Abstract
Background
Physicians often do not recognize when their patients are overweight and infrequently counsel them about weight loss.
Objective
To evaluate a set of electronic health record (EHR)-embedded tools to assist with identification and counseling of overweight patients.
Design
Randomized controlled trial.
Participants
Physicians at an academic general internal medicine clinic were randomized to activation of the EHR tools (n = 15) or to usual care (n = 15). Patients of these physicians were included in analyses if they had a body mass index (BMI) between 27 and 29.9 kg/m2.
Intervention
The EHR tool set included: a physician point-of-care alert for overweight (BMI 27–29. 9 kg/m2); a counseling template to help physicians counsel patients on action plans; and an order set to facilitate entry of overweight as a diagnosis and to order relevant patient handouts.
Main Measures
Physician documentation of overweight as a problem; documentation of weight-specific counseling; physician perceptions of the EHR tools; patient self-reported progress toward their goals and perspectives about counseling received.
Key Results
Patients of physicians receiving the intervention were more likely than those of usual care physicians to receive a diagnosis of overweight (22% vs. 7%; p = 0.02) and weight-specific counseling (27% vs. 15%; p = 0.02). Most patients receiving counseling in the intervention group reported increased motivation to lose weight (90%) and taking steps toward their goal (93%). Most intervention physicians agreed that the tool alerted them to patients they did not realize were overweight (91%) and improved the effectiveness of their counseling (82%); more than half (55%) reported counseling overweight patients more frequently (55%). However, most physicians used the tool infrequently because of time barriers.
Conclusions
EHR-based alerts and management tools increased documentation of overweight and counseling frequency; the majority of patients for whom the tools were used reported short-term behavior change.
KEY WORDS: overweight, counseling, electronic health record
BACKGROUND
One third of adults in the United States are overweight, defined as body mass index [BMI] 25–29.9 kg/m2. Overweight adults are at increased risk for developing hypertension and diabetes, and of becoming obese.1–3 While intensive efforts to manage obesity have resulted in relatively modest and un-sustained weight loss, prevention of obesity among overweight non-obese patients may be more effective because overweight patients are less likely to recognize themselves as overweight, have less weight to lose, and could consider weight maintenance as a reasonable goal.2,4,5
Physician acknowledgement of patients’ overweight status and advice to lose weight increase the accuracy of patient weight perceptions, attempts to lose weight, and weight loss.6–8 However, advice is delivered in only 13% of visits with overweight patients.9,10 Physicians also rarely provide guidance on how to achieve weight loss.11 Barriers to weight counseling include failure to recognize that patients are overweight, time constraints, insufficient training, and limited access to weight loss tools.12 Electronic health record (EHR) systems have the potential to overcome these barriers through computerized decision support tools to remind physicians to counsel overweight patients and linked resources to facilitate a structured, evidence-based approach to counseling.13,14 The purpose of this study was to evaluate a set of electronic tools to assist with identification and counseling of overweight patients in a general internal medicine (GIM) clinic. We hypothesized that the tools would increase physician documentation of overweight, increase documented weight counseling and goal-setting among overweight patients, and facilitate patient progress toward their goals.
METHODS
Setting and Participants
This study was conducted at the Northwestern Medical Faculty Foundation (NMFF) GIM clinic (Chicago, IL), an academic clinic with 40 physicians and a volume of >60,000 patient visits yearly. The clinic is supported by a commercial EHR (EpicCare, Epic Systems Corporation, Verona, WI). Physicians in the practice already had several years of experience utilizing point-of-care reminders within EPIC for preventive care and chronic disease management. Physicians who saw patients for at least 8 hours per week (exclusive of study investigators, n = 2) were approached for participation and informed consent (n = 35). Eligible patients were adults ages 18–65 who had a visit with a consenting physician during the 6 month study period (March 19–September 20, 2010), and whose most recently measured weight and height corresponded to a calculated BMI 27–29.9 kg/m2. We limited inclusion to individuals with a BMI 27–29.9 kg/m2 to focus on overweight individuals who were at highest risk for weight-related complications and most likely to progress to obesity. The Northwestern University Institutional Review Board granted a waiver of informed consent to identify and review electronic charts of patients who were overweight at the time of their visit to a consenting physician.
