Abstract
The aim of this study was to investigate the hepatoprotective effect of Matrine salvianolic acid B salt on carbon tetrachloride (CCl4)-induced hepatic fibrosis in rats. Salvianolic acid B and Matrine has long been used to treat liver fibrosis. Matrine salvianolic acid B salt is a new compound containing Salvianolic acid B and Matrine. Hepatic fibrosis induced by CCl4 was studied in animal models using Wistar rats. Organ coefficient, serum aspartate aminotransferase (AST), alanine aminotransferase (ALT), hexadecenoic acid (HA), laminin (LN), hydroxyproline (Hyp), and glutathione (GSH), malondialdehyde (MDA), superoxide dismutase (SOD) in liver tissues were measured, respectively. Histopathological changes in the livers were studied by hematoxylin-eosin (H&E) staining and Masson Trichrome (MT) examination. The expression of transforming growth factor-β1 (TGF-β1) and α-smooth muscle actin (α-SMA) was observed by immunohistochemical analysis. A significant reduction in serum levels of AST, ALT, HA, LN and Hyp was observed in the Matrine salvianolic acid B salt treated groups, suggesting that the salt had hepatoprotective effects. The depletion of GSH and SOD, as well as MDA accumulation in liver tissues was suppressed by Matrine salvianolic acid B salt too. The expression of TGF-β1 and α-SMA measured by immunohistology was significantly reduced by Matrine salvianolic acid B salt in a dose-dependent manner. Matrine salvianolic acid B salt treatment attenuated the necro-inflammation and fibrogenesis induced by CCl4 injection, and thus it is promising as a therapeutic anti-fibrotic agent against hepatic fibrosis.
Keywords: Carbon tetrachloride, Hepatic fibrosis, Matrine salvianolic acid B salt
Introduction
Hepatic fibrosis is a dynamic process characterized by excessive deposition of extracellular matrix (ECM) components, and can ultimately cause liver cirrhosis. Activation of hepatic stellate cells (HSCs) is the key step during the progress of hepatic fibrosis [1]. Upon activation by liver injuries, HSCs transform into Myofibroblastic cells which are proliferative and fibrogenic, with enhanced production of ECM components including α-smooth muscle actin (α-SMA), hexadecenoic acid (HA) and laminin (LN) [2]. Generally, CCl4 is metabolized by microsomal monooxygenase system (cytochrome P450 2E1) to its active metabolite, this process results in the fragmentation of the lipid peroxide radicals, lipid hydroperoxides and other products, each acting like an active oxidizing agent [3-6]. Furthermore, these processes are immediately followed by the infiltration of inflammatory cells and release of various cytokines and growth factors [6]. Thus, lipid peroxidation caused by free radicals of CCl4 metabolism plays a vital role on the CCl4-induced liver injury [6,7]. In addition to lipid peroxidation, transforming growth factor β1 (TGF-β1) is also an important activator of HSCs in the course of hepatic fibrogenesis [3].
Sophora flavescens ait
Has a wide range of pharmacological and toxicological activities [8]. This herb has been used traditionally in China against several pathophysiological states, such as cancer, viral hepatitis, cardiac arrhythmia, and asthma [9]. Matrine is one of the most important alkaloids extracted from this herb and it exerts a variety of pharmacological effects, such as anti-inflammatory, immunoregulatory, antivirus, anti-fibrosis and anti-tumor [10,11]. In recent years, Matrine has been used in the treatment of chronic liver disease and has a significant effect on the inhibition of liver fibrosis [12].
Salvia miltiorrhiza Bge
Is a well-known traditional Chinese herb which is broadly planted in China. It has been used clinically for the treatment of various diseases such as cardiovascular, cerebrovascular, hyperlipidemia, and acute ischemic stroke diseases [13] and has increasingly attracted the attention of research groups in recent years especially in biotechnological field. Salvianolic acid B (Sal-B) is one of the water-soluble components of this herb. Previous studies have shown that Salvianolic acid B is effective in improving liver function, alleviating ischemic damage, antioxidation, antihepatotoxicity and anticoagulation [14]. At present, the pharmacology activity of the salvianolic acid B magnesium salt has been widely studied [15].
In order to obtain the cheap and highly efficient anti-fibrosis drug, we adopted salvianolic acid B and Matrine as raw materials to prepare Matrine salvianolic acid B salt, which is first reported in this article. The structural of Matrine salvianolic acid B salt has been confirmed by the technique of TLC, UV, IR, NMR and TG-DSC. Matrine salvianolic acid B salt has a good stability and can overcome the shortcomings of salvianolic acid B and Matrine [16]. Previous studies have shown its protective effect against acute hepatotoxicity by reducing serum AST and ALT levels induced by the treatment of CCl4, Thioacetamide(TAA) and D-Galactosamine (D-GalN) respectively in mice. The present study aimed to investigate the protective effects of Matrine salvianolic acid B salt on the liver fibrosis induced by CCl4. ( Additional file 1).
Materials and methods
Drug material
Matrine (blanc needle crystal, >98%) was obtained from Shan xi yi xing biological engineering limited company (Shanxi, China). Salvianolic acid B (amber powder, >95%) and Matrine salvianolic acid B salt (amber powder) were prepared by ourself. The voucher specimen (No. 20070816066) is deposited in School of Pharmacy faculty, Shihezi University.
