Abstract
Background
In order to maximize organ donation opportunities, the American College of Surgeons (ACS) requires verified trauma centers to have: 1) a relationship with an organ procurement organization (OPO), 2) a policy for notification of the OPO, 3) a process to review organ donation rates, and 4) a protocol for declaring neurologic death. We hypothesized that meeting the ACS requirements will be associated with improved donation outcomes.
Study Design
24ACS-verified Level I and II trauma centers were surveyed for the following registry data points from 2004-2008: admissions, ICU admissions, patients with a head abbreviated injury score ≥ 5, deaths, and organ donors. Centers were also queried for the presence of the ACS requirements as well as other process measures and characteristics. The main outcome measure was the number of organ donors per center normalized for patient volume and injury severity. The relationship between center characteristics and outcomes was determined.
Results
21 centers (88%) completed the survey and referred 2,626 trauma patients to the OPO during the study period, 1008 were eligible to donate, and 699 became organ donors. Compliance with the 4 ACS requirements was not associated with increased organ donation outcomes. However, having catastrophic brain injury guidelines (CBIGs) and the presence of a trauma surgeon on a donor council were associated with significantly more organ donors per 1000 trauma admissions (6.3 vs. 4.2 and 6.0 vs. 4.2, respectively, p<0.05).
Conclusions
While the ACS trauma center organ donation-related requirements were not associated with improved organ donor outcomes, involvement of trauma surgeons on donor councils and CBIGs were and should be encouraged. Additionally, the incorporation of quantitative organ donation measures into the verification process should be considered.
Keywords: trauma center verification, organ donation, catastrophic brain injury guidelines, process improvement, outcomes
Introduction
The shortage of organs available for transplantation continues to be a public health crisis. As of November 2011, there were over 112,000 patients on the Organ Procurement and Transplantation Network (OPTN)/United Network for Organ Sharing (UNOS) waiting list and only 28,000 transplants performed in the last year(1). One of the contributing factors to this gap between needed and available organs is a static number of deceased organ donors over the past several years(1). However, when one considers that over 75% of families consent to organ donation when approached by an appropriate requestor (Organ and Procurement Transplantation Network data January 2008–June 2010) and that approximately 41% of the adult population in the United States is currently registered to be an organ donor on a state registry(2), it is evident that the desire to donate organs is prevalent in both our patients and their families.
In order to respect and carry out these wishes as well as to help alleviate the shortage of organs available for transplantation, the Revised Uniform Anatomical Gift Act requires organ procurement organizations (OPOs) and donor hospitals to have the necessary policies and procedures in place to preserve the option of donation for every patient and their family(3). Furthermore, given that the majority of organs procured for transplantation are obtained from donors after neurologic determination of death (DNDD, revised terminology for “brain death”), trauma patients with catastrophic brain injuries represent an important group of potential donors. In an effort to maximize donation opportunities, the American College of Surgeons (ACS) qualitatively evaluates each hospitals organ donation practices during the trauma center verification process(4). Specifically, the American College of Surgeons requires verified trauma centers to(4): 1) establish a relationship with an OPO 2) develop policies and clinical triggers for notification of the OPO about patients with the potential for neurologic death, 3) have a formal process to review organ donation rates, and 4) implement protocols for the declaration of neurologic death. No study to date has evaluated the impact of meeting these requirements on outcomes.
Given this, the objectives of this study were to 1) evaluate the impact of these current qualitative requirements on organ donation-related outcomes in order to ascertain if they should be considered sufficient for trauma center verification, 2) to determine if there are other trauma center process measures and characteristics that are associated with improved outcomes, and 3) to identify quantitative, as opposed to qualitative, measures of trauma center performance that may be more appropriate in evaluating each trauma center’s performance related to preserving the option of donation for their patients and families.
