Abstract
Purpose
The primary goal of this study was to assess the difference in active flexion between patients with a mobile versus a fixed bearing, cruciate retaining, and total knee arthroplasty. The study was designed as a randomised controlled multi-centre trial.
Methods
Participants were assigned to interventions by using block-stratified, random allocation. Outcome parameters were active flexion, passive flexion, and Knee Society Score (KSS). Outcome parameters were assessed preoperatively and at 3, 6, and 12 months postoperatively by an independent nurse.
Results
Ninety-two patients from one centre were included, 46 in each group. Active flexion was comparable for the two groups, 99.9° for the mobile bearing group and 101° for the fixed bearing group with a baseline controlled difference of 1.0 (95% CI −3.9 to 5.8, n.s.). The Clinical KSS was comparable between the two bearing groups (Mobile 90.0 vs. fixed 92.4, n.s.). The functional KSS showed a difference that was attributable to the stair climbing subscore, which showed a difference in favour of the fixed bearing design between preoperative and 3 months (7.3 point difference; 95% CI 2.3–12.5; P = 0.005) as well as 12 months (4.8 point difference; 95% CI 0.1–9.6; P = 0.045).
Conclusions
There were no short-term differences in active flexion between fixed bearing and mobile bearing total knee arthroplasty.
Level of evidence
I.
Keywords: Knee arthroplasty, Functional performance, Prostheses and implants, Osteoarthritis, Mobile bearing, Knee flexion
Introduction
The mobile insert was introduced because it is believed to reduce polyethylene wear, to reduce interface stresses at the tibial plateau, and to improve kinematics by increasing range of motion (ROM) and facilitating axial rotation. The possible disadvantages of the mobile insert are dislocation and increased wear from the interface between the insert and the tibial component.
However, review of the literature revealed no evidence of superiority of either design with respect to improvement of kinematics as defined by flexion or range of motion [10, 15] Haas et al. [7] showed a group with lower flexion for a mobile bearing group compared to a fixed bearing group. Randomised studies by Rees et al. [18] and Mockel et al. [14] showed more natural kinematic patterns for the mobile bearing. Other randomised trials found no statistical significant difference in passive flexion as measured by the Knee Society Score [12, 13, 17, 22]. Banks et al. [1] found an influence of femur position on the tibia on weight-bearing flexion with several implant designs with mobile bearings having a relative anterior position and less flexion. Improved movement possibilities, among which active flexion is most important one is the working mechanism for the mobile bearing knee. With regard to active flexion, the relative effectiveness of these two prostheses with the different bearing types has not yet been established. The goal of this study is, therefore, to evaluate the difference in active flexion at 1 year between mobile and fixed bearing total knee arthroplasty (TKA). The hypothesis was that mobile bearing total knee arthroplasty would result in a better flexion at 1 year than fixed bearing TKA.
Materials and methods
A multi-centre, randomised trial with two treatment arms was performed in two centres: Sint Maartenskliniek in Nijmegen, The Netherlands and Ziegler Spital in Bern, Switzerland. In the Netherlands, 6 surgeons contributed patients; in Switzerland, 2 surgeons contributed patients. The null hypothesis was that there is no difference in active ROM between mobile and fixed bearing total knee prostheses. The study was conducted in compliance with the study protocol, Declaration of Helsinki, ICH-GCP [5], EN 540: The European Standard on Clinical Investigation of Medical Devices for Human Subjects, and applicable regulatory requirements. The study was approved by the regional ethical review board (nr 2001/211).
Patients scheduled for surgery between 2002 and 2006 were selected for the participation. See Table 1 for inclusion and exclusion criteria. Patients selected were informed and asked for consent by auto-reply mail.
Table 1.