Animals
Wistar Albino rats weighing between 180 and 250 g were used with free access to food and water. Rats were housed at room temperature with 12 h light/dark cycle. The use of these animals was approved by the institute ethnics committee of Shihezi University. The chronic liver injury was induced by CCl4 injection as previously described [5-7]. Rats were randomized into eight groups (n = 12 in each group). The normal control group was allowed free access to food and water; Liver injury was performed in the remaining seven groups by i.p. 1.0 ml/kg CCl4 and olive oil (2:3 v/v) mixture, twice in a week for 8 weeks. The rats of the remaining seven groups except the model group were intragastric (i.g.) administrated quantum satis (q.s.) dosages respectively (Matrine salvianolic acid B salt group: 25 mg/kg, 50 mg/kg, 100 mg/kg respectively; Matrine control group: 50 mg/kg; Salvianolic acid B control group: 150 mg/kg; Positive control group: 780 mg/kg). Orally administration of different drugs were performed at the day before CCl4 administration, and applied once per day for 8 weeks.
Rats were sacrificed by cervical dislocation on the day after the last intragastrical administration. Blood and liver tissue samples were harvested for further examinations. Serum was obtained by the centrifuge at 3,000 rpm for 10 min under 4°C, and stored at −20°C before use. Liver tissues were collected for the measurements of glutathione (GSH), malondialdehyde (MDA), superoxide dismutase (SOD), as well as the histopathological changes.
Biochemical analysis
At 12 h after last intragastrical administration, rats were killed. The blood sample were collected and then centrifuged at 3,000 rpm for 10 min at 4°C. Serum Aspartate aminotransferase (AST) and Alanine aminotransferase (ALT) were determined using Olympus kits (Olympus Corp., Tokyo, Japan) in an Olympus AU 600 Autoanalyzer. The observation absorbance of the reaction was read at 505 nm and the enzyme activity was calculated as U/L.
Serum Hexadecenoic acid (HA), Laminin (LN) and Hydroxyproline (Hyp) levels were measured by the enzyme-linked immunosorbent assay method using the kit obtained from Sigma-Aldrich Chemicals Co., USA. The observation absorbance of the reaction was read at 450 nm.
Measurement of malondialdehyde (MDA) formation in lipid peroxidation
Liver homogenate (10%, w/v) was prepared by homogenizing the liver tissue in 150 mM Tris–HCl buffered saline (pH 7.2) with a polytron homogenizer. The level of MDA in liver tissues was measured by following the protocol provided by the kit from Jiancheng Biological Engineering Institute (Nanjing, China).
Determination of antioxidant and antioxidant enzyme activity
SOD activity was determined by the commercial kit from Jiancheng Biological Engineering Institute (Nanjing, China) following the protocol provided by manufacture. Data are expressed as SOD U/mg protein. The measurement of GSH was conducted by modified protocol provided by GSH kit from Jiancheng Biological Engineering Institute (Nanjing, China). The observation absorbance of the reaction was read at 420 nm and the enzyme activity was calculated as mg/g protein. The protein content was measured by the methods of Lowry et al. (1951) with bovine serum albumin as a standard.
Histopathological evaluation
Four-micrometer-thick sections obtained from paraffin blocks were stained by hematoxylin-eosin (H&E) and Masson trichrome (MT), and then examined with an Olympus BX-50 microscope by × 40, ×100, ×200, and × 400 magnifications. The histopathological evaluation was performed by an expert pathologist blinded to the study groups. The sections, stained with H&E, were examined by light microscopy by × 200 magnification. In the sections stained with MT, the central vein was focused, and the images randomly taken from ten fields were evaluated using image analysis, a specially designed software program by × 200 magnification. The liver damage was graded as following: _, absent; +, few; ++, mild and +++, moderate. Hepatic fibrosis was graded according to the method of Ruwart et al. (1989) [17] as the following: _, absent, normal liver; +, few, increase of collagen without formation of septa; ++, mild, formation of incomplete septa from portal tract to central vein (septa that do not interconnect with each other); and +++, moderate, complete but thin septa interconnecting with each other (incomplete cirrhosis). The final numerical score was calculated by dividing the sum of the number per grade of affected rat by the total number of examined rat.
Immunohistological analysis
The activation of HSCs was identified by immunohistochemical analysis, staining by monoclonal α-SMA and TGF-β1 antibody in deparaffinized tissue sections. Paraffin section deparaffinage, use distilled water and 0.1 mol•L−1 PBS flush 5 min respectively; Then use 3% H2O2 incubation 10 min in room temperature, in order to deactivation endogenous peroxydase; Use 0.1 mol•L−1 PBS flush 5 min, three times, normo-goat serum 37°C blockage 30 min; Dropwise 1:50 diluted primary antibody 4°C to stay overnight, 0.1 mol•L–1 PBS flush 5 min, three times; Then dropwise 1:100 diluted biotinylation goat anti-rabbit secondary antibody, 37°C incubation 20 min; 0.1 mol•L−1 PBS flush 5 min, three times, dropwise SP, 37°C incubation 20 min; Use 0.1 mol•L−1 PBS flush 5 min, three times, DAB colouration; Distilled water flush, termination colouration; Hematoxylin counterstain; Gradient alcoholic dehydration, dimethyl benzene transparent and neutro-resin mounting. Observed under the microscope, the positive part shows Buffy.
Statistical analysis
All Data were expressed as Means ± Standard Deviations, and analyzed with one-way analysis of variance (ANOVA). Statistical significance was analyzed by SPSS software using LSD’s test.