Methods
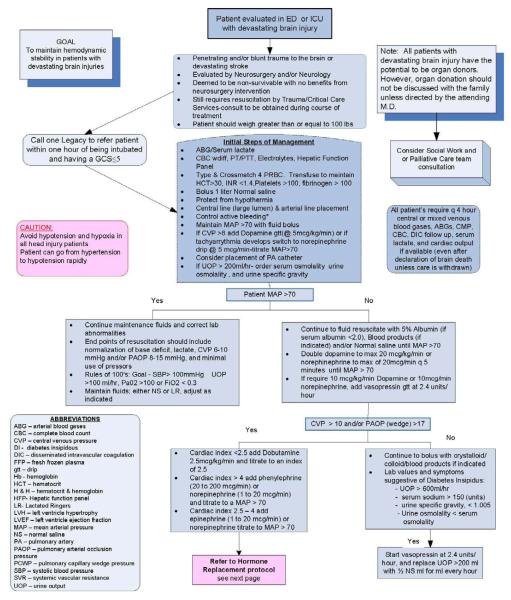
A survey study of all Level I and Level II trauma centers in the seven-county greater Los Angeles donation service area was conducted and respondents were sent a check for $50 for their time and effort. These centers were surveyed for data from 2004-2008. Specifically, these trauma centers were queried for their number of trauma admissions, as well as how many of these trauma admissions were admitted to the intensive care unit, how many had a head abbreviated injury score (AIS) ≥ 5, how many died, and the number who became organ donors. This data was used to normalize the number of trauma organ donors per center based on patient volume and injury severity.Additionally, the trauma centers were surveyed on the presence of the four qualitative ACS requirements, the presence of other organ donation-related process measures (catastrophic brain injury guidelines [CBIGs, see Figure 1 for an example] and the capacity for conducting donation after circulatory determination of death [DCDD, synonymous with “donation after cardiac death” or “DCD”]), as well as the following institutional characteristics: the presence of an organ donor council and if there was a trauma surgeon present on the council, the presence of a transplant program, the presence of a surgery residency program, the level of trauma center, and whether there was an academic affiliation. In regards to CBIGs, it is important to note that they come in many forms (order sets, clinical pathways, treatment algorithms, etc.) and contain recommendations for assessing and managing the physiologic derangements that accompany severe brain injuries or neurologic death. They are useful in management of patients who have been deemed to have “non-survivable” neurologic injuries by a neurosurgery/neurology consulting service and typically contain treatments that are aimed at achieving hemodynamic stability as well as standard critical care endpoints of resuscitation, but do not involve efforts to monitor or treat intracranial pressure (ICP). By so doing, they enable providers to maintain hemodynamic stability and perfusion to the entire body. This affords the opportunity to observe a patient’s true clinical trajectory, allowing for clinical improvement and not eliminating any end-of-life care options at the same time. In regards to capacity for DCDD, this was defined as hospitals with the policies and procedures in place to conduct DCDD.
Figure 1.
Example of a Catastrophic Brain Injury Guideline (CBIG) (Figure initially published in the Western Journal of Emergency Medicine, Volume 10, Issue 1, Pages 11-7. Reprinted courtesy of the authors.
Survey results from each trauma center were combined with an existing database containing all referrals for donation and their outcomes in the seven county greater Los Angeles donation service area covered by the OneLegacy OPO. Normalized donation related outcomes (e.g. the number of organ donors per 1000 trauma admissions, donors per 1000 ICU admissions, etc.) as well as the Health Resources and Services Administration (HRSA) collaborative conversion rate were compared in trauma centers with and without the following characteristics: compliance with the four qualitative ACS requirements, presence of CBIGs, capacity for DCDD, presence of an organ donor council, presence of a trauma surgeon on the organ donor council, presence of a transplant program, presence of surgery residents, level of trauma center, and academic affiliation. According to HRSA guidelines, the collaborative conversion rate was defined as the sum of eligible donors and noneligble donors divided by the sum of eligible deaths and noneligible donors. Eligible deaths were defined as those patients who were declared dead by neurologic criteria, were less than 70 years old, and did not have medical contraindications for transplantation. Noneligible donors were defined as either DNDDs who were greater than 70 years of age or those who were DCDDs.
