Abstract
Objective
To examine how persons move back and forth along levels of mobility disability.
Design
Self-reported mobility limitations were used to create categories of annual transition states. The total cost to Medicare associated with each year was calculated for each participant. In addition, we examined cost relative to transition state, adjusting for demographic and other health status variables.
Setting
National survey.
Participants
Participants in the longitudinal Medicare Current Beneficiary Survey from 1992 to 2005.
Interventions
Not applicable.
Main Outcome Measures
Annual self-reported mobility limitations and total Medi costs.
Results
Most participants remained without mobility limitations or improved over time. Reported average costs were 10 times higher for those who transitioned to severe limitations, unable to walk, or death compared with persons who reported no mobility limitation. Estimated costs were highest for those transitioning to increased states of disability and to death.
Conclusions
Mobility limitations in older adults are dynamic, and improvement (as measured by annual transitions) occurred for a large number of Medicare beneficiaries. High total annual costs were observed in groups that transitioned to worsening mobility states, suggesting a link between mobility limitation transitions and cost. Prevention and treatment of mobility limitation may be an important factor to consider in health care reform.
Keywords: Delivery of health care, Disabled persons, Health care reform, Rehabilitation
The concept that disability is either a fixed state or an inevitably worsening process is engrained in our culture and reinforced by definitions of work disability that require long-term limitations to qualify for payments. However, a significant amount of research1-3 and contemporary models of functioning suggest that disability is not necessarily a stable condition.4 Although many persons may become more limited over time, a considerable number also recover. This concept has become increasingly important as we gather more knowledge about the needs of people with disabilities regarding delivery of health care services, satisfaction with care, and associated costs.5-7 What is missing in the literature is an in-depth examination of the probabilities and factors that are associated with disability transitions and the medical costs that may be required to move along the continuum of functioning. A better understanding of this process may help clinicians identify and treat persons with disabilities, and inform policymakers of the disability-related costs in the health care delivery system.
Transition probabilities (the probability of moving from one disability state to another) have been estimated for outcomes related to stroke, osteoarthritis, general health status, and activities of daily living.3, 8-11 There has been some examination of the influence of age suggesting that the oldest adults rarely improve.9 However, other studies, which have evaluated the influence of sex and race on transitions, have produced no consistent findings.1, 8, 10 Diehr and Patrick11 examined self-rated health states for older adults in a longitudinal study. Transition probabilities were found to vary by initial health state, age, and sex. More recent use of transitions has focused on disability in older ages, for those 75 years and older.12 However, although the authors examined longitudinal data (1982-1994), their analysis was limited to 4 states: disabled, nondisabled, nursing home, and deceased. They did not find any consistent trends in their study, although results suggested that few persons were returning to a nondisabled state over time. Other researchers examining trends in disability have found a decreasing prevalence of disability over time.13, 14
In this project, we estimate the transition probabilities among various levels of mobility limitation in older adults. We chose to assess mobility limitations because this domain typically precedes development of limitations in activities of daily living15 and is the strongest predictor of self-perceived disability.16 In addition, it has few floor and ceiling effects, and because of its tight link to falls, it is highly associated to health care costs.17, 18 Using the MCBS, we estimated the probabilities of transition among mobility limitation states in the Medicare population. We evaluated the relationship between those transitions and total Medicare costs incurred during the year between the 2 mobility assessments. Finally, we estimated total cost based on individual characteristics, including type of transition of mobility limitation.
METHODS
Survey Sample
The sample was composed of persons who participated in the MCBS from 1992 to 2005. This ongoing national survey selects a representative sample from all Medicare beneficiaries enrolled during a calendar year by using a multistage sampling procedure, which divides the United States into 107 geographic primary sampling units, each composed of a group of counties. Primary sampling units are subdivided into zip code areas, within which systematic random samples stratified by age are collected. Participants are enrolled in the MCBS for up to 4 years (5 years in the first years of the survey) and are interviewed regarding various aspects of their health status (once a year) and health care utilization (2 more interviews 4 months apart). Demographic and health status variables are collected in the autumn quarter, while survival and health-related costs refer to the entire year period. More details about the MCBS study design can be found at http://www.cms.hhs.gov/MCBS/.19
Data Description
Data were drawn from responses of participants 65 years or older at the time of their first interview. The number of participants per calendar year varied from 10,000 to 17,000, and most years had 12,000 to 13,000 participants. Proxy respondents varied from 10% to 13%. Each participant had from 1 to 4 interviews, with some (2.9% of the sample) having 5 interviews. The variable number of interviews per person was primarily due to the study design, as MCBS enrollees in the last few years of available data had not completed a full 4 years of follow-up. Death was another reason for not having a full follow-up period. Participants could have declined to continue to participate in the MCBS; the data available do not contain this information. Only participants who had a minimum of 2 consecutive interviews were included in this study. Nonresponse rates for variables included in the study were minimal (<2% across all variables), with the amount of missing data noted in tables.