Randomization
Consenting physicians were randomized, stratified by gender,15,16 to activation of the electronic tool set or usual care (Fig. 1). Intervention physicians received access to a tool set including: 1) a point-of-care alert for overweight; 2) a counseling template to help patients make an action plan; and 3) an order set to assist with entry of overweight as a diagnosis and to order relevant handouts. To promote physician uptake of the tool, we sought feedback from physicians on the NMFF GIM Quality Committee regarding tool design. Intervention physician participants received a 1 hour group training session on tool usage and were offered an additional optional one-on-one hands-on 20 minute booster session. Physicians were encouraged to utilize the tools by a local physician champion (JT); no financial incentives were provided. Given the nature of the intervention, it was not possible to blind physicians to group assignment.
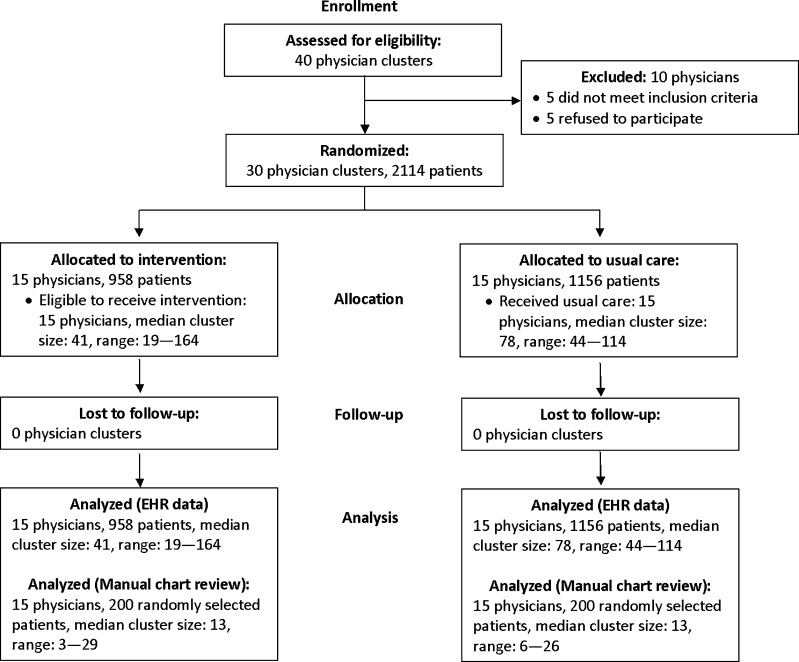
Figure 1.
Consort diagram for cluster randomized trials depicting the flow of physician clusters and patients through eligibility, assessment, randomization, intervention, and outcome analysis.
Intervention
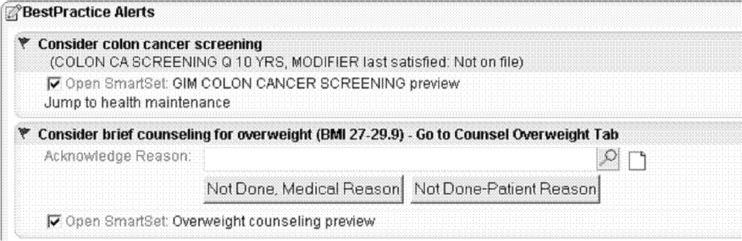
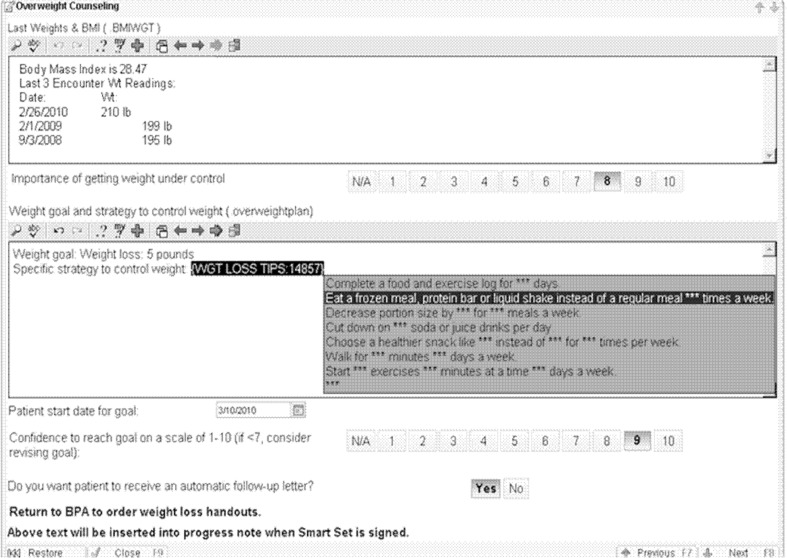
A point-of-care alert for overweight was designed as a passive prompt within the patient’s medical record (Fig. 2). Upon viewing the alert, physicians were directed to open the counseling template (Fig. 3), which supported evidence-based weight-related counseling through goal-setting and action planning.17,18 The template guided physicians through assessing the patient’s rated importance of weight management, setting a target weight, selecting from a list of specific strategies to control weight, and assessing the patient’s confidence to adhere to the selected strategies. The template included a list of effective strategies for weight loss often overlooked by physicians (e.g., logging diet and use of meal replacements).19 After completing the template, physicians could open an order set that facilitated entry of overweight as a diagnosis, imported the template information into the physician note, and enabled ordering of handouts specific to a patient’s chosen goals.
