Abstract
Objective
A group dissonance-based eating disorder prevention program, in which young women critique the thin-ideal, reduces eating disorder risk factors and symptoms, but it can be difficult to identify school clinicians with the time and expertise to deliver the intervention. Thus, we developed a prototype Internet version of this program and evaluated it in a preliminary trial.
Method
Female college students with body dissatisfaction (N = 107; M age = 21.6 SD = 6.6) were randomized to the Internet intervention, group intervention, educational video condition or educational brochure condition.
Results
Internet and group participants showed greater pre-post reductions in eating disorder risk factors and symptoms than video controls (M d = .47 and .54 respectively) and brochure controls (M d = .75 and .72, respectively), with many effects reaching significance. Effects did not differ significantly for Internet versus group participants (M d = -.13) or for video versus brochure controls (M d = .25). Effect sizes for the Internet intervention were similar to those previously observed for group versions of this intervention.
Conclusions
Results suggest that this prototype Internet intervention is as efficacious as the group intervention, implying there would be merit in completing this intervention and evaluating it in a fully powered trial.
Keywords: prevention, Internet, body dissatisfaction, eating disorder
Eating disorders, which afflict 10% of adolescent girls and young women, are marked by functional impairment, morbidity, mortality, and increased risk for future health and mental health problems (Arcelus, Mitchell, Wales, & Nielsen, 2011; Crow et al., 2009; Stice, Marti, Shaw, & Jaconis, 2009a). Thus, a public health priority is to develop and disseminate effective eating disorder prevention programs.
Considerable support has emerged for a selective dissonance-based eating disorder prevention program (Body Project) in which young women at risk for eating disorders due to body image concerns critique the thin ideal espoused for women in verbal, written, and behavioral exercises (Stice, Mazotti, Weibel, & Agras, 2000). These activities theoretically cause cognitive dissonance that motivates participants to reduce pursuit of the thin-ideal, decreasing body dissatisfaction, unhealthy weight control behaviors, negative affect, and eating disorder symptoms. Efficacy trials have found that the Body Project produces greater reductions in eating disorder risk factors (e.g., thin-ideal internalization, body dissatisfaction, negative affect), eating disorder symptoms, functional impairment, and future onset of eating disorders over a 3-year follow-up than assessment-only or alternative intervention control conditions (e.g., Stice et al., 2000; Stice, Shaw, Burton, & Wade, 2006; Stice, Marti, Spoor, Presnell, & Shaw, 2008). Efficacy trials conducted by independent researchers have also found that dissonance-based prevention programs produce greater reductions in risk factors and eating disorder symptoms relative to an assessment-only control condition (Mitchell, Mazzeo, Rausch, & Cooke, 2007) and an alternative intervention (Becker, Smith, & Ciao, 2005).
Consistent with the intervention theory for the Body Project, reductions in thin-ideal internalization appear to mediate the effects of the intervention on change in the outcomes (Seidel, Presnell, & Rosenfield, 2009; Stice, Marti, Rohde, & Shaw, 2011a; Stice, Presnell, Gau, & Shaw, 2007a) and completion of the Body Project offsets the risk for eating disorder onset conveyed by the most potent risk factor in a high-risk sample – denial of costs of pursuing the thin-ideal – which had an odds ratio of 5.0 (Stice, Rohde, Gau, & Shaw, in press). In support of the thesis that dissonance induction contributes to the effects of this intervention, participants assigned to high-dissonance versions of this program show significantly greater reductions in eating disorder symptoms than those assigned to low-dissonance versions of this program (Green, Scott, Divankova, Gasser, & Pederson, 2005; McMillan, Stice, & Rohde, 2011).
Effectiveness trials have confirmed that the Body Project produces similar effects when high school counselors recruit at risk young women with body image concerns and deliver the intervention under ecologically valid conditions, including significant reductions in eating disorder symptoms that persist through 3-year follow-up (Stice, Rohde, Gau, & Shaw, 2009; Stice, Rohde, Shaw, & Gau, 2011c). Even larger effects are emerging in an ongoing effectiveness trial (Stice, Rohde, Shaw, Butryn, & Marti, 2011b), in which college counselors recruit young women with body image concerns and deliver an enhanced-dissonance program. The enhanced-dissonance program added elements that putatively increase dissonance induction, including components that (a) underscore the voluntary nature of participation in the sessions, (b) increase public accountability for counter thin-ideal perspectives, and (c) make in-session and home exercises more effortful. However, these effectiveness trials have revealed that it can be difficult to identify and recruit clinicians at high schools and colleges who have the time and expertise to competently deliver the program. Further, clinician turnover has caused implementation and sustainability challenges.
One solution to this dissemination barrier would be to develop an Internet version of this program, which would facilitate broad implementation. Meta-analytic reviews have found that the average effect for Internet interventions was a d = .60 for depression and anxiety (Barak et al., 2008) and a d = .53 for a broader range of health and mental health problems (Speck et al., 2007), both of which are medium effects. Other meta-analytic reviews found that there was no significant difference in the magnitude of effects for Internet interventions and face-to-face versions of the same intervention (Andersson & Cuijpers, 2009; Barak et al., 2008). Given that over 95% of adolescent girls/young women have access to the Internet (Odell et al., 2008), spending an average of 1.2 hours per day using the Internet (Rideout, Foehr, & Roberts, 2010), this medium appears particularly germane to this population.
The Internet-based eating disorder prevention program that has been evaluated most extensively is Student Bodies (e.g., Celio et al., 2000; Winzelberg et al., 1998, 2000; Zabinski et al., 2001). However, even the version of this pioneering selective prevention program that includes 8 hours of live therapist-led chat room interchanges and face-to-face meetings, which is over twice the therapist contact hours of the Body Project, has not significantly reduced eating disorder symptoms or eating disorder onset (Low et al., 2006; Taylor et al., 2006; Zabinski et al., 2004). As noted, our effectiveness trials revealed that a key dissemination barrier is that many schools do not have clinicians available to deliver prevention programs, whether in person or via the Internet. We believed a dissonance-based Internet prevention program could be more effective because it would (a) use empirically supported dissonance-induction procedures to reduce an established eating disorder risk factor, (b) be informed by qualitative input we have received over 12 years from hundreds of participants and dozens of facilitators regarding how to improve the dissonance-inducing activities, (c) be interactive, which is associated with larger effects for eating disorder prevention programs (Stice, Shaw, & Marti, 2007b), and (d) tap into a wellspring of perceived injustice about how our culture expects women to conform to this unrealistic beauty ideal. A meta-analytic review found that Internet interventions are more likely to produce strong effects if they focus on body image, avoid educational material, and are interactive (Barak et al., 2008), which also suggests that our intervention would be effective, as it included a focus on each of these elements. Given that youth are deeply immersed in the computer culture and the Internet is a source of pro-thin-ideal images and messages, we believe it is time to utilize this medium to extend the reach of the efficacious dissonance-based eating disorder prevention program.
