Abstract
Bone is a target in many inflammatory rheumatic diseases. Inflammation leads to a wide range of changes in bone, and especially bone remodeling. In ankylosing spondylitis (AS) bone loss has been documented, but measuring bone density in the spine is hampered by new bone formation in syndesmophytes, periost and within the vertebrae. The risk of vertebral fractures is increased in AS. The diagnosis of vertebral fractures requires imaging and adequate evaluation of vertebral heights. In addition, in the ankysosed spine segments, additional imaging is often needed to diagnose spinal fractures at unusual locations (cervical spine) or in the posterior arch structures. Risk factors for vertebral fractures are helpful for case finding. Fracture prevention is indicated in high risk patients with AS, especially when they have already a vertebral fracture or in the presence of osteoporosis.
Keywords: osteoporosis, epidemiology, fractures, ankylosing spondylitis
Introduction
Bone is a target in many inflammatory rheumatic diseases, including rheumatoid arthritis (RA) and ankylosing spondylitis (AS). Inflammation leads to a wide range of changes in bone, and especially bone remodeling. Although this is well recognized to lead to an increased risk of fractures in RA, AS has been less well studied [Geusens and Lems, 2011; Roux, 2011]
AS belongs to the group of spondyloarthropathies (SpAs), which also includes psoriatic arthritis, SpA associated with inflammatory bowel disease, reactive arthritis, juvenile-onset SpA and undifferentiated SpA. This review will focus on some recent data on what is known about the bony changes that occur in AS with particular reference to osteoporosis and fractures.
Bone changes in AS
Bone is a major target in AS. Inflammation results in intravertebral bone loss and bone erosions, and, in contrast to RA, is followed by bone formation within and outside bone. On imaging of the spine, this results in bone edema, which reflects replacement of bone marrow by inflammation, bone erosions with subchondral sclerosis and intravertebral bone loss. New bone formation is found below and within bone erosions, and in the ligamentous structures between the vertebrae at the anterior and posterior longitudinal ligaments, in the other interspinal ligaments and in the intervertebral discs (Figure 1) [Cawley et al. 1972].
Figure 1.
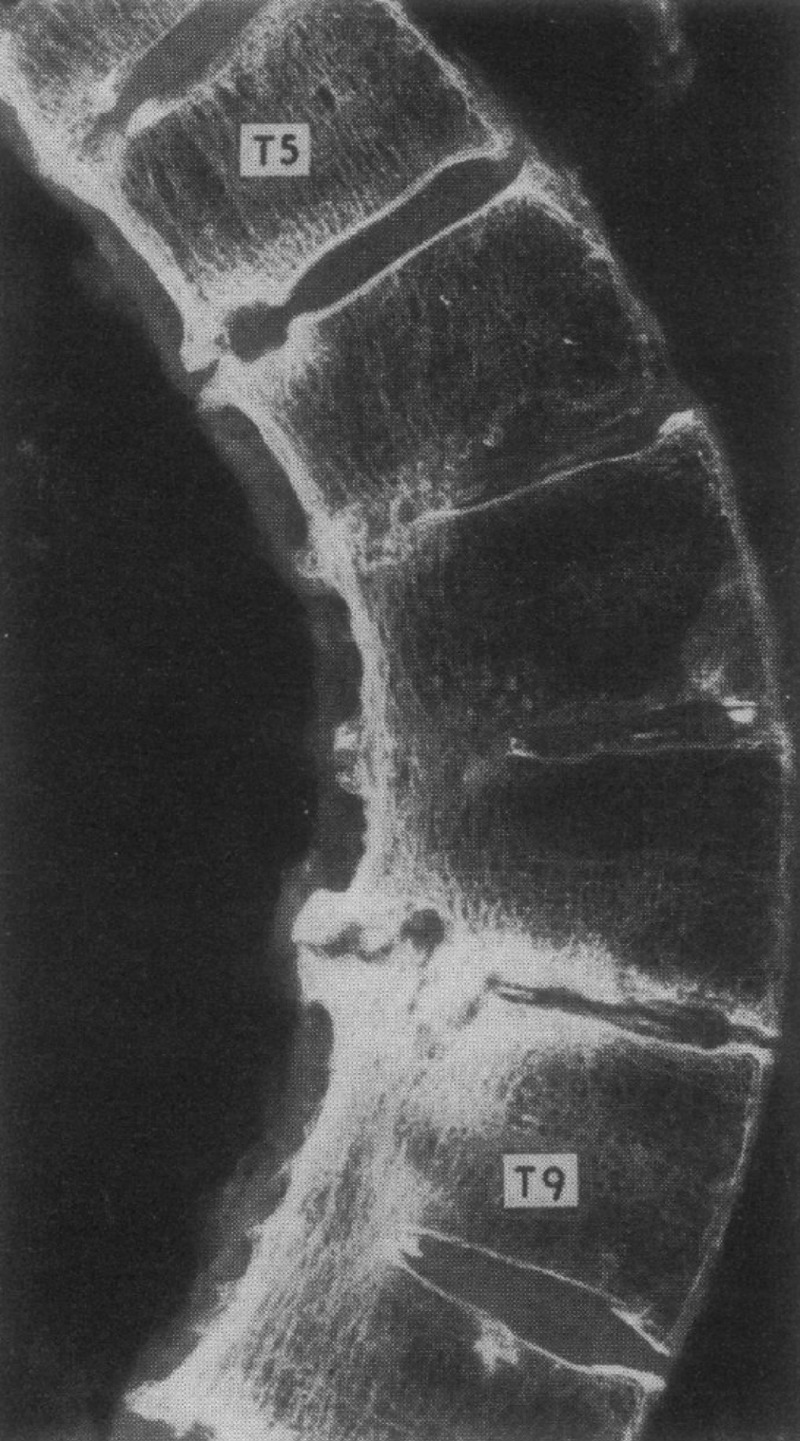