Figure 2.
Point-of-Care Best Practice Alert: Best Practice Alerts are passive point-of-care alerts within the patient medical record which notify physicians when preventive or chronic disease management quality care metrics have not been satisfied. We created a point-of-care alert within this existing system for brief counseling for overweight. The alert directs physicians to first go to the “Counsel Overweight Tab” to open the counseling template, and then to subsequently open a linked order set (“Smart Set”).
Figure 3.
Counseling Template: The counseling template opens upon clicking on the “Counsel Overweight Tab.” The template guides physicians through reviewing the patient’s last three recorded weights, assessing the patient’s rated importance of getting weight under control, setting a target weight, selecting from a list of specific strategies to control weight, assessing the patient’s confidence to reach the goal, and opting to have a follow-up letter sent to the patient regarding their specific goals. Physicians can use commands to pull in relevant text and drop down menus within each text box.
Measures
Primary outcomes were physician documentation of overweight as a diagnosis and counseling for overweight. These outcomes were assessed through manual chart review for a random sample of patients with BMI 27-29.9 kg/m2 who had a visit with an intervention or control physician during the study period (n = 200 per group). Patients were categorized as receiving a diagnosis of overweight if overweight was listed as an encounter diagnosis or problem in the assessment and plan. Documentation of weight-specific counseling was categorized based on presence or absence of a documented recommendation for weight loss or maintenance. In addition, we conducted an electronic query for entry of appropriate ICD9 code for overweight (278.02) as an encounter diagnosis for all qualifying visits with which to corroborate manual chart review results. We were unable to electronically query for weight-related counseling because CPT codes for preventive counseling (e.g., V65.3 Dietary surveillance and counseling) are rarely used. Visit type was categorized as: 1) new visit if a patient had a 40 minute visit to establish care, 2) preventive visit if the primary diagnosis code was for an annual physical exam (V70.0) or a patient’s stated chief complaint was annual physical,20 3) other visit if a patient was seen by his or her usual physician for a non-preventive care visit, and 4) acute visit if a patient had an urgent complaint and was seen by a physician other than their primary care physician. Patients were categorized as having a weight-related co-morbid condition if they had a recorded diagnosis of hypertension, hyperlipidemia, diabetes mellitus, coronary artery disease, peripheral vascular disease, or obstructive sleep apnea.
For each intervention physician, we assessed frequency of tool usage, defined as the number of patients for whom the counseling template or order set was used divided by the number of eligible patients. When the tool was used, we assessed frequency of documenting overweight as an encounter diagnosis and an action plan. These data were assessed via electronic query of the enterprise data warehouse (EDW). After 6 months, intervention physicians completed an anonymous survey assessing perceptions of the EHR tools. Physicians rated agreement (1 = strongly disagree; 5 = strongly agree) with the tool helping to identify more overweight patients, improve counseling effectiveness, and increase counseling frequency. Physicians rank ordered barriers to tool use (time, tool is complicated, patient and/or personal disinterest in discussing weight).
We queried the EDW weekly to identify patients counseled using the EHR tools. These patients were contacted by phone approximately 3 weeks after their appointment; verbal informed consent was requested to participate in a structured follow-up phone interview. At least 4 attempts were made to contact each patient. Patients were asked if they recalled the conversation regarding weight, their self-assessed weight status (underweight, about the right weight, or overweight), to identify their goals set, and to rate their progress toward these goals (1 = Not started working toward the goal(s); 5 = I am doing better than I said). Patients were asked to report if their weight had changed; those reporting weight loss were asked to quantify the weight loss. Patients rated how seriously they previously had thought about modifying their diet and exercise patterns (1 = Not at all seriously; 4 = Very seriously) and if they had made changes in their diet or activity prior to the visit (1 = Strongly disagree; 5 = Strongly agree). Patients were asked to rate their agreement (1 = Strongly disagree; 5 = Strongly agree) with physician counseling being helpful, being more motivated to manage their weight, and making lifestyle changes due to counseling; a response of 4 or 5 (somewhat/strongly agree) was categorized as agreement with the statement. Qualitative responses were solicited regarding general perceptions of counseling received and specific aspects of the intervention perceived to be useful.
