Abstract
Background: National vaccination coverage rates for individuals at increased risk of influenza-related complications represent a useful public health indicator of preparedness. We compared European countries regarding (i) vaccination coverage among high-risk groups and (ii) the likelihood that high-risk individuals reported influenza vaccination compared with those at lower risk. Methods: We used data from the Survey of Health, Ageing and Retirement in Europe (SHARE) collected in 2004–05. Adults aged ≥50 years from 11 countries provided self-reports of an influenza vaccination in the previous year (n = 16 913). We defined four high-risk groups (age ≥65 years, presence of vascular disease, chronic lung disease or diabetes) and calculated vaccination coverage with 95% confidence intervals for each country. Country-specific multivariable logistic regression was used to estimate odds ratios (ORs) for membership in a high-risk group and vaccination. Results: The Netherlands had the highest influenza vaccination coverage in high-risk groups (≥75% in any group) while Greece had the lowest (<27% in any group). Older age was positively associated with report of vaccination in all countries, but the strength of this association varied from an OR of <2 (Germany) to >13 (The Netherlands). The ORs for the chronic disease groups was ≥4 for The Netherlands and were considerably lower (and often not statistically significant) for the other countries. Conclusion: Influenza vaccination coverage among high-risk groups varies considerably between European countries. Our findings highlight potential opportunities for reducing influenza-related complications through support for vaccination programs that target high-risk individuals more effectively.
Introduction
Each year, 3–5 million severe cases of seasonal influenza occur worldwide resulting in 250 000–500 000 deaths.1 Influenza and its complications have a profound socio-economic impact in terms of direct (e.g. treatment and hospitalization) and indirect costs (e.g. absenteeism and presenteeism).2,3 Specific population groups are at higher risk of influenza-related complications. These high-risk groups include, among others, older adults and individuals with chronic disease. Vaccination of high-risk groups lowers risk for adverse health outcomes4 including influenza-associated complications and mortality among older adults by up to 60 and 80%, respectively.1 Vaccination of high-risk groups is therefore recommended by the World Health Assembly (WHA)5 as well as by national guidelines of most European countries.6,7
Previous estimates suggest that more than 110 million adults in European Union (EU) Member States belong to one or more high-risk groups that would potentially benefit from vaccination.4,8 However, the extent to which high-risk individuals currently receive influenza vaccination varies considerably between European countries7,9,10 with some EU countries achieving very low rates of coverage. These disparities may, in turn, translate into substantial public health consequences in the event of an European influenza pandemic.
Our current understanding of international differences in influenza coverage is based on reports with several limitations. Many previous studies, for example, rely upon reporting by national gatekeepers who draw on diverse data sources to provide estimates for national vaccination coverage.7,9 Although there are many publications drawing on primary data on influenza coverage for North American samples11–13 or samples of single European countries,14–18 studies simultaneously assessing representative samples from multiple nations within the EU are uncommon.10,19,20 In those that do, data collection techniques are rarely standardized across countries, thereby threatening the validity of cross-country comparisons. Other shortcomings of past work include focus on a limited number of countries under study19 and a failure to provide data on vaccination coverage in high-risk groups (e.g. those with cardiovascular or respiratory disease).10,20 Data on high-risk groups are essential for guiding public health policy to curtail the impact of influenza outbreaks at the national and international level.
In this study, we draw upon data from a large population-based study conducted in 11 European countries. Specifically, we compared (i) the influenza vaccination coverage among high-risk groups and (ii) the strength of the association between high-risk group membership and vaccination coverage between European countries. These data may help identify Member States in which efforts to target influenza vaccination could be intensified.