Bone changes in ankylosing spondylitis: intravertebral bone loss and sclerosis, vertebral wedging, squaring, syndesmophytes and sclerosis at erosive sites [Cawley et al. 1972].
Osteoporosis in AS
Low bone mineral density (BMD) and bone loss has been well documented in the spine and hips of patients with AS, from early on in the disease [Geusens and Lems, 2011; Roux, 2011]. With progressive disease, however, the use of bone densitometry in the spine is confounded by the presence of syndesmophytes and periosteal bone formation. Low BMD is present in early disease, independent of spine mobility and exercise. Risk factors include disease indices such as the Bath Ankylosing Spondylitis Radiology Index (BASRI), syndesmophyte score, modified Stoke Ankylosing Spondylitis Spinal Score (mSASSS), active disease and increased inflammatory parameters and markers of resorption [Baek et al. 2005; Cooper et al. 1994; Feldtkeller et al. 2006; Geusens et al. 2001; Jun et al. 2006; Karberg et al. 2005; Lange et al. 2005; Sinigaglia et al. 2006; Vosse et al. 2004, 2006].
Furthermore, bone loss has been demonstrated in the hip, and has been associated with vertebral fractures in AS patients [Baek et al. 2005; Lange et al. 2005]. Ghozlani and colleagues [Ghozlani et al. 2009] has recently reported the prevalence of vertebral fractures (grades 2–3) to be 29.6% using World Health Organization (WHO) criteria for BMD at the total hip and 33.3% using WHO criteria for osteoporosis. Moreover the prevalence was 11.1% in those with normal BMD. In a study of 80 male AS patients (mean age 33, mean disease duration 8 years) 35% had WHO defined osteoporosis at one of four skeletal sites compared with 2.5% of controls [Vasdev et al. 2011].
In chronic AS cases more sophisticated techniques, such as quantitative CT, have shown bone loss within the vertebrae and hips, further progressing when cortical bone increased [Lange et al. 2005].
Measuring BMD in early disease should include densitometry of the spine and hip. In advanced disease, spine densitometry should not be used as a risk predictor for fracture, but hip BMD that is related to fracture risk. When available, quantitative CT of the vertebrae should be considered.
Vertebral fractures in AS
In AS, the risk of vertebral fractures is definitely increased. However, diagnosing vertebral fractures in AS is not easy in general, although their clinical consequences in aggravating spine deformation (hyperkyphosis) and complications are increasingly recognized [Geusens et al. 2007].
