Abstract
Rationale
Criteria for a clinically significant bronchodilator response (BDR) are mainly based on studies in patients with obstructive lung diseases. Little is known about the BDR in healthy general populations, and even less about the worldwide patterns.
Methods
10 360 adults aged 40 years and older from 14 countries in North America, Europe, Africa and Asia participated in the Burden of Obstructive Lung Disease study. Spirometry was used before and after an inhaled bronchodilator to determine the distribution of the BDR in population-based samples of healthy non-smokers and individuals with airflow obstruction.
Results
In 3922 healthy never smokers, the weighted pooled estimate of the 95th percentiles (95% CI) for bronchodilator response were 284 ml (263 to 305) absolute change in forced expiratory volume in 1 s from baseline (ΔFEV1); 12.0% (11.2% to 12.8%) change relative to initial value (%ΔFEV1i); and 10.0% (9.5% to 10.5%) change relative to predicted value (%ΔFEV1p). The corresponding mean changes in forced vital capacity (FVC) were 322 ml (271 to 373) absolute change from baseline (ΔFVC); 10.5% (8.9% to 12.0%) change relative to initial value (ΔFVCi); and 9.2% (7.9% to 10.5%) change relative to predicted value (ΔFVCp). The proportion who exceeded the above threshold values in the subgroup with spirometrically defined Global Initiative for Chronic Obstructive Lung Disease (GOLD) stage 2 and higher (FEV1/FVC <0.7 and FEV1% predicted <80%) were 11.1%, 30.8% and 12.9% respectively for the FEV1-based thresholds and 22.6%, 28.6% and 22.1% respectively for the FVC-based thresholds.
Conclusions
The results provide reference values for bronchodilator responses worldwide that confirm guideline estimates for a clinically significant level of BDR in bronchodilator testing.
Keywords: Bronchodilator response, spirometry, populations, COPD epidemiology, COPD exacerbations, emphysema, respiratory measurement, asthma epidemiology, clinical epidemiology, bronchoscopy, asthma, occupational lung disease, tobacco and the lung, COPD mechanisms
Key messages.
What is the key question?
What is the distribution of bronchodilator response in healthy populations worldwide?
What is the bottom line?
We have generated global population-based thresholds for bronchodilator reversibility testing.
Why read on?
The article provides new insights into global bronchodilator response and reversibility.
Introduction
Airway responsiveness to a bronchodilator is widely performed in most clinical respiratory function laboratories throughout the world. Bronchodilator response (BDR) is used to predict a patient's response to bronchodilator treatment, to establish best attainable lung function, and in clinical trials, to rule in or rule out asthma and chronic obstructive pulmonary disease (COPD).1–5 Although much has been learned about BDR, there continues to be confusion about its clinical usefulness,6 7 its pathophysiological basis, its expression8–10 and its determinants.11
There is also a lack of consensus on the criteria for a significant or increased BDR.12 13 One obstacle is the lack of agreement on how the response should be expressed.8–10 12 Another is paucity of normative reference data derived from healthy general populations, as has been recommended by the American Thoracic Society (ATS)12 and the European Respiratory Society (ERS) guidelines.13 The most common recommendation of a ‘cut-off’ of 12% change in FEV1 from baseline for significant bronchial responsiveness has been derived from patients with obstructive lung disease.8 9 14–17 It is conceivable that these cut-offs may not reflect the spectrum of responsiveness in a healthy general population.12 To date, the information derived from general populations is patchy,18–20 and none comes from non-Western countries. A better understanding of the worldwide distribution of BDR in health and disease would be helpful for developing global criteria for BDR for clinical use and research.
In this paper we report the BDR in terms of changes in forced expiratory volume in 1 s (FEV1) and in forced vital capacity (FVC), measured in population-based samples from 14 country sites that participated in the Burden of Obstructive Lung Disease (BOLD) study.21 22 The focus in this descriptive report is the distribution of BDR in healthy populations, with comparison in subpopulations with chronic airway obstruction. From these, we generated the 95th percentiles and tested for variability and consistency across countries and within the pooled sample from all countries. This study, which drew participants from countries in North America, Europe, Africa, and Asia, provided the opportunity for a systematic evaluation of the reference range of airway response after bronchodilator in healthy general populations in different regions of the world.
Methods
Subject design and participants
The target population included women and men aged 40 years and older in random population samples from 14 countries in North America, Europe, Africa and Asia. A detailed description of the study design and rationale, and initial results of the BOLD study have been published elsewhere.21 22 Population-based sampling plans were used to recruit participants who were then invited to complete interviewer-administered standardised questionnaires on respiratory health and symptoms, smoking history, quality of life, use of healthcare services, cardiovascular comorbidities and other respiratory diseases. Pre-bronchodilator and post-bronchodilator spirometry testing was done for all eligible participants.
Spirometric testing and quality assurance review
Lung function was obtained at all BOLD sites with the use of a portable spirometer (EasyOne, ndd Medical Technologies, Andover, Massachusetts, USA) to collect data on FEV1 and FVC with forced expiratory time standardised at >6 s or a plateau in the last second of expiration. With the rare exception in which spirometry was contraindicated,21 22 all sites attempted to collect pre- and post-bronchodilator measurements from all participants. Lung function was measured before and 15 min after administering two doses of 100 μg of salbutamol (albuterol) via a spacer. All spirograms were reviewed by the BOLD Pulmonary Function Reading Center and assigned a quality score based on acceptability and repeatability criteria from the ATS.23 Data for FEV1 and FVC were deemed usable and included in this analysis if they fully met ATS acceptability criteria and were repeatable to within 200 ml.
Definition of COPD
As in all BOLD publications, we used the Global Initiative for Chronic Obstructive Lung Disease (GOLD) post-bronchodilator lung function criteria for defining and staging COPD,21 24 and the prediction equations for Caucasian derived from the third US National Health and Nutrition Examination Survey25 to compute percentage predicted FEV1 and FVC. COPD is defined as GOLD stage 2 and greater for subgroups computation.
Statistical analysis
Indices of BDR
We generated six measures of BDR, three each for FEV1 and FVC, using indices recommended by the ATS12 and the ERS10: Absolute change from baseline values (ΔFEV1 and ΔFVC)10; 12 percentage change relative to initial value (%ΔFEV1i and %ΔFVCi)10 12; and percentage change relative to predicted value (%ΔFEV1p and %ΔFVCp).8 9 13 18
Establishment of the upper normal limit of BDR
The ‘normal’ range of BDR was determined from its distribution among healthy never-smoking participants, defined as never smokers who did not report current asthma, chronic bronchitis, doctor diagnosis of emphysema, COPD or tuberculosis. The upper limit of normality of the BDR was defined as the observed upper 95th percentile18 calculated separately for each site. These estimates and their associated 95% CIs were then used to generate forest plots and accompanying weighted estimates of the 95th percentiles that are pooled across sites along with tests for heterogeneity across sites. Individual sites are weighted according to the precision of the estimate at that site and these weights are reflected in the forest plots. We used simple unweighted statistics to summarise various statistics in tabular form for the cohort overall and for subgroups. All analyses were done using Stata V.10.0 (Stata Corp), and the forest plot analyses used the metan procedure.