Data Analyses
Descriptive statistics were used to characterize all outcomes. Baseline characteristics for patients of intervention and control physicians were compared using chi-square or t-tests as appropriate. We used logistic regression to compare frequency of diagnosis and counseling for overweight among intervention and control groups. P values were adjusted for clustering of patients within physicians’ practices; the intra-class correlation coefficient was 0.11 for documented diagnosis of overweight and 0.07 for weight specific counseling. Examples of representative qualitative responses are presented. Qualitative comments from patient interviews were reviewed by a single individual (JT). Specific factors contributing to the usefulness of the counseling were individually noted and tallied if mentioned by multiple participants.
RESULTS
Baseline Sample Characteristics
Thirty physicians (85%) consented to participate, and were randomized to receive access to the EHR tools (n = 15) or serve as usual care controls (n = 15) (Fig. 1). During the 6-month study period, 1,156 unique control group and 958 unique intervention group patients were seen. Of these, 200 patients from each group were randomly selected for chart review; selected patients did not differ by age, gender, BMI, presence of a weight-related co-morbid condition, or visit type (Table 1).
Table 1.
Demographic and Visit Characteristics of 400 Randomly Sampled Intervention and Control Group Patients*
| Intervention (n = 200) | Control (n = 200) | |
|---|---|---|
| Age, years [mean (SD)] | 46.4 (10.8) | 46.8 (12.0) |
| BMI (kg/m2) [mean (SD)] | 28.2 (2.5) | 28.4 (1.3) |
| % Female | 48.5 | 54.5 |
| Weight-related co-morbid condition (%) | 48.5 | 56.5 |
| Visit type | ||
| New/preventive (%) | 28.5 | 33.0 |
| Acute (%) | 16.5 | 22.5 |
| Other (%) | 55.0 | 44.5 |
*Comparisons between intervention and control groups were tested using t-tests (age, BMI) and chi-square tests (gender). There were no statistically significant differences between the groups (p > 0.05 for all comparisons)
Physician Documentation of Overweight and Weight-related Counseling
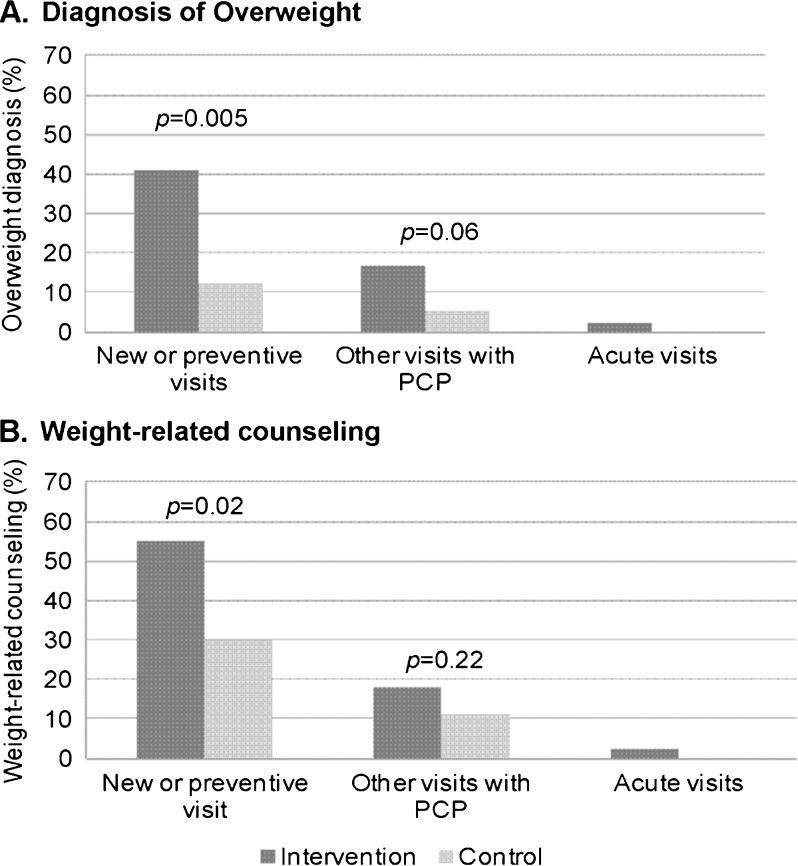
Based on electronic query of all eligible patients, patients of intervention physicians were more likely than patients of control physicians to receive an ICD9 diagnosis of overweight (17% vs. 4.8%; OR = 4.1, 95% CI 1.3 to 12.7; p = 0.02). Chart review yielded marginally higher diagnosis rates in both groups (21.5% vs. 6.5%; OR = 3.9, 95% CI 1.3 to 12.1]; p = 0.02). Chart review revealed that patients of intervention physicians were more likely than patients of control physicians to receive weight-specific counseling (26.5% vs. 14.5%; OR = 2.1, 95% CI 1.1 to 4.1; p = 0.02) (Fig. 4). Both higher overall rates and greater differences in rates of diagnosis of overweight and weight-specific counseling were observed among intervention and control patients presenting for new or preventive visits compared to acute or other visits (Fig. 4). Patients with weight-related co-morbid conditions were no more likely to receive a diagnosis of overweight or weight-specific counseling. The counseling template and order set were utilized by intervention physicians for 40% of the encounters during which weight-specific counseling was documented.
Figure 4.