Results
The effect of Matrine salvianolic acid B salt on body weight decreasing induced by CCl4 treatment
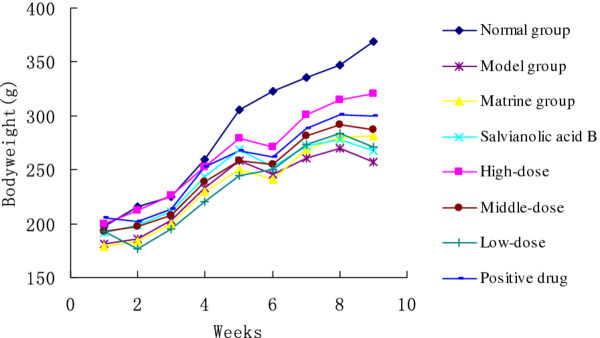
There was no significant difference among the mean initial body weights of all groups (p < 0.05, Figure 1). However, body weights of CCl4-and drug-treatment groups were lower than that of the control group by the end of the study (p < 0.05 for three doses of Matrine salvianolic acid B salt group, Figure 1). And there was no significant dose-respond relationship on the decreasing of body weight among drug-treatment groups (p < 0.05, Figure 1).
Figure 1.
The body weight of animals in the control, CCl4- and drug-treated groups.
The effect of Matrine salvianolic acid B salt on organ coefficient increasing induced by CCl4 treatment
Organ coefficients including liver, spleen and kidney coefficients were evaluated in rats. Similar to previous studies [18], liver and spleen coefficients were significantly increased in rats with CCl4-treatment (p < 0.01, Table 1); In contrast, there is no difference in kidney coefficient among all treated groups. As demonstrated in Table 1, the increase of liver coefficient caused by CCl4 treatment in rats was reduced by Salvianolic acid B (150 mg/kg), Matrine salvianolic acid B salt (25, 50, and 100 mg/kg), and Fu fang bie jia ruan gan pian treatment (780 mg/kg) individually (p < 0.05, Table 1), expect for Matrine treatment. Then the protective effect against the increase of spleen coefficient was observed in rats with Matrine (50 mg/kg), Matrine salvianolic acid B salt (25, 50 and 100 mg/kg) and Fu fang bie jia ruan gan pian treatment (780 mg/kg) (p < 0.01, Table 1), expect for Salvianolic acid B treatment (150 mg/kg). Dose-effect correlation was observed in Matrine salvianolic acid B salt groups regarding to the increase of liver and spleen coefficient by CCl4-treatment.
Table 1.
Effect of Matrine salvianolic acid B salt on organ coefficient in hepotic fibrosis rats
| Treatment | Doses (mg/kg) |
Liver coefficient % | Spleen coefficient % |
Kidney coefficient % |
|---|---|---|---|---|
| Normal control |
—— |
2.55 ± 0.23 |
0.19 ± 0.05 |
0.73 ± 0.04 |
| CCl4 |
—— |
3.53 ± 0.37## |
0.27 ± 0.04## |
0.71 ± 0.10 |
| Matrine+ CCl4 |
50 |
3.33 ± 0.19 |
0.20 ± 0.03** |
0.75 ± 0.19 |
| Salvianolic acid B+ CCl4 |
150 |
3.14 ± 0.55* |
0.26 ± 0.02 |
0.76 ± 0.16 |
| |
25 |
3.18 ± 0.46* |
0.21 ± 0.03** |
0.73 ± 0.13 |
| Matrine salvianolic acid B Salt+ CCl4 |
50 |
3.17 ± 0.26* |
0.20 ± 0.04** |
0.71 ± 0.17 |
| |
100 |
3.16 ± 0.49* |
0.19 ± 0.05** |
0.67 ± 0.12 |
| Fu fang bie jia ruan gan pian+ CCl4 | 780 | 3.16 ± 0.35* | 0.20 ± 0.04** | 0.72 ± 0.08 |
Data is expressed as the mean±SD (n = 12).
##p < 0.01 vs. the normal control group; *p < 0.05, **p < 0.01 vs. the CCl4-treated group.
The effect of Matrine salvianolic acid B salt on the increase of serum AST and ALT in rats
There were dramatic increases of serum ALT and AST after CCl4 treatment in rats, which were 4 and 6 times higher compared to that of control group (p < 0.01, Table 2). Consistent with previous studies [19], Fu fang bie jia ruan gan pian treatment (780 mg/kg) showed a significantly protective effect against the increase of serum ALT and AST after long-term CCl4 injection in rats (p < 0.01, Table 2). Similarly, Matrine (50 mg/kg) and Salvianolic acid B treatment (150 mg/kg) decreased the elevation of serum ALT and AST to the level relevant to that of Fu fang bie jia ruan gan pian group after long-term CCl4 injection in rats (p < 0.01, Table 2). Furthermore, the decrease of serum ALT and AST in rats treated with CCl4 was observed in Matrine salvianolic acid B salt groups (25, 50 and 100 mg/kg), and the doses of Matrine salvianolic acid B salt 100 mg/kg showed a significantly protective effect (p < 0.01, Table 2).
Table 2.