Results
Of a total of 10 712 subjects, 10 360 (97%) had either acceptable pre-bronchodilator and post-bronchodilator FEV1 data (n=10 217) or acceptable pre-bronchodilator and post-bronchodilator FVC data (n=9546) and are included in this analysis. Table 1 shows their demographical and baseline characteristics by site. The mean ages and SDs ranged from 52.3 (10.3) years in the Philippines to 60.1 (12.8) years in Norway. Patterns of current cigarette smoking varied widely across sites: the lowest smoking rate was 14% in Canada; the highest smoking rate was 46% in South Africa. The intensity of tobacco exposure for smokers expressed as mean (SD) pack-years ranged from 17.0 (17.4) in South Africa to 38.6 (28.9) in Kentucky, USA.
Table 1.
Demographics and baseline characteristics of 10 360 participants with usable spirometry data
| Australia | Austria | Canada | China | Germany | Iceland | Kentucky | Norway | Philippines | Poland | South Africa | Sweden | Turkey | UK | |
| N | 558 | 1298 | 845 | 572 | 704 | 760 | 517 | 676 | 916 | 562 | 865 | 553 | 846 | 688 |
| Age (years) | 59.0 (12.4) | 57.7 (11.6) | 56.1 (11.9) | 54.0 (10.9) | 58.2 (11.0) | 56.4 (11.8) | 56.7 (9.9) | 60.1 (12.8) | 52.3 (10.3) | 55.8 (11.6) | 54.2 (10.4) | 58.4 (11.0) | 53.7 (10.6) | 58.2 (11.5) |
| Current smoker, % | 14.3 | 19.2 | 13.5 | 28.2 | 20.6 | 18.3 | 26.3 | 26.0 | 32.4 | 28.8 | 45.9 | 14.7 | 33.7 | 21.1 |
| Cigarette exposure | ||||||||||||||
| Pack-years (full cohort) | 12.4 (25.4) | 13.2 (20.9) | 11.9 (23.4) | 11.1 (17.9) | 15.1 (20.9) | 12.8 (24.9) | 23.4 (29.3) | 12.7 (16.5) | 9.7 (17.1) | 16.1 (25.3) | 11.5 (16.3) | 10.5 (16.2) | 16.0 (27.0) | 16.3 (31.8) |
| Pack-years (ever smokers) | 24.6 (31.3) | 25.3 (23.1) | 22.7 (29.1) | 26.8 (18.8) | 25.1 (21.9) | 21.0 (29.1) | 38.6 (28.9) | 20.1 (16.7) | 18.5 (19.8) | 26.3 (28.0) | 17.0 (17.4) | 18.3 (17.7) | 29.6 (30.8) | 26.3 (36.9) |
| BMI (kg/m2) | 28.0 (5.1) | 26.4 (4.2) | 26.7 (5.2) | 23.2 (3.4) | 27.3 (4.6) | 27.9 (4.9) | 30.7 (6.9) | 26.5 (4.3) | 24.8 (4.7) | 27.6 (4.7) | 27.8 (7.4) | 27.0 (4.4) | 29.5 (5.5) | 27.1 (5.0) |
| Pre-BD FEV1, % pred | 93.3 (18.1) | 92.8 (17.5) | 95.6 (18.4) | 84.8 (14.8) | 95.2 (17.5) | 89.8 (16.4) | 83.4 (18.8) | 92.3 (16.7) | 74.7 (15.4) | 92.2 (18.3) | 76.8 (19.5) | 93.0 (16.1) | 89.0 (18.5) | 87.6 (17.9) |
| Post-BD FEV1, % pred | 95.9 (17.3) | 95.5 (16.7) | 99.2 (17.9) | 86.5 (14.5) | 97.5 (16.9) | 93.0 (16.0) | 86.7 (18.2) | 94.7 (16.5) | 77.0 (15.1) | 94.9 (17.8) | 79.4 (19.0) | 95.8 (16.1) | 92.3 (17.7) | 90.7 (17.3) |
| GOLD stages* | ||||||||||||||
| Stage 1, % | 8.3 | 14.8 | 10.2 | 4.3 | 8.1 | 8.6 | 5.4 | 11.9 | 1.2 | 11.6 | 4.0 | 9.6 | 8.6 | 11.0 |
| Stage 2, % | 9.3 | 8.3 | 6.3 | 5.6 | 5.6 | 6.7 | 10.7 | 7.7 | 7.1 | 8.6 | 13.0 | 4.7 | 9.1 | 9.3 |
| Stage 3, % | 1.3 | 1.1 | 0.7 | 1.5 | 0.7 | 1.6 | 3.7 | 0.9 | 3.7 | 1.8 | 5.8 | 1.5 | 1.1 | 2.1 |
| Stage 4, % | 0.0 | 0.1 | 0.2 | 0.2 | 0.2 | 0.3 | 0.2 | 0.5 | 0.7 | 0.0 | 0.6 | 0.0 | 0.4 | 0.2 |
| Any respiratory medication, % | 23.0 | 6.4 | 32.4 | 2.6 | 19.7 | 30.0 | 44.0 | 13.8 | 26.5 | 8.6 | 9.8 | 41.6 | 6.0 | 22.5 |
| Asthma ever, % | 17.2 | 7.1 | 14.3 | 3.2 | 9.7 | 16.7 | 22.1 | 17.3 | 6.6 | 7.3 | 14.7 | 14.5 | 6.4 | 19.5 |
Continuous data presented as mean (SD) unless otherwise stated.
GOLD stage I: FEV1/FVC<70% and FEV1≥80% predicted; GOLD stage II: FEV1/FVC<70% and 50%≤FEV1<80% predicted; GOLD stage III: FEV1/FVC<70% and 30%≤FEV1<50% predicted; GOLD stage IV: FEV1/FVC<70% and FEV1<30% predicted.
BMI, body mass index; FEV1, forced expiratory volume in 1 s; GOLD, Global Initiative for Chronic Obstructive Lung Disease; FVC, forced vital capacity; Pre-BD FEV1 % pred, pre-bronchodilator FEV1 % predicted; Post-BD FEV1 % pred, post-bronchodilator FEV1 % predicted.
All indices of BDR in FEV1 and FVC displayed normal or near-normal distribution for the whole study population. Table 2 shows the simple unweighted estimates of the mean change and SD of BDR. For the healthy subgroup, these averages were several fold smaller than the mean values for the subgroup with COPD. Table 3 shows the simple unweighted estimates of the upper 95th percentiles (and associated 95% CIs) for the whole study population and for selected subgroups. BDR, when expressed as an absolute change, was larger in men than in women. However the opposite pattern was seen when BDR was expressed as a percentage change. In addition, per cent change when expressed relative to initial value was always greater (sometimes markedly so) when expressed relative to initial rather than predicted value. Finally, the 95th percentiles were consistently larger for individuals with COPD (regardless of comorbid asthma status) than for healthy lifetime never smokers.
Table 2.