Analyses of categorical variables were conducted using either the Pearson’s chi-square or Fisher’s Exact test, and analyses of continuous variables were performed using the Mann Whitney U test. A p value < 0.05 was considered significant and values in the text and tables are reported as median (interquartile range). Statistical analysis was performed with SPSS version 18.0 for Windows (SPSS, Chicago, Illinois). This study was submitted to the Institutional Review Board at the University of California Irvine and was determined to be non-human subjects research.
Results
Of the 24 Level I and Level II trauma centers surveyed, 21 responded yielding a response rate of 88%. In the 21 hospitals that responded, 2,262 trauma patients with imminent neurologic death were referred to the OPO from 2004-2008. Of these, 1,008 were eligible deaths and 699 became organ donors.
The results of the comparison of normalized donation related outcomes and the collaborative conversion rate between trauma centers with and without the aforementioned hospital characteristics are presented in Tables 1-3. Across all 21 centers, the median number of donors per 1000 trauma admission was 5.3, per 1000 ICU admissions was 19, per 1000 patients with head AIS ≥ 5 was 117, and per 1000 trauma deaths was 127. The mean collaborative conversion rate was found to be 67%.
Table 1.
Comparison of Normalized Donation-Related Outcomes and the Collaborative Conversion Rate between Trauma Centers Based on Compliance with the Four American College of Surgeon Qualitative Requirements
| Trauma center characteristic |
No. of centers | Donors per 1,000, median (IQR) | Conversion rate, % |
|||
|---|---|---|---|---|---|---|
| Trauma admissions |
ICU admissions |
Head AIS ≥5 patients |
Trauma deaths |
|||
| Overall | 21 (100%) |
5.3 (3.8-6.6) |
19 (11-23) |
117 (84-164) |
127 (108-152) |
67 |
| ACS Compliant | 14 (67%) |
5.1 (3.4-6.7) |
20 (13-24) |
117 (90-161) |
130 (101-152) |
68 |
| ACS Non- Compliant |
7 (33%) |
5.3 (2.1-7.1) |
15 (6.3-21) |
129 (73-812) |
119 (101-213) |
64 |
| p Value | N/A | 0.88 | 0.26 | 0.62 | 0.87 | 0.20 |
IQR, Interquartile Range; ICU, Intensive Care Unit; AIS, Abbreviated Injury Scale; ACS, American College of Surgeons; Conversion rate: eligible and non-eligible donors/eligible deaths + non-eligible donors.
Table 3.
Comparison of Normalized Donation Related Outcomes and the Collaborative Conversion Rate between Trauma Centers Based on Institutional Characteristics
| Trauma center characteristic |
No. of trauma centers (%) |
Donors per 1,000, median (IQR) | Conversion rate, % |
|||
|---|---|---|---|---|---|---|
| Trauma admissions |
ICU Admissions |
Head AIS ≥5 patients |
Trauma deaths |
|||
| Overall | 21 (100) |
5.3 (3.8-6.6) |
19 (11-23) |
117 (84-164) |
127 (108-152) |
67 |
| Organ Donor Council |
18 | 5.4 (4.1-6.9) |
20 (13-24) |
119 (93-166) |
128 (107-155) |
68 |
| No Organ Donor Council |
3 | 2.1* | 7.2* | 75* | 114* | 64 |
| p Value | N/A | 0.13 | 0.48 | 0.63 | 0.87 | 0.47 |
| Trauma surgeon on Organ Donor Council |
14 (67) |
6.0 (4.3-7.3) |
21 (15-24) |
143 (95-193) |
127 (101-168) |
67 |
| No trauma surgeon on council or no council at all |
7 (33) |
4.2 (1.7-5.5) |
11 (6.3-16) |
87 (66-450) |
133 (107-182) |
68 |
| p Value | N/A | 0.04 | 0.03 | 0.19 | 0.68 | 0.86 |
| Transplant program |
9 (43) |
4.6 (2.2-6.9) |
19 (11-24) |
155 (81-168) |
135 (122-188) |
66 |
| No transplant program |
12 (57) |
5.4 (3.9-6.6) |
18 (11-25) |
103 (78-231) |
119 (98-146) |
69 |
| p Value | N/A | 0.72 | 0.89 | 0.54 | 0.25 | 0.33 |
| Surgery residents present |
13 (62) |
4.5 (2.2-4.6) |
15 (9-25) |
103 (67-158) |
126 (90-141) |
