportionally underrepresented in institutions specialized in the diagnosis of autism. The investigators reported that medical professionals were more likely to classify a case as autism when judging clinical vignettes of European children with ASD than vignettes of non-European minorities.
The reasons for disparities in age of diagnosis for minority and non-minority children with ASD are numerous and may include factors related to financial and educational resources, and cultural and language barriers. Poverty rates are usually higher among minorities (Gradin, 2008), which can limit their access to information, education, and quality health care. Many studies have reported a positive association between socio-economic status and prevalence rates of autism (Durkin et al., 2010; Fountain, King, & Bearman, 2010; Liptak, Benzoni, Mruzek, Nolan, Thingvoll, Wade, & Fryer, 2008; Schopler, Andrews, & Strupp, 1979); however, this association is usually explained by an ascertainment bias. For example, Durkin et al. (2010) surveyed data of 3680 8-year-old children with a pre-existing diagnosis of ASD or whose symptoms were consistent with a diagnosis of ASD from the Autism and Developmental Disabilities Monitoring Network. They found a positive relationship between SES and the prevalence rates of autism especially among children with a pre-existing diagnosis of autism. Similarly, Fountain et al. (2010) have shown that children whose parents are highly educated are usually diagnosed at a younger age; and this might be because parents with higher education and SES are more likely to seek out facilities that practice state-of-the-art health-care, and have a higher level of health literacy regarding the early signs of atypical child development.
Cultural barriers, on the other hand, may have more indirect influences by affecting the way people think and behave and interact with others. Minority groups have cultural practices, value systems, and expectations that usually differ from the dominant culture. For example, families from diverse ethnic and cultural backgrounds are likely to differ in their perceptions of their children's developmental milestones. This becomes relevant for early detection of ASD when early-developing social abilities fail to emerge in typical fashion, such as affect sharing and joint attention, and should raise red flags of concern for ASD. One example of this has been provided by the finding that Puerto Rican mothers expected their typically developing children to attain social milestones, such as recognizing the mother and smiling at faces, at a later age compared to Caucasian mothers (Pachter & Dworkin, 1997). Similarly, the use of index finger pointing as a communicative bid to share interest is not a common practice in some Asian cultures, and may not be considered an important acquisition in children's social development in these cultures (Zang, Wheeler, & Richey, 2006). The standard early indicators of ASD in mainstream American culture may not elicit concern at an early age in some minority cultures. Thus, different cultural practices and beliefs about child development may indirectly affect the age of ASD detection and access to services among minority groups.
Cultural practices and value systems of ethnic minorities may also affect communication with health care providers in ways that deter diagnostic decision making. It is possible that some minority parents engage in less interactional communication with health-care providers, and, hence, may be at a disadvantage to receive an informed diagnosis for their children. For example cultures that place a priority on respect for authority, as in Asian and Hispanic cultures, may engage in less bi-directional, interactive communication with health care providers (Rodgers-Adkinson, Ochoa, & Delgado, 2003). Similarly, Post, Cegala, and Marinelli (2001) compared African-American and Caucasian patients who participated in a training program to improve patient-physician communication as they interacted with their primary care physicians. African-American patients addressed fewer medically-related questions to their physicians, and provided and obtained less information on their condition.
To better understand whether minority groups differ from non-minorities in the nature and timing of interactions with professionals related to diagnosis of developmental disruptions associated with ASD, a study is needed that examines child characteristics as close in time to the actual ASD diagnosis as possible. This approach would permit comparison of very early ASD symptoms and other developmental features between minority and non-minority children. To our knowledge, the only study that has investigated group differences in the symptamotology of autism is Cuccaro et al.'s (2007) study of the phenotypic differences in clinical features between African-American and Caucasian individuals with autism. Using the Autism Diagnostic Interview-Revised (ADI-R), Cuccaro et al. (2007) interviewed parents/caregivers of individuals with ASD who were between 3 and 21 years of age, and reported that African-Americans showed greater impairments in language but did not differ from Caucasians on core autism features.
The current study is the first research examination of ethnic differences in the presentation of autism symptoms in toddlers with ASD as contemporaneously reported by their parents and clinicians. Using pre-treatment data from participants in an ongoing early intervention study, we compared minority and non-minority (i.e., Caucasian white) children with a diagnosis of ASD on standardized tests measuring receptive and expressive language, cognitive, social, and motor skills. We hypothesized that minority and non-minority children would differ in developmental profiles, particularly in language functioning, given the literature reviewed above.