Mean and SD (unweighted values) for bronchodilator responses for whole study population, healthy and COPD subgroups
| Variables | Study population | Healthy subgroup | COPD GS2+ | COPD GS2+ (without asthma) | ||
| All | Men | Women | Men and women | Men and women | Men and women | |
| FEV1-based measures | N1=10 217 | N1=4826 | N1=5391 | N1=3922 | N1=1009 | N1=745 |
| ΔFEV1 (ml) | 82 (139) | 95 (156) | 70 (120) | 72 (130) | 114 (157) | 104 (153) |
| ΔFEV1i (%) | 3.7 (6.9) | 3.6 (6.5) | 3.8 (7.3) | 3.1 (6.0) | 8.8 (11.9) | 7.7 (11.0) |
| ΔFEV1p (%) | 2.8 (4.8) | 2.7 (4.6) | 2.8 (5.0) | 2.6 (4.8) | 4.2 (5.7) | 3.7 (5.5) |
| FVC-based measures | N2=9546 | N2=4560 | N2=4986 | N2=3593 | N2=976 | N2=723 |
| ΔFVC (ml) | 0 (237) | 4 (257) | −4 (217) | −21 (219) | 153 (280) | 138 (273) |
| ΔFVCi (%) | 0.5 (7.9) | 0.5 (6.9) | 0.5 (8.7) | −0.3 (7.4) | 6.9 (12.2) | 6.2 (11.9) |
| ΔFVCp (%) | 0.1 (6.6) | 0.2 (5.9) | 0 (7.3) | −0.5 (6.7) | 4.4 (7.9) | 4.0 (7.6) |
ΔFEV1 (ml) and ΔFVC (ml) are absolute change after bronchodilator; ΔFEV1i and ΔFVCi are change as a per cent of initial value.
ΔFEV1p and ΔFVCp are change as per cent of predicted value. N1 is number with non-missing FEV1 values and N2 is number with non-missing FVC values.
COPD GS2+ = FEV1/FVC <0.7 and FEV1% predicted<80%; COPD GS2+ (without asthma) = post-bronchodilator spirometrically defined COPD excluding those with self-reported asthma.
COPD, chronic obstructive pulmonary disease; FEV1, forced expiratory volume in 1 s; FVC, forced vital capacity.
Table 3.
Upper 95th percentiles with 95% CI (unweighted values) for bronchodilator responses for whole study population, healthy and COPD subgroups
| Variables | Study population | Healthy Subgroup | COPD GS2+ | COPD GS2+ (without asthma) | ||
| All | Men | Women | Men and women | Men and women | Men and women | |
| FEV1-based measures | N1=10 217 | N1=4826 | N1=5391 | N1=3922 | N1=1009 | N1=745 |
| ΔFEV1 (ml) | 314 (306 to 324) | 354 (340 to 368) | 265 (257 to 278) | 291 (279 to 309) | 371 (343 to 402) | 341 (323 to 381) |
| ΔFEV1i (%) | 14.6 (14.1 to 15.3) | 14.0 (13.2 to 14.6) | 15.4 (14.5 to 16.0) | 12.5 (11.9 to 13.2) | 30.9 (27.8 to 33.8) | 27.7 (21.6 to 30.9) |
| ΔFEV1p (%) | 10.6 (10.3 to 10.9) | 10.2 (9.9 to 10.6) | 10.9 (10.5 to 11.3) | 10.1 (9.7 to 10.7) | 13.1 (12.3 to 14.6) | 12.3 (11.6 to 13.5) |