Accordingly, we developed a prototype of an Internet version of the Body Project and evaluated it in a preliminary trial. We based the new Internet intervention (eBody Project) on the new enhanced-dissonance version of the Body Project (Stice et al., 2011b), which is producing effects that are larger than those observed in the high school effectiveness trial that used the original Body Project program (Stice et al., 2006) and four times larger than the average effect for eating disorder prevention programs observed in a meta-analytic review (Stice et al., 2007b). In addition to preserving the activities and therapeutic elements from the enhanced-dissonance program, we included additional dissonance-inducing activities that should contribute to even larger effects.
This preliminary trial compared the eBody Project to an educational brochure control condition because most colleges provide this minimal intervention (Mann et al., 1997) and this allowed us to benchmark the effects from this trial against the effects from Body Project groups delivered by school counselors in our effectiveness trials that used this control condition (Stice et al., 2009, 2011). We also compared the eBody Project to an educational video that provides information on body image and eating disorders, which is a more rigorous active comparison condition than used in past trials of an Internet eating disorder prevention programs. More critically, we compared the eBody Project to the group version of the Body Project, which is the eating disorder prevention program that has produced the largest effects of any eating disorder prevention program evaluated to date. Aim 1 was to test whether the eBody Project would produce significantly larger reductions in eating disorder risk factors and symptoms relative to the educational video and brochure control conditions. Aim 2 was to test whether the eBody Project produced reductions in outcomes0 that were similar to the reductions observed for the group Body Project conducted by college counselors, which was also expected to produce larger effects than the educational video and brochure control conditions. Aim 3 was to benchmark the magnitude of the intervention effects of the eBody Project against effects for the Body Project from our efficacy trial with high school and college students (Stice et al., 2006), our effectiveness trial with high-school students (Stice et al., 2009), our effectiveness trial with college students (Stice et al., 2011b), and sorority-led groups with college students (Becker et al., 2010; Parez et al., 2010).
Methods
Participants and Procedure
Participants were 107 young women (M age = 21.6, SD = 6.6) recruited from a local university with a mean body mass index (BMI = kg/m2) of 23.7 (SD = 4.3). We focused on college-aged women because the peak period of risk for eating disorder onset occurs during late adolescence and because women are at much higher risk for eating disorders than men (Hudson, Hiripi, Pope, & Kessler, 2007; Stice et al., 2009a). We targeted female students with body image concerns because a meta-analytic review indicated that prevention programs targeting high-risk individuals produce larger effects than those offered universally (Stice et al., 2007b). Young women with body image concerns are at increased risk for future escalation of eating disorder symptoms and onset of eating disorders (e.g., Johnson & Wardle, 2005; Killen et al., 1996). The sample was 7% American Indian/Alaska Native, 12% Asian, 1% African American, 2% Native Hawaiian/Pacific Islander, and 78% European American, which was a slightly more diverse sample than the city from which we sampled (1% American Indian/Alaska Native, 5% Asian, 1.5% African American, 0.2% Native Hawaiian/Pacific Islander, and 86% European American, 4% mixed racial heritage). Parental education, a proxy for socioeconomic status, was 17% high school graduate or less, 18% some college, 38% college graduate, and 27% graduate or professional degree, which was somewhat higher than the education of adults in the city (27% high school graduate or less; 25.7% some college; 21.9% college graduate; 17.2% graduate or professional degree).
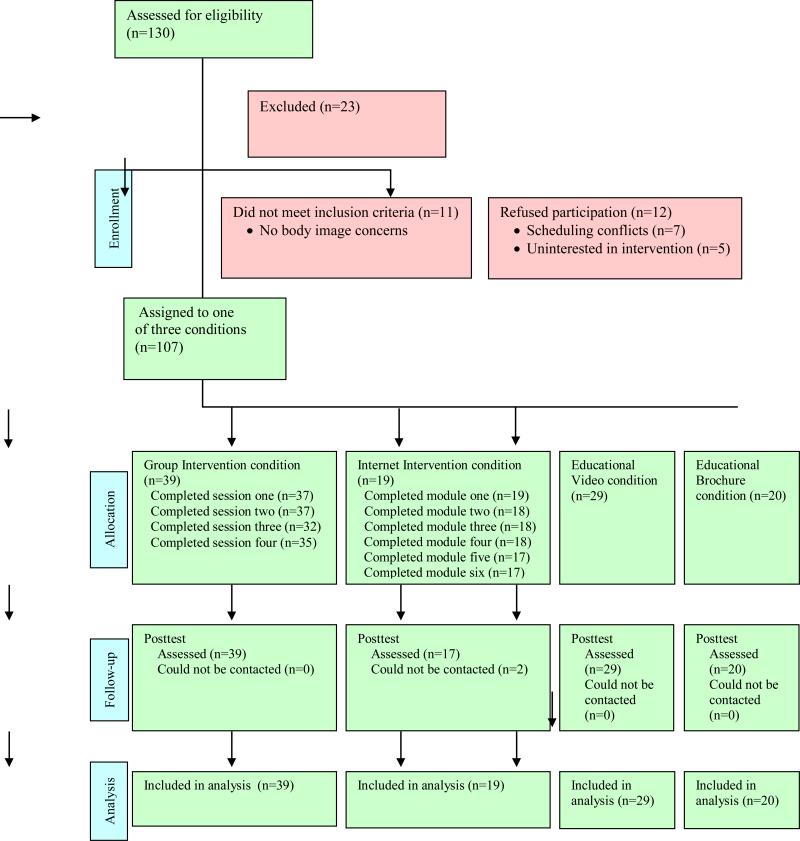
Participants were recruited using email messages and posters inviting female students with body image concerns to participate in a study evaluating various body acceptance interventions. We provided clinicians from the university Psychology Clinic with the recruitment materials; they were responsible for sending the email invitations and hanging the posters. Participants had to verbally affirm that they had body image concerns during a phone call conducted by research staff to schedule the baseline assessment. The sole exclusion criterion was meeting criteria for current DSM-IV anorexia nervosa, bulimia nervosa, or binge eating disorder. Figure 1 provides information on participant flow through this trial.
Figure 1.