Effect of Matrine salvianolic acid B salt on AST and ALT in rats
| Treatment | Doses (mg/kg) | AST (U/L) | ALT (U/L) |
|---|---|---|---|
| Normal control |
—— |
45.59 ± 3.68 |
32.12 ± 14.09 |
| CCl4 |
—— |
211.20 ± 42.07## |
221.24 ± 42.35## |
| Matrine+ CCl4 |
50 |
142.87 ± 36.99** |
138.87 ± 32.67** |
| Salvianolic acid B+ CCl4 |
150 |
104.22 ± 20.67** |
154.92 ± 60.64** |
| Matrine salvianolic acid B Salt+ CCl4 |
25 |
159.10 ± 46.19** |
169.92 ± 51.42** |
| 50 |
119.80 ± 25.69** |
144.33 ± 44.93** |
|
| 100 |
102.49 ± 25.71**b |
96.09 ± 27.28**ac |
|
| Fu fang bie jia ruan gan pian+ CCl4 | 780 | 110.3 ± 26.62** | 117.26 ± 40.70** |
Data is expressed as the mean±SD (n = 12).
##p < 0.01 vs. the normal control group; **p < 0.01 vs. the CCl4-treated group;
ap < 0.05, bp < 0.01 vs. the Matrine group; cp < 0.01 vs. the Salvianolic acid B group.
The effect of Matrine salvianolic acid B salt on the increase of serum HA, LN and Hyp in rats
After CCl4 admimistration, the levels of serum HA, LN and Hyp were significantly increased, compared with that of control group (p < 0.01, Table 3). However, treatment with Fu fang bie jia ruan gan pian (780 mg/kg) significantly decreased the levels of serum LN and HyP induced by CCl4 (p < 0.05, p < 0.01, Table 3), While there is no significant difference between the levels of HA. Meanwhile, Matrine (50 mg/kg) and Salvianolic acid B treatment (150 mg/kg) markedly decreased the elevation of serum HA, LN and HyP after long-term CCl4 injection in rats (p < 0.05, p < 0.01, Table 3). In addition, except the levels of LN in the group of 25 mg/kg Salt + CCl4, the levels of serum HA, LN and Hyp were all lower in the Matrine salvianolic acid B salt three doses group compared to CCl4-treated group (p < 0.05, p < 0.01, Table 3). Moreover, it has showed a good dose-effect relationship in various doses of Matrine salvianolic acid B salt.
Table 3.
Effect of Matrine salvianolic acid B salt on HA, LN and Hyp in rats
| Treatment | Doses (mg/kg) |
HA (ng/ml) | LN (ng/ml) | HyP (ng/ml) |
|---|---|---|---|---|
| Normal control |
—— |
213.46 ± 21.62 |
85.39 ± 3.98 |
16.38 ± 1.30 |
| CCl4 |
—— |
328.71 ± 18.42## |
109.93 ± 18.16## |
32.34 ± 6.41## |
| Matrine+ CCl4 |
50 |
292.49 ± 30.73* |
94.79 ± 19.24* |
27.14 ± 1.58** |
| Salvianolic acid B+ CCl4 |
150 |
290.66 ± 53.77* |
88.36 ± 19.44** |
22.25 ± 1.88** |
| |
25 |
289.88 ± 27.00* |
99.79 ± 23.42 |
19.71 ± 1.52**bc |
| Matrine salvianolic acid B Salt+ CCl4 |
50 |
276.77 ± 47.19** |
85.61 ± 14.21** |
19.14 ± 1.86**bd |
| |
100 |
264.70 ± 49.62** |
81.61 ± 16.22**a |
18.65 ± 1.94**bd |
| Fu fang bie jia ruan gan pian+ CCl4 | 780 | 299.76 ± 33.99 | 97.37 ± 15.35* | 18.86 ± 1.79** |
Data is expressed as the mean±SD (n = 12).
##p < 0.01 vs. the normal control group; *p < 0.05, **p < 0.01 vs. the CCl4-treated group;
ap < 0.05, bp < 0.01 vs. the Matrine group; cp < 0.05, dp < 0.01 vs. the Salvianolic acid B group.
The effect of Matrine salvianolic acid B salt on liver tissue GSH, MDA and SOD levels in rats
GSH and SOD could scavenge the lipid peroxide radicals, lipid hydroperoxides and other products which is a toxic metabolite of the CCl4. Therefore, we measured the contents of GSH and SOD in liver tissue of rats. From Table 4, we can clearly see the vast difference between CCl4-treated group and the control group, the levels of GSH and SOD were largely decreased (p < 0.01, Table 4) in CCl4-treated group compared with that of control group. The levels of GSH in Fu fang bie jia ruan gan pian treatment had significantly increased (p < 0.01, Table 4), while there was no significant difference in the level of SOD compared to the group of CCl4. After Salvianolic acid B treatment, The levels of GSH and SOD were higher than CCl4 treatment, but no significant difference. However, treatment with Matrine salvianolic acid B salt (25, 50 and 100 mg/kg) significantly recovered the CCl4-induced GSH and SOD depletion (p < 0.05, p < 0.01, Table 4). In addition, CCl4 rats exhibited a significant increase in hepatic MDA (a marker of lipid peroxidation levels) (p < 0.01, Table 4), when compared with the control group. On the other hand, treatment with Matrine salvianolic acid B salt (25, 50 and 100 mg/kg) showed a significant decrease in MDA levels with a dose-dependent manner, to 2.58 ± 0.62, 2.11 ± 0.31 (p < 0.01, Table 4) and 1.79 ± 0.43 (p < 0.01, Table 4) respectively.
Table 4.