Frequency of physician identification and counseling for overweight by visit type. The p values comparing intervention and control group physicians were calculated using logistic regression with adjustment for clustering. The intra-class correlation coefficient was calculated to be 0.11 for documented diagnosis of overweight and 0.07 for weight-specific counseling. Of the 400 charts reviewed, the breakdown by visit type was 123 new/preventive visits, 199 other visits with PCP, and 89 acute visits not with the PCP.
Tool Usage Among Intervention Physicians
The counseling template and order set were used in response to 10.7% of alerts. Usage decreased over time (11.8% for first 3 months vs. 7.9% during subsequent 3 months, p = 0.03) and was higher among female physicians (13.7% female physicians vs. 4.5% male physicians, p < 0.001). There was substantial variability in usage of the counseling template and order set among individual physicians. A subgroup of five physicians used these tools more frequently than others (i.e., 18–35% of eligible patients). Three physicians never used the tools. When the counseling template and order set were used, physicians nearly always entered overweight as an encounter diagnosis (97%) and documented an action plan (98%).
Intervention Physician Perspectives Regarding the EHR Tool
Eleven of 15 intervention physicians responded to an anonymous survey (73% response rate). All respondents reported using the EHR tool at least once. Most agreed that the tool alerted them to patients they did not realize were overweight (91%) and improved the effectiveness of their counseling (82%). Over half (55%) agreed that the tool increased their counseling frequency. Physicians estimated the tool required 7.5 minutes to use, and rated time as the most important barrier to tool use. Other barriers included tool complexity, and patient disinterest. Only one physician ranked personal disinterest as a top barrier to counseling.
Self-reported Outcomes Among Patients Counseled Using EHR Tools
Of the 104 patients who received counseling utilizing the EHR tools, 61 completed phone interviews (59% response rate). Compared with non-responders, responders were slightly older (mean age 47.1 vs. 40.2 years, p < 0.003), and more likely to be male (46% vs. 33%, p = 0.06). Among patients surveyed, 98% considered themselves overweight. Virtually all patients recalled discussing weight with their physician (98%); 73% reported the conversation was initiated by their physician or mutually initiated. The majority recalled setting a weight management plan (93%), and taking steps toward their plan (93%). Fifty-six percent of patients reported losing weight, with the median reported weight loss of 4 lbs. Most patients reported having thought seriously about making changes to their lifestyle prior to the office visit (93%) and had taken steps toward improving their diet or physical activity (79%); however, 94% patients still perceived benefit from physician counseling. Specifically, 90% of patients reported increased motivation and 84% reported new changes in their diet or physical activity. Themes of increased motivation and commitment were highlighted in patients’ qualitative comments (n = 10). A 43 year-old man stated, “I’ve been thinking about trying to lose weight for a while, but just needed an extra push.” A 38 year-old woman remarked, “After talking with my doctor, I feel more committed to losing weight.” Patients cited being provided concrete options from which to select a specific action plan (n = 3), setting up a follow-up appointment (n = 2), and being queried about confidence level (n = 1) as useful counseling strategies.