Participant Flow Chart
Participants were randomly assigned to the eBody Project intervention, the group Body Project intervention, an educational video control condition, or an educational brochure control condition. More participants were randomized to the Body Project condition than the other conditions because this pilot study was an add-on to the college effectiveness trial of the group intervention (Stice et al., 2011b). Participants provided interview and survey data at pretest and posttest (intervention termination), which occurred 4-6 weeks after the baseline assessment. Female assessors, who had at least a bachelor's degree in psychology, were blinded to the condition of participants. Assessors attended 24 hours of training, wherein they received instruction in interview skills, reviewed diagnostic criteria for relevant disorders, observed simulated interviews, and role-played interviews. They also attended annual training workshops. They had to demonstrate high inter-rater agreement (kappa [k] > .80) with supervisors using 12 tape-recorded interviews conducted with individuals with and without eating disorders before collecting data. Weekly consensus meetings were held to resolve ambiguous diagnostic issues. Participants were paid $30 for completing the baseline assessment and $35 for the posttest assessment, but were not compensated for completing the Body Project or eBody Project interventions or for viewing the educational video or reading the educational brochure. Participants provided consent for this Institutional Review Board-approved project.
eBody Project
Participants were asked to complete six modules in which they engage in written and behavioral activities designed to critique the thin-ideal over the course of three weeks. Each module took between 30-40 minutes to complete, which kept the total intervention time similar to the 240-minute duration of the group dissonance intervention. We designed the prototype modules to last approximately 35 minutes because this is approximately the average amount of time women typically spend playing videogames per session (Winn & Heeter, 2009). Each module included one user-driven self-education exercise, one contest designed to promote accountability for thin-ideal perspectives (creating and adding to a user profile page with links to posted material from the user), and one off-line exercise, all of which are designed to induce dissonance regarding pursuing the thin-ideal. Table 1 provides the content of each module and details how we preserved virtually all elements of the group-based dissonance intervention. One new feature of the eBody Project is that participants earn points (“Body Project Bucks”) for completing assignments that can be used to purchase small products (e.g., water bottles, coffee mugs, shirts) that contained the Body Project logo at the end of the program. The prototype eBody Project does not contain the educational videogames that we plan to develop. To minimize cost and facilitate dissemination, we developed a stand-alone intervention that did not involve moderated interaction with a clinician or require monitoring.
Table 1.
| Content of Group Body Project | Content of eBody Project |
|---|---|
| Introduction and overview (Sessionl [S1]) | Introduction and overview (Module1 [M1]) |
| Voluntary commitment (at start of every session) | Voluntary commitment (at start of every module) |
|
Definition of the thin-ideal (S1) Participants select magazine pictures of models; discuss definition and history of the thin-ideal. |
Definition of the thin-ideal: Online self-education (M1) Users select images of models and questions about the definition and history of the thin-ideal are posed. |
|
Costs of pursuing the thin-ideal (S1) Participants generate costs of pursuing the thin-ideal; identify who benefits from the ideal. |
Costs of pursuing the thin-ideal: Online contest (M1-2) Users generate top-10 list of costs of pursuing the thin-ideal, post online in M2, and vote for best list; winners receive BP bucks. |
|
Trivial pursuit: Online self-education (M1) Usersplay multiple-choice trivia game to learn the symptoms and costs of eating disorders, earning BP bucks for correct answers. |
|
|
Letter to younger girl (S1-2) Users write a letter to a younger girl about the costs of the thin-ideal; letter is read aloud to the group and videotaped with an option to post it online. |
Letter to younger girl: Offline exercise (M1-2) Users write a letter to a younger girl about the costs of the thin-ideal, post the letter or a video of themselves reading the letter online, and vote for the best posting; winners receive BP bucks. |
|
Role-play to discourage pursuit of thin-ideal (S2) Participants take turns dissuading the facilitator (posing as a dieter or eating disordered individual) from pursing thin-ideal. |
Discouraging the thin-ideal: Online self-education (M2) Users argue someone out of pursuing the thin-ideal through a virtual texting interchange. |
|
Costs of eating disorders: Online exercise (M2) Users write a story about someone with an eating disorder, post the story, and vote for the best story; winners receive BP bucks. |
|
|
Mirror self-affirmation exercise (S1-2) Participants stand in front of mirror and write down positive qualities about themselves; read their list aloud to group. |
Mirror mirror on the wall: Offline exercise (M2-3) Users stand in front of mirror, write positive features, post online, vote for best posting; winners receive BP bucks. |
|
Quick comebacks to thin-ideal statements (S3) Role-play wherein participants challenge thin-ideal statements made by facilitators, generating anti-thin- ideal comebacks. |
Challenging thin-ideal quips: Online self-education (M3) Users generate quick comebacks to thin-ideal statements and earn BP bucks for quick responses. |
|
Top-10 body activism list home exercise (S2) Participants create top-10 list of things women can do to resist thin-ideal. |
Body activism: Online self-education (M3) Users make top-10 lists of body activism activities, earning BP bucks for each idea. |
|
Body activism home exercise (S3-4) Participants do at least one body activism activity on their own, sharing results with the group. |
Body activism: Online self-education (M3-4) Users do at least one body activism activity and post written or video report online, vote on others’ posting; winners received BP bucks. |
|
Verbal challenges home exercise (S2-3) Participants pick three real-life examples of pressures to be thin and create a verbal challenge to each pressure. Participants read to the group and are videotaped. |
Rewind response letter: Offline exercise (M4) Users write letter to someone who said hurtful thin-ideal comment to them and how they could have responded; users are encourage to respond in an assertive manner in the future to such comments. |
|
Self-affirmation exercise (S4) Participants make commitment to engage in some sort of self-affirmation exercise with a friend, sibling, etc. |
Self-affirmation exercise: Offline exercise (M4) Users generate 5 self-affirmation exercises and commit to engage in them with a friend, sibling, etc. |
|
Behavioral challenge (S3-4) Participants asked to do something they normally wouldn't do because of body image concerns (e.g., wear shorts) and write a brief report to the group of how it went. |
Behavioral challenge: Offline exercise (M4-5) Users asked to do something that they normally wouldn't do because of body image concerns, post a brief written/video report online, vote for best report; winners receive BP bucks. |
|
Letter to younger girl (S4) Participants write letter to a younger girl about ways to avoid body image concerns and send to facilitator via email. |
Helping the next generation letter: Offline exercise (M5-6) Users write letter to a younger girl about avoiding body image concerns, post the letter or video, vote on best posting; winners receive BP bucks. |
|
Anti-thin ideal commercial: Offline exercise (M5-6) Users make short, 1-2 minute commercials and post them online, vote on best commercial; winners receive BP bucks. |
|
|
Challenging fat talk (S4) Participants get a list of subtle thin-ideal statements and discuss how this promotes the thin-ideal and ways to stop this. |
|
|
Future pressures to be thin (S4) Participants provide examples of future pressures to follow the thin-ideal and how they will respond to them. |
Planning ahead: Online self-education (M6) Circumstances that can cause body image concerns are presented (e.g., senior prom) and users develop a response plan for each. |
|
Passing along the wisdom: Offline exercise (M6) Users are asked to talk to a real person about the program and tell this person what they learned (e.g., a friend or parent). |
Note: S stands for session (e.g., session 1) and M stands for module (e.g., module 1).