Effect of Matrine salvianolic acid B salt on GSH, MDA and SOD in rats
| Treatment | Doses (mg/kg) |
GSH (mg/gprotein) |
MDA (nmol/mgprotein) |
SOD (U/mg protein) |
|---|---|---|---|---|
| Normal control |
—— |
3.00 ± 0.14 |
1.03 ± 0.22 |
262.95 ± 30.43 |
| CCl4 |
—— |
1.85 ± 0.28## |
3.00 ± 0.45## |
151.95 ± 20.25## |
| Matrine + CCl4 |
50 |
2.36 ± 0.53** |
2.52 ± 0.87 |
151.74 ± 11.44 |
| Salvianolic acid B + CCl4 |
150 |
2.16 ± 0.65 |
2.12 ± 0.43** |
159.85 ± 22.28 |
| |
25 |
2.28 ± 0.59* |
2.58 ± 0.62 |
169.94 ± 25.16 |
| Matrine salvianolic acid B Salt + CCl4 |
50 |
2.48 ± 0.33** |
2.11 ± 0.31** |
184.65 ± 24.90**ab |
| |
100 |
2.63 ± 0.29**b |
1.79 ± 0.43**a |
191.71 ± 48.32**ac |
| Fu fang bie jia ruan gan pian + CCl4 | 780 | 2.52 ± 0.32** | 1.76 ± 0.76** | 171.39 ± 28.90 |
Data is expressed as the mean±SD (n = 12).
##p < 0.01 vs. the normal control group; *p < 0.05, **p < 0.01 vs. the CCl4-treated group;
ap < 0.01 vs. the Matrine group; bp < 0.05, cp < 0.01 vs. the Salvianolic acid B group.
The effect of Matrine salvianolic acid B salt on histopathological evaluation
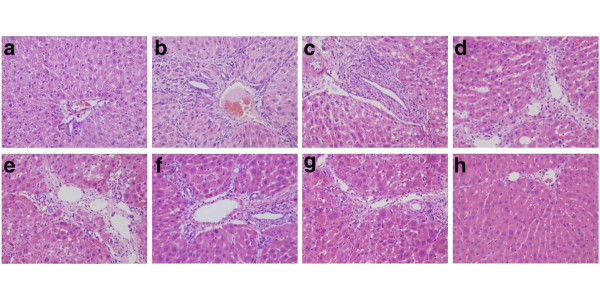
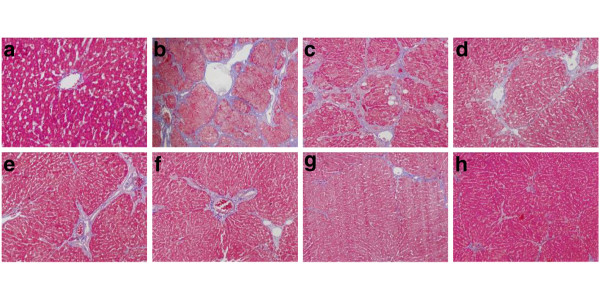
In normal control group, liver sections showed normal hepatic cells with well preserved cytoplasm, prominent nucleolus and central vein (Figure 2a). The liver sections of CCl4 treated group showed a moderate degree of centrilobular necrosis, and mild degree of leukocytes infiltration, bile duct proliferation, mitosis and calcification (Figure 2b). The histological pattern of the livers treated by Matrine salvianolic acid B salt showed a few to milder degree of infiltration of leukocytes, absent to few degree of necrosis, and bile duct proliferation (Figure 2e, f and g). Similar trends were also observed in group of Fu fang bie jia ruan gan pian (Figure 2h). The histological observations also supported the results obtained from the serum enzyme assay. Further, histopathological changes of fibrosis occurred in CCl4-intoxicated and prevention by the treatment with Matrine salvianolic acid B salt are shown in Figure 3 The livers of rat treated with CCl4 showed extensive accumulation of connective tissue resulting in formation of continuous fibrotic septa, nodules of regeneration, and noticeable alterations in the central vein as compared to the normal control (Figure 3a and b). The group treated with Matrine salvianolic acid B salt and Fu fang bie jia ruan gan pian resulted in less pronounced destruction of the liver architecture without fibrosis (Figure 3e, f, g and h). According to microscopic examinations, severe hepatic fibrosis induced by CCl4 was remarkably reduced by the administration of Matrine salvianolic acid B salt, which was in good correlation with the results of the serum aminotransferase activities and hepatic antioxidant enzyme activities.
Figure 2.
The H&E (×200) of the liver sections in rats. (a) Normal group; (b) CCl4-treated group; (c) Matrine + CCl4; (d) Salvianolic acid B + CCl4; (e), (f) and (g) are Matrine salvianolic acid B salt group treated with 25, 50 and 100 mg/kg respectively; (h) Positive-drug + CCl4.
Figure 3.
The MT examinations (×200) of the liver sections in rats. (a) Normal group; (b) CCl4-treated group; (c) Matrine + CCl4; (d) Salvianolic acid B + CCl4; (e), (f) and (g) are Matrine salvianolic acid B salt group treated with 25, 50 and 100 mg/kg respectively; (h) Positive-drug + CCl4.