Diagnosis of vertebral fractures
The diagnosis of vertebral fractures is difficult for several reasons. First, only one out of three to one out of four vertebral fractures comes to clinical attention with typical signs and symptoms of an acute fracture [Cooper et al. 1992]. Even in the presence of symptomatic clinical vertebral fractures, however, they are often clinically overlooked as both acute and chronic back pain is common in AS. The diagnosis is often missed by attributing the pain to disease activity, especially if a vertebral fracture is not considered in the differential diagnosis of back pain. Second, fractures of the vertebral body are often overlooked even when radiographs are available [Delmas et al. 2005]. Third, in addition to fractures of the vertebral body, other types of spinal fractures occur in AS. For example fractures of the dorsal arch and its pedicles, which are quite rare in postmenopausal osteoporosis, have been reported in patients with AS and are difficult to diagnose because of their location [Wang et al. 2005] (Figure 2). Fractures in newly formed bone in the osteoligamentous components (syndesmophytes, transdiscal, interspinal) are even more difficult to diagnose [Campagna et al. 2009; Sambrook and Cooper, 2006].
Figure 2.
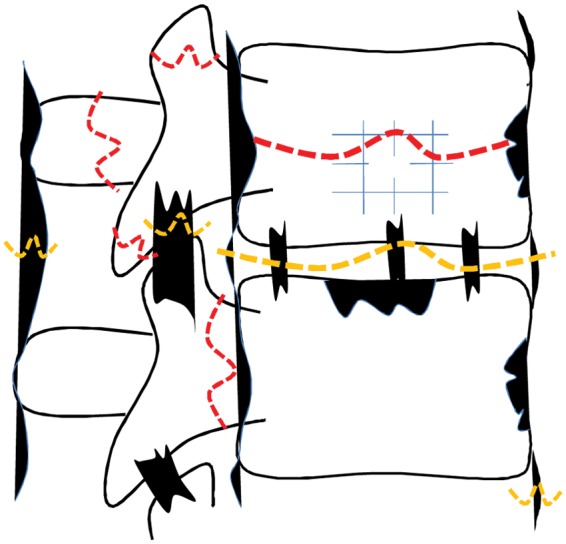
Fractures in ankylosing spondylitis: fractures in existing bone (red on white) and in newly formed bone (yellow on black).
Fourth, in cohort surveys of AS, such as the OASIS cohort, radiographs of the thoracic spine are often of relatively low imaging quality for evaluation of disease indices such as the mSASSS due to overlying soft tissues and ribs. In such surveys, data are often only available for the lumbar spine, not the thoracic spine, and thus cannot be used to study the true prevalence of all vertebral fractures. Also, although there is growing consensus about the definition of vertebral fractures [Sambrook and Cooper, 2006], several definitions are available and there is no universally accepted gold standard for diagnosing vertebral fractures. The prevalence and incidence of vertebral fractures is therefore influenced by the definition of the degree of deformation of the vertebral body.
In addition, no data are available on the prevalence of vertebral deformities/fractures in the young adult population, which makes it difficult to interpret data in AS patients younger than 50 years.
Fractures of the vertebral body in AS
Several surveys have reported the prevalence of vertebral fractures [Geusens et al. 2007], of which some are summarized in Table 1.
Table 1.
Prevalence of vertebral fractures [Geusens et al. 2007].
| Study | N | Age | % VF | Recruitment |
|---|---|---|---|---|
| Cooper | 158 | 34 | 9.5 | Population |
| Toussirot | 71 | 39 | 1.4 | Consecutive |
| Baek | 76 | 28 | 4 | Consecutive |
| Donnelly | 87 | 44 | 10.3 | Consecutive |
| Jun | 68 | 31 | 16 | Consecutive |
| Ralston | 111 | 41 | 18 | Consecutive |
| Mitra | 66 | 38 | 17 | Mild AS |
| Lange | 84 | 32–46 | 0–20 | Dis Activity |
| Geusens | 50 | 50 | 58 | Wide DA |
| Vosse | 135 | 46–54 | 31 | OASIS |
| Hansen | 50 | 29–79 | 4 | ND |
| Devogelaer | 70 | 35–39 | 4 | ND |
| Sivn | 22 | 36 | 41 | ND |
VF, vertebral fractures; AS, ankylosing spondylitis; ND, no data.