Mobility limitation status of each participant was obtained during the yearly interview. Mobility limitation was defined according to the algorithm developed by Shumway-Cook et al, 18 resulting in 5 limitation categories: none, mild, moderate, severe, and does not walk. The algorithm was developed using the following 4 walking-related questions: “Do you have any difficulty walking?” “Do you have any difficulty walking one fourth of a mile?” “Do you need help from a person to walk?” and “Do you use equipment to walk?” persons who reported no difficulty with walking any distance were categorized as “none” (no limitation). Those who had no difficulty walking, but had difficulty walking 2 to 3 blocks, or reported difficulty walking but did not need help or equipment were categorized as mild limitation. Persons who had difficulty and used equipment, but did not need personal help were categorized as moderate limitation, and those who had difficulty and needed personal help with walking were categorized as having severe limitation. Persons who reported not walking were categorized as “does not walk”.
For each individual, the MCBS files have costs for health care that were paid by Medicare during the calendar year in which the person was enrolled in the survey. MCBS provides data on yearly costs for the following categories of service: inpatient, medical provider, outpatient, prescription medication, dental, facility, and institutional. Because it is not possible to find which of the costs were specifically related to mobility limitations, we used the total cost per year (the summary of all categories), after adjusting for inflation (all data presented are in 2005 dollars). For descriptive analyses and stratification of the sample, we included the following additional variables assessed at each yearly interview: age, sex, education level (less than high school vs high school graduate or higher education), income level (<$25,000 vs ≥$25,000/y), marital status (married vs not married), living status (living alone vs not living alone), living setting (living in the community for part or all of the year vs living in a facility for the entire year), self-reported health status (fair, poor, good, very good, or excellent health), and number of comorbidities (none, 1, 2, 3, or 4 or more of 18 self-reported medical conditions such as high blood pressure and arthritis).
Transition States and Estimation of Transition Probabilities
The 5 mobility limitation categories plus the category “death” constituted the set of all possible states that could be reported in a yearly interview.18 A mobility transition was defined as a set of 2 states: the first representing the person’s mobility state at an interview, and the second representing the mobility state in the subsequent interview (1 year later). In initial analyses, each person could contribute up to 4 transitions, depending on the number of interviews in which the person participated and whether the person died during a certain year. Death is an absorbent state because no further transitions are possible. Transitions could occur in several ways. For example, a participant could report (1) no mobility limitation in one year and mild limitation in the next year (getting worse); (2) moderate limitation in one year and mild in the next year (getting better); (3) moderate limitation in one year and die during the next year in the MCBS (going to the absorbent state and not contributing to any subsequent transitions); or (4) a limitation status that remains the same in both years (no change). The probability of transition from an initial state to another was estimated as the number of observed transitions of that type divided by the total number of transitions in that initial state. In the second set of analyses, only those participants who contributed a minimum of 3 years of data (2 transitions) were included, such that the transition from year 1 to year 2 could be compared with the transition from year 2 to year 3.
Statistical Analysis
Descriptive analyses were performed for all variables in the study. Estimates of the transition probabilities were calculated as described above. Initially, using all transitions from each person, we calculated estimates and presented them in transition probability matrices.20 In addition, to examine group differences in the probability of moving from no mobility limitations to another state, we stratified the estimation of transition probability by sex, education, and income level across age. Those differences are presented graphically. Second, we also looked for patterns over time using 2 transitions (based on 3 interviews). Participants were classified as “no change, ” “worsening, ” and “becoming better” according to their mobility transition from interview 1 to 2, and tables of estimate transition probabilities were created for the transition from interview 2 to 3.The first transition for each individual (from interview 1 to interview 2) was used to estimate the median total cost per individual and to estimate total costs for Medicare.