Methods
Participants and data collection
We used data from the first wave of the Survey of Health, Ageing and Retirement in Europe (SHARE), conducted in 2004–05.21,22 Briefly, at enrolment, SHARE participants resided in one of 11 countries (Austria, Belgium, Denmark, France, Germany, Greece, Italy, The Netherlands, Spain, Sweden and Switzerland), were aged ≥50 years, not institutionalized or living abroad, and spoke the official language(s) of their home country. The participant's partner/spouse was included as well (regardless of age). A variety of probability sampling techniques were used to generate nationally representative samples.22 In Belgium, two independent samples were recruited (in Wallonia and Flanders), which are addressed separately in this article. In the Belgian samples, most data were collected between January and June in 2005. In all other countries data were gathered in 2004, mostly between April and October.
Data were collected by face-to-face interviews and questionnaires that had been pretested and refined in participating countries.22 Interview response rates ranged from 74% (Spain) to 93% (France) (country mean = 85%). Items on influenza vaccination were included in self-completed questionnaires, with response rates ranging between 70% in Sweden and 93% in Greece (country mean = 81%).
Influenza vaccination was assessed by the question: ‘In the last year, have you had a flu vaccination?’ The definition of high-risk groups was consistent with vaccination guidelines in effect in most EU Member States in 2006–07.15 We assumed that the national recommendations for the 2006–07 influenza season would not substantially differ from those in 2003–04. The exact definitions based on self-reported data were as follows:
‘Older adults’ were defined as ≥65 years of age because individuals in the majority of the included countries should be vaccinated at ≥65 years according to national guidelines.23 This operational approach is also consistent with the WHO definition.1
The presence of vascular disease, as indicated by one or more of the following: physician-diagnosed stroke/cerebral vascular disease or heart attack (including myocardial infarction or coronary thrombosis or any heart problem including congestive heart failure), or current, regular use of medications (at least weekly) for treatment of coronary or cerebrovascular disease or other heart diseases.
The presence of chronic lung diseases, as indicated by one or more of the following: physician-diagnosed asthma, physician-diagnosed chronic lung disease or current, regular use of medications (at least weekly) for treatment of asthma or chronic bronchitis.
Diabetes, as indicated by report of physician-diagnosed diabetes, high blood sugar or current, regular use of medications to treat diabetes.
The SHARE data contained an item identifying physician-diagnosed Parkinson's disease, a condition frequently highlighted in national vaccination guidelines as carrying greater risk. The number of individuals reporting Parkinson's disease was low, however, and it was therefore not considered in our statistical analysis.
Statistical analyses
Complete data on the variables required to define high-risk group membership, vaccination and confounders (see below) were available for 16 913 individuals. On the country-level, the sample size ranged from n = 682 (Switzerland) to n = 2083 (Sweden).
We first estimated overall- and country-specific age- and sex-weighted vaccination coverage along with corresponding 95% confidence intervals (CIs). Next, associations between influenza vaccination and individual risk conditions were explored by logistic regression estimating odds ratios (ORs) and corresponding 95% CIs.
Logistic regression models were initially adjusted for sex and, if appropriate for age (≥65 years vs <65 years). In a second step, variables representing membership in any high-risk group were entered into the same model (thus, mutually adjusted) and were adjusted for the following confounders: income (tertiles of total gross household income adjusted for purchasing power parity and divided by the number of household members), education (measured according to the 1997 International Standard Classification of Education24 and categorized into three groups: those with less than a completed secondary education, those with secondary or post-secondary education, and those having completed the first and second stage of tertiary education), and the number of contacts with physicians per year categorized as 0–1, 2–5, 6–10 and >10. To reflect the probability of selection, individual sample weights calibrated against the distribution of each country's residents by age group and sex were incorporated into the analyses. Analyses were conducted using SAS 9.2. (Proc Surveyfreq and Proc Surveylogistic, SAS Institute Inc., Cary, North Carolina, USA). Variances for both coverage rate and ORs were estimated by the Taylor series linearization method to account for the complex survey design.
As mentioned, the cut-off used to define a high-risk group based on age is ≥65 in most countries. To test the sensitivity of our results, we developed models using an age cut-off at ≥60.