DISCUSSION
In this study, EHR-based alerts and management tools increased documentation of overweight and frequency of counseling. The counseling rate seen in our control group was comparable to nationally reported frequencies for overweight non-obese adults.9,10 Among patients for whom the tools were used, the vast majority reported short-term behavior change and positive attitudes about the intervention. To our knowledge, this randomized controlled trial is the first to evaluate the impact of EHR tools on physician weight-related counseling. Although the increase in diagnosis and counseling was modest, if reproducible at other sites it has potential for a substantial public health impact.
Our intervention was most effective within the context of new or preventive visits; more than 50% of these patients seen by intervention physicians received counseling about weight. The differential benefit seen for these visits may be due to their pre-specified focus on preventive health or the longer visit duration (i.e., 40 minutes versus 20 minutes for other visits),21,22 whereas competing demands and time constraints may have made weight-related counseling infeasible for other types of visits. However, for patients unlikely to present for annual visits (e.g., men under age 45),20 routine visits for low acuity issues may be the only chance to identify and counsel overweight patients.23,24
Although intervention physicians more frequently diagnosed and counseled for overweight, overall usage of the counseling template and order set were low. Physicians noted that the alert frequently increased their recognition of weight as a health problem, yet time constraints remained the main barrier to tool usage. Physicians estimated that tool usage required 7.5 minutes; national surveys indicate physicians are only willing to devote 1 minute to prevention during a typical visit.25 Strategies such as bringing back interested patients for a visit devoted to weight management may address such perceived time barriers. However, payment mechanisms (i.e., reimbursement for weight-related counseling for obesity prevention) would need to be re-aligned for this strategy to be feasible. An alternative approach is to build support systems that decrease the time needed for physicians to effectively counsel patients, for instance through pre-activation and preparation of patients prior to visits.26
Contrary to concerns that patients may be offended by their physicians bringing up a discussion about weight, patients were highly receptive to counseling, reporting that counseling increased motivation and commitment to making lifestyle changes. This study adds to the growing literature on goal setting and action planning within primary care quality improvement initiatives, which has shown similarly high rates of progress toward goals related to diet, exercise, and medication adherence.27,28 Informing physicians of patients’ receptivity to counseling and resultant attempts to change behaviors may provide motivation to counsel more frequently.
This study has several limitations. The study was completed at a single academic institution with a strong culture of quality improvement and physicians who are highly experienced EHR users. Although baseline diagnosis and counseling rates for individual providers are not available, our prior work within this clinic suggests that overall rates are low (Tang et al., unpublished data). Because physicians were randomly assigned to intervention and control groups, baseline diagnosis and counseling rates were likely relatively balanced. Only intervention physicians received brief education regarding weight-related counseling focused on electronic tool usage; however, prior studies have demonstrated that brief educational sessions in isolation from systemic supports have minimal impact on physician counseling patterns.29–31 Attitudes of intervention physicians who did not use the tools are not known since these individuals did not complete the survey. We did not review all available charts due to time and resource limitations; our sample size was adequately powered to detect a significant difference between groups. Only marginal differences were observed in diagnosis rates when comparing electronic and manual query results. Patient outcomes were self-reported, short-term, and may have been subject to social desirability bias; in addition, physicians may have chosen to use the EHR tools among a more motivated patient group, which would lead us to overestimate the effect of the intervention on patient attitudes and behaviors. Future studies will need to assess whether EHR tools can contribute to verified weight loss. We did not interview control group patients or patients of intervention physicians who were counseled without the use of the EHR tool. Therefore, we cannot determine if patient-reported behavior change was due to the alert alone, the counseling tools, or was self-motivated due to increased attention to health around the time of a doctor’s visit.
In summary, this study demonstrates that EHR-based alerts and management tools have potential to increase documentation of overweight, frequency of counseling, and short-term behavior change. As new health care reform legislation places increasing emphasis on promoting universal adoption and meaningful use of EHRs,32 this research will help inform the inclusion of behavioral measures within meaningful use criteria to improve recognition and counseling for weight management.
Acknowledgements
Dr. Tang was supported by an institutional award from the Agency for Health care Research and Quality, T-32 HS 000078 training grant. These results were previously presented at the 2011 SGIM National Meeting in Phoenix, AZ, for which the abstract was selected as a finalist for the Mack Lipkin Sr. Associate Member Award.
Conflict of Interest
The authors declare that they do not have a conflict of interest.