Body Project
Participants voluntarily engaged in verbal, written, and behavioral exercises in which they critiqued the thin-ideal ideal during four 1-hour group sessions held on a weekly basis and in home exercises. For example, participants wrote a counter-attitudinal essay about the costs associated with pursuing the thin-ideal, engaged in a counter-attitudinal role-play in which they attempted to dissuade facilitators from pursuing the thin-ideal, and engaged in one self-selected form of body activism that challenged the thin-ideal outside of the sessions. Groups typically contained 7-9 participants. Pairs of clinicians from the university Psychology Clinic delivered the intervention. A scripted manual was used for the Body Project intervention. Facilitator training involved reading the manual to become familiar with the intervention, and attending a 4-hour workshop to learn the conceptual rationale and supporting evidence for the intervention, discuss and role-play key elements from the sessions, and discuss process issues (e.g., making referrals). Sessions were video-recorded and reviewed by Drs. Rohde and Shaw for general guidance in competence and adherence to the scripted manual. Group facilitators received supervision based on the video-recordings during delivery of the first two groups conducted by facilitator pairs. Fifty percent of the video-recorded sessions were rated for fidelity and competence.
Educational video condition
Participants were asked to view Dying to be Thin, a 55-min documentary on eating disorders, body dissatisfaction, and body acceptance. Topics include the cultural pressures to be thin, physical and emotional consequences of subscribing to this ideal, and treatment/recovery from life-threatening eating disorders, which are covered through presentations from experts and the personal stories of survivors of eating disorders. Participants were sent the link to a web page where they could view the video at no cost.
Educational brochure control condition
Participants received a 2-page brochure produced by the National Eating Disorders Association in 2002 which describes negative and positive body image, notes that negative body image is associated with increased risk for onset of eating disorders, and offers 10 steps for achieving a positive body image. Control participants were mailed the educational brochures after randomization, which occurred after the baseline assessment. Participants were referred to treatment if they met criteria for threshold or subthrehold anorexia nervosa, bulimia nervosa, or binge eating disorder at posttest (as were participants in the other conditions).
Measures
Thin-ideal internalization
The Ideal-Body Stereotype Scale-Revised assessed thin-ideal internalization (Stice et al., 2006). Items used a response format ranging from 1 = strongly disagree to 5 = strongly agree and were averaged for this scale and those described below. This scale has shown internal consistency (α = .91), 2-week test-retest reliability (r = .80), predictive validity for bulimic symptom onset, and sensitivity to detecting intervention effects (Stice et al., 2006; α = .78 at pretest).
Body dissatisfaction
Items from the Satisfaction and Dissatisfaction with Body Parts Scale (Berscheid, Walster, & Bohrnstedt, 1973) assessed dissatisfaction with nine body parts using a response scale ranging from 1 = extremely satisfied to 6 = extremely dissatisfied. This scale has shown internal consistency (α = .94), 3-week test-retest reliability (r = .90), predictive validity for bulimic symptom onset, and sensitivity to detecting intervention effects (Stice et al., 2006; α = .91 at pretest).
Dieting
The Dutch Restrained Eating Scale (DRES; van Strien, Frijters, van Staveren, Defares, & Deurenberg, 1986) assesses the frequency of various dieting behaviors using a response scale ranging from 1 = never to 5 = always. The DRES has shown internal consistency (α = .95), 2-week test-retest reliability (r = .82), convergent validity with self-reported caloric intake (but not objectively measured caloric intake), predictive validity for bulimic symptom onset, and sensitivity to detecting intervention effects (Stice, Sysko, Roberto, & Allison, 2010; Stice et al., 2006; van Strien et al., 1986; α = .92 at pretest).
Negative affect
The 21-item Beck Depression Inventory (BDI, Beck et al., 1988) assessed negative affect using a response scale ranging from no symptoms (0) to severe symptoms (2). The BDI has shown internal consistency (α = .73-.95), test-retest reliability (r = .60-.90), and convergent validity with clinician ratings of depressive symptoms (M r = .75; Beck et al., 1988; α = .94 at pretest).
Eating pathology
The Eating Disorder Diagnostic Interview assessed DSM-IV eating disorder symptoms. Items assessing symptoms in the past month were summed to form an overall eating disorder symptom composite. This composite has shown internal consistency (α = .92), 1-week test-retest reliability (r = .90), inter-rater agreement (ICC r = .93), sensitivity to detecting effects of eating disorder prevention and treatment interventions, and predictive validity for future onset of depression (Burton & Stice, 2006; Stice et al., 2009b).
Results
Preliminary Analyses
Participants in the four conditions did not significantly differ on demographic factors or outcome measures at pretest. Only two participants from the Internet intervention condition (1.8%) did not complete the posttest assessment, making it unlikely that attrition biased results. Nonetheless, we used the last-observation-carried-forward approach, in which the pretest values of the outcomes were entered for the missing posttest scores, which conservatively assumes that the two participants who dropped did not show improvements on outcomes. Acceptability of the Internet prototype was high, with 17/19 users (89%) completing all 6 modules (1 completed 2 modules and 1 completed 5). User logs indicated that the average time to complete the sessions was 27 minutes, which was slightly less than anticipated. A total of 31/39 participants (79%) in the group condition attended all 4 sessions, 18% attended 3 sessions, and 3% attended 1 session. If a participant missed a session, a brief (10-15 minute) individual session was conducted to review missed material when possible. Of the 8 participants who missed one or more session, 5 completed a make-up session. Facilitators closely adhered to the intervention manual and were mostly competent in their delivery of the program. Implementation fidelity ratings (1-10 scale) had a mean of 7.8 (SD = 0.85; range = 5 – 9; only 3% of the components had less than “fair” adherence, defined as a score of 5 or less). Facilitator competence ratings (10-point scale) had a mean of 7.3 (SD = 0.94; range = 4 – 9; 12% of items were rated less than “good/average” competence, defined as a score of 5 or less). With regard to the educational video control condition, 25 of 29 (83%) participants assigned to the video condition reported watching half or more of the video (76% watched all).
The condition by time interaction from an omnibus repeated measures MANOVA model confirmed that change in the outcomes over time differed across all four conditions (F [15,303] = 1.99, p = .016). Follow-up repeated measures ANOVA models tested whether there were differential changes in outcomes across each pair of conditions from pre-to-post (condition was a 2-level between-subjects factor and time was a 2-level within-subject factor). Table 1 provides Ms and SDs for all outcomes across time points and conditions. Table 2 provides the effect sizes and significance levels for each contrast comparing the four conditions.
Table 2.