Method
Participants
Eighty four toddlers with ASD and their parents participated in this study. Parents of 19 toddlers identified themselves as being of ethnic minority descent (children's mean age = 26.78 months); parents of 65 toddlers identified themselves as being Caucasian (children's mean age = 27.69 months, see Table 1). The minority group included 11 African-American children, 7 Asian children, and 1 Hispanic child and their primary caregivers. Participants included 14 girls (minority = 2, non-minority = 12) and 70 boys. Children were diagnosed with ASD by expert clinical researchers and met algorithm criteria for ASD or autism on the Autism Diagnostic Observation Schedule-Generic (Lord, Rutter, DiLavore, & Rissi, 1999). The parents of the children were self-referred or were referred by their physician or early intervention assessment teams to the early intervention study. All provided consent to participate in this IRB-approved study.
Table 1.
Descriptive statistics for minority and non-minority groups.
| Minority | Non-Minority | |
|---|---|---|
| N | 19 | 65 |
| Mean (SD) / Range | Mean (SD) / Range | |
| Age in months | 26.79 (3.73) / 20-33 | 27.69 (4.39) / 16-38 |
| Maternal educationa | 6.05 (1.13) / 4-7 | 6.02 (.91) / 4-7 |
| Paternal educationa | 6.06 (.99) / 4-7 | 5.94 (1.03) / 4-7 |
| SES/Five classes | ||
| Percentage | Percentage | |
| Lower | 5.55% | 0% |
| Lower-middle | 11.11% | 5.00% |
| Middle | 11.11% | 23.33% |
| Upper-middle | 44.44% | 55.00% |
| Upper | 27.77% | 16.66% |
Represents education categories: 7=Graduate degree, 6=college degree, 5=1-3 years of college, 4=high school degree, 3=10-11 years of school, 2=7-9 years of school, 1=less than 7 years of school.
Measures
The Communication and Symbolic Behavior Scales Developmental Profile Caregiver Questionnaire (CSBS-DP CQ; Wetherby & Prizant, 2002) is a parent-completed questionnaire normed for children between 6 and 24 months of age, and provides information on children's language and social development. Raw scores on the following scales were used for analyses: CSBS-DP CQ-Words, which measures expressive vocabulary and includes a brief checklists of words for basic objects, people, and body parts (e.g., dog, book, ball, mommy, daddy, eye, nose); CSBS-DP CQ-Understanding Words, which measures language comprehension and includes a brief checklist of words for basic objects, people, and body parts; and CSBS-DP CQ-Social Composite, which includes items that measure eye contact, joint attention, and use of gestures.
The Mullen Scales of Early Learning (Mullen, 1995) is a comprehensive assessment of development normed for ages birth to 5 years, 8 months that includes the following scales: Visual Reception, Expressive and Receptive Language, and Fine and Gross Motor. The Mullen yields both standard T scores and age equivalents for each scale. Age-equivalent scores were used for analyses, since the majority of the participants had floor effects on the T scores for some Mullen scales.
The Autism Diagnostic Observation Schedule-Generic (ADOS; Lord et al., 1999) is a gold-standard play-based assessment for ASD with standardized administration and scoring schema. No age norms are provided. Children's behavior is sampled through the use of systematic probes for autism symptoms in social interaction, communication, play, and stereotyped behaviors and repetitive interests. Algorithm criteria for ASD and autism classification, based on Communication and Reciprocal Social Interaction summary scores, are provided. The dependent variables from the ADOS used in analyses within this paper were total scores on the algorithm Communication and Reciprocal Social Interaction domains.
Socio-economic status
In order to control for participants’ socioeconomic status (SES), Hollingshead (1975) two-factor index of social position (ISP) was calculated. Hollingshead's two-factor index of SES is the most widely used measure of social class and is based on education and occupation levels of the parents. The distribution of minority and non-minority parents across different groups of SES is presented in Table 1.
Procedure
Children were administered the ADOS and Mullen by research clinicians, and parents completed the CSBS-DP CQ prior to the child's entry into the intervention.
Analyses
First, chi-square analysis was conducted to determine whether minority children differed from non-minority children on SES. Second, we compared scores of minority and non-minority children on standardized measures using non-parametric tests. Finally, binary logistic regression was conducted to investigate the factors predicting ethnic group membership (i.e., minority vs. non-minority).