Results
The SHARE subsample included in this study had a mean age of 64.5 years (SD = 9.8 years) with more than half being female (54.5%). Overall, 35.6% of the study population received an influenza vaccination, 46.0% were aged ≥65 years, and the prevalences of vascular disease, chronic lung disease and diabetes were 15.6, 9.1 and 9.9%, respectively. A description of the size and characteristics of each national sample is published as supplementary online material (Supplementary table S1). Figure 1 depicts influenza vaccination coverage within high-risk groups by countries (tabulated exact estimates can be found online, Supplementary tables 2–5) Coverage rates among high-risk groups varied considerably between countries across a range of >50%. The ranking of countries by coverage was similar across all high-risk groups: The Netherlands consistently had the highest coverage in each high-risk group (≥75%) followed by the two Belgian samples (≥64%). Germany (except for diabetes), Austria and Greece consistently had the lowest coverage across risk groups with Greece performing at the lowest levels (<27%) for all risk groups.
Figure 1.
Prevalence of influenza vaccination and corresponding 95% confidence intervals by country and high-risk group
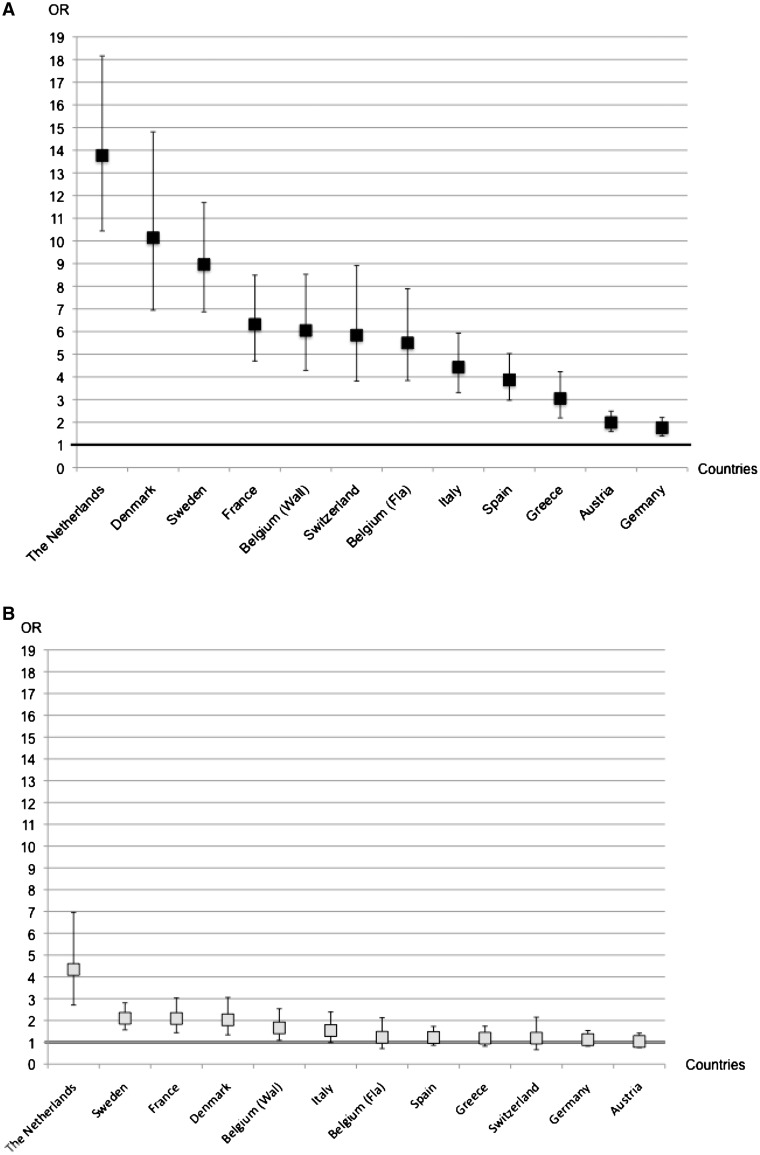
Multivariable ORs for influenza vaccination in high-risk groups are shown in figure 2 (see online material for exact estimates). The OR of vaccination for those aged ≥65 years (versus <65 years) was significantly elevated in all countries. However, the strengths of this association varied considerably between countries. The highest ORs were observed for the Netherlands (OR = 13.8, 95% CI 10.4–18.2), Denmark (OR = 10.2, 95% CI 6.9–14.8) and Sweden (OR=9.0, 95% CI=6.9–11.7), while the lowest ORs were found in Austria (OR = 2.0, 95% CI 1.6–2.5) and Germany (OR = 1.8, 95% CI 1.4–2.2). ORs were generally lower and less variable across countries for those at high risk based on the presence of specific diseases compared with those at high risk based on age. For individuals with chronic diseases, the highest ORs were consistently observed for The Netherlands (all ORs exceeding 4.3, P < 0.05). ORs for other countries were generally lower and all within the same range. Our analysis suggested that adults with chronic lung disease, vascular disease or diabetes were not significantly more likely to be vaccinated than adults without these conditions in a majority of countries.