| FVC-based measures | N2=9546 | N2=4560 | N2=4986 | N2=3593 | N2=976 | N2=723 |
| ΔFVC (ml) | 395 (381 to 414) | 454 (419 to 486) | 347 (328 to 374) | 337 (317 to 358) | 635 (591 to 678) | 619 (547 to 668) |
| ΔFVCi (%) | 13.3 (12.7 to 13.9) | 12.6 (11.8 to 13.4) | 14.1 (13.2 to 15.1) | 11.2 (10.5 to 12.2) | 29.4 (26.6 to 31.6) | 26.7 (24.4 to 30.6) |
| ΔFVCp (%) | 10.8 (10.4 to 11.4) | 10.4 (9.7 to 10.8) | 11.6 (10.7 to 12.5) | 9.6 (9.1 to 10.3) | 18.0 (17.0 to 19.7) | 17.3 (15.7 to 18.8) |
ΔFEV1 (ml) and ΔFVC (ml) are absolute change after bronchodilator; ΔFEV1i and ΔFVCi are change as a per cent of initial value; ΔFEV1p and ΔFVCp are change as per cent of predicted value. N1 is number with non-missing FEV1 values and N2 is number with non-missing FVC values.
COPD GS2+ = FEV1/FVC <0.7 and FEV1% predicted<80%; COPD GS2+, without asthma = COPD GS2+ but with no self-reported diagnosis of asthma.
In the COPD subgroups, the CIs for individual sites were large due to small sample size (<50).
COPD, chronic obstructive pulmonary disease; FEV1, forced expiratory volume in 1 s; FVC, forced vital capacity.
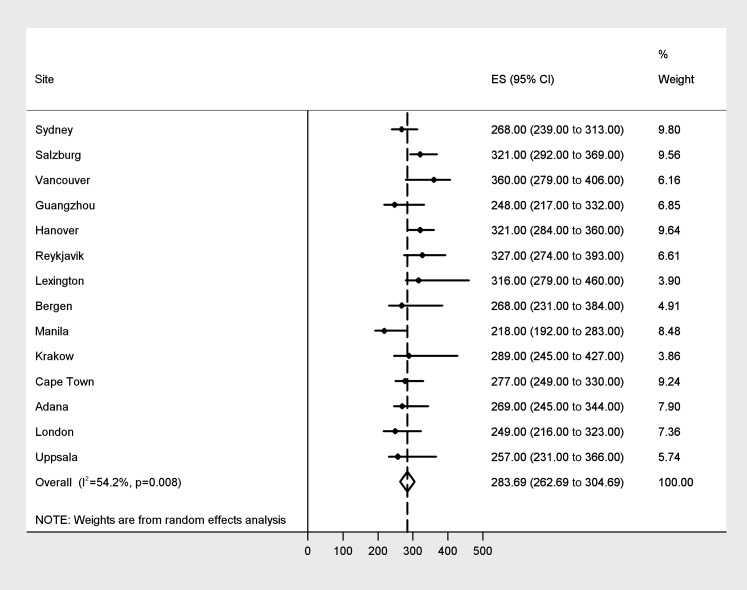
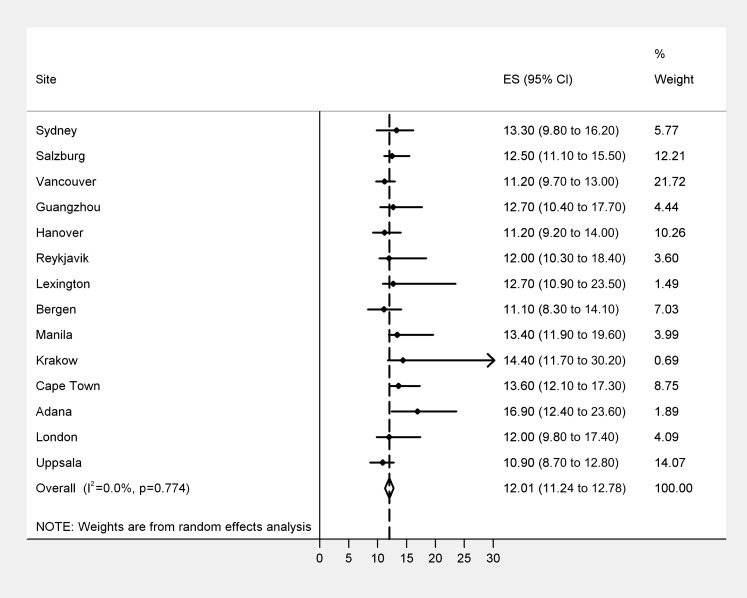
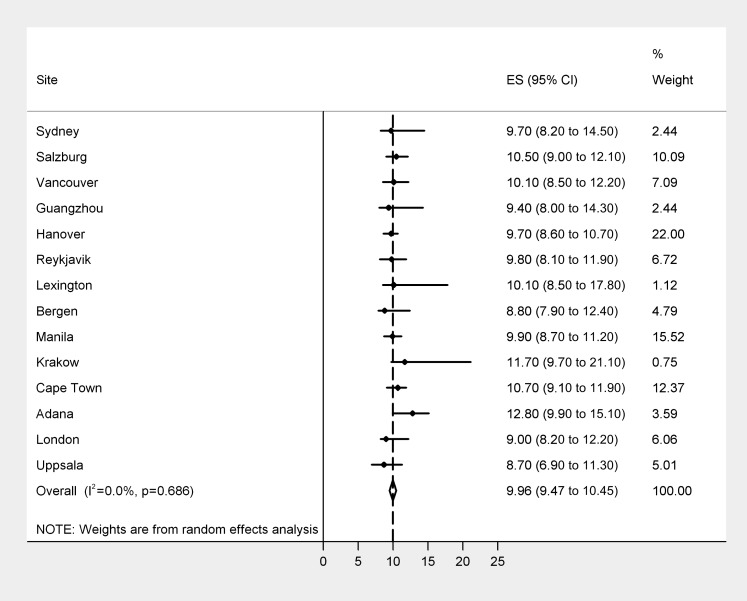
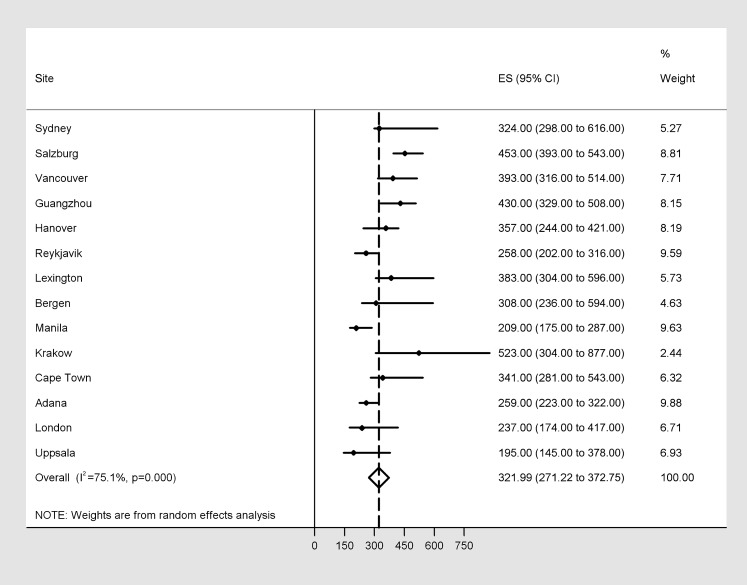
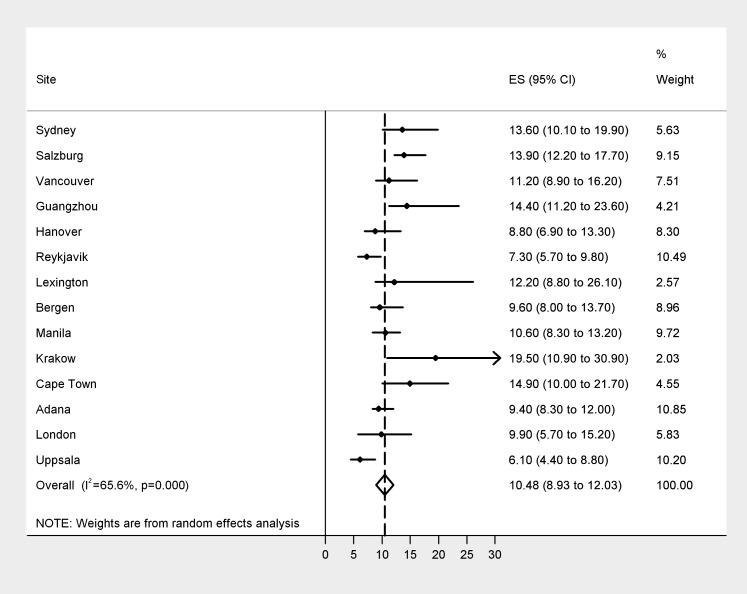
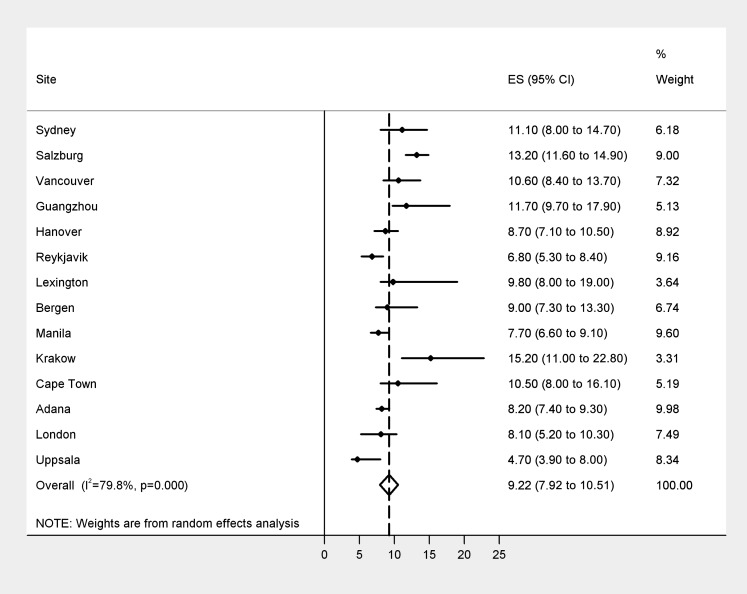
Figures 1–6 show the forest plots of the upper 95th percentile for the six measures of BDR for the subset of healthy never smokers. More precise estimates received greater weight, as shown in the figures, when calculating the pooled estimates, and hence the pooled estimates here differ somewhat from the unweighted estimates of 95th percentiles for all subjects shown in table 3, although they are qualitatively similar. In healthy lifetime non-smokers, the pooled weighted estimate of the threshold for absolute change (ΔFEV1) is 284 ml, with significant cross-site heterogeneity in estimates, that is 54% of overall variation in estimate comes from site to site variability (figure 1). The pooled weighted estimate for %ΔFEV1p (figure 3) is smaller than for %ΔFEV1i (figure 2), with no cross-site heterogeneity in both cases. In contrast, the estimates for the FVC-based thresholds (figures 4–6) all demonstrated marked cross-site heterogeneity, ranging from 66% to 80%.