Results
The upper-middle class was the largest group for both minority and non-minority families (42.10 % and 50.76 %, respectively). A crosstab analysis between SES and ethnicity did not reveal significant group differences (p > .10). That is, the majority of parents belonged to the upper classes irrespective of ethnic membership (see Table 1).
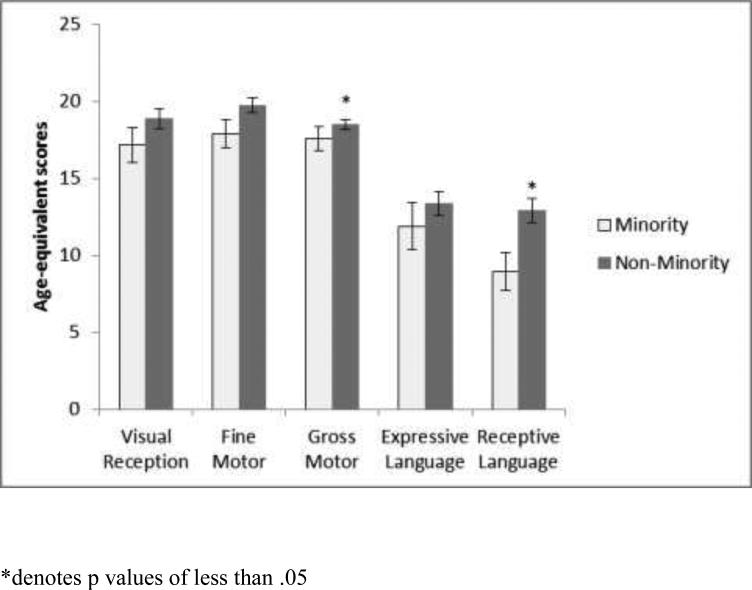
Since the data were not normally distributed, non-parametric tests were conducted to investigate the difference between minority and non-minority children and parents. The variables that were entered into the analyses include CSBS-DP CQ-Words (a measure of expressive vocabulary), CSBS-DP CQ-Understanding Words, CSBS-DP CQ-Social Composite, ADOS algorithm Communication domain score, ADOS algorithm Reciprocal Social Interaction domain score, and age equivalent scores from the Mullen Visual Reception, Receptive Language, Expressive Language, and Fine and Gross Motor scales. The toddlers in the minority group scored significantly lower than the non-minority group on the following: CSBS-DP CQ-Words (Mann-Whitney U = 207.00, p < .01); CSBS DP CQ Understanding Words (Mann-Whitney U = 185.00, p < .01); ADOS Communication (Mann-Whitney U = 831.00, p = .02); Mullen Receptive Language scale (Mann-Whitney U = 391.50, p = .02) and Mullen Gross Motor scale (Mann-Whitney U = 331.50, p = .05) (see Table 2 and Figure 1).
Table 2.
Group differences on sample characteristics and dependent measures.
| Minority | Non-Minority | |||||
|---|---|---|---|---|---|---|
| N | 19 | 65 | ||||
| Mean | SD | Mean | SD | U | p | |
| Age (Months) | 26.79 | 3.73 | 27.69 | 4.39 | 421.00 | .40 |
| SES (Hollingshead ISP) | 2.17 | 1.04 | 2.17 | .76 | 512.50 | .36 |
| ADOS-Social Interaction | 11.57 | 2.36 | 10.40 | 2.41 | 792.50 | .06 |
| ADOS-Communication | 5.94 | 1.58 | 5.01 | 1.64 | 831.50 | .02* |
| Mullen-Gross Motora | 17.56 | 3.34 | 18.48 | 2.66 | 331.50 | .05 |
| Mullen-Fine Motora | 17.89 | 3.88 | 19.75 | 4.05 | 474.50 | .15 |
| Mullen-Visual Receptiona | 17.16 | 4.90 | 18.87 | 5.02 | 482.00 | .17 |
| Mullen-Expressive Languagea | 11.89 | 6.59 | 13.34 | 6.31 | 505.00 | .26 |
| Mullen-Receptive Languagea | 8.95 | 5.43 | 12.91 | 6.48 | 396.50 | .02* |
| CSBS-DP CQ-Wordsb | 2.60 | 2.81 | 7.70 | 6.83 | 207.00 | <.01** |
| CSBS-DP CQ-Under. Wordsb | 6.68 | 3.55 | 12.61 | 6.65 | 185.00 | <.01** |
| CSBS-DP CQ-Social Comp.b | 24.78 | 6.76 | 27.07 | 6.40 | 435.50 | .75 |
Scores represent age-equivalent scores
Scores represent raw scores
<.05
<.01
Figure 1.