Figure 2.
Multivariable odds ratios (ORs) and 95% confidence intervals for the association between high-risk group membership and influenza vaccination, by country. (A) Older age (≥65 years vs 50–64 years) and vaccination; (B) Vascular disease (yes vs no) and vaccination; (C) Chronic lung disease (yes vs no) and vaccination; (D) Diabetes (yes vs no) and vaccination. ORs are adjusted for high-risk group membership, sex, income, education and the number of annual contacts with physicians
When we used a cut-off at ≥60 years for all countries to define eligibility for vaccination based on age, countries’ rankings according to ORs (for age or for high-risk disease groups) were not substantially affected.
Discussion
The present study found that influenza vaccination coverage in high-risk groups differed considerably between European countries in 2003–04. The ranking of countries was generally consistent across high-risk groups with The Netherlands and Belgium attaining the highest reported coverage rates while Germany, Austria and Greece had the lowest coverage. Further, our data suggest that older adults were targeted to a significant extent in some countries compared with those of younger age, but this finding varied profoundly between countries. With regard to chronic disease groups, the Netherlands appeared to have used a consistently more targeted approach than other countries. Individuals with chronic disease seemed to have been targeted less well than individuals identified as high risk by age.
Previous investigations collecting original data on influenza vaccination rates in multiple European countries include a series of studies conducted during various influenza seasons.10,20,25 One study covering the 2003–04 influenza season, for example, examined rates in five European countries and reported vaccination prevalence estimates in line with our findings among adults aged ≥65 years.20 A second study conducted within the same influenza season in a separate sample of nations19 also agrees substantially with results from our study, while differing with respect to reports of higher vaccination coverage in older adults from Sweden (54% vs 46%) and lower coverage for Germany (41% vs 53%). We note, however, that the availability of a significantly larger sample of older adults enrolled in SHARE may have accounted for differences in estimate precision. Although other earlier reports on vaccination coverage in EU countries exist,7,9 their reliance on dissimilar forms of data provided by national experts examining health record data, surveys or pharmaceutical data make comparison with our findings less accurate.
Our study found similar influenza vaccination coverage in the older age group and in groups at high risk due to chronic disease. This finding contradicts two earlier studies (Kroneman et al.19 and Blank et al.20). Such inconsistency may result from different definitions applied to disease groups: Kroneman et al.,19 for example, defined the presence of chronic disease in adults younger than 65 years of age only while we defined disease risk groups without respect to age. As a result, many adults with chronic disease in our study may have been vaccinated because they also qualified for vaccination due to their age. We believe that the operational approach we used better reflects clinical decision making given a strong association between older age and the presence of chronic disease. The inconsistency of our findings with those of the study by Blank et al.20 could be explained by differing age distributions of the samples under study. The mean age in SHARE was 64.5 years with a minimum age of 50 years; in contrast, the sample evaluated by Blank et al.20 was generally younger with a smaller proportion of individuals with chronic disease. Only Kroneman et al.19 defined specific chronic disease groups and found considerable between-country differences. The coverage rates among the high-risk groups of adults with heart disease, lung disease and diabetes were lower than in our study—probably due to differences in the definition of high-risk groups and the lower precision associated with smaller sample sizes.
