Summary
We report a patient with a wide-necked aneurysm arising at the bifurcation of the right internal carotid artery and the persistent primitive trigeminal artery (PPTA) treated successfully by Matrix detachable coil occlusion and assisted by a Neuroform intracranial stent. First, a Neuroform self-expanding intracranial stent was delivered via a 5-F Guider Softtip XP and placed as desired, then the aneurysm dome was embolized with two Matrix detachable coils through the interstices of the stent. The aneurysm was 80% occluded angiographically and the parent artery was patent. DSA imaging six months after the procedure showed the aneurysm to be obliterated at angiography and the neck tissue thickness of the aneurysm to be increased, but the parent artery diameter was not impacted. We describe the case in detail and discuss our preliminary experience of using the Neuroform stent and Matrix detachable coils for the treatment of a PPTA wide-necked aneurysm.
Key words: persistent primitive trigeminal artery, aneurysm, neuroform intracranial stent, Matrix detachable coil, embolization, endovascular therapy
Introduction
Persistent primitive carotid-basilar artery anastomoses are uncommon, and are usually seen on an angiogram or discovered at autopsy. The most frequent type of anastomosis is the persistent trigeminal artery. The PPTA and PPTA variant are frequently associated with intracranial aneurysms (in 14 and 24% of cases, respectively) 12.
Treatments include surgical reconstruction, prophylactic extracranial-intracranial bypass, internal carotid artery ligation, and PPTA clipping 16,10,13,2,6,5,15. We describe herein a PPTA broad-necked aneurysm treated successfully by Matrix detachable coils occlusion and assisted by a Neuroform intracranial stent 9,3.
Case Report
A 28-year-old woman presented with a two-year history of intermittent right migraine. The patient had no history of head trauma, no history of paroxysmal severe headache or coma. Magnetic resonance angiography (figure 1A) and cerebral angiography (figure 1B) demonstrated that the right-sided PPTA arose from the posterior bend of the distal horizontal segment of the intracavernous carotid artery, and then joined the basilar artery. The aneurysm originated from the root of the right-sided PPTA, the maximum diameter of the lesion was 3.2 mm and the neck was 4 mm wide-necked unruptured aneurysm. We explained to the patient and her family the need for treatment, the various methods of treatment and the risks associated with each method. The patient elected endovascular embolization with coils. As it was a wide-necked unruptured aneurysm, embolization using only detachable coils was considered dangerous and technically difficult, so we decided to treat it with Neuroform stentsupported coil embolization. The patient was pretreated with 650 mg aspirin and 75 mg clopidogrel (Plavix; Bristol-Myers Squibb/Sanofi Pharmaceuticals, New York, NY) for three days. All procedures were performed while the patient was under general anesthesia with electrocardiographic monitoring. First, we placed a Neuroform self-expanding intracranial stent (Boston Scientific/Smart, San Leandro, CA. 4.5 mm 20 mm) in the desired position. The stent length was chosen to provide at least a 5 mm landing zone on either side of the aneurysm neck9. Then the microcatheter was manipulated into the aneurysm through the stent interstices for coil embolization over a 200 cm Synchro 0.014 in microwire. After that, two Matrix detachable coils (Boston Scientific/Target, Fremont, CA. 3 mm 6 cm-3D, 2 mm 6 cm-2D) were embolized into the aneurysm (figure 3A). Right common ICA angiography immediately after embolization showed the aneurysm was embolized about 80% angiographically, the right ICA was patent, and the PPTA was well visualized (figure 2).
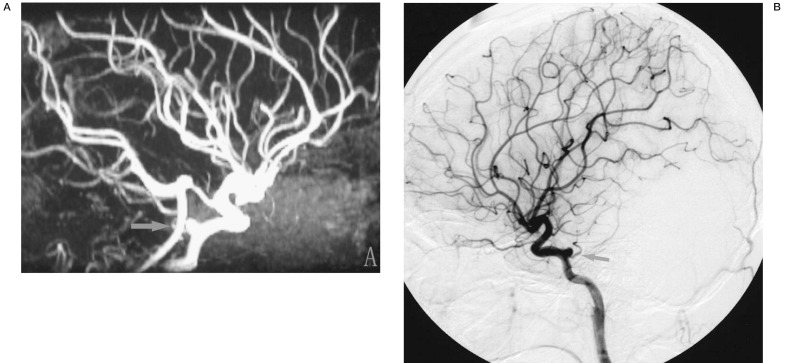
Figure 1.