Age-equivalent scores on the Mullen for minority and non-minority groups
We used logistic regression to assess whether scores on the standardized tests predicted group membership (minority vs. non-minority). At step 1 of the analysis, SES was introduced as a control variable. At step 2, the dependent variables included Mullen Gross Motor Scale, nonverbal cognitive functioning as measured by Mullen Visual Reception Scale, expressive language functioning (Mullen Expressive Language scale), and receptive language functioning (Mullen Receptive Language scale). The omnibus test for the overall model was significant (χ2 = 10.67, p = .01). As shown in Table 3, the only measure that distinguished between the two ethnic groups was the Mullen Receptive Language scores: a one point increase in Mullen Receptive Language scale decreased the likelihood of belonging to the non-minority group by 25 % (OR: .75, p = .02).
Table 3.
Logistic regression for ethnic membership (minority vs. non-minority)
| β | SE | Wald's χ2 | df | p | odds ratio | 95%CI | |
|---|---|---|---|---|---|---|---|
| Control | |||||||
| SES | .49 | .44 | 1.26 | 1 | .26 | 1.64 | .69-3.91 |
| Standardized Scores | |||||||
| Mullen Gross Motor | -.07 | .17 | .18 | 1 | .66 | .93 | .67-1.29 |
| Mullen Visual Reception | .07 | .09 | .51 | 1 | .47 | 1.07 | .88-1.30 |
| Mullen Expressive Language | .05 | .09 | .29 | 1 | .58 | 1.05 | .87-1.25 |
| Mullen Receptive Language | -.28 | .12 | 5.26 | 1 | .02* | .75 | .59-.96 |
Non parametric tests were also conducted on SES to investigate whether children from the five different categories of SES (i.e., upper class, upper-middle class, middle class, lower-middle class, and lower class) differed from each other on the standardized tests. Dependent variables from the following measures were entered into the analyses: CSBS DP CQ Words, Understanding Words, and Social Composite; ADOS Communication and Reciprocal Social Interaction domain scores; and, from the Mullen, Visual Reception, Receptive Language, Expressive Language, Fine Motor, and Gross Motor scale age equivalent scores. A Kruskall-Wallis test did not distinguish among the five SES groups on any of these standardized measures (ps > .05).
Discussion
This study compared ethnic minorities in the Unites States to non-minorities (i.e., Caucasian white) in the clinical presentation of autism symptoms in their toddlers with ASD. The majority of toddlers and their parents in this study belonged to the upper-middle to upper classes, and this was independent of ethnicity. This finding is particularly interesting considering the fact that poverty rates in the United States tend to be higher among minorities (Costello, Keeler, & Angold, 2001); specifically, poverty rates among African-Americans and Hispanics are twice as high as those among non-minorities (Gradin, 2008). The socio-economic characteristic of our sample suggests that early ASD detection is more likely to occur in highly educated families, possibly due to better access to quality health-care services and better financial and educational resources among these families. Moreover, our finding also indicate that ASD children from lower SES backgrounds are underrepresented in research, and that young minority ASD children area at increased risk for delayed enrollment into early intervention services than children from higher socioeconomic classes.
Despite the fact that minorities and non-minorities were from similar SES groups, they differed from each other on the clinical presentation of autism symptoms: minority children with ASD had scores that were indicative of more delayed or atypical language and communication scores on standardized tests as measured by both parent-completed and clinician-administered measures. Cultural differences in views of typical as well atypical development might contribute to this finding. More specifically, minority parents may not identify early and subtle signs of ASD as concerning, but instead may ascribe a different meaning to atypical behaviors or delayed milestones in their children that is meaningful within their cultural context. For example, in some Asian cultures, making direct eye contact with adults or imitating behaviors of parents may be considered disrespectful, and using the index finger to communicate sharing of interest is not as common as in Western cultures (Zang et al., 2006). Moreover, it has been reported that parents of children with disabilities from diverse ethnic backgrounds may view early difficulties in communication and social skills as temporary (Danesco, 1997), or as part of the normal developmental process. Therefore, minority parents of ASD children may not index these behaviors as developmental benchmarks in their young children, and, instead, may rely on more global and observable impairments in areas including language and motor development, which may be easier to identify than the more subtle impairments in social and communication skills that signal the early manifestation of ASD.