These studies indicate that vertebral fractures are a regular finding in patients with AS but their prevalence is highly variable. These differences are at least in part a reflection of differences in recruitment methods [e.g. consecutive patients, selected patients based on disease activity or occiput-to-wall distance (OWD), sex distribution, age, clinical versus systematic morphometric fractures and the definition of vertebral fractures]. The most exact estimate of the prevalence and incidence of vertebral fractures in AS appears to be derived from the study by Cooper and colleagues [Cooper et al. 1992]. This retrospective population-based study on clinical fractures reported an increased odds ratio (OR) of 7.7 (95% confidence interval 4.3–12.6) for clinical vertebral fractures (as found in the hospital files of patients with clinical vertebral fractures confirmed by a radiologist without specification of the degree of deformity). The cumulative incidence of clinical vertebral fractures was higher in men (OR 10.7 versus 4.2 in women) and increased during the first 5 years of the disease, peaking at 17%, 20–30 years after diagnosis. Of interest, in the Cooper study, the cumulative incidence of nonvertebral fractures was similar to the control population. As this population study involved clinical vertebral fractures, it is still remains unclear what is the exact prevalence and incidence of morphometric vertebral fractures in AS.
Fractures of the vertebral body result in acute or chronic back pain or remain clinically silent [Cooper et al. 1992]. Wedging of the vertebrae can contribute to hyperkyphosis, independent of mSASSS score [Geusens and Lems, 2011; Vosse et al. 2006]. Increased hyperkyphosis can, therefore, be regarded not only as a clinical consequence but also as an indicator of the presence of vertebral wedged fractures in AS [Sinigaglia et al. 2006; Vosse et al. 2006]. The most common levels affected are T8-L2 [Ghozlani et al. 2009].
Other spinal fractures in AS
These fractures are characterized by their unusual location (e.g. at the cervical spine, dens), the involvement of the posterior arch structures of the vertebrae, their anatomic location (transvertebral with variable degrees of dislocation, transdiscal through the syndesmophytes) and complications with variable degrees of neurological deficits [Wang et al. 2005] (Figure 2).
These fractures have been classified according to their location (Table 2).
Table 2.
Fracture locations in ankylosing spondylitis [Campagna et al. 2009].
| Anterior column involvement |
| Transvertebral |
| Transdiscal |
| Middle column involvement |
| Posterior longitudinal ligament |
| Posterior column involvement |
| Facet joints |
Many of these fractures have been described in AS patients with an ankylosed spine, even after trivial trauma. In these cases, even when a fracture is considered, diagnosis can be difficult, as fractures of the posterior arch are often difficult to visualize by conventional radiographic examination, even more so at the level of the cervical spine. Additional imaging techniques such as bone scintigraphy, CT and MRI are than necessary for adequate diagnosis and this delay can contribute to a worse outcome [Wang et al. 2005].
Erosive lesions at the adjacent vertebral plates can accompany noninfectious discitis in AS, resulting in a radiographic picture of vertebral deformities [Wang et al. 2005].
The unusual characteristics of some fractures (cervical level, dorsal arch, dislocation, neurological deficits) are responsible for significant morbidity, and in some cases mortality (Table 3). These complications include spinal cord lesions, nerve root lesions, and the occurrence of paravertebral hematomas resulting in variable degrees of sensory or motor deficits. Owing to defective fracture healing, pseudoarthosis with instability in the posterior arch structures of the vertebrae can occur [Sinigaglia et al. 2006; Wang et al. 2005]. In cases of severe or persisting neurological deficits, surgery may be necessary.
Table 3.
Possible complications of vertebral fractures in ankylosing spondylitis.
| Spinal deformation |
| Spinal cord involvement (edema, contusion, compression) |
| Epidural hematoma |
| Vertebral artery injury |
| Neurological deficit |
Risk factors for vertebral fractures
Fracture risk is associated with bone and falls. Some fracture risks are more prevalent in patients with rheumatic diseases than in the general population, such as those with immobility. The presence of such risks, variations in the level and duration of disease activity, the interference of extraosseous calcification in the spine, and the limited methods available to measure structural and material characteristics of bone have been a problem in identifying the independent role of osteoporosis and systemic inflammation in fracture risk in AS.