Our data also suggest that the older adults were better targeted with regard to influenza vaccination than those with chronic disease. This finding is consistent with results from previous work20 illustrating, for each of the five included countries, stronger associations between vaccination and older age than between vaccination and presence of a relevant chronic disease.
Vaccination effectively reduces the risk of adverse influenza-related health outcomes in older adults and in those with chronic diseases4 and a targeted approach to vaccination of these risk groups represents a cost-saving preventive measure.8 Although the WHA proposed a goal for vaccination coverage of 50% of older adults by 2006,5 we observed a substantial shortfall in delivery of this public health measure among older adults as well as among individuals qualifying for vaccination due to disease in many European countries in 2003–04. Further, in many countries, vaccination efforts seemed to be targeted to a lesser extent. One explanation may be that health care systems perform very differently concerning the effective implementation and adherence to national vaccination guidelines. The vaccine distribution per 1000 individuals in 2003 in the countries included in this study26 seems to have little bearing on the level of vaccination reported by respondents within our large international sample. For example, more vaccines were distributed in Germany than in Sweden26 in 2003, but we found the prevalence of vaccination among older adults (and also adults aged 50–64 years) to be lower in Germany. Public reimbursement for influenza vaccination administration costs may also be a crucial factor. Influenza vaccination was, for example, not subsidized in Austria in 2003,26 which may partly explain the low prevalence of vaccination in that country. However, public reimbursement is unlikely to fully explain our findings, as our data and those published previously7,10 suggest that vaccination uptake among high-risk groups in Europe seems to vary considerably even between those countries who fully reimburse vaccination of older adults and/or vaccination of individuals with underlying chronic disease. Studies from North America suggest however that introduction of free influenza immunizations may help to increase vaccination rates in high-risk groups.27,28
Country differences may also be explained by between-country variation in the prevalence of determinants of vaccination uptake. For instance, in many countries, socio-demographic factors such as income and education have been found to predict having a flu shot.13,29–32 While we accounted for the confounding effects of these factors when we calculated country-specific ORs, we cannot rule out the possibility that these factors partially explain observed differences between countries. In our study, educational levels and the median income varied profoundly between the included countries (see Supplementary table S1), but the ranking of countries according to these demographics was not in close keeping with their ranking according to vaccination coverage or the odds of vaccination for high-risk groups. However, neither unmeasured confounding nor residual confounding (e.g. related to the measurement of demographics) can be excluded.
In many countries, patients’ risk awareness (e.g. the perception of influenza as a minor vs serious illness) has also been identified as a crucial factor in the decision to obtain an influenza vaccination or to refrain from it10,19,20 and may partly explain cross-country differences observed in the current study. Another factor that may influence receipt of influenza vaccination is recommendation by a health-care worker.10,19,20 A strong central role for general practitioners (GPs) within the Dutch health care system may explain why The Netherlands outperformed other European countries concerning the vaccination coverage of high-risk groups. This health care system relies strongly on GPs as the first point of contact for health care for the general population and as the gatekeeper for regulating access to more specialized care: systems in which GPs play a dominant role may result in the more efficient coordination and targeted delivery of public health measures such as influenza vaccination. Indeed, this explanation is consistent with studies conducted in other national settings in which GPs play a central role in the health care system.10,20 These studies suggested that the UK has the most targeted approach to vaccination of older adults and, even more so, to vaccination of individuals with chronic disease.