A communication gap between parents and health care professionals might also contribute to the differences in symptom presentation of ASD between minorities and non-minorities. Perceived status differences that may stem from unequal levels of authority between professionals and families might be particularly relevant here. Parents from cultures that place a strong emphasis on a “respect for authority,” as in Asian and Hispanic cultures, may not question the health care provider's practices (e.g., failure to screen for ASD), or decisions (e.g., stating that the child is fine without asking about parent concerns, or despite parent-communicated concerns) (Hilton, Fitzgerald, Jackson, Maxim, Bosworth, Shattuck, 2009; Rogers-Adkinson et al., 2006). Such parent-professional interaction styles may diminish minority parents’ willingness to engage in an open discussion about their children's development, which may result in deferred diagnosis of ASD or misdiagnosis.
In order to reduce cultural barriers to accessing diagnostic and intervention services among minority children with ASD, an increased awareness amongst clinicians and health educators of diverse cultural practices and biases within families is needed. There is a need to develop more culturally-sensitive screening and assessment practices, with a special focus on educating parents by providing more detailed information and examples about ASD-specific behaviors. Outreach efforts to minority communities, especially those with lower SES, are needed to enhance awareness of the early signs of ASD and to provide strategies for communication with health care practitioners. The relatively low representation of minorities in our intervention study, a pattern consistent with other research enterprises, highlights the need for outreach materials and efforts to inform minority groups about what is involved in research, how their rights and privacy will be protected, and how research findings translate into improved health care and education for children from minority backgrounds. Moreover, understanding parents’ beliefs and perceptions about their children's development, examining communication styles of parents from diverse cultural backgrounds, and a genuine attempt to incorporate parents into the assessment and treatment process may also empower minority parents to enhance their children's development within their own cultural framework.
It is also possible that differences in clinical presentation of autism symptoms between minorities and non-minorities that we observed in this study (i.e., lower motor and communication scores of minority children with ASD on standardized tests) may represent phenotypic differences between groups. Many complex diseases have different manifestations in different ethnic groups (Cuccaro et al., 2007), such as the higher incidence of schizophrenia among the Black population (Veling, Susser,Van Os, Mackenbach, Selten, & Hoek, 2006) and the involvement of different genes in the development of Alzheimer's diseases in African-Americans and Caucasians (Desai, Hendrie, & Evans, 2003). Cuccaro et al. (2007) showed that parents of 3- to 21-year-old individuals with ASD reported later acquisition of words and phrase speech when interviewed on ADI-R, and proposed that phenotypic differences in clinical features of ASD, particularly impairments in language acquisition, may index genetically meaningful subgroups of ASD. Delineating a possible relation between phenotypic traits and underlying genetic mechanisms is beyond the scope of this paper, and further research is needed in this area to determine whether such an association exists.
In this study, the minority group included participants of African-American, Asian, and Hispanic descent. One limitation of this study includes analyzing minorities from three different ethnicities as one single group. Future research is needed to examine a variety of minority groups to investigate group-specific differences in the symptom presentation of autism. A second limitation of the present study is the lack of information about the age at which parents first noticed signs of developmental disruption in their children, and the nature of the behavior that gave rise to that concern. We are currently investigating this question in another study and will soon report those findings.
Acknowledgments
We would like to thank the toddlers and families who participated in this study. We also thank the research staff at the Kennedy Krieger REACH laboratory in the Center for Autism and Related Disorders who contributed to this project through scheduling, data organization, data collection, and data processing. Rebecca Landa, principal investigator, thanks the National Institute of Mental Health for support of her research through grant #154MH066417, the Maternal and Child Health Research Program - Maternal and Child Health Bureau (Combatting Autism Act), Health Resources and Services Administration, Department of Health and Human Services the Health Resources and Services Administration grant R40 MC 15594, and the Krieger Foundation for their funding.