Inclusion and exclusion criteria
| Inclusion criteria |
| Diagnosed with osteoarthritis (also referred to as gonarthrosis). |
| Candidate for primary total knee arthroplasty for this reason |
| Expected to undergo only one arthroplasty procedure within next 12 months |
| Willing to attend all the follow-up examinations |
| Expected to make a full recovery |
| 60–75 years old |
| Preoperative alignment (varus or valgus) <10° |
| BMI <30 |
| Live independently |
| Exclusion criteria |
| Missing or having an insufficient posterior cruciate ligament |
| Need cementing of the tibial stem due to osteoporosis |
| Currently enrolled in a clinical investigation with either a drug or an investigational device or has been enrolled in such an investigation during the last 6 months. |
| Suffer from heart or lung disease |
Surgeon-dependent block (size 4) randomisation was performed with computer-generated randomisation lists by the trial coordinator (WJ). Treatment allocation was concealed to all persons in the patient selection process with opaque closed envelopes kept and opened at the order of the sequential randomisation number. Allocation was revealed during surgery, only after identification of intact PCL. Absence of the PCL excludes the mobile bearing as a treatment option, so these patients had to be excluded before randomisation.
Interventions
The two interventions under investigation were the mobile and the fixed bearing total knee arthroplasties of the BalanSys™ type, Mathys Medical Ltd Bettlach, Switzerland. The mobile bearing has anterior–posterior gliding (7–9 mm) and rotational (15°) degrees of freedom. The fixed and mobile bearing types of this system are identical in all other factors. All procedures were posterior cruciate retaining without patella resurfacing. The proximal tibial bone cut was performed perpendicular to the mechanical axis of the tibia with external guide, and the distal femoral bonecut was performed with an intramedullary guide corrected for radiographic deviation of the mechanical axis from the anatomical axis. Rotational alignment (anterior and posterior bone cuts) of the femoral implant was determined during flexion balancing with 100 N with the BalanSys tensioner. Both the tibia and femur components were cemented.
Outcome parameters
The primary outcome parameter, active flexion, was assessed by an independent nurse. To assess the active flexion, the patient was asked to stand upright and to flex the knee as much as possible using patients’ own muscle force.
Secondary outcome parameters were clinical and radiological outcome. Knee Society Clinical and Functional Score by Insall et al. [9] were assessed by independent nurse trained in the assessment. Radiological parameters were assessed by one independent surgeon according to the Knee Society radiological scoring system [6]. Radiolucent lines were scored as absent, being less than 1 mm, 1–2 mm and more than 2 mm on lateral radiographs made under fluoroscopic guidance.
All outcome parameters were assessed preoperatively and at 3, 6, and 12 months postoperatively. No blinding was attempted at any of the assessments.
Statistical analysis
Sample size was calculated to be 122, 61 in each group, in order to be able to detect a clinically relevant difference of 10° in range of motion with a power of 0.90 and a significance level of 0.05. A two-sided interval was used to establish a superiority design. This sample size was estimated to provide adequate power for the secondary outcome parameters to a cumulative significance level of 0.05.
Statistical analysis was performed with SPSS 17.0.1 (SPSS Inc©). Active flexion was analysed with analysis of covariance (ANCOVA) with preoperative flexion as a covariate. A repeated measures design with preoperative values included was used for secondary variables (KSS clinical, KSS functional and subscores, passive flexion). A χ2 test was used to test the occurrence of radiolucent lines and extension deficit at final follow-up.
Results
One centre with 30 patients was excluded from the analysis due to randomisation error: loss of allocation envelopes made the validity of the allocation untracable. The remaining sample (n = 14) was too small and statistically different from the other, larger centre.
