Summary
A gold standard of cerebral vessel imaging remains the digital subtraction angiography (DSA) performed in three projections. However, in specific clinical cases, many additional projections are required, or a complete visualization of a lesion may even be impossible with 2D angiography. Three-dimensional (3D) reconstructions of rotational angiography were reported to improve the performance of DSA significantly. In this pictorial essay, specific applications of this technique are presented in the management of intracranial aneurysms, including: preoperative aneurysm evaluation, intraoperative imaging, and follow-up. Volumetric reconstructions of 3D DSA are a valuable tool for cerebral vessels imaging. They play a vital role in the assessment of intracranial aneurysms, especially in evaluation of the aneurysm neck and the aneurysm recanalization.
Keywords: digital subtraction angiography, neurosurgery, intracranial aneurysm, embolization, remodeling
Background
Digital subtraction angiography (DSA) in anteroposterior, lateral and oblique views is commonly called a contemporary gold standard of cerebral vessel imaging [1–3]. However, due to the increasing difficulty of interventional neuroradiological procedures and the steady progress in therapeutic devices, two-dimensional (2D) DSA became insufficient to precisely depict the three-dimensional structure of intracranial vascular tree in a significant number of cases.
Three-dimensional (3D) reconstruction of rotational angiography was reported to improve the performance of DSA significantly [1–5]. Theoretical advantages of 3D over 2D DSA include the possibility of free rotation of chosen structures, the ability to differentiate between contrast agents like embolic material or bones, and the possibility of elimination of unnecessary image elements. In clinical practice, 3D DSA is more sensitive than 2D DSA to small aneurysms [3,5] and aneurysm remnants [4]. Moreover, the use of 3D reconstructions improves delineation of the aneurysm morphology, its neck, and parent arteries.1 Therefore, 3D DSA was proposed to become a new gold standard of interventional cerebral vascular imaging [3,5].
The purpose of this pictorial review was to outline basic concepts of 3D volumetric reconstructions of cerebral rotational DSA, and to present the application, advantages and limitations of 3D DSA in imaging and intravascular management of intracranial aneurysms.
Technique
The 3D reconstruction of DSA images requires a flat-panel angiographic system with a motorized rotating C-arm. A complete acquisition consists of two rotational scans. The first scan collects subtraction masks, and the second one acquires images during the passage of a contrast medium. Subsequent software reconstructions enable extraction of residual bony structures, deletion of unnecessary vessels, zooming and rotation of the image, as well as differentiation between contrast filling the vessels and vascular devices (coils, stents or clips, Figure 1).
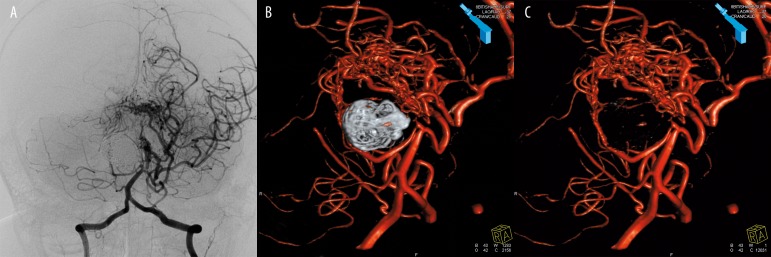
Figure 1.
Image processing in a patient with an arteriovenous malformation (AVM) and an embolized giant aneurysm in the posterior circulation. Conventional DSA image is inconclusive regarding both the AVM supply, and the aneurysm occlusion (A). Three-dimensional reconstructions confirm the completeness of the aneurysm embolization (B), and allow for a better AVM depiction after elimination of the coil mesh (C).
Preoperative Aneurysm Evaluation
Several authors reported that 3D DSA is more sensitive in detecting small aneurysms than the conventional 2D DSA, despite its lower spatial resolution [3,5]. The difference is caused by significant postprocessing capabilities, including free rotation of the vessel tree (Figure 2), and elimination of redundant image elements. Three-dimensional reconstructions allow for an excellent spatial delineation of the regional vascular anatomy and the aneurysm neck (Figures 3, 4). This is crucial for the choice of treatment method, i.e. coiling vs. clipping, planning of the vascular access to the sac, and for the use of the neck remodeling technique. However, due to the volume averaging, 3D reconstructions tend to overestimate the area filled with the contrast medium (Figure 5). Therefore, the actual neck size may be smaller than the one measured on 3D images [6].