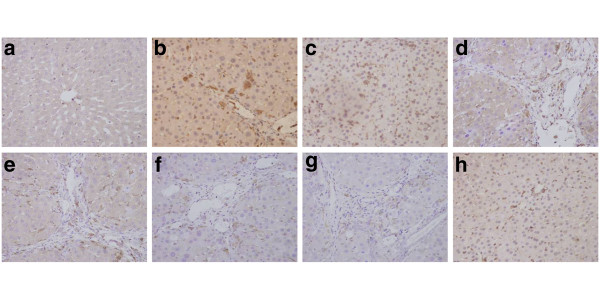
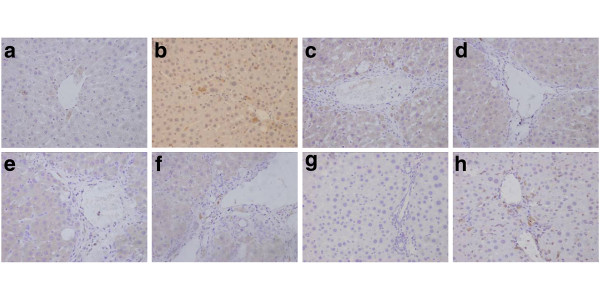
The effect of Matrine salvianolic acid B salt on immunohistochemistry analisis
Histological examination of livers from CCl4 rats revealed the increase and expansion of fibrous septa, compared with normal control rats. α-SMA and TGF-β1 expression were more distinctly observed in the liver of CCl4 rats as compared with normal control rats (Figure 4a, b and Figure 5a, b). Treatment with Matrine salvianolic acid B salt decreased α-SMA and TGF-β1 staining (Figure 4e, f, g and Figure 5e, f, g). The fibrosis score in CCl4 rats was significantly increased as compared to that of control rats, and treatment of Matrine salvianolic acid B salt significantly ameliorated hepatic fibrosis in CCl4 rats. Similarly, protein components of α-SMA and TGF-β1 were significantly down-regulated in the group of Matrine, Salvianolic acid B and Fu fang bie jia ruan gan pian. Moreover, ascite was detected in three rats from the CCl4-treated group with an odds ratio, while it was not observed in the other groups (Figures 4 and 5).
Figure 4.
The immunohistochemical examination of α-SMA positive cells (×400) of the liver sections in rats. (a) Normal group; (b) CCl4 -treated group; (c) Matrine + CCl4; (d) Salvianolic acid B + CCl4; (e), (f) and (g) are Matrine salvianolic acid B salt group treated with 25, 50 and 100 mg/kg respectively; (h) Positive-drug + CCl4.
Figure 5.
The immunohistochemical examination of TGF-β1positive cells (×400) of the liver sections in rats. (a) Normal group; (b) CCl4-treated group; (c) Matrine + CCl4; (d) Salvianolic acid B + CCl4; (e), (f) and (g) are Matrine salvianolic acid B salt group treated with 25, 50 and 100 mg/kg respectively; (h) Positive-drug + CCl4.
Discussion
CCI4-induced toxic liver injury which is a well characterized model for hepatic fibrosis has been extensively performed [5,6]. Hepatic fibrosis is a dynamic cascade beginning with hepatocyte necrosis followed by the activation of the inflammatory cells including macrophage, the activation and proliferation of HSCs, and the release of fibrogenic mediators [20]. AST and ALT are the aminotransferase in liver cells. They are cytoplasmic in nature, but upon liver injury these enzymes enter into the circulatory system due to altered permeability of membrane. So the elevated serum ALT and AST levels were indicative of hepatotoxicity. In addition, excessive deposition of extracellular matrix components such as collagen protein, proteoglycan and osamine protein is also an important factor in liver fibrosis. HA is an important composition of Connective tissue matrix, which participate to form proteoglycan. HyP is mainly in collagen protein, thus, HA, LN and HyP are an important index to appraisal hepatic fibrosis [21]. In our present study, CCl4 caused a significant elevation of serum levels of ALT and AST in rats, and pretreatment with Matrine salvianolic acid B salt significantly attenuated the increased activities of ALT and AST. Moreover, liver index and levels of serum HA, LN, Hyp were increased in CCl4-treated rats, and Matrine salvianolic acid B salt markedly decreased the levels of serum HA, LN, Hyp and liver index, suggesting its hepatoprotective effects. Histopathological observations further confirmed that liver injury induced by CCl4 was largely prevented by pretreatment of Matrine salvianolic acid B salt,for it has been demonstrated that Matrine salvianolic acid B salt attenuates the necro-inflammatory and fibrogenic effects of CCl4, histopathologically.
CCI4 damages hepatocellular membrane via lipid peroxidation, and this is followed by the release of inflammatory mediators from the activated inflammatory cells which are thought to potentiate CCl4-induced hepatic injury [2,22]. In the present study, the level of lipid peroxide (MDA) in liver tissue was increased and the activities of SOD and GSH were diminished in the CCI4-treated rats. However, pretreatment with Matrine salvianolic acid B salt reduced the amount of MDA and increased the activities of SOD and GSH. Together these evidences suggest that the hepatoprotective effects of Matrine salvianolic acid B salt might be in part due to ability to protect biomembrance against the formation of lipid peroxidation.
It is well known that activation of HSCs plays a key role in the pathogenesis of liver fibrosis [3,20]. In our study, CCl4 enhanced expression of α-SMA, while the administration of Matrine salvianolic acid B salt prevented the development of fibrosis by inhibiting the activation of HSCs, which has been supported by the reduction in the activation of HSCs as seen by immunohistochemical staining of α-SMA. It has been reported that the activation of HSCs is associated with the elevation of NF-κB activity, and it is well known that cytokines including TGF-β1 activate NF-κB signaling [23]. TGF-β1 is the most important profibrotic cytokine, and it enhances the type I procollagen synthesis [24,25]. Previous study reported that, proliferation of fibroblast and production of collagen are enhanced by growth factors such as TGF-β1. It has been reported that anti-TGF-β1 antibody ameliorates concanavalin A-induced hepatic fibrosis [26]. In our study, administration of Matrine salvianolic acid B salt relatively reduced the increased levels of TGF-β1 induced by CCl4 and therefore, it may be speculated that the anti-fibrotic effect of Matrine salvianolic acid B salt may be mediated by its suppressory effect on TGF-β1.