66 |
| No surgery residents present |
8 (38) |
6.9 (3.9-8.7) |
21 (13-23) |
149 (103-239) |
138 (111-183) |
71 |
| p Value | N/A | 0.10 | 0.77 | 0.19 | 0.36 | 0.11 |
| Level 1 | 6 (29) |
4.9 (1.8-5.9) |
19 (11-29) |
149 (78-243) |
127 (75-158) |
65 |
| Level 2 | 15 (71) |
5.5 (3.8-7.1) |
19 (11-23) |
115 (75-171) |
128 (110-163) |
69 |
| p Value | N/A | 0.39 | 0.76 | 0.76 | 0.36 | 0.22 |
| Academic | 6 (29) |
4.9 (1.6-5.9) |
19 (11-29) |
149 (103-243) |
132 (100-162) |
66 |
| Not Academic | 15 (71) |
5.5 (3.8-7.1) |
19 (11-23) |
107 (68-171) |
125 (103-163) |
68 |
| p Value | N/A | 0.31 | 0.88 | 0.36 | 0.97 | 0.38 |
n=3 so interquartile range was not calculated.
IQR, Interquartile Range; ICU, Intensive Care Unit; AIS, Abbreviated Injury Scale; Conversion rate = eligible and non-eligible donors/eligible deaths + non-eligible donors.
Regarding compliance with the ACS trauma center requirements, 67% (14/21) of the surveyed trauma centers were compliant with all four requirements. Comparing hospitals that were compliant to those that were not, no statistical significance difference in organ donation related outcomes was observed (Table 1).
The results of the association between other trauma center process measures and outcomes is presented in Table 2. Comparing hospitals with CBIGs to those without, a significant difference in organ donation-related outcomes was noted. Specifically, hospitals with CBIGs had significantly more median number of donors per 1000 trauma admissions (6.3 vs. 4.2, p = 0.04) as well as a significantly higher conversion rate (70% vs. 63%, p = 0.01). However, only 48% (10/21) of the surveyed trauma centers had CBIGs. The presence of the capacity for DCDD was not associated with a difference in outcomes.
Table 2.
Comparison of normalized donation-related outcomes and the collaborative conversion rate between trauma centers based on the presence of other organ donation-related process measures.
| Trauma center characteristic |
No. of trauma centers (%) |
Donors per 1,000, median (IQR) | Conversion rate, % |
|||
|---|---|---|---|---|---|---|
| Trauma admissions |
ICU Admissions |
Head AIS ≥5 patients |
Trauma deaths |
|||
| Overall | 21 (100) |
5.3 (3.8-6.6) |
19 (11-23) |
117 (84-164) |
127 (108-152) |
67 |
| Catastrophic Brain Injury Guidelines |
10 (48) |
6.3 (4.6-8.1) |
22 (14-24) |
161 (122-293) |
132 (124-174) |
70 |
| No Catastrophic Brain Injury Guidelines |
11 (52) |
4.2 (2.1-5.5) |
15 (11-21) |
98 (68-119) |
114 (85-148) |
63 |
| p Value | N/A | 0.04 | 0.32 | 0.07 | 0.16 | 0.01 |
| Capacity for DCDD |
17 (81) |
5.3 (3.3-6.7) |
16 (11-23) |
113 (73-161) |
129 (105-159) |
67 |
| No Capacity for DCDD |
4 (19) |
4.7 (2.5-10) |
23 (10-46) |
189 (85-1174) |
121 (101-244) |
67 |
| p Value | N/A | 0.93 | 0.33 | 0.35 | 1.00 | 0.99 |
IQR, Interquartile Range; ICU, Intensive Care Unit; AIS, Abbreviated Injury Scale; DCDD, donation after circulatory determination of death; Conversion rate, eligible and non-eligible donors/eligible deaths + non-eligible donors
Table 3 contains the results of the analysis of the association between additional institutional characteristics and organ donation-related outcomes. Hospitals with trauma surgeons on their organ donor councils had significantly more median number of donors per 1000 trauma admissions (6.0 vs. 4.2, p = 0.04) as well as significantly more donors per 1000 ICU admissions (21 vs. 11, p = 0.03). Overall, however, only 67% of trauma centers had a trauma surgeon on their organ donor council. None of the other institutional characteristics were found to be associated with significantly different organ donation-related outcomes.