Figure 1.
Absolute change in forced expiratory volume in 1 s (FEV1) in ml after bronchodilator (ΔFEV1) expressed as 95th percentile with 95% CI in healthy non-smokers. Those sites whose estimates are most stable get greater weight (right-hand column) in constructing the pooled estimate of 284 ml. We observed significant heterogeneity across sites (p=0.008), with 54% of the overall variability in the data attributable to site–site variability.
Figure 2.
Percentage change in forced expiratory volume in 1 s (FEV1) relative to initial baseline, after bronchodilator (BDR FEV1i) expressed as 95th percentile with 95% CI in healthy non-smokers. The pooled estimate is 12% with no evidence of cross-site heterogeneity.
Figure 3.
Percentage change in forced expiratory volume in 1 s (FEV1) relative to predicted FEV1, after bronchodilator (%ΔFEV1p) expressed as 95th percentile with 95% CI in healthy non-smokers. The pooled estimate is 10% with no evidence of cross-site heterogeneity.
Figure 4.
Absolute change in forced vital capacity (FVC) after bronchodilator (BDR FVC, ml) expressed as 95th percentile with 95% CI in healthy non-smokers. Those sites whose estimates are most stable get greater weight (right-hand column) in constructing the pooled estimate of 322 ml. We observed significant heterogeneity across sites (p<0.0001), with 75% of the overall variability in the data attributable to site–site variability.
Figure 5.
Percentage change in forced vital capacity (FVC) relative to initial baseline, after bronchodilator (BDR FVC1i) expressed as 95th percentile with 95% CI in healthy non-smokers. Those sites whose estimates are most stable get greater weight (right-hand column) in constructing the pooled estimate of 11%. We observed significant heterogeneity across sites (p<0.0001), with 66% of the overall variability in the data attributable to site–site variability.
Figure 6.
Percentage change in forced vital capacity (FVC) relative to predicted FVC, after bronchodilator (BDR FVCp) expressed as 95th percentile with 95% CI in healthy non-smokers. Those sites whose estimates are most stable get greater weight (right-hand column) in constructing the pooled estimate of 9%. We observed significant heterogeneity across sites (p<0.0001), with 80% of the overall variability in the data attributable to site–site variability.
Using the weighted thresholds from figures 1–6, we then calculated the simple, unweighted proportion of individuals who exceeded these thresholds for various subgroups (table 4). The proportion of people without airway obstruction who exceeded the threshold was consistently lower than that for people with airway obstruction for both the FEV1-based and FVC-based thresholds. The proportion of people in the COPD subgroups who exceeded the FEV1-based thresholds (except for ΔFEV1i) decreased with increasing severity of COPD as defined by GOLD stages.24 By contrast, the proportion of people in the COPD subgroups who exceeded the FVC-based thresholds showed a tendency to increase with severity.
Table 4.
The proportion of people in excess of thresholds for overall cohort, for subgroups of normal, GOLD stage 1, GOLD stage 2 and GOLD stage 3–4
| Variables | Overall | Normal | GOLD stage 1 | GOLD stage 2 | GOLD stage 3–4 |
| FEV1-based thresholds | N1=10 217 | N1=7931 | N1=846 | N1=790 | N1=219 |
| ΔFEV1 (>284 ml) | 6.7% | 5.6% | 11.5% | 12.2% | 7.3% |
| ΔFEV1i (>12%) | 7.8% | 4.4% | 11.6% | 27.3% | 43.4% |
| ΔFEV1p (>10%) | 6.0% | 4.3% | 12.3% | 13.9% | 9.1% |
| FVC-based thresholds | N2=9546 | N2=7697 | N2=819 | N2=764 | N2=212 |
| ΔFVC (>322 ml) | 7.5% | 4.0% | 21.2% | 20.7% | 29.7% |
| ΔFVCi (>10.5%) | 7.5% | 3.8% | 17.0% | 24.7% | 42.5% |
| ΔFVCp (>9.2%) | 6.8% | 3.2% | 21.6% | 20.5% | 27.8% |
ΔFEV1 (ml) and ΔFVC (ml) are absolute change after bronchodilator; ΔFEV1i and ΔFVCi are change as a per cent of initial value; ΔFEV1p and ΔFVCp are change as per cent of predicted value. N1 is number with non-missing FEV1 values and N2 is number with non-missing FVC values.
Normal = not classified as any GOLD stage; GOLD stage 1 = FEV1/FVC <0.7 and FEV1 % predicted >80%; GOLD stage 2 = FEV1/FVC <0.7 and FEV1 % predicted <80% and >50%; GOLD stage 3–4 = FEV1/FVC <0.7 and FEV1 % predicted <50%.
COPD, chronic obstructive pulmonary disease; FEV1, forced expiratory volume in 1 s; FVC, forced vital capacity; GOLD, Global Initiative for Chronic Obstructive Lung Disease.
Discussion
We measured the BDR in general population samples, aged 40 and older, from sites in 14 countries spanning four continents. The main findings indicated that the thresholds or upper limit of normality for the per cent change in FEV1 relative to initial level is 12% and for the FEV1 relative to predicted FEV1 is 10% without heterogeneity across populations. These values agree well with current ATS guideline cutoffs for defining a significant BDR and strengthen the applicability of these measures for global interpretation in bronchodilator testing. We further validated these thresholds in people with and without obstruction and confirmed that a higher proportion of people with obstruction of all stages of severity had BDR compared with those without obstruction, findings that are consistent with previous studies in healthy individuals and people with airway obstruction using ATS-ERS thresholds.10
There were two secondary findings. First, the BDR threshold for people with chronic airflow obstruction was lower when asthma was excluded, but there was considerable overlap between the two groups with and without exclusion of asthma, consistent with previous studies.1 26 27 Also, there were differences between the FEV1-based and the FVC-based thresholds in their association with severity of airflow obstruction. The proportion with reversibility measured by changes in FEV1 generally decreased as COPD severity increased while that with reversibility measured by changes in FVC increased with increasing COPD severity, findings which are consistent with the findings reported in clinical trials of patients with COPD, using ATS reversibility criteria.4 These findings support the use of lung volume-based measures of reversibility in addition to FEV1-based measures in patients with more severe COPD.26
In this analysis the thresholds for BDR for healthy people were derived from random samples of adults aged 40 years and over in the general population. According to the ERS guidelines, an ambiguous BDR should exceed spontaneous variability and the response observed in healthy individuals.13 Yet, evidence for the different published criteria had largely been based on data of selected patients with airflow limitation.8 9 14–17 28 Existing data on the upper limit of the BDR in the healthy population are few and dated,18 29 although a recent study of unselected urban population in Iceland reported a 95th percentile of 9% for increase in FEV1 from baseline (%ΔFEV1i).19 Therefore, the results from this study add to reference values from smaller population studies from single countries18–20 and provided global reference values for the interpretation of bronchodilator testing.