In conclusion, it seems that administration of Matrine salvianolic acid B salt is effective in preventing necro-inflammation and fibrogenesis in hepatic fibrosis induced by CCl4. Moreover, Matrine salvianolic acid B salt is a newly prepared compound. This complexes containing one molecular of Salvianolic acid B and one molecular of alkaloids (Matrine). In our study, we can also clearly see the hepatoprotective effect of Matrine salvianolic acid B salt is better than the two monomer componds, indicating Matrine salvianolic acid B salt might be a valuable hepatoprotective agent.
The hepatoprotective effect of Matrine salvianolic acid B salt treatment against CCl4-induced hepatic injury seems to be related to the inhibition of lipid peroxidation and levels of TGF-β1, the most important inflammatory mediator. However, fibrogenesis may occur as a consequence of an ongoing inflammatory process. Therefore, it is difficult to speculate whether the attenuation of fibrosis by Matrine salvianolic acid B salt is merely a reflection of direct effect on fibrogenesis itself. Further experimental studies are necessary to determine the role and mechanisms of Matrine salvianolic acid B salt in the treatment of hepatic fibrogenesis.
Authors’ contributions
The author, Hong-Ying Gao carried out the hepatoprotective effect of Matrine salvianolic acid B salt on carbon tetrachloride (CCl4)-induced hepatic fibrosis in rats, participated in the analysis of the data and drafted the manuscript. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Supplementary Material
Hepatoprotective effect of Matrine salvianolic acid B salt on Carbon Tetrachloride-Induced Hepatic Fibrosis.
Contributor Information
Hong-Ying Gao, Email: gsyunbb@126.com.
Guo-Yu Li, Email: liguoyulisa@163.com.
Meng-Meng Lou, Email: loumeng666@qq.com.
Xiao-Yu Li, Email: 443293224@qq.com.
Xiu-Yan Wei, Email: wei_xiuyan@163.com.
Jin-Hui Wang, Email: wjh.1972@yahoo.com.cn.
Acknowledgements
This work was supported by National Key Technology R&D Program (2012BAI30B02), National Natural Science Foundation (81102785), West Light Program (RCPY200707) and SCI-TECH R & D Program of Shihezi University (ZRKX2009ZD05).
References
- Albanis E, Friedman SL. Hepatic fibrosis. Pathogenesis and principles of therapy. J Clin Liver Dis. 2001;5:315–334. doi: 10.1016/S1089-3261(05)70168-9. [DOI] [PubMed] [Google Scholar]
- Ibrahim HB, Suleyman SK, Orhan KP, Mehmet Y, Ibrahim HO, Bilal U, Ahmet I. Hepatoprotective effect of Infliximab, an Anti-TNF-α Agent, on Carbon Tetrachloride-Induced Hepatic Fibrosis. Inflammation. 2008;31:215–221. doi: 10.1007/s10753-008-9067-1. [DOI] [PubMed] [Google Scholar]
- Lamireau T, Desmouliere A, Bioulac-Sage P. Mechanisms of hepatic fibrogenesis. J Arch Pediatr. 2002;9:392–405. doi: 10.1016/S0929-693X(01)00800-4. [DOI] [PubMed] [Google Scholar]
- Recknagel R, Glende EA, Dolak JA, Waller RL. Mechanisms of carbon tetrachloride toxicity. Pharma Ther. 1989;43:139–154. doi: 10.1016/0163-7258(89)90050-8. [DOI] [PubMed] [Google Scholar]
- Brattin WJ, Glende EA, Recknagel RO. Pathological mechanisms in carbon tetrachloride hepatotoxicity. J Free Radic Biol Med. 1985;1:27–28. doi: 10.1016/0748-5514(85)90026-1. [DOI] [PubMed] [Google Scholar]
- Nadkarni GD, D’Souza NB. Hepatic antioxidant enzymes and lipid peroxidation in carbon tetrachloride-induced liver cirrhosis in rats. Biochem Med Metabol Biol. 1988;40:42–45. doi: 10.1016/0885-4505(88)90102-8. [DOI] [PubMed] [Google Scholar]
- Gassó M, Rubio M, Varela G, Cabré M, Caballería J, Alonso E, Deulofem R, Camps J, Giménez A, Pajares M, Parés A, Mato JM, Rodés J. Effects of S-adenosylmethionine on lipid peroxidation and liver fibrogenesis in carbon tetrachloride-induced cirrhosis. J Hepatol. 1996;25:200–205. doi: 10.1016/S0168-8278(96)80074-2. [DOI] [PubMed] [Google Scholar]
- Jung Y, Wan X, Yan H, Row K. Determination of matrine and oxymatrine in Sophora flavescens ait. Via high performance liquid chromatography. J Liq Chromatogr Related Technol. 2008;31:2752–2761. doi: 10.1080/10826070802388326. [DOI] [Google Scholar]
- Hong M, Lee J, Jung H, Jin D, Go H, Kim J, Jang B, Shin Y, Ko S. Sophora flavescens ait. on inhibits the production of pro-inflammatory cytokines through inhibition of the NF jB/IjB signal pathway in human mast cell line (HMC-1) Toxicol Vitr. 2009;23:251–258. doi: 10.1016/j.tiv.2008.12.002. [DOI] [PubMed] [Google Scholar]