Discussion
Since 2001, over 7,000 patients have died each year while awaiting organ transplantation(1). With the majority of donated organs coming from deceased donors and with traumatic brain injury representing one of the most common mechanisms of neurologic death in these patients, the American College of Surgeons has established qualitative criteria that are used to evaluate each hospitals organ donation practices during the trauma center verification process. Seeking to determine the impact of meeting these requirements on outcomes, this study found that compliance with the current ACS trauma center organ donation-related requirements was not associated with improved organ donation outcomes. However, the presence of CBIGs and the involvement of trauma surgeons on organ donor councils were associated with an increased number of organ donors and higher conversion rates. In addition, quantitative organ donation measures, normalized for patient volume and severity, were identified and a preliminary set of median values with inter-quartile ranges were determined for the greater Los Angeles donation service area.
Currently, the American College of Surgeons qualitative evaluation process can identify a center’s efforts as strengths, weaknesses, or deficiencies. As mentioned, centers meeting all four the qualitative ACS requirements in this investigation were not found to have significantly different organ donation-related outcomes and only two-thirds were actually compliant with the requirements. In order to better evaluate such practices, a quantitative assessment of hospital trauma-related organ donation outcomes could help determine if a trauma center has above, at, or below expected outcomes. Such determinations could create the opportunity to identify the best practices of high-performing centers for dissemination to those centers that have room for improvement. Additionally, quantitative assessment allows for continuous evaluation of the impact of these practices on the number and quality of organs available for transplantation. Potential quantitative organ donation measures that should be considered and were used in this study include, the number of donors per 1000 trauma admissions, per 1000 ICU admissions, per 1000 head AIS ≥5 patients, and per 1000 trauma deaths. By their definition, these measures are normalized for patient volume and severity. Using these measures, specific practices such as the presence of CBIGs as well as the participation of trauma surgeons on organ donor councils were noted to be significantly associated with increased numbers of organ donors.
Many hospitals have adopted CBIGs to assist in the management of patients with neurologic injuries and a very poor prognosis. These guidelines contain standard critical care practices that would be appropriate for many patients with survivable injuries and also reflect the donor management protocols that many OPO personnel utilize after consent. With the use of these guidelines patients who were once thought to have fatal injuries can neurologically improve. Even for patients who regress to neurologic death and subsequently become organ donors, these intensive care unit practices that aim to improve perfusion of the brain will also, by their nature, improve perfusion of the other organs. In the end, optimizing the care of patients with devastating neurologic injuries has the potential to benefit these patients as well as the recipients of their organs for those who go on to donate. These practices also preserve the option of donation for the families of these patients, which has the potential to positively impact their grieving process and has been associated with less risk for depression(5).
Although the impact that CBIGs and other similar management protocols have on organ donation outcomes has been well documented(6-16) there still remain a larger proportion of centers that have yet to adopt them. Specifically, in the current study, of the 21 Level I and Level II trauma centers analyzed, 52% (11/21) of respondents stated that they did not have protocols for managing patients with catastrophic brain injuries or potential organ donors. In order to avoid ambiguity, the survey question stem indicated that such protocols are sometimes referred to as CBIGs, devastating brain injury pathways, or aggressive donor management protocols. Reasons for why these centers currently do not have CBIGs in place could not be discerned from the survey results. There is need for further education about their potential benefits and investigation into the current impediments in implementation.