Abbreviations
- ASD
autism spectrum disorders
- DSM IV-TR
Diagnostic and Statistical Manual IV, Text Revision
- CSBS DP
Communication and Symbolic Behavior Scales Developmental Profile
- ADOS
Autism Diagnostic Observation Schedule
- SES
socioeconomic status
Footnotes
Saime Tek is a post-doctoral fellow of the Johns Hopkins University School of Medicine, at the Center for Autism and Related Disorders of the Kennedy Krieger Institute in Baltimore, MD. Rebecca Landa is the director of the Center for Autism Related Disorders at the Kennedy Krieger Institute and Professor in the Department of Psychiatry and Behavioral Sciences of the Johns Hopkins University School of Medicine, Baltimore, MD. The data for this project were collected at the Kennedy Krieger Institute.
References
- American Psychological Association . Diagnostic and Statistical Manual of Mental Disorders; Volume IV-TR. American Psychological Association; Washington, DC: 2000. [Google Scholar]
- Begeer S, Bouk SE, Boussaid W, Terwogt MM, Koot HM. Underdiagnosis and referral bias of autism in ethnic minorities. Journal of Autism Developmental Disorders. 2009;39:142–148. doi: 10.1007/s10803-008-0611-5. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC) Mental health in the United States: parental report of diagnosed autism in children aged 4–17 years—United States, 2003–2004. 2006 Retrieved from http://www.cdc.gov/ [PubMed]
- Centers for Disease Control and Prevention (CDC) Autism spectrum disorders (ASDs): What should you know? 2010 Retrieved from http://www.cdc.gov/
- Costello EJ, Keeler GP, Angold A. Poverty, race/ethnicity and psychiatric disorder: a study of rural children. American Journal of Public Health. 2001;91:1494–1498. doi: 10.2105/ajph.91.9.1494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuccaro ML, Brinkley JS, Abramson RK, Hall A, Wright HH, Gilbert JR, Pericak-Vance MA. Autism in African-American families: clinical-phenotypic findings. American Journal of Medical Genetics Part B: Neuropsychiatry Genetics. 2007;144:1022–1026. doi: 10.1002/ajmg.b.30535. [DOI] [PubMed] [Google Scholar]
- Danesco ER. Parental belief on childhood disability: insights on culture, child development and intervention. International Journal of Disability, Development and Education. 1997;44:41–52. [Google Scholar]
- Desai PP, Hendrie HC, Evans RM. “Genetic variation in apolipoprotein D affects the risk of Alzheimer disease in African-Americans.”. American Journal of Medical Genetics Part B: Neuropsychiatry Genetics. 2003;116:98–101. doi: 10.1002/ajmg.b.10798. [DOI] [PubMed] [Google Scholar]
- Durkin MS, Maenner MJ, Meaney FJ, Levy SE, DiGuiseppi S, Nicholas JS, Kirby RS, et al. Socioeconomic inequality in the prevalence of autism spectrum disorder: Evidence from a U.S. cross-sectional study. PLoS ONE. 2010;5(7):e11551. doi: 10.1371/journal.pone.0011551. doi:10.1371/journal.pone.0011551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fombonne E. Epidemiological surveys of autism and other pervasive developmental disorders: an update. Journal of Autism and Developmental Disorders. 2003;33:365–382. doi: 10.1023/a:1025054610557. [DOI] [PubMed] [Google Scholar]
- Fountain C, King MD, Bearman PS. Age of diagnosis for autism: individual and community factors across 10 birth cohorts. Journal of Epidemiology and Community Health. 2010:1–10. doi: 10.1136/jech.2009.104588. doi:10.1136/jech.2009.104588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gradin C. Poverty among Minorities in the United States: Explaining the Racial Poverty Gap for Blacks and Latinos, Working Papers 96, Society for the Study of Economic Inequality. 2008 Retrieved from http://www.ecineq.org/milano/WP/ECINEQ2008-96.pdf.