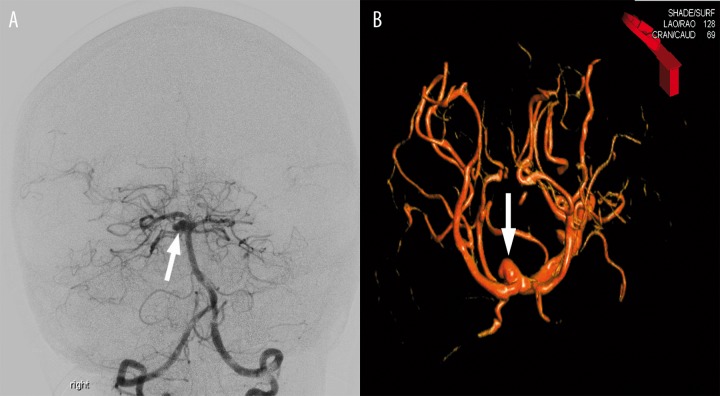
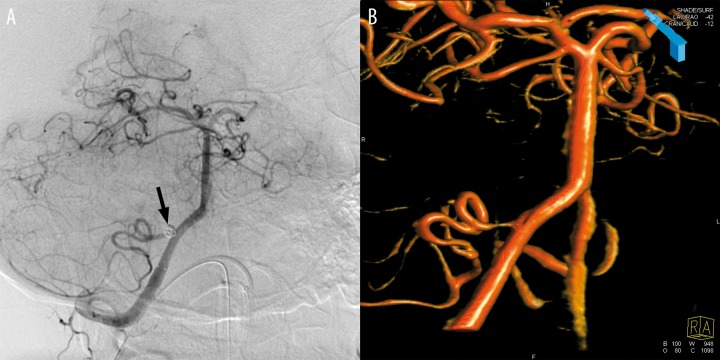
Figure 2.
A basilar tip aneurysm difficult to visualize in detail on conventional DSA images (A arrow). Only 3D reconstructions provide a proper neck delineation (B): note the image cranial angle of 69 degrees, indicating a position unavailable for the C-arm.
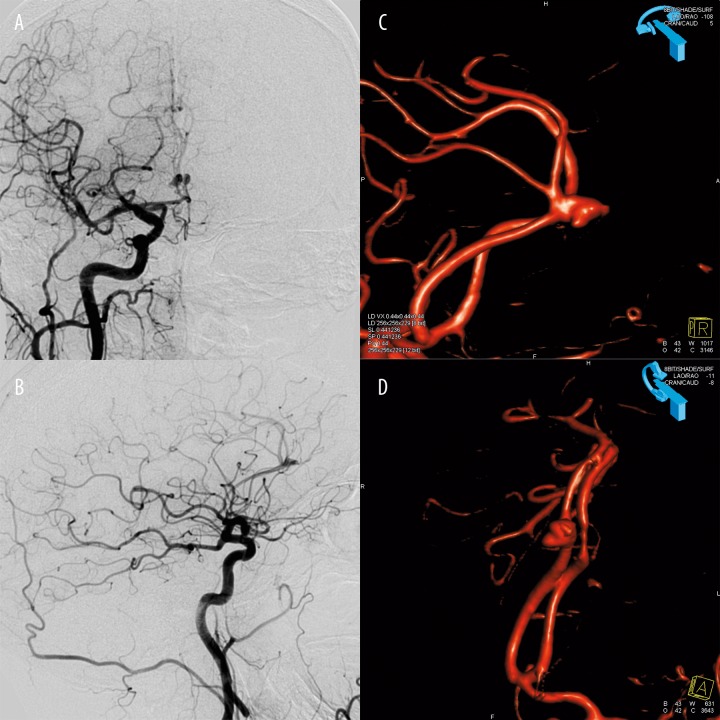
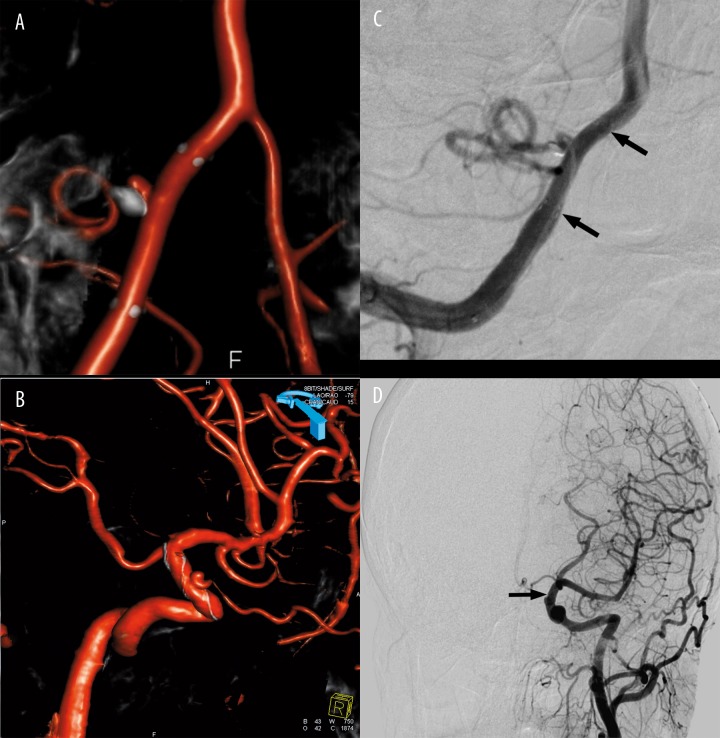
Figure 3.
A right anterior cerebral artery aneurysm poorly delineated on conventional DSA images (A,B). Three-dimensional reconstructions provide appropriate delineation of the neck and adjacent arteries (C,D).
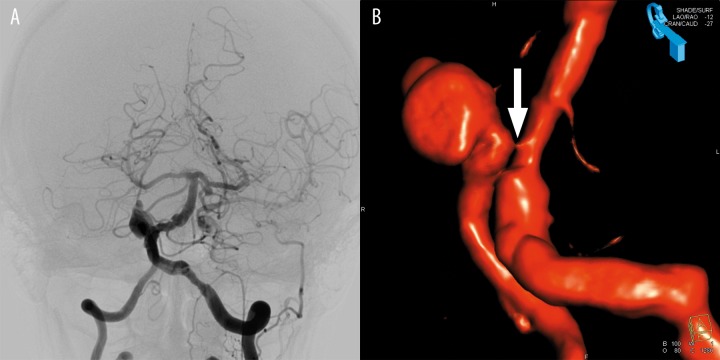