With regards to organ donor councils, a previous investigation by Kong et. al suggests that a multidisciplinary organ donor council consisting of surgeons, intensivists, critical care nurses, hospital administrators, chaplains, and volunteer community members may have a potential benefit on outcomes(17). This previous study, however, did not specifically evaluate the impact of having certain members on the council(17). Using quantitative measures, the current study found that involvement of a trauma surgeon on the organ donor council, who can serve as a clinical champion, is associated with an increased number of organ donors normalized for trauma patient severity and volume. It should be noted, however, that the impact of having other members on the council (e.g. non clinicians) may also have a similar benefit but it was not specifically studied in this report. Regardless, similar to the case with CBIGs, there remains a large portion of respondent hospitals (33%) that currently do not have a trauma surgeon on their organ donor council or do not have a council at all. This serves as another example in which quantitative assessment measures have helped identify a specific practice (i.e. involving a trauma surgeon on the organ donor council) that may improve organ donation-related outcomes.
Limitations of this study should be taken into consideration. As a survey study, data gathered was restricted to that queried at the time of request. For example, information regarding why particular centers did not have specific process measures in place as well as specific details of organ donor council membership would have been beneficial in helping interpret findings, but were not questions that were asked. Further, since this study evaluated the impact of meeting the qualitative requirements used to assess organ donation practices during the ACS trauma center verification process, it only eval uated trauma patient referrals from Level I and Level II centers. Thus, while some process measures (e.g. capacity for DCDD, presence of a transplant program, presence of surgical residents, or academic status) did not seem to have an impact on organ donation related outcomes in this investigation, they may have an impact when all referrals (including those that are non-trauma) are considered. Lastly, it is important to reiterate that there are currently no objective measures of organ donation potential normalized for patient volume or severity. Consequently, the four measures that are suggested (the number of donors per 1000 trauma admissions, per 1000 ICU admissions, per 1000 head AIS ≥ 5 patients, and per 1000 trauma deaths) are intended to be starting points for future evaluation and discussion. Limitations of these measures should thus be kept in mind. For example, although donors per 1000 trauma admissions has the advantage of being a more global measure, it may be suggested that donors per 1000 ICU admissions is a better measure since only intubated patients with severe neurologic injuries have the potential to become brain dead and donate their organs.
The substantial difference between the number of organs available for donation and the expanding list of patients awaiting transplantation have encouraged efforts to increase donation and transplantation. In order to identify best practices of high-performing centers so that they can be disseminated to those who have room for improvement, evaluation of each hospital’s trauma-related organ donation practices using measures that directly reflect outcomes is imperative. Given that meeting the current qualitative measures used during the ACS trauma verification process was not found to significantly impact organ donation-related outcomes, quantitative measures such as those normalized for patient volume and injury severity should be considered. Once organ donation practices can be quantitatively assessed and benchmarks can be established, hospital policies and procedures focused on increasing the number and quality of organs available for transplantation can be created, implemented, and continuously evaluated. Such measures will also serve to preserve the option of donation for patients and their families.
Acknowledgment
The authors would like to thank all of the organ donor families and recipients as well as the staff and leadership of the eight organ procurement organizations in Region 5: Donor Network of Arizona, California Transplant Donor Network, Golden State Donor Services, OneLegacy, Lifesharing, New Mexico Donor Services, Nevada Donor Network, and Intermountain Donor Services.
Supported, in part, by the National Institute of Diabetes and Digestive and Kidney Diseases grant Number 5RO1DK079667. Additionally, this work was supported in part by Health Resources and Services Administration contract 234-2005-37011C. The content is the responsibility of the authors alone and does not necessarily reflect the views or policies of the Department of Health and Human Services, nor does mention of trade names, commercial products, or organizations imply endorsement by the U.S. Government.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosure information: Nothing to disclose.
Abstract presented at the Pacific Coast Surgical Association 82nd Annual Meeting, Scottsdale, AZ, February 2011.
References
- 1. [Accessed Novemeber 1st, 2011];The Organ Procurement and Transplantation Network. Available at: http://optn.transplant.hrsa.gov/
- 2. [Accessed March 9, 2011];Donate Life America National Donor Designation Report Card - April 2010. Available at: http://www.donatelife.net/
- 3.Revised Uniform Anatomical Gift Act [Accessed March 16, 2011];Last Revised or Amended in 2008. Available at: http://uniformlaws.org/Shared/Docs/Finals_NC/UAGA_Final_NC.doc.