To assess the possible effect of transitions on costs, we estimated individual total cost by using the Heckman Full Information Maximum Likelihood model.21, 22 This model uses a 2-equation regression framework: one equation to estimate the probability of having any cost, and another equation to estimate the level of cost in the logarithm of dollars (log[cost]) for those people who had any costs. Both equations adjusted for the following explanatory variables: (1) variables constant through the follow-up period (sex, race); (2) variables observed at interview 1 (age, income level, general health, living situation, number of comorbid conditions); and (3) variables that included change between the first and second interview (mobility transitions categorized into 5 groups: no mobility limitation at both times, no change in limitation [same limitation level at both times], worsening [increasing limitation], becoming better [decreasing limitation], and death occurring before the second interview). Setting was included only in the second model because nearly all persons in facilities had some cost, and that variable would not discriminate between having cost or not. To compare the total costs for groups defined by transition type, we used the Duan Smearing estimate, 23 which uses the results from the second equation to back-transform the logarithm of costs into costs in dollars. Means and SDs of the estimated costs for a specific group of persons were then calculated.
Statistical significance level was set to α=.05. PASW 18.0 for Maca and STATA/SE 11.0 for Macb were used for data analysis.
RESULTS
Demographics
A description of the sample can be found in table 1. The majority of the sample was female, white, and married. More than 25% of the sample endorsed having 4 or more comorbid conditions, and about 97% of the sample lived in the community at least for part of the year (vs a facility for the entire year).
Table 1. Baseline Characteristics of the Sample.
| Characteristics | Values |
|---|---|
| Sample size (N) | 41,267 |
| Age (y) | 76.4±7.4 76.0 (65, 113) |
| Sex (% women) | 58.4 |
| Race (% whites) | 87.1 |
| Marital status (% married)* | 51.9 |
| Income (% with $25,000 or less) | 68.4 |
| Education level (% with < high school)† | 38.2 |
| General health (% with fair or poor)‡ | 23.8 |
| Living situation (% living alone) | 31.8 |
| Smoking status (% smoking now)§ | 11.2 |
| Body mass index (kg/m2)∥ | 25.9±4.9 25.4 (10, 66) |
| No, of comorbidities (% in each category) |
|
| 0 | 13.2 |
| 1 | 22.3 |
| 2 | 22.4 |
| 3 | 16.7 |
| ≥4 | 25.4 |
| Setting (% in each category) | |
| Community | 96.7 |
| Facility | 2.3 |
| Both | 1.0 |
| No. of transitions contributed (% in each category) |
|
| 1 | 19.1 |
| 2 | 71.0 |
| 3 | 7.0 |
| 4 | 2.9 |
| Participants who died (n [%]) | |
| During the first year | 2324 (5.6) |
NOTE. Values are mean ± SD, median (minimum, maximum), or as otherwise indicated.
28 missing values.
587 missing values.
117 missing values.
202 missing values.
527 missing values.
Transition Probabilities
Table 2 shows the estimates of transition probabilities using all observed transitions in the data set. Results suggest that most persons who begin with no mobility limitation remain free of mobility limitation over a 1-year transition (estimated probability, .778). For those with mobility limitations in the first year, we observe a considerable proportion of people who remain in the same state or move to adjacent states (better or worse).
Table 2. Transition Probabilities for All Possible Transitions.
| Mobility Limitation at Beginning of Year |
Mobility Limitation at End of Year |
|||||
|---|---|---|---|---|---|---|
| None | Mild | Moderate | Severe | Does Not Walk |
Death | |
| None | .778 | .176 | .019 | .005 | .001 | .020 |
| Mild | .205 | .584 | .102 | .040 | .008 | .061 |
| Moderate | .045 | .211 | .516 | .101 | .025 | .103 |
| Severe | .017 | .129 | .156 | .398 | .090 | .209 |
| Does not walk | .011 | .079 | .085 | .157 | .402 | .265 |
NOTE. Shaded rows correspond to values for remaining in the same state in the second year.
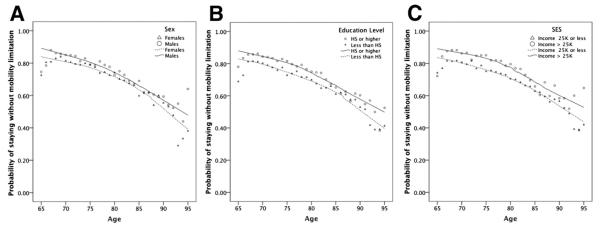
To explore the influence of age, sex, poverty level, and education on the mobility limitations, for the group of people who did not have mobility limitations in the first year, we estimated transition probabilities for the next year by age while stratifying by sex, poverty level, and education. Instead of showing the data in many different tables, we chose to present it graphically after dichotomizing the mobility levels. Figure 1 shows the estimated probabilities of remaining without mobility limitation by sex, level of education, and income level across age. For example, figure 1A shows the estimated probabilities by sex (triangles for women and dots for men). The solid line is a smooth line for the data from men, and the dashed line is for women. Women were generally less likely to remain without mobility limitation compared with men, and the oldest group (85y and older) had the highest probabilities of transition to death. Generally, across all ages, men (see fig 1A), more educated participants (see fig 1B), and those with an annual income of more than $25,000 (see fig 1C) reported remaining without mobility limitation more often than women, less educated participants, and those with a lower income. The discrepancy is larger for education and income level than for sex.