Figure 4.
Conventional angiography, presenting an aneurysm at the region of vertebrobasilar junction, does not allow for determination of the lesion origin (A). A three-dimensional reconstruction localized an aneurysm on the right vertebral artery (RVA), and detected a critical stenosis at the RVA orifice (B, arrow). Because an occlusion of the right subclavian artery was also found, the right brachial access to the RVA was chosen for embolization.
Figure 5.
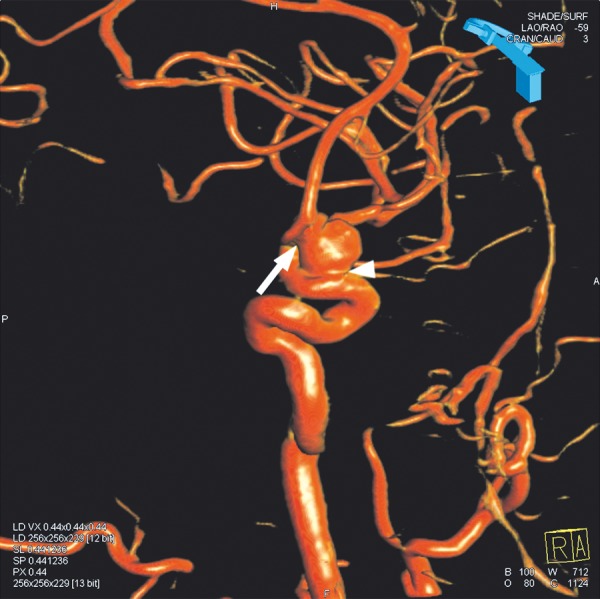
Volume averaging effect simulates a junction between the aneurysm and the anterior cerebral artery (arrow), and the existence of wide neck (arrowhead).