A) Magnetic resonance angiography revealing a saccular aneurysm arising from the posterior bend of the distal horizontal segment of the ICA. B) Angiogram (lateral view) of the right internal carotid showing a wide-necked saccular aneurysm originating from the root of right-sided PPTA.
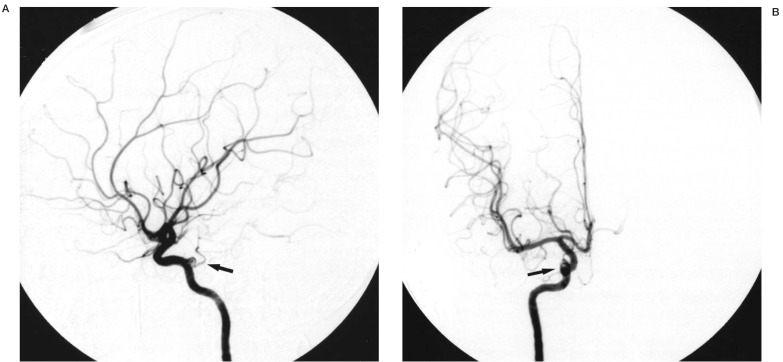
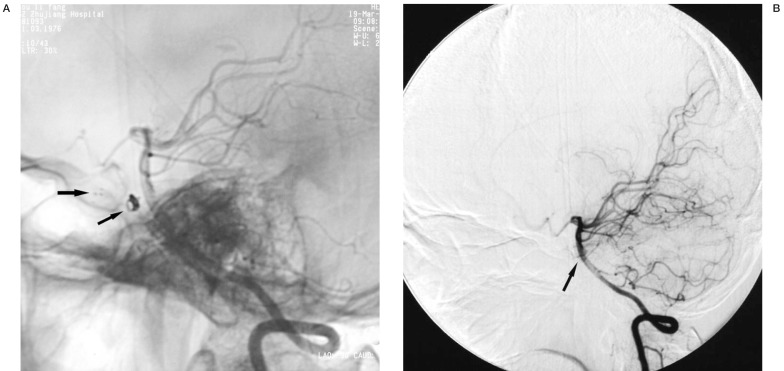
Figure 2.
A) Angiogram (lateral view) of the right internal carotid showing the aneurysm treated with Neuroform stent-supported Matrix coil embolization, partial aneurysm occlusion was achieved. B) Angiogram (anteroposterior view) of the right internal carotid showing partial aneurysm occlusion.
Figure 3.
A) X-ray (lateral view) of the skull showing the position of the Neuroform stent and Matrix coils. B) Left vertebral angiography (lateral view), while the right cervical carotid artery was compressed over, showing the PPTA and the PCA.
Then selective left vertebral angiography, while, the right cervical carotid artery was compressed over, well displayed the PPTA (figure 3B). During and after the procedure, the patient showed no adverse reaction. The patient was maintained on aspirin and clopidogrel for three weeks, followed by aspirin alone, which is continued indefinitely.
Follow-up right common ICA angiography performed six months after treatment showed the aneurysm to be obliterated at angiography and the neck tissue thickness of the aneurysm to be increased, however, the parent artery diameters were not impacted (figure 4), and the stent was well visualized in a good position (figure 5A). In particular, the radiolucent tissue gap between the flowing contrast media in the parent artery and the coil mass in the aneurysm (angiographic evidence of neointima) was no injection of contrast medium to be filled (figure 4C), connective tissue formation was well demonstrated. Then with selective left vertebral angiography, while, the right cervical carotid artery was compressed, the PPTA was visualized (figure 5B) The patient's right migraine disappeared completely, and no other complications were observed.