Fig 1.
Probability of remaining in the no-mobility limitation state by age and sex (A), education level (B), and income level (C). Abbreviations: HS, high school; SES, socioeconomic status; 25K, $25,000.
To allow for full exploration of a participant’s multiple transitions over time, we also looked at the data in a longitudinal fashion. From the initial 41,267 participants, 41,199 had information for mobility status in the first and second interviews. From these, 27,228 (66.1%) did not make a transition in status, 6848 (16.6%) made a transition to worse status, 4799 (11.6%) made a transition to a better status, and 2324 (5.6%) died within that year. Table 3 shows the estimated transition probabilities from second to third interviews for 3 groups: (1) participants who had no transition from first to second interview, (2) participants who worsened from first to second interview, and (3) participants who became better from first to second interview. Cells with a thick border represent no mobility transition from second to third interview, whereas cells highlighted in gray represent transitions that continue the pattern observed in the previous transition. For example, a person who did not have a transition from first to second interview and who reported mild limitation at the second interview had a probability of .667 to remain in the mild limitation category, and of .128 to move to the no-limitation category in the third interview. In this group, not having a previous transition would increase the probability of continuing in the same level of limitation in the third interview. For group 2, there was a large probability that a person reported improved mobility limitation in the third interview after reporting deterioration from the first to the second interview. For group 3, there was a large probability of deterioration in mobility status in the third interview after reporting an improvement from the first to the second interview. These results suggest that groups 2 and 3 are more unstable, moving from one level of mobility limitation to another (in either direction) with higher probabilities than group 1. The data in table 3 for groups 2 and 3 suggest that persons with a previous transition are more likely to have a transition in the subsequent year than persons who did not have a transition in the first year of follow-up, showing that the most likely mobility limitation path is not monotonically increasing in severity. There may be some period during which the persons go back and forth between mobility limitation states.
Table 3. Second Transition Comparing Those With No Change, Worsening, or Improvement in First Transition.
| Mobility Limitation at Second-Year Interview | Mobility Limitation Status at Third-Year Interview |
|||||
|---|---|---|---|---|---|---|
| None | Mild | Moderate | Severe | Does Not Walk |
Death | |
| Group 1: No Change in First Transition From First to Second Year |
||||||
| None | .825 | .141 | .014 | .004 | .001 | .015 |
| Mild | .128 | .667 | .103 | .036 | .006 | .060 |
| Moderate | .022 | .144 | .614 | .092 | .027 | .101 |
| Severe | .004 | .068 | .112 | .490 | .105 | .221 |
| Does not walk | .000 | .039 | .047 | .089 | .502 | .323 |
| Group 2: Worsening in First Transition From First to Second Year |
||||||
| Mild | .389 | .487 | .057 | .018 | .004 | .045 |
| Moderate | .088 | .303 | .431 | .064 | .011 | .103 |
| Severe | .029 | .174 | .230 | .323 | .071 | .174 |
| Does not walk | .023 | .120 | .111 | .169 | .329 | .271 |
| Group 3: Becoming Better in First Transition From First to Second Year |
||||||
| None | .502 | .392 | .055 | .013 | .002 | .035 |
| Mild | .060 | .441 | .280 | .109 | .023 | .086 |
| Moderate | .000 | .135 | .446 | .234 | .075 | .111 |
| Severe | .000 | .056 | .065 | .352 | .231 | .296 |
NOTE: Cells with pale gray shading represent no mobility transition from 2nd to 3rd interview; dark gray shaded cells represent transitions that continue the pattern observed in the previous transition.