Our study comprised nationally representative samples of more than 16 000 adults from 11 European countries and has several strengths. Among these, our data collection tools were carefully standardized for use across countries, a prerequisite for valid cross-country comparisons. Secondly, we minimized the likelihood of selection bias by using data from a study which, in contrast to similar work, achieved good to excellent response rates in all participating national settings. Finally, our estimates have a higher precision than those from earlier studies due to the larger samples of high-risk individuals. With regard to limitations, we acknowledge that our analyses relied on self-reports of influenza vaccination and chronic disease. These have, however, been shown to be sufficiently accurate.33,34 Secondly, one needs to bear in mind that data from most countries pertain to the 2003–04 vaccination season while data from the Belgian samples cover 2004–05, limiting their comparability. Furthermore, our findings may not reflect the current situation in Europe. Thirdly, in each country data were collected throughout various months. In 2004, for instance, most data were collected between April and October. We cannot rule out that recall of vaccination in those who responded to the questionnaire later in the year may have been less accurate than in those who responded earlier. Finally, sample sizes differed between countries, resulting in different degrees of statistical precision.
In conclusion, our study showed considerable differences between European countries with regard to influenza vaccination coverage among high-risk groups defined by age and the presence of chronic disease. The approach to influenza vaccination in The Netherlands deserves greater study to identify insights that may be transferable to other settings. Although international differences in risk awareness by health care consumers or in the role of the GP within national health care systems may explain our findings, further studies are needed to explore these hypotheses as efforts to develop interventions to safeguard public health within Europe and elsewhere.
Supplementary data
Supplementary data are available at EURPUB online.
Funding
SHARE data collection in 2004–07 was primarily funded by the European Commission through its 5th and 6th framework programmes (project numbers QLK6-CT-2001- 00360; RII-CT- 2006-062193; CIT5-CT-2005-028857). Additional funding by the US National Institute on Aging (grant numbers U01 AG09740-13S2; P01 AG005842; P01 AG08291; P30 AG12815; Y1-AG-4553-01; OGHA 04-064; R21 AG025169) as well as by various national sources is gratefully acknowledged (see http://www.share-project.org for a full list of funding institutions).
Conflicts of interest: None declared.
Key points.
Influenza vaccination coverage in older adults and in those with vascular disease, chronic lung disease, or diabetes differed considerably between European countries included in the Survey of Health, Ageing and Retirement in Europe (SHARE).
Older adults were targeted to a significant extent in some countries compared with those of younger age, but this finding varied profoundly between countries.
With regard to individuals with chronic disease, the Netherlands consistently seemed to have had a more targeted approach than other countries.
Individuals with chronic disease were targeted less well than individuals identified as high risk by age.
Our findings highlight potential opportunities for reducing influenza-related complications through support for vaccination programs that target high-risk individuals more effectively.
Supplementary Material
Acknowledgement
This article uses data from SHARE release 2.3.0, as of 13 November 2009.
References
- 1. World Health Organization. Influenza (Seasonal). Fact Sheet N° 211. Available at: http://www.who.int/mediacentre/factsheets/fs211/en (4 May 2010 date last accessed)