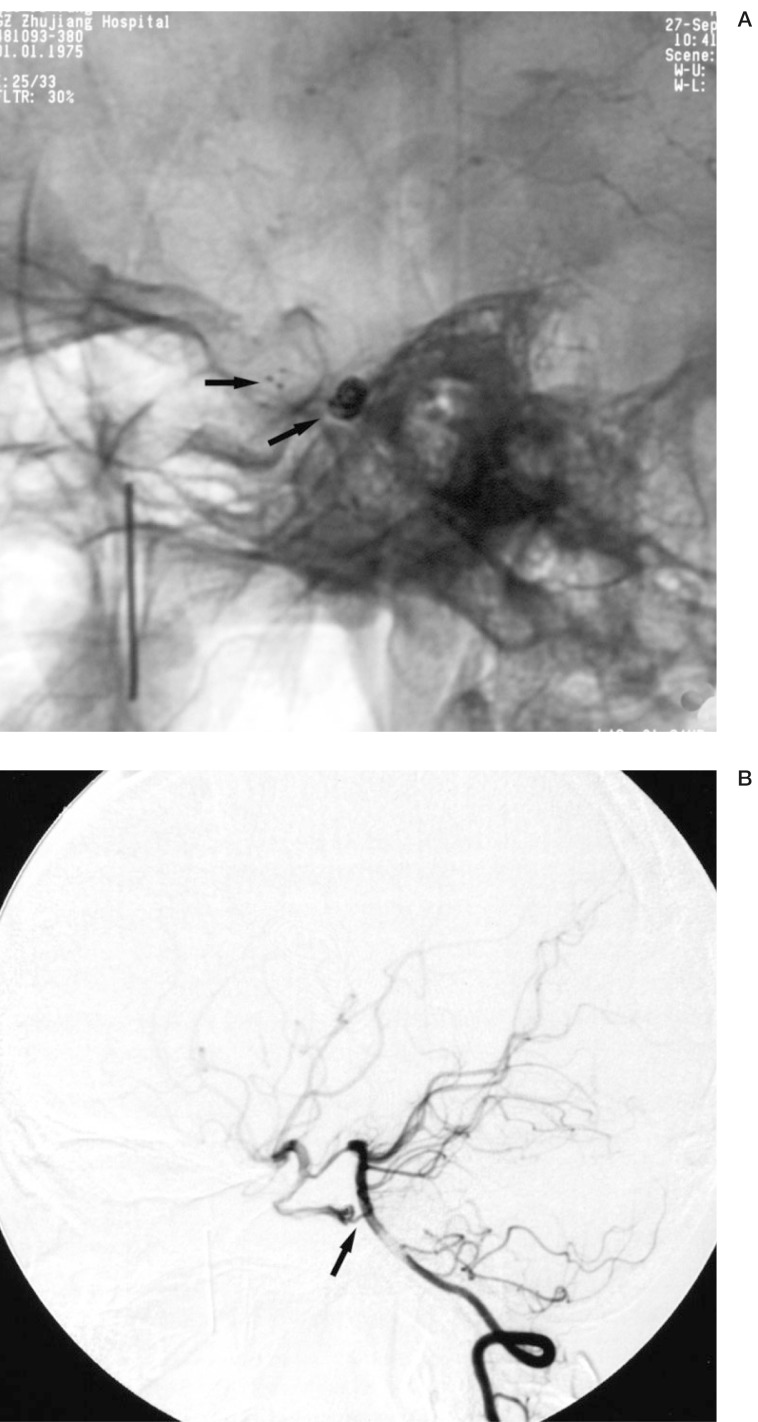
Figure 4.
A) Angiogram (lateral view) of the right internal carotid artery at six months follow-up showing the aneurysm fully occluded and without parent artery stenosis. B) Angiogram (anteroposterior view) of the right internal carotid artery at six months follow-up. C) Angiogram (lateral view, no digital subtraction) of the right internal carotid artery at six months follow-up showing the radiolucent tissue gap between the flowing contrast media in the parent artery and the coil mass in the aneurysm.