- Hilton CL, Fitzgerald RT, Jackson KM, Maxim RA, Bosworth CC, Shattuck PT, et al. Brief report: Under-representation of African Americans in autism genetic research: a rationale for inclusion of subjects representing diverse family structures. Journal of Autism and Developmental Disorders. 2009;40:633–639. doi: 10.1007/s10803-009-0905-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hollingshead AB. Four Factor Index of Social Status. Yale University, Department of Sociology, Working Paper; New Haven: 1975. [Google Scholar]
- Landa R, Holman K, Garrett-Mayer E. Social and communication development in toddlers with early and later diagnosis of autism spectrum disorders. Archives of General Psychiatry. 2007;64:853–864. doi: 10.1001/archpsyc.64.7.853. [DOI] [PubMed] [Google Scholar]
- Liptak GS, Benzoni LB, Mruzek DW, Nolan KW, Thingvoll MA, Wade CM, Fryer E. Disparities in diagnosis and utilization of health services for children with autism: Data from the national survey of children's health. Journal of Developmental and Behavioral Pediatrics. 2008;29:152–160. doi: 10.1097/DBP.0b013e318165c7a0. [DOI] [PubMed] [Google Scholar]
- Lord C, Rutter M, DiLavore P, Risi S. Autism Diagnostic Observation Schedule. Western Psychological Services; Los Angeles, CA: 1999. 1999. [Google Scholar]
- Mandell DS, Listerud J, Levy SE, Pinto-Martin JA. Race differences in the age at diagnosis among Medicaid-eligible children with autism. Journal of the American Academy of Child and Adolescent Psychiatry. 2002;4:1447–1453. doi: 10.1097/00004583-200212000-00016. [DOI] [PubMed] [Google Scholar]
- Mandell D, Novak M. The role of culture in families’ treatment decisions for children with autism spectrum disorders. Mental Retardation and Developmental Disabilities Research Reviews. 2005;11:110–115. doi: 10.1002/mrdd.20061. [DOI] [PubMed] [Google Scholar]
- Mandell DS, Novak MM, Zubritsky CD. Factors associated with the age of diagnosis among children with autism spectrum disorders. Pediatrics. 2005;116:1480–1486. doi: 10.1542/peds.2005-0185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mandell DS, Ittenbach RF, Levy SE, Pinto-Martin JA. Disparities in diagnoses received prior to a diagnosis of autism spectrum disorder. Journal of Autism and Developmental Disorders. 2007;37:1795–1802. doi: 10.1007/s10803-006-0314-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mandell DS, Wiggins LD, Carpenter LA, Daniels J, DiGuiseppi C, Durkin MS, et al. Racial/ethnic disparities in the identification of children with autism spectrum disorders. American Journal of Public Health. 2009;99:493–498. doi: 10.2105/AJPH.2007.131243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mullen EM. Mullen Scales of Early Learning (AGS Edition) American Guidance Service; Circle Pines, MN: 1995. [Google Scholar]
- Pachter LM, Dworkin PH. Maternal expectations about normal child development in 4 cultural groups. Archives of Pediatrics and Adolescent Medicine. 1997;151:1144–1150. doi: 10.1001/archpedi.1997.02170480074011. [DOI] [PubMed] [Google Scholar]
- Post DM, Cegala DJ, Marinelli TM. Teaching patients to communicate with physicians: The impact of race. Journal of the National Medical Association. 2001;93:6–12. [PMC free article] [PubMed] [Google Scholar]
- Roberts KT, Robinson KM, Topp R, Newman J, Smith F, Stewart C. Community perceptions of mental health needs in an underserved minority neighborhood. Journal of Community Health and Nursing. 2008;25:203–217. doi: 10.1080/07370010802421202. [DOI] [PubMed] [Google Scholar]
- Rogers-Adkinson DL, Ochoa TA, Delgado B. Developing cross-cultural competence: Serving families of children with significant developmental needs. Focus on Autism and Other Developmental Disabilities. 2003;18:4–8. [Google Scholar]
- Schopler E, Andrews C, Strupp K. Do autistic children come from upper middle class parents? Journal of Autism and Developmental Disorders. 1979;9:139–152. doi: 10.1007/BF01531530. [DOI] [PubMed] [Google Scholar]
- Veling W, Susser E, Van Os J, Mackenbach JP, Selten JP, Hoek HW. Ethnic density of neighborhoods and incidence of psychotic disorders among immigrants. American Journal of Psychiatry. 2008;165:66–73. doi: 10.1176/appi.ajp.2007.07030423. [DOI] [PubMed] [Google Scholar]
- Wetherby A, Prizant B. CSBS DP Manual: Communication and Symbolic Behavior Scales Developmental Profile. Paul H Brookes Publishing Co.; Baltimore, MD: 2002. [Google Scholar]
- Zhang J, Wheeler JJ, Richey D. Cultural validity in assessment instruments for children with autism from a Chinese cultural perspective. International Journal of Special Education. 2006;21:109–114. [Google Scholar]