- 2.Szucs T. The socio-economic burden of influenza. J Antimicrob Chemother. 1999;44:11–5. doi: 10.1093/jac/44.suppl_2.11. [DOI] [PubMed] [Google Scholar]
- 3.Keech M, Scott AJ, Ryan PJ. The impact of influenza and influenza-like illness on productivity and healthcare resource utilization in a working population. Occup Med. 1998;48:85–90. doi: 10.1093/occmed/48.2.85. [DOI] [PubMed] [Google Scholar]
- 4.Nicoll A, Ciancio B, Tsolova S, Blank P, Yilmaz C. The scientific basis for offering seasonal influenza immunisation to risk groups in Europe. Euro Surveill. 2008;13:7. doi: 10.2807/ese.13.43.19018-en. [DOI] [PubMed] [Google Scholar]
- 5.World Health Organization. Resolution of the World Health Assembly. Prevention and control of influenza pandemics and annual epidemics. World Health Assembly. 2003 WHA56.19. [Google Scholar]
- 6.Blank PR, Szucs TD. Increasing influenza vaccination coverage in recommended population groups in Europe. Expert Rev Vaccines. 2009;8:425–33. doi: 10.1586/erv.09.7. [DOI] [PubMed] [Google Scholar]
- 7.Mereckiene J, Cotter S, Nicoll A, et al. National seasonal influenza vaccination survey in Europe, 2008. Euro Surveill. 2008;13:2. doi: 10.2807/ese.13.43.19017-en. [DOI] [PubMed] [Google Scholar]
- 8.Ryan J, Zoellner Y, Gradl B, et al. Establishing the health and economic impact of influenza vaccination within the European Union 25 countries. Vaccine. 2006;24:6812–22. doi: 10.1016/j.vaccine.2006.07.042. [DOI] [PubMed] [Google Scholar]
- 9.Kroneman M, Paget WJ, van Essen GA. Influenza vaccination in Europe: an inventory of strategies to reach target populations and optimise vaccination uptake. Euro Surveill. 2003;8:130–8. [PubMed] [Google Scholar]
- 10.Blank PR, Schwenkglenks M, Szucs TD. Vaccination coverage rates in eleven European countries during two consecutive influenza seasons. J Infect. 2009;58:446–58. doi: 10.1016/j.jinf.2009.04.001. [DOI] [PubMed] [Google Scholar]
- 11.Center for Disease Control and Prevention (CDC) State-specific influenza vaccination coverage among adults aged > or =18 years–United States, 2003–04 and 2005–06 influenza seasons. MMWR Morb Mortal Wkly Rep. 2007;56:953–9. [PubMed] [Google Scholar]
- 12.Lu P, Bridges CB, Euler GL, Singleton JA. Influenza vaccination of recommended adult populations, U.S., 1989-2005. Vaccine. 2008;26:1786–93. doi: 10.1016/j.vaccine.2008.01.040. [DOI] [PubMed] [Google Scholar]
- 13.Kwong JC, Rosella LC, Johansen H. Trends in influenza vaccination in Canada, 1996/1997 to 2005. Health Rep. 2007;18:9–19. [PubMed] [Google Scholar]
- 14.de Andres AL, Garrido PC, Hernandez-Barrera V, et al. Influenza vaccination among the elderly Spanish population: trend from 1993 to 2003 and vaccination-related factors. Eur J Public Health. 2007;17:272–7. doi: 10.1093/eurpub/ckl242. [DOI] [PubMed] [Google Scholar]
- 15.Kroneman MW, van Essen GA. Variations in influenza vaccination coverage among the high-risk population in Sweden in 2003/4 and 2004/5: a population survey. BMC Public Health. 2007;7:113. doi: 10.1186/1471-2458-7-113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Holm MV, Blank PR, Szucs TD. Trends in influenza vaccination coverage rates in Germany over five seasons from 2001 to 2006. BMC Infect Dis. 2007;7:144. doi: 10.1186/1471-2334-7-144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Holm MV, Szucs TD, Fara GM. Developments in influenza vaccination coverage in Italy over five seasons (2001–2006) Ann Ig. 2007;19:405–15. [PubMed] [Google Scholar]
- 18.Blank PR, Freiburghaus AU, Schwenkglenks M, Szucs TD. Trends in influenza vaccination coverage rates in the United Kingdom over six seasons from 2001–2 to 2006–7. Euro Surveill. 2008;13:3. doi: 10.2807/ese.13.43.19014-en. [DOI] [PubMed] [Google Scholar]
- 19.Kroneman M, van Essen GA, John Paget W. Influenza vaccination coverage and reasons to refrain among high-risk persons in four European countries. Vaccine. 2006;24:622–8. doi: 10.1016/j.vaccine.2005.08.040. [DOI] [PubMed] [Google Scholar]