References
- 1.McTigue KM, Garrett JM, Popkin BM. The natural history of the development of obesity in a cohort of young U.S. adults between 1981 and 1998. Ann Intern Med. 2002;136(12):857–864. doi: 10.7326/0003-4819-136-12-200206180-00006. [DOI] [PubMed] [Google Scholar]
- 2.McTigue KM, Harris R, Hemphill B, et al. Screening and interventions for obesity in adults: summary of the evidence for the U.S. Preventive Services Task Force. Ann Intern Med. 2003;139(11):933–949. doi: 10.7326/0003-4819-139-11-200312020-00013. [DOI] [PubMed] [Google Scholar]
- 3.Vasan RS, Pencina MJ, Cobain M, Freiberg MS, D'Agostino RB. Estimated risks for developing obesity in the Framingham Heart Study. Ann Intern Med. 2005;143(7):473–480. doi: 10.7326/0003-4819-143-7-200510040-00005. [DOI] [PubMed] [Google Scholar]
- 4.Chang VW, Christakis NA. Self-perception of weight appropriateness in the United States. Am J Prev Med. 2003;24(4):332–339. doi: 10.1016/S0749-3797(03)00020-5. [DOI] [PubMed] [Google Scholar]
- 5.Gregory CO, Blanck HM, Gillespie C, Maynard LM, Serdula MK. Perceived health risk of excess body weight among overweight and obese men and women: differences by sex. Prev Med. 2008;47(1):46–52. doi: 10.1016/j.ypmed.2008.01.008. [DOI] [PubMed] [Google Scholar]
- 6.Post RE, Mainous AG, 3rd, Gregorie SH, Knoll ME, Diaz VA, Saxena SK. The influence of physician acknowledgment of patients' weight status on patient perceptions of overweight and obesity in the United States. Arch Intern Med. 2011;171(4):316–321. doi: 10.1001/archinternmed.2010.549. [DOI] [PubMed] [Google Scholar]
- 7.Rodondi N, Humair JP, Ghali WA, et al. Counselling overweight and obese patients in primary care: a prospective cohort study. Eur J Cardiovasc Prev Rehabil. 2006;13(2):222–228. doi: 10.1097/01.hjr.0000209819.13196.a4. [DOI] [PubMed] [Google Scholar]
- 8.Tsai AG, Wadden TA. Treatment of obesity in primary care practice in the United States: a systematic review. J Gen Intern Med. 2009;24(9):1073–1079. doi: 10.1007/s11606-009-1042-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ruser CB, Sanders L, Brescia GR, et al. Identification and management of overweight and obesity by internal medicine residents. J Gen Intern Med. 2005;20(12):1139–1141. doi: 10.1111/j.1525-1497.2005.0263.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Waring ME, Roberts MB, Parker DR, Eaton CB. Documentation and management of overweight and obesity in primary care. J Am Board Fam Med. 2009;22(5):544–552. doi: 10.3122/jabfm.2009.05.080173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Milder IE, Blokstra A, Groot J, Dulmen S, Bemelmans WJ. Lifestyle counseling in hypertension-related visits–analysis of video-taped general practice visits. BMC Fam Pract. 2008;9:58. doi: 10.1186/1471-2296-9-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kushner RF. Barriers to providing nutrition counseling by physicians: a survey of primary care practitioners. Prev Med. 1995;24(6):546–552. doi: 10.1006/pmed.1995.1087. [DOI] [PubMed] [Google Scholar]
- 13.Rattay KT, Ramakrishnan M, Atkinson A, Gilson M, Drayton V. Use of an electronic medical record system to support primary care recommendations to prevent, identify, and manage childhood obesity. Pediatrics. 2009;123(Suppl 2):S100–S107. doi: 10.1542/peds.2008-1755J. [DOI] [PubMed] [Google Scholar]
- 14.Krist AH, Woolf SH, Frazier CO, et al. An electronic linkage system for health behavior counseling effect on delivery of the 5A's. Am J Prev Med. 2008;35(5 Suppl):S350–S358. doi: 10.1016/j.amepre.2008.08.010. [DOI] [PubMed] [Google Scholar]
- 15.Flocke SA, Gilchrist V. Physician and patient gender concordance and the delivery of comprehensive clinical preventive services. Med Care. 2005;43(5):486–492. doi: 10.1097/01.mlr.0000160418.72625.1c. [DOI] [PubMed] [Google Scholar]