Intraoperative Aneurysm Imaging
A proper evaluation of the contrast filling of an aneurysm is essential for making the decision about finishing the embolization. Three-dimensional reconstructions provide a strict differentiation between the embolic material and the blood flow, owing to which it is possible to assess the completeness of embolization (Figure 6). However, in some cases, conventional 2D images may be confusing in this regard, due to pulsatile motions of both the vessels and the aneurysm, resulting in movement artifacts (Figures 7, 8). These artifacts may simulate contrast filling on subtracted images, leading to an unnecessary prolongation of the procedure. Intracranial stents are hardly visible on fluoroscopy and roadmapping images because of their specific design [7] The use of 3D DSA allows for a precise stent localization and determination of actual aneurysm filling (Figure 9).
Figure 6.
Reconstruction made during embolization of the basilar tip two-compartmental aneurysm. Note the non-embolized portion of the aneurysm (arrows).
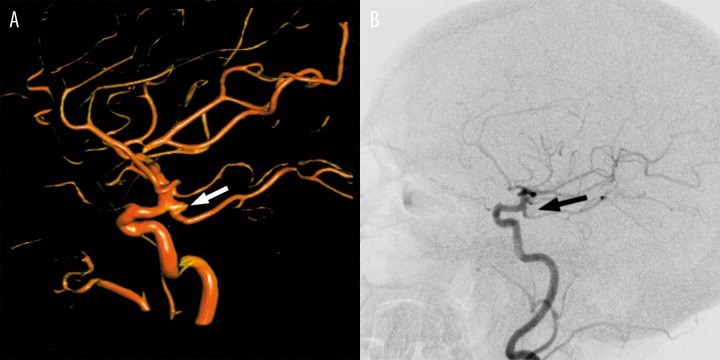
Figure 7.
Artifacts caused by pulsatile motions simulate residual contrast filling on conventional DSA image (A, arrow). The residual filling may be excluded based on 3D reconstruction (B).
Figure 8.

Reconstruction made immediately after complete embolization of a left internal carotid artery. Note the artifacts mimicking residual blood flow (arrow).
Figure 9.
Intracranial remodeling stents: Neuroform3 in the right vertebral artery (A), and Leo in the right internal carotid artery (B). Both stents are hardly visible on conventional DSA images (C,D, respectively, arrows).
Follow-up After Aneurysm Treatment
Detection of an aneurysm recurrence is crucial for patient’s prognosis, because incomplete occlusion of the aneurysm may result in serious or fatal consequences [8]. Follow-up of embolized aneurysms with 3D DSA enables the detection of a residual flow, localization of its origin, and evaluation of adjacent vessel branches (Figures 10, 11). Since the size of the leakage is crucial for the decision on reembolization, three-dimensional measurement of the refilling area without the need for calibration is very helpful. Moreover, it is proposed that magnetic resonance angiography (MRA) should be a primary follow-up imaging modality after coiling, because it offers similar diagnostic performance, is cheaper, safer, and less time-consuming [8,9]. Therefore, 3D DSA remains a reference method for cases of inconclusive MR results, and a method of confirmation of a detected recanalization.
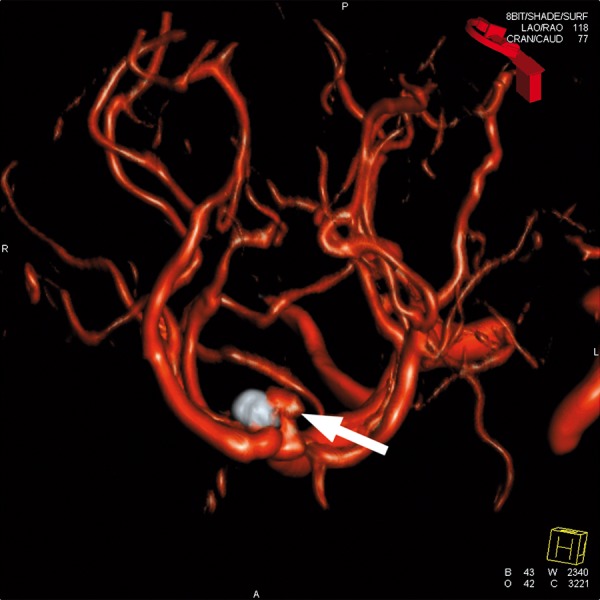
Figure 10.