Means and standard deviations for outcomes from the four conditions at pretest and posttest
| Thin-ideal internalization | Body dissatisfaction | Dieting | Negative affect | Eating disorder symptoms | |
|---|---|---|---|---|---|
| eBody Project | M (SD) | M (SD) | M (SD) | M (SD) | M (SD) |
| Pretest | 3.75 (0.50) | 3.23 (0.56) | 2.62 (0.82) | 10.32 (5.24) | 8.84 (7.62) |
| Posttest | 3.37 (0.60) | 2.78 (0.78) | 2.04 (0.83) | 6.00 (5.40) | 5.95 (4.54) |
| Body Project | |||||
| Pretest | 3.83 (0.42) | 3.44 (0.74) | 2.72 (0.93) | 13.90 (10.68) | 12.92 (13.96) |
| Posttest | 3.47 (0.53) | 2.88 (0.89) | 2.17 (0.98) | 9.21 (10.40) | 6.90 (8.37) |
| Brochure controls | |||||
| Pretest | 3.88 (0.43) | 3.26 (0.65) | 2.68 (0.72) | 11.65 (6.24) | 10.20 (7.19) |
| Posttest | 3.84 (0.52) | 3.33 (0.66) | 2.57 (0.88) | 10.95 (7.48) | 10.25 (11.02) |
| Video controls | |||||
| Pretest | 3.79 (0.51) | 3.17 (0.87) | 2.52 (0.93) | 9.24 (7.36) | 7.48 (7.75) |
| Posttest | 3.68 (0.54) | 3.01 (0.86) | 2.30 (1.01) | 7.78 (6.98) | 5.66 (6.34) |
Time x condition interactions indicated that there were significantly greater pre-to-post reductions for eBody Project participants versus brochure controls for body dissatisfaction (d = 1.32, p < .001), dieting (d = .69, p = .04), and negative affect (d = .72, p = .04). The effect for thin-ideal internalization was marginal (d = .63, p = .07) and the effect for eating disorder symptoms did not reach significance (d = .39, p = .25). eBody Project participants also showed significantly greater reductions than video controls for dieting (d = .63, p = .04) and marginally greater reductions in body dissatisfaction (d = .55, p = .07), but not for thin-ideal internalization (d = .51, p = .09), negative affect (d = .46, p = .13), or eating disorder symptoms (d = .22, p = .47).
Body Project participants showed significantly greater pre-to-post reductions than brochure controls for thin-ideal internalization (d = .67, p = .01), body dissatisfaction (d = 1.25, p < .001), dieting (d = .60, p = .03), and eating disorder symptoms (d = .57, p = .04); the effect for negative affect was marginal (d = .51, p = .06). Body Project participants also showed significantly greater reductions than video controls for thin-ideal internalization (d = .54, p = .03), body dissatisfaction (d = .72, p < .01), dieting (d = .54, p = .03), and eating disorder symptoms (d = .49, p =.05); the effect for negative affect was marginal (d = .42, p = .09).
Reductions in outcomes did not differ for Body Project versus eBody Project participants for thin-ideal internalization (d = -.06, p = .85), body dissatisfaction (d = -.19, p = .47), dieting (d = -.01, p = .87), negative affect (d = -.06, p = .87), or eating disorder symptoms (d = -.31, p = .25). Likewise, there were no significant differences in outcomes for brochure versus video controls for thin-ideal internalization (d = .20, p = .49), body dissatisfaction (d = .46, p = .12), dieting (d = .17, p = .57), negative affect (d = .14, p = .64) or eating disorder symptoms (d = .29, p = .33).
We next benchmarked the effect sizes from the eBody Project and Body Project to parallel effect sizes for the Body Project from an efficacy trial conducted by research-based clinicians with both high school and college students (Stice et al., 2006), effectiveness trials conducted by school-based clinicians with high school (Stice et al., 2009b) and college students (Stice et al., 2011b), and two trials evaluating sorority-led dissonance groups with college students (Becker et al., 2010; Perez et al., 2010). Because two of the trials did not have a control condition (Becker et al., 2010; Perez et al., 2010), we first calculated a within-condition measure of change from pretest to posttest (d = [posttest intervention M – pretest intervention M) / pretest intervention SD]) so that we could compare effects across all trials using a parallel effect size. These effects are presented in the upper half of Table 4. The average within-condition effect size for eBody Project was slightly smaller than the average Body Project effects for the efficacy trial, but larger than the Body Project effects in the current trial, the two effectiveness trials, and the two sorority-led trials. The average within-condition effect for the group Body Project in the current report was smaller than for the efficacy trial and college effectiveness trial, but larger effects than the high school effectiveness trial and the two sorority-led trials.
Table 4.
Comparison of Effect Sizes (Cohen's d) reflecting baseline to posttest change for the eBody Project and Body Project intervention in the present trial relative to the Efficacy Trial, a High School Effectiveness Trial, and College Effectiveness Trial, and two Sorority-led Trials.
| Thin-ideal internalization | Body dissatisfaction | Dieting | Negative affect | Eating disorder symptoms | M effect size | |
|---|---|---|---|---|---|---|
| Pre to post within subjects comparison* | ||||||
| eBody Project | 0.76 | 0.80 | 0.71 | 0.82 | 0.38 | 0.69 |
| Body Project | 0.86 | 0.76 | 0.59 | 0.44 | 0.43 | 0.62 |
| Efficacy trial (Stice et al., 2006) | 1.24 | 0.72 | 0.80 | 0.73 | 0.60 | 0.82 |
| High School Effectiveness trial (Stice et al., 2009b) | 0.71 | 0.52 | 0.62 | 0.50 | 0.47 | 0.56 |
| College Effectiveness trial (Stice et al., 2011b) | 0.76 | 0.85 | 0.73 | 0.54 | 0.51 | 0.68 |
| Sorority-led groups Perez et al., 2010 | 0.61 | 0.37 | 0.29 | N/A | 0.22 | 0.37 |
| Sorority-led groups Becker et al., 2010 | 0.79 | 0.46 | 0.56 | 0.45 | 0.47 | 0.55 |
| Intervention condition vs. brochure control condition | ||||||
| eBody Project | 0.63 | 1.32 | 0.69 | 0.72 | 0.39 | 0.75 |
| Body Project | 0.67 | 1.25 | 0.60 | 0.51 | 0.57 | 0.72 |
| Efficacy trial (Stice et al., 2006) | 0.82 | 0.75 | 0.56 | 0.49 | 0.34 | 0.59 |
| High School Effectiveness trial (Stice et al., 2009b) | 0.43 | 0.58 | 0.41 | 0.24 | 0.49 | 0.43 |
| College Effectiveness trial (Stice et al., 2011b) | 0.79 | 0.86 | 0.75 | 0.57 | 0.50 | 0.69 |
Note: Effect sizes were calculated as d = (post M- baseline M) / SD (baseline)
Our second method of benchmarking compared effect sizes that reflect the degree of change in the outcome from pre-to-post for eBody Project or Body Project participants versus brochure control participants (d = [posttest intervention M – pretest intervention M] – [posttest control M – pretest control M] / pretest control SD); these effect sizes are presented in the lower half of Table 4. The average between-condition effect for the eBody Project was similar to the parallel effect from the group Body Project intervention in the current report and the effects from the efficacy trial and both effectiveness trials. The average between-condition effect for the group Body Project in the current report was larger than for the efficacy trial and high school efficacy trial, but similar to the college effectiveness trial.