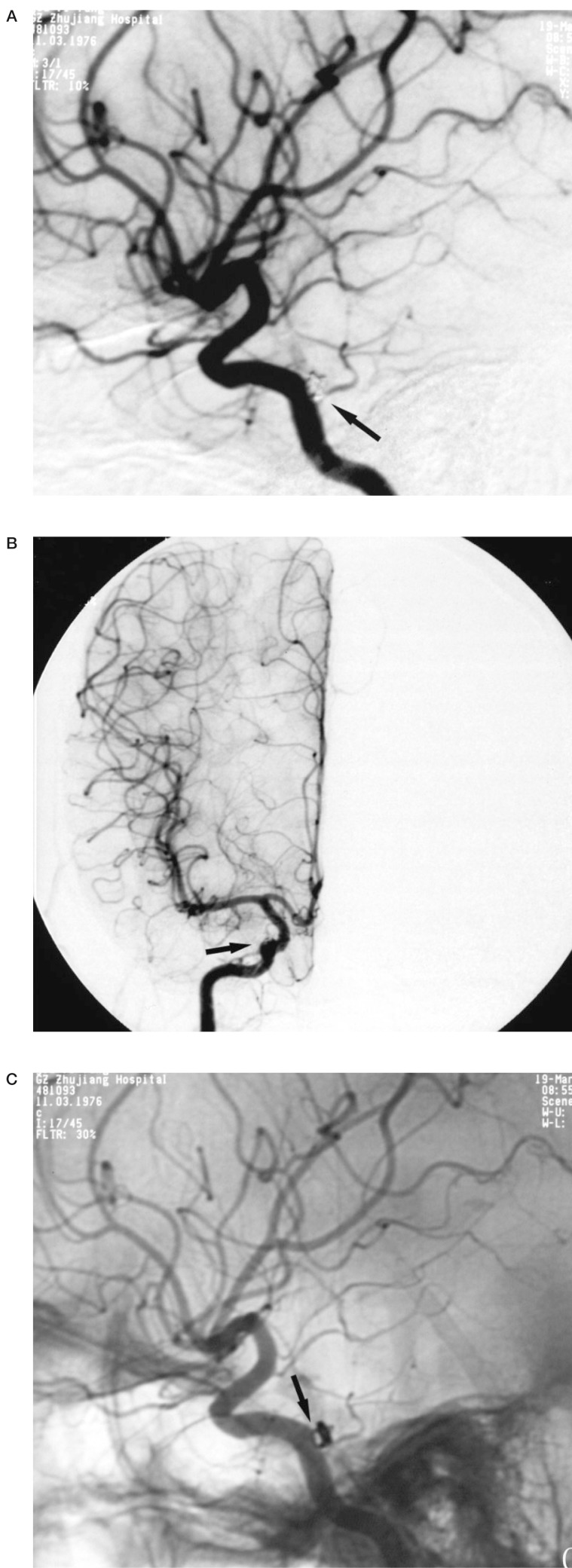
Figure 5.
A) Left vertebral angiography (lateral view, no digital subtraction) at six months follow-up showing the position of the Neuroform stent and Matrix coils. B) Left vertebral angiography (lateral view) at six months follow-up, while the right cervical carotid artery was compressed over, showing the PPTA and the PCA.
Discussion
Anatomically, persistent primitive carotidbasilar artery anastomoses are uncommon, In the 3 to 5 mm human embryo, prominent arterial anastomosis, in the form of the trigeminal, otic, hypoglossal, and proatlantal arteries, joins the dorsal aorta (the future internal carotid artery in its cranial portion) to the bilateral longitudinal neural arteries (the future basilar artery).
The trigeminal artery is the largest of these arteries, this vessel, which originates from the cavernous internal carotid artery, runs along the trigeminal nerve, enters the posterior fossa through Meckel's cave or the isolated dural foramen, and directly supplies the cerebellum, usually being obliterated by the 11.5 to 14 mm embryonic stage. The trigeminal artery is the most common of the primitive carotid-basilar anastomoses that persist into adulthood, with an incidence of 0.1 to 1.0%, it is usually considered the persistent primitive trigeminal artery (PPTA)12. The PPTA and PPTA variant are frequently associated with intracranial aneurysms (in 14 and 24% of cases, respectively) or as a cause of facial pain 16.