Risk factors associated with fractures of the vertebral body include sex (men more than women), age, low body weight, low BMD, disease duration, more extensive syndesmophyte formation, mSASSS score, disease activity, peripheral joint involvement, spinal restriction of movement and increased OWD [Cooper et al. 1992; Feldtkeller et al. 2006; Geusens et al. 2007; Ghozlani et al. 2009; Sinigaglia et al. 2006; Vasdev et al. 2011; Vosse et al. 2004, 2006]. No data are available on the risk of falls in AS patients. In view of the biomechanical changes in the spine, however, even a simple fall or other minor trauma can result in a fracture of the vertebral body or its other components [Vasdev et al. 2011].
Conclusion
Osteoporosis and vertebral fractures are now well recognized features in patients with AS. Diagnosing fractures of the vertebral body and its dorsal arch remains a challenge in studies and in clinical practice. Prospective studies will be necessary to evaluate to what degree such fractures, including morphometric fractures, can be prevented by therapy, for example, bisphosphonates and biologicals. Certainly recent studies of biological suggest BMD loss can be prevented by early intervention [Visvanathan et al. 2009].
The above reviewed offers some suggestions for daily practice, as many rheumatologists do not routinely assess patients with AS for osteoporosis. The presence of a vertebral fracture should be considered in patients at high risk for osteoporosis and fractures (postmenopausal women, low body weight, previous fracture, hip fracture in the mother, use of glucocorticoids, severe immobility) and those at risk more specifically for AS (such as men, severe disease activity, persistent active disease, longstanding disease, OWD >0 cm, persistent pain after even minimal trauma).
On suspecting a vertebral fracture, radiographs of the spine should be performed. Additional imaging techniques are indicated in cases of persistent posttraumatic pain in order to avoid delays in diagnosis and therapy.
Drug treatment for osteoporosis should be considered in patients with a vertebral fracture or BMD with a T score less than -2.5. From the above pathophysiological perspective, the target to prevent vertebral fractures is not only to prevent bone loss within the vertebrae but also to prevent excessive bone formation around the vertebrae.
Contributor Information
Philip N. Sambrook, Institute of Bone and Joint Research, University of Sydney, Sydney, Australia
Piet Geusens, Biomedical Research Institute, University Hasselt, Belgium; Internal Medicine, Department of Rheumatology, Maastricht University Medical Centre, 6202 AZ Maastricht, The Netherlands.
References
- Baek H.J., Kang S.W., Lee Y.J., Shin K.C., Lee E.B., Yoo C.D., et al. (2005) Osteopenia in men with mild and severe ankylosing spondylitis. Rheumatol Int 26: 30–34 [DOI] [PubMed] [Google Scholar]
- Campagna R., Pessis E., Feydy A., Guerini H., Thevenin F., Chevrot A., et al. (2009) Fractures of the ankylosed spine: MDCT and MRI with emphasis on individual anatomic spinal structures. AJR Am J Roentgenol 192: 987–995 [DOI] [PubMed] [Google Scholar]
- Cawley M.I., Chalmers T.M., Kellgren J.H., Ball J. (1972) Destructive lesions of vertebral bodies in ankylosing spondylitis. Ann Rheum Dis 31: 345–358 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper C., Atkinson E.J., O’Fallon W.M., Melton L.J., III (1992) Incidence of clinically diagnosed vertebral fractures: a population-based study in Rochester, Minnesota, 1985–1989. J Bone Miner Res 7: 221–227 [DOI] [PubMed] [Google Scholar]