Discussion
The present trial provided encouraging initial data that suggest that the new eBody Project eating disorder prevention program resulted in significantly greater reductions in body dissatisfaction, self-reported dieting, and negative affect relative to educational brochure controls. However, the fact that this intervention only produced a moderate reduction in thin-ideal internalization and eating disorder symptoms relative to brochure controls, which did not reach significance in this preliminary trial, suggests that it will be important to enhance the efficacy of this intervention before conducting a fully powered prevention trial. The eBody Project intervention also produced significant reductions in self-reported dieting compared to educational video controls, but not for thin-ideal internalization, body dissatisfaction, negative affect, or eating disorder symptoms, implying that the video control condition was more effective at reducing eating disorder risk factors than the brochure control condition. Participants in the enhanced-dissonance Body Project group intervention showed significantly greater reductions than educational brochure controls for thin-ideal internalization, body dissatisfaction, self-reported dieting, and eating disorder symptoms, with a marginal effect for negative affect. Likewise, participants in the enhanced dissonance Body Project group showed significantly greater reductions in thin-ideal internalization, body dissatisfaction, dieting, and eating disorder symptoms, again with a marginal effect for negative affect. It was noteworthy that the enhanced-dissonance group Body Project did not produce significantly different reductions in outcomes relative to the eBody Project (M d = -.13).
Benchmarking indicated that the average between-condition effect size for the eBody Project (M d = .75) compared favorable to the parallel effects for the enhanced group Body Project intervention from the present trial (M d = .72), as well as the average effects from the original dissonance group intervention from the large efficacy trial (M d = .59; Stice et al., 2008), the high school effectiveness trial (M d = .43; Stice et al., 2009), and the college effectiveness trial (M d = .69; Stice et al., 2011b). The benchmarking comparisons of the within-condition effect sizes similarly suggest that the effects from the eBody Project compare favorably to the effects from our past effectiveness and efficacy trials, as well as with those observed in the sorority-led groups (M d = .37, Perez et al., 2010; M d = .55, Becker et al., 2010). The average effect for the eBody Project intervention (M d = .75) also compare favorably to the average pre-post effects for Student Bodies (M d = .22; Celio et al., 2000; Low et al., 2006; Taylor et al., 2006; Winzelberg et al., 1998, 2000; Zabinski et al., 2001, 2004). In addition, the average effect for the eBody Project intervention was considerably larger than the average pre-post effects from a meta-analytic review of eating disorder prevention programs (M d = .13; Stice et al., 2007b).
Also of note, the average effects for the enhanced-dissonance Body Project group intervention (M d = .72) compare favorably to parallel effects for the original dissonance group intervention from our large efficacy trial (M d = .59; Stice et al., 2006) and a high school effectiveness trial (M d = .43; Stice et al., 2009). The average effect for the enhanced-dissonance Body Project was similar to the average effect from the full college effectiveness trial (M d = .69), which is also using the new enhanced-dissonance intervention. This pattern of findings suggests that the new enhanced dissonance group intervention should be used in future effectiveness trials and dissemination efforts.
We also collected qualitative feedback from participants who completed the eBody Project to learn what they liked most and least about this intervention and how it could be improved. Over half of the participants reported liking the eBody Project program either “very much” or “pretty much”. The Body Project Bucks and consequent ability to purchase Body Project products proved popular, with most participants liking the products. Although participants reported enjoying the social networking component of this intervention, half of the participants did not use this element of the intervention. Finally, the majority of participants reported feeling that completing the online program helped them meet most of their goals regarding body acceptance, although a few reported feeling unsure about this question. Participants also reported that the program made them feel more positive about themselves (e.g., “It really helped me to feel more comfortable with my body and who I am”). Some participants reported that they did not like the more difficult “offline projects”. Participants suggested making the exercises less repetitive and introducing a greater variety of activities. They also encouraged us to develop video games to make the intervention more engaging, which was precisely our plan.
Limitations
Although this trial improved upon many prior prevention trials by using random assignment and blinded diagnostic interviews, it is important to consider the study limitations. First, the sample size per condition in this preliminary trial was small. Results need to be replicated with a larger sample. Second, this trial examined only pre-to-post effects. Although this limitation prevented us from comparing the duration of intervention effects, this seemed reasonable for a preliminary trial given that past efficacy and effectiveness trials have confirmed that this brief intervention produces effects that persist through 3-year follow-up (Stice et al., 2008, 2011c). Nonetheless, it will be important to conduct an evaluation of the complete eBody Project intervention in a trial with long-term follow-up once it is fully developed. Third, the sample was relatively homogeneous with regard to ethnicity and socioeconomic status, suggesting that care should be taken in generalizing the results to more diverse populations. However, the Body Project has produced similar effects for Latino, Asian, and European American participants (Rodriguez, Marchand, Ng, & Stice, 2008). Fourth, it will be important to determine whether the eBody Project intervention is effective for high-school aged adolescent females, as they too represent a population at elevated risk for eating pathology.
Implications for Prevention and Future Research
Results suggest that the new Internet-based eBody Project was able to use dissonance-induction procedures to reduce pursuit of the thin-ideal and achieve significant reductions in eating disorder risk factors, implying that it is possible to use the public accountability inherent to the Internet to motivate a reduction in an attitudinal risk factor for eating pathology. Results suggest that the eBody Project has the potential of overcoming difficulties related to identifying school clinicians who can delivery the group-based intervention in a competent fashion and on a enduring basis. The findings from this preliminary trial imply that it would be valuable to complete development of the eBody Project and then conduct a fully powered effectiveness trial relative to the group-based Body Project intervention and a relevant control condition. Future dissemination studies could therefore offer both versions of the intervention to young women with body image concerns to investigate which is more acceptable and more efficacious, as well as investigate individual difference factors that identify participants for whom one or the other intervention is superior in these dimensions. We have used direct recruitment efforts, such as mass mailings, mass email messages, and posters placed at schools, wherein young women with self-identified body image concerns elect to enroll in our prevention trials, which has typically resulted in 7% to 14% of female students at particular high schools or colleges participating in our trials. However, it might be useful to explore alternative recruitment strategies, such as conducting screenings for body image concerns in required health classes or using a FaceBook recruitment page, which might allow delivery of this program to even more young women who could benefit from this intervention. Large-scale evaluations of the eBody Project intervention should also investigate whether degree of utilization of the various components (e.g., using the social networking element and posting of anti-thin-ideal exercise) predicts the magnitude of reductions in the outcomes. With continued refinements based on future randomized trials and qualitative input from participants, we hope to develop an even more effective Internet-based eating disorder prevention program, which has the potential to dramatically extend the reach of this empirically supported intervention and reduce the population prevalence of eating disorders.
Table 3.