Two separate approaches have been used to derive reference values for a BDR. The first method was to assume that values greater than the 95th percentile in distribution of healthy subjects was abnormal.18 The second method was to measure the short-term spontaneous variation or placebo-induced changes in FEV1 in patients.15–17 The first method was used in this study. The joint ATS-ERS guidelines10 recommendation of 12% percentage change from baseline and 200 ml absolute changes in FEV1 and/or FVC in an individual subject to identify a positive/significant BDR was derived using the second approach, but recognised the need to obtain references in healthy populations based on the first method. Thus, the results from this study provided new data relevant to this gap in information.
The ‘cutoff’ values in our analysis differ somewhat compared with those from single site population studies of healthy subjects. For defining a positive response, these studies had suggested 95th percentile thresholds of 130 ml18 or 240 ml19 for absolute change in FEV1; 9%18 or 5.9%19 for percentage change in FEV1 from initial value (%∆FEV1i) and 9%8 18 for change in FEV1 relative to predicted value (%∆FEV1p). In our study, the derived cutoffs for %∆FEV1i and %∆FEV1p are higher but stable as evidenced by the lack of site heterogeneity. Also, these threshold values complied with the caution to exceed the measurement variability of at least 8% change within individuals for defining an unambiguous response.8 30 31 The FVC thresholds were included as the ATS-ERS recommendation included these10 to accommodate flow responders and volume responders to inhaled bronchodilators.32 33 However, it is worth noting that the issue of heterogeneity is much more a concern for FVC than for FEV1, at least so long as the latter is expressed as a per cent change of initial or predicted value.
Comparison of our healthy population-based thresholds with the thresholds of guidelines based on patient studies provided insight into the short-term variability of BDR measurements. In this global study, the 95th percentile cutoffs of BDR in healthy never smokers of 12% for ΔFEV1i was identical to the cutoffs of 12% change in FEV1 or FVC for a positive response required by international guidelines,10 while 10% for ΔFEV1p was similar to the 9% change found by one study.8 The guideline recommendation for a positive BDR had been based on observations in selected patients with asthma and COPD, and on the fact that there was a short-term intra-subject variability of 200 ml in flow volume indices.34 Although the long-term variability in lung function in patients is larger than in healthy subjects, the short-term variability in patients in a stable condition is very similar to normal subjects, with an observed 95% CI of change in FEV1 of 190 ml and 12.3%.15 16 This could be a potential explanation for the similarity between threshold values in our study and the guideline recommendations.10
There is no consensus on how BDR is best expressed: in absolute terms or as percentage of the initial value,10 12 or as percentage of predicted value.13 Of the six indices of BDR in this global study, we showed that the percentage change in FEV1 relative to either baseline or predicted were the most stable across sites, while there was significant site-to-site variability in all FVC estimates and in absolute FEV1 change. Overall, this population-based evidence supports the use of 10% increase relative to predicted FEV1 to determine bronchodilator reversibility, as this feature is stable across sites, is independent of sex and stable across GOLD stages, yet discriminates healthy subjects from obstructive individuals. Nevertheless, in practice, it would be prudent to couple any percentage threshold with a qualifying volume threshold.10
This is the first study to compare BDR in population-based samples from a large number of sites on several continents. This information adds to the growing body of data on lung function that will help us to understand the range of normality and what may influence this. Other strengths of the study include the careful attention to standardisation and quality control used across all sites in the BOLD study21 22 and the well recognised technique of defining the 95th percentile in the healthy population for deriving the reference for BDR thresholds.18 19 In addition, the analysis of FVC data using different criteria is much more comprehensive than in other reports.6
A potential limitation of the study is that our definition of healthy never smokers relies on self-report of doctor-diagnosed lung disorders rather than objectively defined obstructive lung disease, since both diagnostic practices and access to care might vary across our widely dispersed sites. Nonetheless this is standard practice for developing reference equations for lung function.25 Also, we would note that only 4% of our healthy never smokers met criteria for GOLD stage 2 or higher COPD, suggesting that the results would be unlikely to change much by excluding these individuals, and indeed we confirmed this for tables 2 and 3 (data not shown). Second, because the distribution of BDRs are continuous and unimodal as had been shown in clinical studies8 9 15 and population studies,18–20 the cutoff value for a ‘positive’ response in all studies, including ours, remained somewhat arbitrary.35 Third, we used 200 μg of salbutamol/albuterol instead of higher doses as an extra precaution because it was a field study and involved home visits in many sites. While GOLD guidelines recommended 400 μg, many published clinical studies have used different types and doses of drugs as summarised in the recent paper on bronchodilator reversibility by Hanania et al.26 Lastly, we demonstrated the effect of acute reversibility due to bronchodilator in one setting but not its reproducibility on repeated testing and also not the long-term reversibility due to anti-inflammatory drugs. Hence, a lack of a response to bronchodilator testing in one setting may not preclude a clinical response to bronchodilating or anti-inflammatory therapy.10 24
In conclusion, the results from this study add new worldwide data on the distribution of bronchodilator response and airway reversibility. The reference values derived from healthy individuals addressed the reference gap in BDR. The values agreed well with the current guideline cutoffs for a significant BDR, were discriminative for different subpopulations and strengthen the applicability of these measures for global interpretation in bronchodilator testing.
Acknowledgments
BOLD wishes to acknowledge the contributions of Georg Harnoncourt of the ndd Corporation and Paul Enright for their assistance with spirometry training and quality control during the study.