- Cooper C., Carbone L., Michet C.J., Atkinson E.J., O’Fallon W.M., Melton L.J., 3rd (1994) Fracture risk in patients with ankylosing spondylitis: a population based study. J Rheumatol 21: 1877–1882 [PubMed] [Google Scholar]
- Delmas P.D., van de, Langerijt L., Watts N.B., Eastell R., Genant H., Grauer A., et al. (2005) Underdiagnosis of vertebral fractures is a worldwide problem: The IMPACT study. J Bone Mineral Res 20: 557–563 [DOI] [PubMed] [Google Scholar]
- Feldtkeller E., Vosse D., Geusens P., van der Linden S. (2006) Prevalence and annual incidence of vertebral fractures in patients with ankylosing spondylitis. Rheumatol Int 26: 234–239 [DOI] [PubMed] [Google Scholar]
- Geusens P., Lems W.F. (2011) Osteoimmunology and osteoporosis. Arthritis Res Ther 13: 242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geusens P., Vosse D., van der Heijde D., Vanhoof J., van Tubergen A., Raus J., et al. (2001) High prevalence of thoracic vertebral deformities and discal wedging in ankylosing spondylitis patients with hyperkyphosis. J Rheumatol 28: 1856–1861 [PubMed] [Google Scholar]
- Geusens P., Vosse D., van der Linden S. (2007) Osteoporosis and vertebral fractures in ankylosing spondylitis. Curr Opin Rheumatol 19: 335–339 [DOI] [PubMed] [Google Scholar]
- Ghozlani I., Ghazi M., Nouijai A., Mounach A., Rezqi A., Achemlal L., et al. (2009) Prevalence and risk factors of osteoporosis and vertebral fractures in patients with ankylosing spondylitis. Bone 44: 772–776 [DOI] [PubMed] [Google Scholar]
- Jun J.B., Joo K.B., Her M.Y., Kim T.H., Bae S.C., Yoo D.H., et al. (2006) Femoral bone mineral density is associated with vertebral fractures in patients with ankylosing spondylitis: A cross-sectional study. J Rheumatol 33: 1637–1641 [PubMed] [Google Scholar]
- Karberg K., Zochling J., Sieper J., Felsenberg D., Braun J. (2005) Bone loss is detected more frequently in patients with ankylosing spondylitis with syndesmophytes. J Rheumatol 32: 1290 [PubMed] [Google Scholar]
- Lange U., Kluge A., Strunk J., Teichmann J., Bachmann G. (2005) Ankylosing spondylitis and bone mineral density-what is the ideal tool for measurement? Rheumatol Int 26: 115–120 [DOI] [PubMed] [Google Scholar]
- Roux C. (2011) Osteoporosis in inflammatory joint diseases. Osteoporos Int 22: 421–433 [DOI] [PubMed] [Google Scholar]
- Sambrook P., Cooper C. (2006) Osteoporosis. Lancet 367: 2010–2018 [DOI] [PubMed] [Google Scholar]
- Sinigaglia L., Varenna M., Girasole G., Bianchi G. (2006) Epidemiology of osteoporosis in rheumatic diseases. Rheum Dis Clin North Am 32: 631–658 [DOI] [PubMed] [Google Scholar]
- Vasdev V., Bhakuni D., Garg M.K., Narayanan K., Jain R., Chadha D. (2011) Bone mineral density in young males with ankylosing spondylitis. Int J Rheum Dis 14: 68–73 [DOI] [PubMed] [Google Scholar]
- Visvanathan S., van der Heijde D., Deodhar A., Wagner C., Baker D.G., Han J., et al. (2009) Effects of infliximab on markers of inflammation and bone turnover and associations with bone mineral density in patients with ankylosing spondylitis. Ann Rheum Dis 68: 175–182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vosse D., Feldtkeller E., Erlendsson J., Geusens P., van der Linden S. (2004) Clinical vertebral fractures in patients with ankylosing spondylitis. J Rheumatol 31: 1981–1985 [PubMed] [Google Scholar]
- Vosse D., van der Heijde D., Landewe R., Geusens P., Mielants H., Dougados M., et al. (2006) Determinants of hyperkyphosis in patients with ankylosing spondylitis. Ann Rheum Dis 65: 770–774 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y.F., Teng M.M., Chang C.Y., Wu H.T., Wang S.T. (2005) Imaging manifestations of spinal fractures in ankylosing spondylitis. AJNR Am J Neuroradiol 26: 2067–2076 [PMC free article] [PubMed] [Google Scholar]