- 16.Frank E, Segura C, Shen H, Oberg E. Predictors of Canadian physicians' prevention counseling practices. Can J Public Health. 2010;101(5):390–395. doi: 10.1007/BF03404859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lorig K. Action planning: a call to action. J Am Board Fam Med. 2006;19(3):324–325. doi: 10.3122/jabfm.19.3.324. [DOI] [PubMed] [Google Scholar]
- 18.Lorig KR, Holman H. Self-management education: history, definition, outcomes, and mechanisms. Ann Behav Med. 2003;26(1):1–7. doi: 10.1207/S15324796ABM2601_01. [DOI] [PubMed] [Google Scholar]
- 19.Phelan S, Nallari M, Darroch FE, Wing RR. What do physicians recommend to their overweight and obese patients? J Am Board Fam Med. 2009;22(2):115–122. doi: 10.3122/jabfm.2009.02.080081. [DOI] [PubMed] [Google Scholar]
- 20.Mehrotra A, Zaslavsky AM, Ayanian JZ. Preventive health examinations and preventive gynecological examinations in the United States. Arch Intern Med. 2007;167(17):1876–1883. doi: 10.1001/archinte.167.17.1876. [DOI] [PubMed] [Google Scholar]
- 21.Chen LM, Farwell WR, Jha AK. Primary care visit duration and quality: does good care take longer? Arch Intern Med. 2009;169(20):1866–1872. doi: 10.1001/archinternmed.2009.341. [DOI] [PubMed] [Google Scholar]
- 22.McAlpine DD, Wilson AR. Trends in obesity-related counseling in primary care: 1995-2004. Med Care. 2007;45(4):322–329. doi: 10.1097/01.mlr.0000254575.19543.01. [DOI] [PubMed] [Google Scholar]
- 23.Cohen D, DiCicco-Bloom B, Strickland PO, et al. Opportunistic approaches for delivering preventive care in illness visits. Prev Med. 2004;38(5):565–573. doi: 10.1016/j.ypmed.2003.11.013. [DOI] [PubMed] [Google Scholar]
- 24.Stange KC, Flocke SA, Goodwin MA. Opportunistic preventive services delivery. Are time limitations and patient satisfaction barriers? J Fam Pract. 1998;46(5):419–424. [PubMed] [Google Scholar]
- 25.Stange KC, Woolf SH, Gjeltema K. One minute for prevention: the power of leveraging to fulfill the promise of health behavior counseling. Am J Prev Med. 2002;22(4):320–323. doi: 10.1016/S0749-3797(02)00413-0. [DOI] [PubMed] [Google Scholar]
- 26.Bodenheimer T. Helping patients improve their health-related behaviors: what system changes do we need? Dis Manag. 2005;8(5):319–330. doi: 10.1089/dis.2005.8.319. [DOI] [PubMed] [Google Scholar]
- 27.Bodenheimer T, Handley MA. Goal-setting for behavior change in primary care: an exploration and status report. Patient Educ Couns. 2009;76(2):174–180. doi: 10.1016/j.pec.2009.06.001. [DOI] [PubMed] [Google Scholar]
- 28.Handley M, MacGregor K, Schillinger D, Sharifi C, Wong S, Bodenheimer T. Using action plans to help primary care patients adopt healthy behaviors: a descriptive study. J Am Board Fam Med. 2006;19(3):224–231. doi: 10.3122/jabfm.19.3.224. [DOI] [PubMed] [Google Scholar]
- 29.Jay M, Schlair S, Caldwell R, Kalet A, Sherman S, Gillespie C. From the patient's perspective: the impact of training on resident physician's obesity counseling. J Gen Intern Med. 2010;25(5):415–22 [DOI] [PMC free article] [PubMed]
- 30.Ockene IS, Hebert JR, Ockene JK, Merriam PA, Hurley TG, Saperia GM. Effect of training and a structured office practice on physician-delivered nutrition counseling: the Worcester-Area Trial for Counseling in Hyperlipidemia (WATCH) Am J Prev Med. 1996;12(4):252–258. [PubMed] [Google Scholar]
- 31.Puczynski S, Phelps K, Wilke A. Collaborative goal setting to improve lifestyle behaviors: lessons learned from NOPCRN. Ann Fam Med. 2005;3 Suppl 2:S60–S62. doi: 10.1370/afm.364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jha AK. Meaningful use of electronic health records: the road ahead. JAMA. 2010;304(15):1709–1710. doi: 10.1001/jama.2010.1497. [DOI] [PubMed] [Google Scholar]