Effect sizes (d) and significance levels for by the time x condition interactions in repeated measures ANOVA models comparing the conditions
| Pre to post | Thin-ideal internalization | Body dissatisfaction | Dieting | Negative affect | Eating disorder symptoms | M effect sizes |
|---|---|---|---|---|---|---|
| eBody Project vs. brochure control | 0.63 (p=.07) | 1.32 (p=.000) | 0.69 (p=.04) | 0.72 (p=.04) | 0.39 (p=.25) | 0.75 |
| Body Project vs. brochure control | 0.67 (p=.01) | 1.25 (p<.001) | 0.60 (p=.03) | 0.51 (p=.06) | 0.57 (p=.04) | 0.72 |
| eBody Project vs. video control | 0.51 (p= .09) | 0.55 (p=.07) | 0.63 (p=.04) | 0.46 (p=.13) | 0.22 (p=.47) | 0.47 |
| Body Project vs. video control | 0.54 (p=.03) | 0.72 (p=.005) | 0.54 (p=.03) | 0.42 (p=.096) | 0.49 (p=.05) | 0.54 |
| eBody Project vs. Body Project | -0.06 (p=.85) | -0.19 (p=.47) | -0.01 (p=.87) | -0.06 (p=.87) | -0.31 (p=.25) | -0.13 |
| Video vs. brochure controls | 0.20 (p=.49) | 0.46 (p=.12) | 0.17 (p=.57) | 0.14 (p=.64) | 0.29 (p=.33) | 0.25 |
Acknowledgments
This study was supported by grants (MH70699, MH86582) from the National Institutes of Health.
We thank the college clinicians, Allison Waters, Rosemary Bernstein and Amber Thalmayer for delivering the Body Project intervention; Danny Decker, Andrew Puddifoot, and Cody Galloway from Harlow Interactive for developing the eBody Project intervention; and the participants who made this study possible.
Footnotes
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at www.apa.org/pubs/journals/ccp
References
- Andersson G, Cuijpers P. Internet-based and other computerized psychological treatments for adult depression: A meta-analysis. Cognitive Behaviour Therapy. 2009;38:196–205. doi: 10.1080/16506070903318960. [DOI] [PubMed] [Google Scholar]
- Arcelus J, Mitchell A, Wales J, Nielsen S. Mortality rates in patients with anorexia nervosa and other eating disorders: A meta-analysis of 36 studies. Archives of General Psychiatry. 2011;68:724–731. doi: 10.1001/archgenpsychiatry.2011.74. [DOI] [PubMed] [Google Scholar]
- Barak A, Hen. L, Boniel-Nissim M, Shapira N. A comprehensive review and meta-analysis of the effectiveness of Internet-based psychotherapeutic interventions. Journal of Technology in Human Services. 2008;26:109–160. [Google Scholar]
- Beck AT, Steer RA, Garbin MG. Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. Clinical Psychology Review. 1988;8:77–100. [Google Scholar]
- Becker C, Wilson C, Williams A, Kelly M, McDaniel L, Elmquist J. Peer-facilitated cognitive dissonance versus healthy weight eating disorders prevention: A randomized comparison. Body Image. 2010;7:280–288. doi: 10.1016/j.bodyim.2010.06.004. [DOI] [PubMed] [Google Scholar]
- Becker CB, Bull S, Schaumberg K, Cauble A, Franco A. Effectiveness of peer-led eating disorders prevention: A replication trial. Journal of Consulting and Clinical Psychology. 2008;76:347–354. doi: 10.1037/0022-006X.76.2.347. [DOI] [PubMed] [Google Scholar]
- Becker CB, Smith L, Ciao AC. Reducing eating disorder risk factors in sorority members: A randomized trial. Behavior Therapy. 2005;36:245–254. [Google Scholar]
- Becker CB, Smith LM, Ciao AC. Peer facilitated eating disorders prevention: A randomized effectiveness trial of cognitive dissonance and media advocacy. Journal of Counseling Psychology. 2006;53:550–555. [Google Scholar]
- Berscheid E, Walster E, Bohrnstedt G. The happy American body: A survey report. Psychology Today. 1973;7:119–131. [Google Scholar]
- Burton E, Stice E. Evaluation of a healthy-weight treatment program for bulimia nervosa: a preliminary randomized trial. Behaviour Research and Therapy. 2006;44:1727–1738. doi: 10.1016/j.brat.2005.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Celio AA, Winzelberg AJ, Wilfley DE, Eppstein-Herald D, Springer EA, Dev P, Taylor C. Reducing risk factors for eating disorders: Comparison of an Internet- and a classroom-delivered psychoeducational program. Journal of Consulting and Clinical Psychology. 2000;68:650–657. [PubMed] [Google Scholar]
- Crow SJ, Peterson CB, Swanson SA, Raymond NC, Specker S, Eckert ED, Mitchell JE. Increased mortality in bulimia nervosa and other eating disorders. American Journal of Psychiatry. 2009;166:1342–1346. doi: 10.1176/appi.ajp.2009.09020247. [DOI] [PubMed] [Google Scholar]
- Green M, Scott N, Diyankova I, Gasser C, Pederson E. Eating disorder prevention: An experimental comparison of high level dissonance, low level dissonance, and no-treatment control. Eating Disorders. 2005;13:157–169. doi: 10.1080/10640260590918955. [DOI] [PubMed] [Google Scholar]
- Hudson J, Hiripi E, Pope H, Kessler R. The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biological Psychiatry. 2007;61:348–358. doi: 10.1016/j.biopsych.2006.03.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson F, Wardle J. Dietary restraint, body dissatisfaction, and psychological distress: A prospective analysis. Journal of Abnormal Psychology. 2005;114:119–124. doi: 10.1037/0021-843X.114.1.119. [DOI] [PubMed] [Google Scholar]
- Killen J, Taylor C, Hayward C, Haydel K, Wilson D, Hammer L, Strachowski D. Weight concerns influence the development of eating disorders: A 4-year prospective study. Journal of Consulting and Clinical Psychology. 1996;64:936–940. doi: 10.1037//0022-006x.64.5.936. [DOI] [PubMed] [Google Scholar]
- Low KG, Charanasomboon S, Lesser J, Reinhalter K, Martin R, Jones H, et al. Effectiveness of a computer-based interactive eating disorder prevention program at long-term follow-up. Eating Disorders. 2006;14:17–30. doi: 10.1080/10640260500403816. [DOI] [PubMed] [Google Scholar]
- Mann T, Nolen-Hoeksema S, Huang K, Burgard D, Wright A, Hanson K. Are two interventions worse than none? Joint primary and secondary prevention of eating disorders in college females. Health Psychology. 1997;16:215–225. doi: 10.1037//0278-6133.16.3.215. [DOI] [PubMed] [Google Scholar]
- McMillan W, Stice E, Rohde P. High- and low-level dissonance-based eating disorder prevention programs with young women with body image concerns: An experimental trial. Journal of Consulting and Clinical Psychology. 2011;79:129–134. doi: 10.1037/a0022143. [DOI] [PubMed] [Google Scholar]
- Mitchell KS, Mazzeo SE, Rausch SM, Cooke KL. Innovative interventions for disordered eating: Evaluating dissonance-based and yoga interventions. International Journal of Eating Disorders. 2007;40:120–128. doi: 10.1002/eat.20282. [DOI] [PubMed] [Google Scholar]
- Odell PM, Korgen KO, Schumacher P, Delucchi M. Internet use among male and female college students. CyberPsychology & Behavior. 2000 Oct;3(5):e. [Google Scholar]