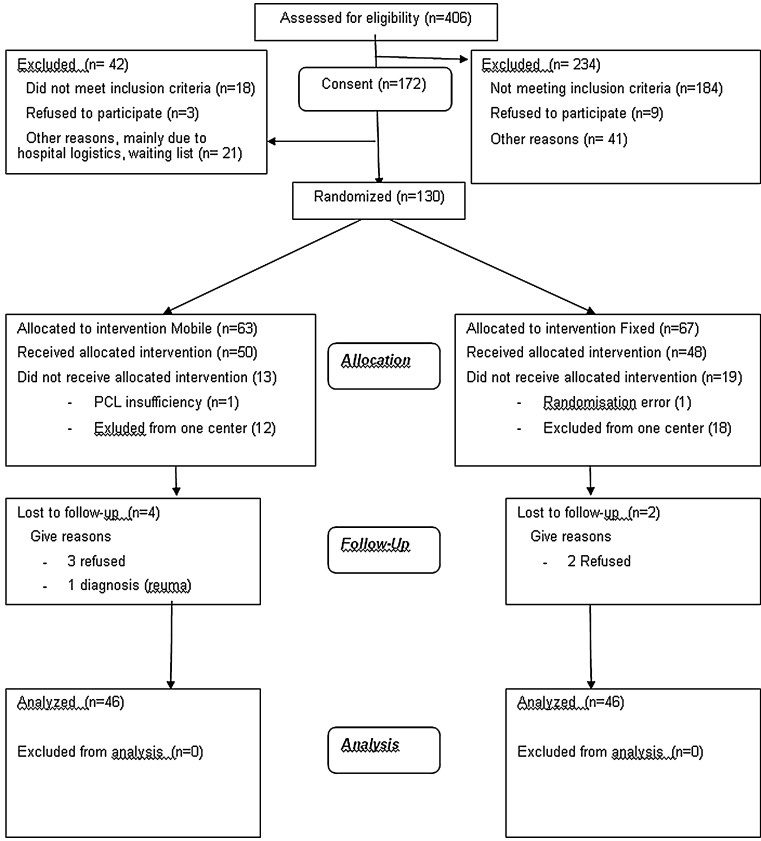
The number of patients recruited, included and excluded at the various stages are represented in Fig. 1 according to the CONSORT statement [4]. In conclusion, 100 patients were randomised, of whom 51 with a mobile bearing and 49 with a fixed bearing total knee prosthesis. One patient in each group was lost during randomisation, one due to randomisation error and one was excluded because of missing PCL. In the mobile bearing group, 4 patients were lost to follow-up after randomisation because of refusal to attend any further visits (3) and one patient presented with rheumatoid arthritis after the surgery. In the fixed bearing group, two patients were lost after randomisation because of consent withdrawal. In the mobile bearing group, data from three patients were incomplete because of death (2) and revision (1), in the fixed bearing group one patient died.
Fig. 1.
Consort statement flowchart
Demographic characteristics of the patients are shown in Table 2. Previous surgery and concomitant medical conditions were evenly divided among the two groups. Preoperatively, groups were comparable on all factors. For the results at all follow-up moments for active flexion, KSS clinical and functional score, see Table 3. The difference of 1.0° (95% CI −3.9 to 5.8) at 12 months for active flexion (primary question) was not significant (Ancova with preoperative flexion as covariate; n.s.). Also, repeated measures analysis did not reveal any significant effects. Post hoc power to detect a 10° difference was 0.996. For the KSS clinical score, no statistically significant differences were found at 12 months or with repeated measures analysis. For the KSS functional score, the repeated analysis showed a significant difference between the two groups (P = 0.017). Further analysis showed that this was mainly attributable to the stair climbing score, which showed a difference in favour of the fixed bearing design between preoperative and 3 months (7.3 point difference; 95% CI 2.3–12.5; P = 0.005) as well as 12 months (4.8 point difference; 95% CI 0.1–9.6; P = 0.045). The passive flexion component of the KSS was also not significantly different between the two groups (mobile: 110 vs. fixed: 112; n.s.).
Table 2.
Demographics
| Mobile bearing (n = 46) | Fixed bearing (n = 46) | |
|---|---|---|
| Age at surgery (Years)a | 67.6 (4.4) | 66.7 (4.6) |
| Male/Female | 13:33 | 14:32 |
| Left/Right | 18:28 | 23:23 |
| Operating time (min)a | 84 (14) | 86 (14) |
| Other knee with implant (n) | 19 | 19 |
| One or both hip implants (n) | 4 | 3 |
aAverage (SD)
Table 3.