Recanalization of the right internal carotid artery aneurysm. The recanalization is apparent on the 3D reconstruction (A, arrow), but not on 2D subtracted image (B, arrow).
Figure 11.
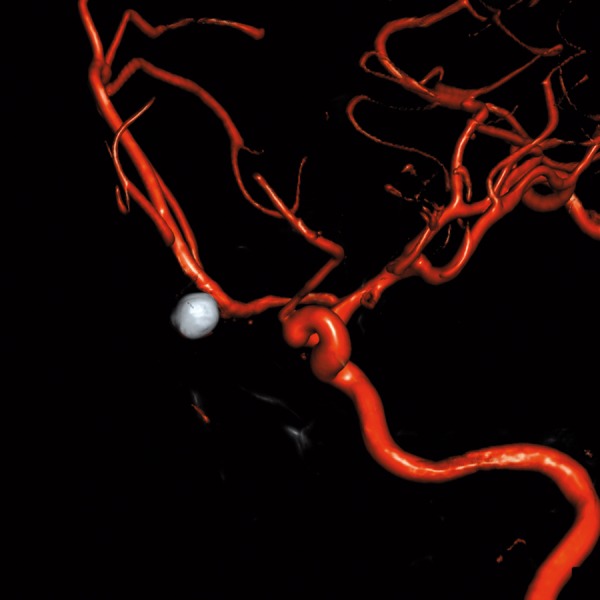
Completely embolized aneurysm of the anterior communicating artery without features of recanalization.
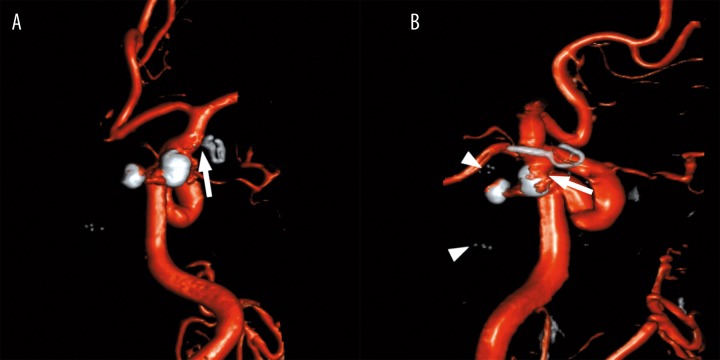
In the case of surgically clipped aneurysms, computed tomography angiography (CTA) become a method of choice for follow-up, because of its non-invasiveness and the lower cost [10]. 3D DSA may be used as a second imaging modality in patients with multiple or cobalt clips (Figure 12), and in case of unequivocal results of CTA.
Figure 12.
Follow-up of clipped and coiled aneurysms. A projection axial to the surgical clip confirmed there was no neck remnant (arrow) of the RICA aneurysm (A). In this patient, the follow-up angiography was scheduled instead of CTA due to multiple metallic implants (B). Note the partially recanalized RICA aneurysm (arrow), the embolized LICA aneurysm, and the stent in the LICA (arrowheads).
Current Role of 3D DSA for Imaging of Intracranial Aneurysms
Despite its technological advancement, 3D DSA has a margin of false findings, which result mainly from pulsatile motions and volume averaging effect. False-negative results may be reflected by an underestimation of the actual aneurysm size by as much as 20% [11]. Pulsatile aneurysm motion, which prevents an optimal image reconstruction, may result in a false-positive diagnosis of residual flow within the embolized aneurysm, especially on the surface of the coil mesh (Figure 8). Moreover, volumetric 3D DSA was reported to overestimate the aneurysm neck size, which may lead to an abuse of remodeling techniques or to change the treatment towards open surgery [6]. Finally, both false-positive and false-negative results of volumetric reconstructions may result from an inappropriate image adjustment [6], which tend to hide small image details or to enhance artifacts. Therefore, reconstructed images therefore always have to be compared with native 2D images.