Ahmad I et Al 1 reported a case of a PPTA aneurysm treated with a prophylactic extracranial-intracranial bypass, internal carotid artery ligation, and PPTA clipping. Endovascular treatment has now attained an important place in the therapeutic arsenal for treating intracranial aneurysms. In this case, we discuss the ideal treatment of the PPTA broad-necked aneurysm by new interventional products. A common feature of broad-necked aneurysms is the difficulty of therapeutic management, which often requires a combination of techniques 3,17,4. The "Remodeling Technique" is often used and proved very useful in the treatment of broadnecked aneurysms.
During the procedure, the aneurysm was catheterized with a microcatheter and then a temporary balloon was placed as desired and inflated to cover the neck of the aneurysm. After that, permanent coil occlusion was undertaken with platinum coils and at the end of the procedure the balloon was deflated and occlusion of the aneurysm completed. In spite of this, endosaccular occlusion of wide-necked aneurysms with coils was considered dangerous and technically difficult.
Wide-necked intracranial aneurysms with severely tortuous parent artery could not be treated effectively with traditional endovascular techniques (e.g., coil embolization with or without balloon assistance). Now the "Remodeling Technique" has improved, instead of using a temporary balloon, permanent Neuroform self-expanding intracranial stents are used in the endosaccular occlusion of broad-necked aneurysms.
The Neuroform microstent - a flexible, self-expandable, microcatheter-delivered, nitinol stent designed for the treatment of cerebral aneurysms - was recently approved for use in patients 9,3,14,7. The Neuroform stent is a useful device for the treatment of patients with aneurysms that may not otherwise be amenable to endovascular therapy. The Neuroform stent is a very easy and safe intracranial stent for embolization of broad-necked intracranial aneurysm. Even within the most tortuous segments of the cerebral vasculature, the stent can be deployed accurately and clinically significant complications are uncommon 3,14,7.
Application of intracranial stents to support the coil embolization of cerebral aneurysms offers significant technical and theoretical advantages. Until recently, however, no dedicated intracranial stents were available, and only stents designed for use in the coronary arteries were of an appropriate size for deployment in the cerebral vasculature. Correspondingly, the feasibility of intracranial stenting had been significantly limited by the physical characteristics of the available balloon-mounted coronary stents. The inflexibility of these stents frequently precluded safe negotiation through the tortuous cerebral vasculature to a targeted landing zone 3,7. Matrix coils consist of thin platinum coils covered with a bioabsorbable, polymeric material (polyglycolic acid/lactide) and attached to a stainless steel delivery wire. It can accelerate of thrombogenesis and connective tissue formation in endovascular aneurysm repair. Acceleration of intra-aneurysmal clot organization and fibrosis may be a solution to prevent aneurysm recanalization after endovascular treatment 11,8. This aneurysm was 80% occluded angiogarphically during the procedure, the aneurysm was not densely packed using Matrix coils. However, six months later, the Matrix-embolized aneurysm exhibits complete covering of the neck with a thick radiolucent tissue. Murayama Y. et Al 11 reported an experimental study on swine: three and six months after treatment by Matrix coils, the aneurysm specimens exhibited fibrous tissue covering the neck of the aneurysms. No excessive tissue reaction at the neck was observed with Matrix-treated aneurysms. These observations were confirmed by microscopy.
The swine model variables of increased thickness of tissue at aneurysm neck, increased clot organization at two weeks, and decreased size of aneurysm at three months have not yet been validated as predictors of decreased rate of aneurysm recurrence in humans.
In this case, follow-up right common ICA angiography performed six months after treatment, showed the lumen and neck of the aneurysm to be filled by coils and connective tissue, the PPTA perisisted as before. Although a good angiographic result was achieved, longerterm angiographic follow-up is necessary.