Appendix 1. BOLD Collaborative Research Group
NanShan Zhong (Principal Investigator (PI)), Shengming Liu, Jiachun Lu, Pixin Ran, Dali Wang, Jingping Zheng, Yumin Zhou (Guangzhou Institute of Respiratory Diseases, Guangzhou Medical College, Guangzhou, China); Ali Kocabaş (PI), Attila Hancioglu, Ismail Hanta, Sedat Kuleci, Ahmet Sinan Turkyilmaz, Sema Umut, Turgay Unalan (Cukurova University School of Medicine, Department of Chest Diseases, Adana, Turkey); Michael Studnicka (PI), Bernd Lamprecht, Lea Schirnhofer (Paracelsus Medical University, Department of Pulmonary Medicine, Salzburg Austria); Eric Bateman (PI), Anamika Jithoo (PI), Desiree Adams, Edward Barnes, Jasper Freeman, Anton Hayes, Sipho Hlengwa, Christine Johannisen, Mariana Koopman, Innocentia Louw, Ina Ludick, Alta Olckers, Johanna Ryck, Janita Storbeck (University of Cape Town Lung Institute, Cape Town, South Africa); Thorarinn Gislason (PI), Bryndis Benedikdtsdottir, Kristin Börundsdottir, Lovisa Gudmundsdottir, Sigrun Gudmundsdottir, Gunnar Gundmundsson (Department of Allergy, Respiratory Medicine and Sleep, Landspitali University Hospital, Reykjavik, Iceland); Ewa Nizankowska-Mogilnicka (PI), Jakub Frey, Rafal Harat, Filip Mejza, Pawel Nastalek, Andrzej Pajak, Wojciech Skucha, Andrzej Szczeklik,Magda Twardowska (Division of Pulmonary Diseases, Department of Medicine, Jagiellonian University School of Medicine, Krakow, Poland); Tobias Welte (PI), Isabelle Bodemann, Henning Geldmacher, Alexandra Schweda-Linow (Hannover Medical School, Hannover, Germany); Amund Gulsvik (PI), Tina Endresen, Lene Svendsen (Department of Thoracic Medicine, Institute of Medicine, University of Bergen, Bergen, Norway); Wan C Tan (PI), Wen Wang (iCapture Center for Cardiovascular and Pulmonary Research, University of British Columbia, Vancouver, BC, Canada); David M Mannino (PI), John Cain, Rebecca Copeland, Dana Hazen, Jennifer Methvin (University of Kentucky, Lexington, Kentucky, USA); Renato B Dantes (PI), Lourdes Amarillo, Lakan U Berratio, Lenora C Fernandez, Norberto A Francisco, Gerard S. Garcia, Teresita S de Guia, Luisito F Idolor, Sullian S Naval, Thessa Reyes, Camilo C Roa, Jr, Ma. Flordeliza Sanchez, Leander P Simpao (Philippine College of Chest Physicians, Manila, Philippines); Christine Jenkins (PI), Guy Marks (PI), Tessa Bird, Paola Espinel, Kate Hardaker, Brett Toelle (Woolcock Institute of Medical Research, Sydney, Australia); Peter Burney (PI), Caron Amor, James Potts, Michael Tumilty, Fiona McLean (National Heart and Lung Institute, Imperial College, London); Christer Janson (PI), Inga Sif Olafsdottir, Katarina Nisser, Ulrike Spetz Nyström, Gunilla Hägg, Gun-Marie Bodman Lund (Department of Medical Sciences: Respiratory Medicine & Allergology, Uppsala university, Uppsala, Sweden); Peter Burney (PI), Caron Amor, James Potts, Michael Tumilty, Fiona McLean (National Heart and Lung Institute, Imperial College, London).
Footnotes
Contributors: WT and WMV had full access to all of the data in the study, and take responsibility for the integrity of the data and the accuracy of the data analysis. WT and WMV contributed to data analysis and writing the manuscript. BL, DMM, AJ, EN-M, FM, PB, TG and SB contributed to writing and revising the manuscript.
Funding: The BOLD initiative has been funded in part by unrestricted educational grants to the Operations Center (http://www.boldcopd.org) from ALTANA, Aventis, AstraZeneca, Boehringer-Ingelheim, Chiesi, GlaxoSmithKline, Merck, Novartis, Pfizer, Schering-Plough, Sepracor, and University of Kentucky. Additional local support for BOLD clinical sites was provided by: Boehringer Ingelheim China (GuangZhou, China); Turkish Thoracic Society, Boehringer-Ingelheim, and Pfizer (Adana, Turkey); Altana, Astra-Zeneca, Boehringer-Ingelheim, GlaxoSmithKline, Merck Sharpe & Dohme, Novartis, Salzburger Gebietskrankenkasse, and Salzburg Local Government (Salzburg, Austria); Research for International Tobacco Control, the International Development Research Centre, the South African Medical Research Council, the South African Thoracic Society GlaxoSmithKline Pulmonary Research Fellowship, and the University of Cape Town Lung Institute (Cape Town, South Africa); and Landspítali-University Hospital-Scientific Fund, GlaxoSmithKline Iceland, and AstraZeneca Iceland (Reykjavik, Iceland); GlaxoSmithKline Pharmaceuticals, Polpharma, Ivax Pharma Poland, AstraZeneca Pharma Poland, ZF Altana Pharma, Pliva Kraków, Adamed, Novartis Poland, Linde Gaz Polska, Lek Polska, Tarchomińskie Zakłady Farmaceutyczne Polfa, Starostwo Proszowice, Skanska, Zasada, Agencja Mienia Wojskowego w Krakowie, Telekomunikacja Polska, Biernacki, Biogran, Amplus Bucki, Skrzydlewski, Sotwin, and Agroplon (Cracow, Poland); Boehringer-Ingelheim, and Pfizer Germany (Hannover, Germany); the Norwegian Ministry of Health's Foundation for Clinical Research, and Haukeland University Hospital's Medical Research Foundation for Thoracic Medicine (Bergen, Norway); AstraZeneca, Boehringer-Ingelheim, Pfizer, and GlaxoSmithKline (Vancouver, Canada); Marty Driesler Cancer Project (Lexington, Kentucky, USA); Altana, Boehringer Ingelheim (Phil), GlaxoSmithKline, Pfizer, Philippine College of Chest Physicians, Philippine College of Physicians, and United Laboratories (Phil) (Manila, Philippines); Air Liquide Healthcare P/L, AstraZeneca P/L, Boehringer Ingelheim P/L, GlaxoSmithKline Australia P/L, Pfizer Australia P/L (Sydney, Australia); UK Department of Health's Policy Research Programme (London, UK); Swedish Heart-Lung Foundation, the Swedish Heart and Lung Association, and GlaxoSmithKline (Uppsala, Sweden). The sponsors of the study had no role in the study design, data collection, data analysis, data interpretation, or writing of the report.
Competing interests: WMV, ASB, TG, BL, ENM and WCT received funding for the BOLD study Operations Center and/or other research from unrestricted educational grants from GlaxoSmithKline, Pfizer, Boehringer Ingelheim, AstraZeneca, ALTANA, Novartis, Merck, Chiesi, Schering Plough, and Sepracor. Several authors have served on advisory boards for GlaxoSmithKline (ASB), ALTANA (ASB), Merck (ASB, WMV), Novartis (ASB). Several authors have participated in COPD workshops funded by Merck (WMV), AstraZeneca (ASB, TG), Pfizer (TG), GlaxoSmithKline (ASB, TG, WMV) and Telacris (WCT). All other authors declare they have no conflict of interest.
Ethics approval: Institutional Ethics Review Board at each study site.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: Data sharing is available via the BOLD process (through Peter Burney; e mail: p.burney@imperial.ac.uk).