The current role of 3D DSA for imaging of intracranial aneurysms is generally related to the intended endovascular treatment [2]. The method is commonly used for detection of aneurysms in cases of SAH, when the diagnosis is followed by an embolization. Consequently, 3D DSA is useful for intra-operative imaging, and for planning of reembolization. As a method of reference, 3D DSA is also performed in patients with SAH and a negative result of 2D DSA, CTA, or MRA [3,5]. The follow-up with the use of 3D DSA is restricted to cases when stents, coils protruding into the parent artery, or surgical clips produce artifacts on MRA or CTA image hampering sufficient evaluation of the lesion and adjacent arteries.
Conclusions
Volumetric reconstructions of 3D DSA are a valuable tool for imaging of cerebral vessels. They play a vital role in the intraoperative assessment of intracranial aneurysms, especially in evaluation of the aneurysm neck and residual aneurysm flow. However, because of volume averaging and lower spatial resolution than in case of conventional DSA, reconstructed images always have to be compared with native 2D images.
Footnotes
Source of support: This paper was supported by a scientific grant from Nicolaus Copernicus University, Toruń, Poland
References:
- 1.Sugahara T, Korogi Y, Nakashima K, et al. Comparison of 2D and 3D digital subtraction angiography in evaluation of intracranial aneurysms. Am J Neuroradiol. 2002;23:1545–52. [PMC free article] [PubMed] [Google Scholar]
- 2.Anxionnat R, Bracard S, Ducrocq X, et al. Intracranial aneurysms: clinical value of 3D digital subtraction angiography in the therapeutic decision and endovascular treatment. Radiology. 2001;218:799–808. doi: 10.1148/radiology.218.3.r01mr09799. [DOI] [PubMed] [Google Scholar]
- 3.van Rooij WJ, Sprengers ME, de Gast AN, et al. 3D rotational angiography: the new old standard in the detection of additional intracranial aneurysms. Am J Neuroradiol. 2008;29:976–79. doi: 10.3174/ajnr.A0964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhou B, Li MH, Wang W, et al. Three-dimensional volume-rendering technique in the angiographic follow-up of intracranial aneurysms embolized with coils. J Neurosurg. 2010;112:674–80. doi: 10.3171/2009.7.JNS081718. [DOI] [PubMed] [Google Scholar]
- 5.Ishihara H, Kato S, Akimura T, et al. Angiogram-negative subarachnoid hemorrhage in the era of three dimensional rotational angiography. J Clin Neurosci. 2007;14:252–55. doi: 10.1016/j.jocn.2006.01.011. [DOI] [PubMed] [Google Scholar]
- 6.Brinjikji W, Cloft H, Lanzino G, et al. Comparison of 2D digital subtraction angiography and 3D rotational angiography in the evaluation of dome-to-neck ratio. Am J Neuroradiol. 2009;30:831–34. doi: 10.3174/ajnr.A1444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Richter G, Engelhorn T, Struffert T, et al. Flat panel detector angiographic CT for stent-assisted coil embolization of broad-based cerebral aneurysms. Am J Neuroradiol. 2007;28:1902–8. doi: 10.3174/ajnr.A0697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.van Rooij WJ, Sluzewski M. Opinion: imaging follow-up after coiling of intracranial aneurysms. Am J Neuroradiol. 2009;30:1646–48. doi: 10.3174/ajnr.A1673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schaafsma JD, Velthuis BK, Majoie CB, et al. Intracranial aneurysms treated with coil placement: test characteristics of follow-up MR angiography. Multicenter study. Radiology. 2010;256:209–18. doi: 10.1148/radiol.10091528. [DOI] [PubMed] [Google Scholar]
- 10.Zachenhofer I, Cejna M, Schuster, et al. Image quality and artefact generation post-cerebral aneurysm clipping using a 64-row multislice computer tomography angiography (MSCTA) technology: A retrospective study and review of the literature. Clin Neurol Neurosurg. 2010;112:386–91. doi: 10.1016/j.clineuro.2010.02.001. [DOI] [PubMed] [Google Scholar]
- 11.Jou LD, Mohamed A, Lee DH, et al. 3D rotational digital subtraction angiography may underestimate intracranial aneurysms: findings from two basilar aneurysms. Am J Neuroradiol. 2007;28:1690–92. doi: 10.3174/ajnr.A0652. [DOI] [PMC free article] [PubMed] [Google Scholar]