- 20.Blank PR, Schwenkglenks M, Szucs TD. Influenza vaccination coverage rates in five European countries during season 2006/07 and trends over six consecutive seasons. BMC Public Health. 2008;8:272. doi: 10.1186/1471-2458-8-272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Börsch-Supan A, Hank K, Jürges HA. A new comprehensive and international view on ageing: introducing the ‘Survey of Health, Ageing and Retirement in Europe’. Eur J Ageing. 2005;2:245–53. doi: 10.1007/s10433-005-0014-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Börsch-Supan A, Jürges HA, editors. The Survey of Health, Aging, and Retirement in Europe – Methodology. Mannheim: Mannheim Research Institute for the Economics of Aging (MEA). Availabe at: http://www.share-project.org (4 May 2010, date last acessed)
- 23. Vaccine European New Integrated Collaboration Effort, European Centre for Disease Prevention and Control. Final Report – National Seasonal Influenza Vaccination Survey in Europe, 2007. Collaboration between VENICE project and ECDC. Work Package No 3. Available at: http://venice.cineca.org/reports.html (21 January 2011, date last acessed)
- 24. UNESCO. ISCED 1997. International Standard Classification of Education. Available at: http://www.uis.unesco.org/ev.php?ID=3813_201&ID2=DO_TOPIC.UNESCO (2 September 2010, date last acessed)
- 25.Müller D, Szucs TD. Influenza vaccination coverage rates in 5 European countries: a population-based cross-sectional analysis of the seasons 02/03, 03/04 and 04/05. Infection. 2007;35:308–19. doi: 10.1007/s15010-007-6218-5. [DOI] [PubMed] [Google Scholar]
- 26.The Macroepidemiology of Influenza Vaccination (MIV) Study Group. The macro-epidemiology of influenza vaccination in 56 countries, 1997–2003. Vaccine. 2005;23:5133–43. doi: 10.1016/j.vaccine.2005.06.010. [DOI] [PubMed] [Google Scholar]
- 27.Ives DG, Lave JR, Traven ND, Kuller LH. Impact of medicare reimbursement on influenza vaccination rates in the elderly. Prev Med. 1994;23:134–41. doi: 10.1006/pmed.1994.1019. [DOI] [PubMed] [Google Scholar]
- 28.Yoo BK, Berry A, Kasajima M, Szilagyi PG. Association between medicaid reimbursement and child influenza vaccination rates. Pediatrics. 2010;126:998–1010. doi: 10.1542/peds.2009-3514. [DOI] [PubMed] [Google Scholar]
- 29.La Torre G, Iarocci G, Cadeddu C, Boccia A. Influence of sociodemographic inequalities and chronic conditions on influenza vaccination coverage in Italy: results from a survey in the general population. Public Health. 2010;124:690–7. doi: 10.1016/j.puhe.2010.06.006. [DOI] [PubMed] [Google Scholar]
- 30.Linn ST, Guralnik JM, Patel KV. Disparities in influenza vaccine coverage in the United States, 2008. J Am Geriatr Soc. 2010;58:1333–40. doi: 10.1111/j.1532-5415.2010.02904.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Andrew MK, McNeil S, Merry H, Rockwood K. Rates of influenza vaccination in older adults and factors associated with vaccine use: a secondary analysis of the Canadian Study of Health and Aging. BMC Public Health. 2004;4:36. doi: 10.1186/1471-2458-4-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Endrich MM, Blank PR, Szucs TD. Influenza vaccination uptake and socioeconomic determinants in 11 European countries. Vaccine. 2009;27:4018–24. doi: 10.1016/j.vaccine.2009.04.029. [DOI] [PubMed] [Google Scholar]
- 33.Kriegsman DM, Penninx BW, van Eijk JT, et al. Self-reports and general practitioner information on the presence of chronic diseases in community dwelling elderly. A study on the accuracy of patients’ self-reports and on determinants of inaccuracy. J Clin Epidemiol. 1996;49:1407–17. doi: 10.1016/s0895-4356(96)00274-0. [DOI] [PubMed] [Google Scholar]
- 34.Mangtani P, Shah A, Roberts JA. Validation of influenza and pneumococcal vaccine status in adults based on self-report. Epidemiol Infect. 2007;135:139–43. doi: 10.1017/S0950268806006479. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.