- 4.Resources for Optimal Care of the Injured Patient. American College of Surgeons; Chicago: 2006. [PubMed] [Google Scholar]
- 5.Merchant SJ, Yoshida EM, Lee TK, et al. Exploring the psychological effects of deceased organ donation on the families of the organ donors. Clin Transplant. 2008;22:341–347. doi: 10.1111/j.1399-0012.2008.00790.x. [DOI] [PubMed] [Google Scholar]
- 6.DuBose J, Salim A. Aggressive organ donor management protocol. J Intensive Care Med. 2008;23:367–375. doi: 10.1177/0885066608324208. [DOI] [PubMed] [Google Scholar]
- 7.Jenkins DH, Reilly PM, Schwab CW. Improving the approach to organ donation: a review. World J Surg. 1999;23:644–649. doi: 10.1007/pl00012362. [DOI] [PubMed] [Google Scholar]
- 8.Ullah S, Zabala L, Watkins B, et al. Cardiac organ donor management. Perfusion. 2006;21:93–98. doi: 10.1191/0267659106pf851oa. [DOI] [PubMed] [Google Scholar]
- 9.Powner DJ, Darby JM, Kellum JA. Proposed treatment guidelines for donor care. Progress in transplantation. 2004;14:16–26. doi: 10.1177/152692480401400103. quiz 27-18. [DOI] [PubMed] [Google Scholar]
- 10.Salim A, Martin M, Brown C, et al. The effect of a protocol of aggressive donor management: Implications for the national organ donor shortage. The Journal of trauma. 2006;61:429–433. doi: 10.1097/01.ta.0000228968.63652.c1. discussion 433-425. [DOI] [PubMed] [Google Scholar]
- 11.Salim A, Velmahos GC, Brown C, et al. Aggressive organ donor management significantly increases the number of organs available for transplantation. The Journal of trauma. 2005;58:991–994. doi: 10.1097/01.ta.0000168708.78049.32. [DOI] [PubMed] [Google Scholar]
- 12.Rosendale JD, Kauffman HM, McBride MA, et al. Aggressive pharmacologic donor management results in more transplanted organs. Transplantation. 2003;75:482–487. doi: 10.1097/01.TP.0000045683.85282.93. [DOI] [PubMed] [Google Scholar]
- 13.Wheeldon DR, Potter CD, Dunning J, et al. Haemodynamic correction in multiorgan donation. Lancet. 1992;339:1175. doi: 10.1016/0140-6736(92)90778-2. [DOI] [PubMed] [Google Scholar]
- 14.Straznicka M, Follette DM, Eisner MD, et al. Aggressive management of lung donors classified as unacceptable: excellent recipient survival one year after transplantation. J Thorac Cardiovasc Surg. 2002;124:250–258. doi: 10.1067/mtc.2002.123813. [DOI] [PubMed] [Google Scholar]
- 15.Rosendale JD, Chabalewski FL, McBride MA, et al. Increased transplanted organs from the use of a standardized donor management protocol. American journal of transplantation: official journal of the American Society of Transplantation and the American Society of Transplant Surgeons. 2002;2:761–768. doi: 10.1034/j.1600-6143.2002.20810.x. [DOI] [PubMed] [Google Scholar]
- 16.Angel LF, Levine DJ, Restrepo MI, et al. Impact of a lung transplantation donor-management protocol on lung donation and recipient outcomes. Am J Respir Crit Care Med. 2006;174:710–716. doi: 10.1164/rccm.200603-432OC. [DOI] [PubMed] [Google Scholar]
- 17.Kong AP, Barrios C, Salim A, et al. A multidisciplinary organ donor council and performance improvement initiative can improve donation outcomes. The American surgeon. 2010;76:1059–1062. doi: 10.1177/000313481007601007. [DOI] [PubMed] [Google Scholar]