- Cheng H, Xia B, Zhang L, Zhou F, Zhang YX, Ye M, Hu ZG, Li J, Li J, Wang ZL, Li C, Guo QS. Matrine improves 2,4,6-trinitrobenzene sulfonic acid-induced colitis in mice. Pharmacol Res. 2006;53:202–208. doi: 10.1016/j.phrs.2005.11.001. [DOI] [PubMed] [Google Scholar]
- Ma L, Wen S, Zhan Y, He Y, Liu X, Jiang J. Anticancer effects of the chinese medicine matrine on murine hepatocellular carcinoma cells. Planta Med. 2008;74:245–251. doi: 10.1055/s-2008-1034304. [DOI] [PubMed] [Google Scholar]
- Zhang JP, Zhang M, Jin C, Zhou B, Xie WF, Guo C. Matrine inhibits production and actions of fibrogenic cytokines released by mouse peritoneal macrophages. Acta Pharmacol Sin. 2001;22:765–768. [PubMed] [Google Scholar]
- Zhou L, Zuo Z, Chow MSS. Danshen: an overview of its chemistry, pharmacology, pharmacokinetics, and clinical use. J Clin Pharmacol. 2005;45:1345–1359. doi: 10.1177/0091270005282630. [DOI] [PubMed] [Google Scholar]
- Tsai MK, Lin YL, Huang YT. Effects of salvianolic acids on oxidative stress and hepatic fibrosis in rats. Toxicol Appl Pharmacol. 2010;242:155–164. doi: 10.1016/j.taap.2009.10.002. [DOI] [PubMed] [Google Scholar]
- Zhang J. Inhibitory Action of Salvianolic Acid B on the Contraction of Hepatic Stellate Cells Induced by Endothelin and its Mechanism. Shanghai University of Traditional Chinese Medicine, Chinese, Shanghai; 2004. [Google Scholar]
- Gao HY, Li GY, Wang HY, Wang JH. Structure identification of Matrine Salvianolic acid B salt. Mod Chin Med. 2010;12:22–25. [Google Scholar]
- Ruwart MJ, Wilkinson KF, Rush BD. The integrated value of serum procollagen III peptide over time predicts hepatic hydroxyproline content and stainable collagen in a model of dietary cirrhosis in the rat. Hepatology. 1989;10:801–806. doi: 10.1002/hep.1840100509. [DOI] [PubMed] [Google Scholar]
- Tsai CF, Hsu YW, Chen WK, Chang WH, Yen CC, Ho YC, Lu FJ. Hepatoprotective effect of electrolyzed reduced water against carbon tetrachloride-induced liver damage in mice. Food Chem Toxicol. 2009;47:2031–2036. doi: 10.1016/j.fct.2009.05.021. [DOI] [PubMed] [Google Scholar]
- Li J, Niu JZ, Zeng Y. Effects of FFBJRGP on collagen deposition in hepatic Disse space in alcohol induced liver fibrosis in rat. Med J Chin PLA. 2004;29:567–570. [Google Scholar]
- Friedman SL. Liver fibrosis from bench to bedside. J Hepatol. 2003;38:S38–S53. doi: 10.1016/s0168-8278(02)00429-4. [DOI] [PubMed] [Google Scholar]
- Nyberg A, Anna EL, Loof L. Serum hyaluronate in primary biliary cirrhosis: a biochemical marker for progrewssive liver damage. Hepatology. 1988;8:142–146. doi: 10.1002/hep.1840080127. [DOI] [PubMed] [Google Scholar]
- Koca SS, Bahcecioglu IH, Poyrazoglu OK, Ozercan IH, Sahin K, Ustundag B. The treatment with antibody of TNF-alpha reduces the inflammation, necrosis and fibrosis in the non-alcoholic steatohepatitis induced by methionine and cholinedeficient diet. Inflammation. 2007;31:91–98. doi: 10.1007/s10753-007-9053-z. [DOI] [PubMed] [Google Scholar]
- Freedman AR, Sharma RJ, Nabel GJ, Emerson SG, Griffin GE. Cellular distribution of nuclear factor kappa B binding activity in rat liver. Biochem J. 1992;287:645–649. doi: 10.1042/bj2870645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tilg H. The role of cytokines in the pathophysiology of chronic liver diseases. Int J Clin Lab Res. 1993;23:179–185. doi: 10.1007/BF02592306. [DOI] [PubMed] [Google Scholar]
- Gurujeyalakshmi G, Giri SN. Molecular mechanisms of antifibrotic effect of interferon gamma in bleomycin-mouse model of lung fibrosis: down regulation of TGF-beta and procollagen I and III gene expression. Exp Lung Res. 1995;21:791–808. doi: 10.3109/01902149509050842. [DOI] [PubMed] [Google Scholar]
- Kimura K, Ando K, Ohnishi H, Ishikawa T, Kakumu S, Takemura M, Muto Y, Moriwaki H. Immunopathogenesis of hepatic fibrosis in chronic liver injury induced by repeatedly administered concanavalin A. Int Immunol. 1999;11:1491–1500. doi: 10.1093/intimm/11.9.1491. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Hepatoprotective effect of Matrine salvianolic acid B salt on Carbon Tetrachloride-Induced Hepatic Fibrosis.