Results for average active flexion, KSS clinical, and functional score for both allocated groups
| Outcome | Allocation | Preoperative | 3 months | 6 months | 12 months |
|---|---|---|---|---|---|
| Active flexion | Mobile bearing | 94.6 (15.8) | 91.8 (9.7) | 95.0 (11.7) | 99.9 (13.1) |
| Fixed bearing | 97.1 (13.2) | 95.0 (13.0) | 97.9 (11.3) | 101.0 (9.8) | |
| KSS Clinical score | Mobile bearing | 51.5 (13.2) | 85.2 (14.7) | 91.3 (10.7) | 90.9 (13.5) |
| Fixed bearing | 53.6 (13.4) | 88.5 (12.2) | 90.3 (11.6) | 93.1 (9.5) | |
| KSS functional score | Mobile bearing | 53.6 (11.0) | 70.4 (21.8) | 81.2 (14.6) | 84.9 (17.3) |
| Fixed bearing | 46.9 (16.0) | 79.7 (17.1) | 83.7 (16.2) | 88.8 (12.8) |
SD in brackets
None of the prostheses were radiologically loose. Twenty-four knees (53%) in the fixed group and 21 (49%) in the mobile group showed radiolucent lines. Five knees in the fixed bearing group showed radiolucent lines of 1–2 mm as opposed to six in the mobile group. In the mobile group, 4 knees showed radiolucent lines of more than 2 mm. Only three knees had slightly progressive radiolucent lines (two mobile; one fixed). Occurrence of radiolucent lines was not different between the two groups (χ2: df = 2; n.s.).
There was one distal femur fracture due to unknown cause in the fixed bearing group. In the mobile group, there were 3 extension deficits that were successfully treated with braces. Also in the mobile group, there was also one suspicion of an infection that resolved after treatment with Genta beads.
Discussion
The most important finding of the present study was that there is no statistically significant difference between mobile and fixed bearing knee arthroplasty on active knee flexion. The amount of active flexion that could be achieved by the patients is lower than the passive flexion reported by other studies, but these findings with regard to passive flexion are in line with the literature where there are also no statistically significant differences in five meta-analyses [10, 15, 16, 19, 21].
Both component types were posterior cruciate retaining. An earlier review on PCL retention versus sacrifice [11] showed that PCL sacrifice only resulted in better ROM if a post and cam (posterior stabilised) system was added. Banks et al. [1] showed in a fluoroscopy study that posterior contact point of the femur on the tibia produced a greater weight-bearing flexion. They also found that posterior stabilised designs facilitated this posterior position. In another fluoroscopy study, they showed that a posterior stabilised design had a more posterior contact point during stair stepping [2].
A significant difference was found in the stair climbing aspect of the Knee Society functional score favouring the fixed bearing design. This is in contrast to the study group of Price et al. and Rees et al. [17, 18], who found a more natural patella tendon angle for the mobile bearing devices. In another gait study, Mockel et al. [14] found a higher flexion for the mobile bearing device, indicating a better biomechanical situation. Tibesku et al. [20] found less interindividual variability for a mobile bearing design, but only in a loaded condition. Although a more natural patella tendon angle and better biomechanics are among the goals of a mobile bearing insert, this was not investigated these in this study. If present in this study, this was not translated in better stair climbing abilities (use of rail) for the mobile bearing design. Stair climbing ability could also be influenced by anterior knee pain. Mobile bearings might show a paradoxical roll-back of the femur causing fat-pad impingement. This has been described with AP gliding LCS components as well [3]. The freedom of anterior movement also allows a more anterior tibiofemoral contact point in flexion causing increased pressure on the patella. In a fluoroscopic study during stair stepping, Banks et al. found a more anterior contact point for mobile bearing knees compared to fixed bearing knees [2]. The third possible explanation is rotation of the tibia plateau causing maltracking of the patella. In this study, maltracking or anterior knee pain was not studied, so these explanations cannot be excluded.
Knee Society clinical subscore is the common outcome parameter for evaluation of total knee arthroplasty. It is a composite score including pain, range of motion and laxity characteristics of the patient and the knee. Several studies could not find a difference between fixed and mobile bearing knees prostheses [8, 12–14, 22], except Price et al. [17] who found a better KSS and Oxford knee score for mobile bearing implants, but does not mention which aspect of the composite score was responsible for the difference.
In this study, a higher percentage of radiolucent lines was found than in other randomised controlled trials on the subject [8, 12, 13, 22]. Most of the lines were minimal, less than 1 mm. Because of the cemented components, it is difficult to distinguish narrow radiolucent lines from sclerotic lines related to the cement. Watanabe et al. [22] found 14% for fixed bearing and 27% for mobile bearing, but this only involves lines of 1 mm or larger, the total percentage could therefore be higher. Kim et al. found in two studies [12, 13] 17 and 34% for fixed bearing and 12 and 25% for mobile bearing. Henricson et al. found 27% in both groups [8]. The wide range of these findings implies the problems of inter-rater variability with the measurement of radiolucent lines. Regardless of these problems, as in this study, none of the studies found a significant difference between the two prosthesis types in the occurrence of radiolucent lines.