- Perez M, Becker CB, Ramirez A. Transportability of an empirically supported dissonance-based prevention program for eating disorders. Body Image: An International Journal of Research. 2010;7:179–186. doi: 10.1016/j.bodyim.2010.02.006. [DOI] [PubMed] [Google Scholar]
- Rideout V, Roberts D, Foehr U. Generation M: Media in the lives of 8–18 Year-olds. Kaiser Family Foundation; Washington, D.C.: 2005. [Google Scholar]
- Rodriguez R, Marchand E, Ng J, Stice E. Effects of a cognitive dissonance-based eating disorder prevention program are similar for Asian American, Hispanic, and White participants. International Journal of Eating Disorders. 2008;41:618–625. doi: 10.1002/eat.20532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seidel A, Presnell K, Rosenfield D. Mediators in the dissonance eating disorder prevention program. Behaviour Research and Therapy. 2009;47:645–653. doi: 10.1016/j.brat.2009.04.007. [DOI] [PubMed] [Google Scholar]
- Spek V, Cuijpers P, Nyklíček I, Pier H, Keyzer J, Pop V. Internet-based cognitive behaviour therapy for symptoms of depression and anxiety: a meta-analysis. Psychological Medicine. 2007;37:319–328. doi: 10.1017/S0033291706008944. [DOI] [PubMed] [Google Scholar]
- Stice E, Marti CN, Shaw H, Jaconis M. An 8-year longitudinal study of the natural history of threshold, subthreshold, and partial eating disorders from a community sample of adolescents. Journal of Abnormal Psychology. 2009a;118:587–597. doi: 10.1037/a0016481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Marti CN, Spoor S, Presnell K, Shaw H. Dissonance and healthy weight eating disorder prevention programs: Long-term effects from a randomized efficacy trial. Journal of Consulting and Clinical Psychology. 2008;76:329–340. doi: 10.1037/0022-006X.76.2.329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Marti N, Rohde P, Shaw H. Testing mediators hypothesized to account for the effects of a dissonance eating disorder prevention program over longer-term follow-up. Journal of Consulting and Clinical Psychology. 2011a;79:398–405. doi: 10.1037/a0023321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Mazotti L, Weibel D, Agras WS. Dissonance prevention program decreases thin-ideal internalization, body dissatisfaction, dieting, negative affect, and bulimic symptoms: A preliminary experiment. International Journal of Eating Disorders. 2000;27:206–217. doi: 10.1002/(sici)1098-108x(200003)27:2<206::aid-eat9>3.0.co;2-d. [DOI] [PubMed] [Google Scholar]
- Stice E, Presnell K, Gau J, Shaw H. Testing mediators of intervention effects in randomized controlled trials: An evaluation of two eating disorder prevention programs. Journal of Consulting and Clinical Psychology. 2007a;75:20–32. doi: 10.1037/0022-006X.75.1.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Rohde P, Gau J, Shaw H. An effectiveness trial of a dissonance-based eating disorder prevention program for high-risk adolescent girls. Journal of Consulting and Clinical Psychology. 2009b;77:825–834. doi: 10.1037/a0016132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Rohde P, Gau J, Shaw H. Effect of a dissonance-based prevention program on risk for eating disorder onset in the context of eating disorder risk factors. Prevention Science. doi: 10.1007/s11121-011-0251-4. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Rohde P, Shaw H, Butryn M, Marti CN. Effectiveness trials of a dissonance eating disorder prevention program are producing large and persistent effects.. Presentation at the Eating Disorder Research Society Meeting; Edinburgh, Scotland. Sept, 2011.2011b. [Google Scholar]
- Stice E, Rohde P, Shaw H, Gau J. An effectiveness trial of a selected dissonance-based eating disorder prevention program for female high school students: Long-term effects. Journal of Consulting and Clinical Psychology. 2011c;79:500–508. doi: 10.1037/a0024351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Shaw H, Burton E, Wade E. Dissonance and healthy weight eating disorder prevention programs: A randomized efficacy trial. Journal of Consulting and Clinical Psychology. 2006;74:263–275. doi: 10.1037/0022-006X.74.2.263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Shaw H, Marti CN. A meta-analytic review of eating disorder prevention programs: Encouraging Findings. Annual Review of Clinical Psychology. 2007b;3:233–257. doi: 10.1146/annurev.clinpsy.3.022806.091447. [DOI] [PubMed] [Google Scholar]
- Stice E, Sysko R, Roberto CA, Allison S. Are dietary restraint scales valid measures of dietary restriction? Additional objective behavioral and biological data suggest not. Appetite. 2010;54:331–339. doi: 10.1016/j.appet.2009.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor C, Bryson S, Luce KH, Cunning D, Doyle A, Abascal LB, Wilfley DE. Prevention of Eating Disorders in At-Risk College-Age Women. Archives of General Psychiatry. 2006;63:881–888. doi: 10.1001/archpsyc.63.8.881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Strien T, Frijters JE, Van Staveren WA, Defares PB, Deurenberg P. The predictive validity of the Dutch Restrained Eating Scale. International Journal of Eating Disorders. 1986;5:747–755. [Google Scholar]
- Winn J, Heeter C. Gaming, gender, and time: Who makes time to play? Sex Roles. 2009;61:1–13. [Google Scholar]
- Winzelberg AJ, Eppstein D, Eldredge KL, Wilfley D, Dasmahapatra R, Dev P, Taylor C. Effectiveness of an Internet-based program for reducing risk factors for eating disorders. Journal of Consulting and Clinical Psychology. 2000;68:346–350. doi: 10.1037//0022-006x.68.2.346. [DOI] [PubMed] [Google Scholar]
- Winzelberg AJ, Taylor C, Sharpe T, Eldredge KL, Dev P, Constantinou PS. Evaluation of a computer-mediated eating disorder intervention program. International Journal of Eating Disorders. 1998;24:339–349. doi: 10.1002/(sici)1098-108x(199812)24:4<339::aid-eat1>3.0.co;2-j. [DOI] [PubMed] [Google Scholar]
- Zabinski MF, Pung MA, Wilfley DE, Eppstein DL, Winzelberg AJ, Celio A, Taylor C. Reducing risk factors for eating disorders: Targeting at-risk women with a computerized psychoeducational program. International Journal of Eating Disorders. 2001;29:401–408. doi: 10.1002/eat.1036. [DOI] [PubMed] [Google Scholar]
- Zabinski MF, Wilfley DE, Calfas KJ, Winzelberg AJ, Taylor C. An Interactive Psychoeducational Intervention for Women at Risk of Developing an Eating Disorder. Journal of Consulting and Clinical Psychology. 2004;72:914–919. doi: 10.1037/0022-006X.72.5.914. [DOI] [PubMed] [Google Scholar]