References
- 1.Ahmad I, Tominaga T, et al. Primitive trigeminal artery associated with cavernous aneurysm: case report. Surg Neurol. 1994;41:75–79. doi: 10.1016/0090-3019(94)90211-9. [DOI] [PubMed] [Google Scholar]
- 2.Baskaya MK, Roberts R, et al. Persistent primitive trigeminal artery associated with posterior communicating artery aneurysm and hypoplastic vertebral artery. Surg Radiol Anat. 2001;23:169–171. doi: 10.1007/s00276-001-0169-9. [DOI] [PubMed] [Google Scholar]
- 3.Broadbent LP, Moran CJ, et al. Management of Neuroform stent dislodgement and misplacement. Am J Neuroradiol. 2003;24:1819–1822. [PMC free article] [PubMed] [Google Scholar]
- 4.Castro E, Fortea F, et al. Treatment of a giant aneurysm of the right middle cerebral artery with GDCs after extracranial to intracranial bypass. Interventional Neuroradiology. 1999;5:51–56. doi: 10.1177/159101999900500109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cloft HJ, Razack N, et al. Prevalence of cerebral aneurysms in patients with persistent primitive trigeminal artery. J Neurosurg. 1999;90:865–867. doi: 10.3171/jns.1999.90.5.0865. [DOI] [PubMed] [Google Scholar]
- 6.Ekinci G, Baltacioglu F, et al. A rare cause of hyperprolactinemia: persistent trigeminal artery with stalksection effect. Eur Radiol. 2001;11:648–650. doi: 10.1007/s003300000573. [DOI] [PubMed] [Google Scholar]
- 7.Fiorella D, Albuquerque FC, et al. Preliminary experience using the Neuroform stent for the treatment of cerebral aneurysms. Neurosurgery. 2004;54:6–16. doi: 10.1227/01.neu.0000097194.35781.ea. [DOI] [PubMed] [Google Scholar]
- 8.Fujiwara NH, Kallmes DF. Healing response in elastase-induced rabbit aneurysms after embolization with a new platinum coil system. Am J Neuroradiol. 2002;23:1137–1144. [PMC free article] [PubMed] [Google Scholar]
- 9.Howington JU, Hanel RA, et al. The Neuroform Stent, the First Microcatheter-delivered Stent for Use in the Intracranial Circulation. Neurosurgery. 2004;54:2–5. doi: 10.1227/01.neu.0000099370.05758.4d. [DOI] [PubMed] [Google Scholar]
- 10.Ikushima I, Arikawa S, et al. Basilar artery aneurysm treated with coil embolization via persistent primitive trigeminal artery. Cardiovasc Intervent Radiol. 2002;25:7071. doi: 10.1007/s00270-001-0053-3. [DOI] [PubMed] [Google Scholar]
- 11.Murayama Y, Tateshima S, et al. Matrix and bioabsorbable polymeric coils accelerate healing of intracranial aneurysms: long-term experimental study. Stroke. 2003;34:2031–2037. doi: 10.1161/01.STR.0000083394.33633.C2. [DOI] [PubMed] [Google Scholar]
- 12.Nigel S, Jorge M, et al. Persistent Trigeminal Artery: A Unique Anatomic Specimen-Analysis and Therapeutic Implications. Neurosurgery. 2000;47:428–434. doi: 10.1097/00006123-200008000-00030. [DOI] [PubMed] [Google Scholar]
- 13.Nishio A, Nishijima Y, et al. Primitive trigeminal artery variant aneurysm treated with Guglielmi detachable coils--case report. Neurol Med Chir (Tokyo) 2001;41:446–449. doi: 10.2176/nmc.41.446. [DOI] [PubMed] [Google Scholar]
- 14.Pride GL, Jr, Replogle RE, et al. Stent-coil treatment of a distal internal carotid artery dissecting pseudoaneurysm on a redundant loop by use of a flexible, dedicated nitinol intracranial stent. Am J Neuroradiol. 2004;25:333–337. [PMC free article] [PubMed] [Google Scholar]
- 15.Rasmussen JN, Bjerre P. Aneurysm on a persisting primitive trigeminal artery occluded with Guglielmi detachable coils. Interventional Neuroradiology. 1998;4:91–93. doi: 10.1177/159101999800400112. [DOI] [PubMed] [Google Scholar]
- 16.Tamura Y, Shimano H, et al. Trigeminal Neuralgia Associated with a Primitive Trigeminal Artery Variant: Case Report. Neurosurgery. 2003;52:1217–1220. [PubMed] [Google Scholar]
- 17.Uchino A, Takase Y, et al. Giant aneurysm of the cervical internal carotid artery treated by proximal coil embolization under temporary balloon occlusion. Interventional Neuroradiology. 2001;7:331–335. doi: 10.1177/159101990100700409. [DOI] [PMC free article] [PubMed] [Google Scholar]