There are some methodological limitations in this study. One of the two centres was lost due to randomisation errors. However, the power of the remaining sample remains adequate for detecting a clinically relevant difference in active flexion. This can be explained by the lower variability (SD) of the sample. In addition, the difference observed (1°, 95% confidence interval −3.9 to 5.8) is far below the predefined clinically relevant difference of 10°. To prevent publication bias, there is an obligation to adhere to the policy to present all trials, including those with negative results. Blinding was not applied in this study. Observer bias was minimised by using an independent nurse for the clinical assessments.
The follow-up was short. The primary interest of the study was active flexion, a functional measure which is clinically relevant within the first year postoperative. However, long-term outcome is also important, especially because it is believed that contact stresses and therefore loosening could be improved by the mobile bearing. For that reason, the patients will be followed-up until 10 years postoperatively.
Conclusion
There is no statistically significant difference on active flexion between the mobile and fixed bearing total knee arthroplasty types. From the secondary parameters, stair climbing was better with the fixed bearing type.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
References
- 1.Banks S, Bellemans J, Nozaki H, Whiteside LA, Harman M, Hodge WA. Knee motions during maximum flexion in fixed and mobile-bearing arthroplasties. Clin Orthop Relat Res. 2003;410:131–138. doi: 10.1097/01.blo.0000063121.39522.19. [DOI] [PubMed] [Google Scholar]
- 2.Banks SA, Hodge WA. Implant design affects knee arthroplasty kinematics during stair-stepping. Clin Orthop Relat Res. 2004;426:187–193. doi: 10.1097/01.blo.0000138956.04316.ac. [DOI] [PubMed] [Google Scholar]
- 3.Bauze AJ, Falworth MS, Oakeshott RD. Early results of total knee arthroplasty with a low contact stress anteroposterior glide. J Orthop Surg (Hong Kong) 2009;17(2):174–178. doi: 10.1177/230949900901700210. [DOI] [PubMed] [Google Scholar]
- 4.Begg C, Cho M, Eastwood S, Horton R, Moher D, Olkin I, Pitkin R, Rennie D, Schulz KF, Simel D, Stroup DF (1996) Improving the quality of reporting of randomized controlled trials. The CONSORT statement. JAMA 276(8):637–639 [DOI] [PubMed]
- 5.European agency for the evaluation of medicinal products ICH topic E6: guideline for good clinical practice (1997) http://www.emea.europa.eu/pdfs/human/ich/013595en.pdf
- 6.Ewald FC. The Knee Society total knee arthroplasty roentgenographic evaluation and scoring system. Clin Orthop Relat Res. 1989;248:9–12. [PubMed] [Google Scholar]
- 7.Haas B, Dennis DA, Komistek RD, Brumley JT, Hammill C (2001) Range of motion of posterior-cruciate-substituting total knee replacements: the effect of bearing mobility. J Bone Joint Surg Am 83-A Suppl 2(Pt 1):51–55 [DOI] [PubMed]
- 8.Henricson A, Dalen T, Nilsson KG. Mobile bearings do not improve fixation in cemented total knee arthroplasty. Clin Orthop Relat Res. 2006;448:114–121. doi: 10.1097/01.blo.0000224004.40883.ab. [DOI] [PubMed] [Google Scholar]
- 9.Insall JN, Dorr LD, Scott RD, Scott WN. Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res. 1989;248:13–14. [PubMed] [Google Scholar]
- 10.Jacobs W, Anderson P, Limbeek J, Wymenga A (2004) Mobile bearing vs fixed bearing prostheses for total knee arthroplasty for post-operative functional status in patients with osteoarthritis and rheumatoid arthritis. Cochrane Database Syst Rev (2):CD003130 [DOI] [PubMed]