References
- 1.Calverley PM, Burge PS, Spencer S, et al. Bronchodilator reversibility testing in chronic obstructive pulmonary disease. Thorax 2003;58:659–64 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dompeling E, van Schayck CP, Molema J, et al. A comparison of six different ways of expressing the bronchodilating response in asthma and COPD: reproducibility and dependence of prebronchodilator FEV1. Eur Respir J 1992;5:975–81 [PubMed] [Google Scholar]
- 3.Nicklaus TM, Burgin WW, Jr, Taylor JR. Spirometric tests to diagnose suspected asthma. Am Rev Respir Dis 1969;100:153–9 [DOI] [PubMed] [Google Scholar]
- 4.Tashkin DP, Celli B, Decramer M, et al. Bronchodilator responsiveness in patients with COPD. Eur Respir J 2008;31:742–50 [DOI] [PubMed] [Google Scholar]
- 5.Anthonisen NR, Lindgren PG, Tashkin DP, et al. Bronchodilator response in the lung health study over 11 yrs. Eur Respir J 2005;26:45–51 [DOI] [PubMed] [Google Scholar]
- 6.Hansen EF, Vestbo J. Bronchodilator reversibility in COPD: the roguish but harmless little brother of airway hyperresponsiveness? Eur Respir J 2005;26:6–7 [DOI] [PubMed] [Google Scholar]
- 7.Vestbo J, Edwards LD, Scanlon PD, et al. Changes in forced expiratory volume in 1 second over time in COPD. N Engl J Med 2011;365:1184–92 [DOI] [PubMed] [Google Scholar]
- 8.Brand PL, Quanjer PH, Postma DS, et al. Interpretation of bronchodilator response in patients with obstructive airways disease. The Dutch Chronic Non-Specific Lung Disease (CNSLD) Study Group. Thorax 1992;47:429–36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Eliasson O, Degraff AC., Jr The use of criteria for reversibility and obstruction to define patient groups for bronchodilator trials. Influence of clinical diagnosis, spirometric, and anthropometric variables. Am Rev Respir Dis 1985;132:858–64 [DOI] [PubMed] [Google Scholar]
- 10.Pellegrino R, Viegi G, Brusasco V, et al. Interpretative strategies for lung function tests. Eur Respir J 2005;26:948–68 [DOI] [PubMed] [Google Scholar]
- 11.Lehmann S, Vollset SE, Nygaard HA, et al. Factors determining performance of bronchodilator reversibility tests in middle-aged and elderly. Respir Med 2004;98:1071–9 [DOI] [PubMed] [Google Scholar]
- 12.Anonymous. Lung function testing: selection of reference values and interpretative strategies. American Thoracic Society. Am Rev Respir Dis 1991;144:1202–18 [DOI] [PubMed] [Google Scholar]
- 13.Quanjer PH, Tammeling GJ, Cotes JE, et al. Lung volumes and forced ventilatory flows. Report Working Party Standardization of Lung Function Tests, European Community for Steel and Coal. Official Statement of the European Respiratory Society. Eur Respir J Suppl 1993;16:5–40 [PubMed] [Google Scholar]
- 14.Anonymous. Criteria for the assessment of reversibility in airways obstruction. Report of the Committee on Emphysema American College of Chest Physicians. Chest 1974;65:552–3 [DOI] [PubMed] [Google Scholar]
- 15.Sourk RL, Nugent KM. Bronchodilator testing: confidence intervals derived from placebo inhalations. Am Rev Respir Dis 1983;128:153–7 [DOI] [PubMed] [Google Scholar]
- 16.Tweeddale PM, Alexander F, McHardy GJ. Short term variability in FEV1 and bronchodilator responsiveness in patients with obstructive ventilatory defects. Thorax 1987;42:487–90 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tweeddale PM, Merchant S, Leslie M, et al. Short term variability in FEV1: relation to pretest activity, level of FEV1, and smoking habits. Thorax 1984;39:928–32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dales RE, Spitzer WO, Tousignant P, et al. Clinical interpretation of airway response to a bronchodilator. Epidemiologic considerations. Am Rev Respir Dis 1988;138:317–20 [DOI] [PubMed] [Google Scholar]
- 19.Kainu A, Lindqvist A, Sarna S, et al. FEV1 response to bronchodilation in an adult urban population. Chest 2008;134:387–93 [DOI] [PubMed] [Google Scholar]
- 20.Lehmann S, Bakke PS, Eide GE, et al. Bronchodilator reversibility testing in an adult general population; the importance of smoking and anthropometrical variables on the response to a beta2-agonist. Pulm Pharmacol Ther 2006;19:272–80 [DOI] [PubMed] [Google Scholar]
- 21.Buist AS, McBurnie MA, Vollmer WM, et al. International variation in the prevalence of COPD (the BOLD Study): a population-based prevalence study. Lancet 2007;370:741–50 [DOI] [PubMed] [Google Scholar]
- 22.Buist AS, Vollmer WM, Sullivan SD, et al. The Burden of Obstructive Lung Disease initiative (BOLD): rationale and design. COPD 2005;2:277–83 [PubMed] [Google Scholar]
- 23.Crapo RO, Hankinson JL, Irvin C, et al. Standardization of spirometry, 1994 update. American Thoracic Society. Am J Respir Crit Care Med 1995;152:1107–36 [DOI] [PubMed] [Google Scholar]
- 24.GOLD-Global Initiative for Chronic Obstructive Lung Disease Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. 2010. http://www.goldcopd.org/uploads/users/files/GOLDReport_April112011.pdf (accessed 25 Apr 2012). [Google Scholar]
- 25.Hankinson JL, Odencrantz JR, Fedan KB. Spirometric reference values from a sample of the general U.S. population. Am J Respir Crit Care Med 1999;159:179–87 [DOI] [PubMed] [Google Scholar]
- 26.Hanania NA, Celli BR, Donohue JF, et al. Bronchodilator reversibility in COPD. Chest 2011;140:1055–63 [DOI] [PubMed] [Google Scholar]
- 27.Kesten S, Rebuck AS. Is the short-term response to inhaled beta-adrenergic agonist sensitive or specific for distinguishing between asthma and COPD? Chest 1994;105:1042–5 [DOI] [PubMed] [Google Scholar]
- 28.Anthonisen NR, Wright EC. Bronchodilator response in chronic obstructive pulmonary disease. Am Rev Respir Dis 1986;133:814–19 [PubMed] [Google Scholar]
- 29.Watanabe S, Renzetti AD, Jr, Begin R, et al. Airway responsiveness to a bronchodilator aerosol. I. Normal human subjects. Am Rev Respir Dis 1974;109:530–7 [DOI] [PubMed] [Google Scholar]
- 30.Enright PL, Beck KC, Sherrill DL. Repeatability of spirometry in 18,000 adult patients. Am J Respir Crit Care Med 2004;169:235–8 [DOI] [PubMed] [Google Scholar]
- 31.Guyatt GH, Townsend M, Nogradi S, et al. Acute response to bronchodilator. An imperfect guide for bronchodilator therapy in chronic airflow limitation. Arch Intern Med 1988;148:1949–52 [DOI] [PubMed] [Google Scholar]
- 32.Schermer T, Heijdra Y, Zadel S, et al. Flow and volume responses after routine salbutamol reversibility testing in mild to very severe COPD. Respir Med 2007;101:1355–62 [DOI] [PubMed] [Google Scholar]
- 33.Walker PP, Calverley PM. The volumetric response to bronchodilators in stable chronic obstructive pulmonary disease. COPD 2008;5:147–52 [DOI] [PubMed] [Google Scholar]
- 34.Hankinson JL, Bang KM. Acceptability and reproducibility criteria of the American Thoracic Society as observed in a sample of the general population. Am Rev Respir Dis 1991;143:516–21 [DOI] [PubMed] [Google Scholar]
- 35.Pride NB, Vermeire P, Allegra L. Diagnostic labels applied to model case histories of chronic airflow obstruction. Responses to a questionnaire in 11 North American and Western European countries. Eur Respir J 1989;2:702–9 [PubMed] [Google Scholar]