- 11.Jacobs WC, Clement DJ, Wymenga AB. Retention versus removal of the posterior cruciate ligament in total knee replacement: a systematic literature review within the Cochrane framework. Acta Orthop. 2005;76(6):757–768. doi: 10.1080/17453670510045345. [DOI] [PubMed] [Google Scholar]
- 12.Kim YH, Kim DY, Kim JS (2007) Simultaneous mobile- and fixed-bearing total knee replacement in the same patients. A prospective comparison of mid-term outcomes using a similar design of prosthesis. J Bone Joint Surg Br 89(7):904–910 [DOI] [PubMed]
- 13.Kim YH, Kook HK, Kim JS. Comparison of fixed-bearing and mobile-bearing total knee arthroplasties. Clin Orthop Relat Res. 2001;392:101–115. doi: 10.1097/00003086-200111000-00013. [DOI] [PubMed] [Google Scholar]
- 14.Mockel G, Perka C, Gabler J, Zippel H. Early postoperative functional differences between total knee arthroplasties supplied with mobile-bearing platform or fixed-bearing system–an analysis of gait pattern. Z Orthop Ihre Grenzgeb. 2004;142(1):40–45. doi: 10.1055/s-2004-818028. [DOI] [PubMed] [Google Scholar]
- 15.Oh KJ, Pandher DS, Lee SH, Sung JS, Jr, Lee ST. Meta-analysis comparing outcomes of fixed-bearing and mobile-bearing prostheses in total knee arthroplasty. J Arthroplasty. 2008;24(6):873–884. doi: 10.1016/j.arth.2008.06.002. [DOI] [PubMed] [Google Scholar]
- 16.Post ZD, Matar WY, van de Leur T, Grossman EL, Austin MS. Mobile-bearing total knee arthroplasty: better than a fixed-bearing? J Arthroplasty. 2010;25(6):998–1003. doi: 10.1016/j.arth.2009.07.014. [DOI] [PubMed] [Google Scholar]
- 17.Price AJ, Rees JL, Beard D, Juszczak E, Carter S, White S, de SR, Dodd CA, Gibbons M, Lardy-Smith P, Goodfellow JW, Murray DW (2003) A mobile-bearing total knee prosthesis compared with a fixed-bearing prosthesis. A multicentre single-blind randomised controlled trial. J Bone Joint Surg Br 85(1):62–67 [DOI] [PubMed]
- 18.Rees JL, Beard DJ, Price AJ, Gill HS, Lardy-Smith P, Dodd CA, Murray DW. Real in vivo kinematic differences between mobile-bearing and fixed-bearing total knee arthroplasties. Clin Orthop Relat Res. 2005;432:204–209. doi: 10.1097/01.blo.0000150372.92398.ba. [DOI] [PubMed] [Google Scholar]
- 19.Smith H, Jan M, Mahomed NN, Davey JR, Gandhi R (2011). Meta-analysis and systematic review of clinical outcomes comparing mobile bearing and fixed bearing total knee arthroplasty. J Arthroplasty:PMID: 21295940 [DOI] [PubMed]
- 20.Tibesku CO, Daniilidis K, Vieth V, Skwara A, Heindel W, Fuchs-Winkelmann S. Sagittal plane kinematics of fixed- and mobile-bearing total knee replacements. Knee Surg Sports Traumatol Arthrosc. 2011;19(9):1488–1495. doi: 10.1007/s00167-011-1462-8. [DOI] [PubMed] [Google Scholar]
- 21.Van der Bracht H, Van MG, Verdonk P, Almqvist KF, Verdonk R, Freeman M. Is there any superiority in the clinical outcome of mobile-bearing knee prosthesis designs compared to fixed-bearing total knee prosthesis designs in the treatment of osteoarthritis of the knee joint? A review of the literature. Knee Surg Sports Traumatol Arthrosc. 2010;18(3):367–374. doi: 10.1007/s00167-009-0973-z. [DOI] [PubMed] [Google Scholar]
- 22.Watanabe T, Tomita T, Fujii M, Hashimoto J, Sugamoto K, Yoshikawa H. Comparison between mobile-bearing and fixed-bearing knees in bilateral total knee replacements. Int Orthop. 2005;29(3):179–181. doi: 10.1007/s00264-005-0646-6. [DOI] [PMC free article] [PubMed] [Google Scholar]