Cost per Group Defined by Mobility Transitions
Using only data from the first mobility transition of each participant in the MCBS, we calculated the percentage of Medicare beneficiaries who had each type of transition. For each group defined by transition type, we calculated the median cost for persons and the total cost for Medicare for those groups. We show the median values in table 4, with rows highlighted where mobility limitations were reported to be the same in both years. For example, 39.98% of participants reported no mobility limitations in interview 1 and no mobility limitations in interview 2, whereas 9.02% of participants reported no mobility limitations in interview 1 and mild mobility limitations in interview 2. In those groups, the median costs for the year for an individual were $1779 and $2907, respectively. At an individual level, median costs for Medicare beneficiaries increased as levels of mobility limitations in either interview increased, and as one transitioned to worse mobility levels.
Table 4. Total Costs Observed in the Sample for Groups Defined by Mobility Transition From Interview 1 to 2.
| Mobility Limitation at |
Sample Size* (n) |
Percent of Total Sample† |
Median of Individual’s Total Cost‡ ($) |
Estimated Total Cost for Medicare§ ($) |
|
|---|---|---|---|---|---|
| Interview 1 | Interview 2 | ||||
| None | None | 16,500 | 39.98 | 1779 | 25.34 |
|
| |||||
| Mild | 3722 | 9.02 | 2907 | 9.34 | |
| Moderate | 372 | 0.90 | 5153 | 1.65 | |
| Severe | 113 | 0.27 | 7133 | 0.69 | |
| Does not walk |
31 | 0.08 | 10,490 | 0.30 | |
| Dead | 445 | 1.08 | 9724 | 3.74 | |
| Mild | None | 2697 | 6.54 | 2438 | 5.68 |
|
| |||||
| Mild | 7406 | 17.95 | 3289 | 21.04 | |
|
| |||||
| Moderate | 1252 | 3.03 | 5311 | 5.73 | |
| Severe | 508 | 1.23 | 7203 | 3.16 | |
| Does not walk |
121 | 0.29 | 5262 | 0.54 | |
| Dead | 776 | 1.88 | 13,123 | 8.79 | |
| Moderate | None | 206 | 0.50 | 3388 | 0.60 |
| Mild | 956 | 2.32 | 4140 | 3.42 | |
|
| |||||
| Moderate | 2184 | 5.29 | 4325 | 8.15 | |
|
| |||||
| Severe | 450 | 1.09 | 8623 | 3.35 | |
| Does not walk |
108 | 0.26 | 7006 | 0.65 | |
| Dead | 455 | 1.10 | 11,657 | 4.57 | |
| Severe | None | 40 | 0.10 | 4325 | 0.15 |
| Mild | 292 | 0.71 | 5181 | 1.31 | |
| Moderate | 333 | 0.81 | 4943 | 1.43 | |
|
| |||||
| Severe | 836 | 2.03 | 12,971 | 9.38 | |
|
| |||||
| Does not walk |
171 | 0.41 | 17,199 | 2.51 | |
| Dead | 455 | 1.10 | 10,828 | 4.24 | |
| Does not walk |
None | 9 | 0.02 | 3374 | 0.02 |
| Mild | 66 | 0.16 | 4241 | 0.24 | |
| Moderate | 67 | 0.16 | 5725 | 0.33 | |
| Severe | 133 | 0.32 | 16,700 | 1.90 | |
|
| |||||
| Does not walk |
302 | 0.73 | 13,044 | 3.39 | |
|
| |||||
| Dead | 193 | 0.47 | 9950 | 1.67 | |
NOTE. Shaded rows correspond to no change in mobility status from interview 1 to 2.
Sample size on which median cost was calculated.
Percent of entire sample (41,199 observations).
Median cost of participants within the specific cell (in dollars adjusted for 2005 value).
Estimated total cost (in billions of dollars adjusted for 2005 value) for Medicare based on population size of 35.63 million beneficiaries in 2005 (each cell is 35.63 × percent of total sample × median total cost).
The median total cost for Medicare was estimated for each of the groups defined by transitions from interview 1 to 2 (see table 4, last column). We used the total population of 35,633,683 Medicare beneficiaries 65 years and older for 2005 as the basis for the total cost estimated for Medicare. For example, 39.98% of 35.6 million represents 14.25 million of that population who remained without mobility limitation, with an estimated total cost of more than $25 billion (14.25 million × $1779). Overall, approximately $25 billion was estimated to be spent on persons with no mobility limitation, $42 billion on persons with stable (no change) levels of mobility limitation, $28 billion on those who worsened, $15 billion on those who improved, and $23 billion on those who died.
Estimated Total Cost by Mobility Group
We sought to explain the cost based on characteristics of the individual, including age, sex, race, socioeconomic status, general health, living situation (alone vs not alone), comorbidities, and transition state. Using the 2-part model, we estimated the cost for each individual in the sample, and averaged those costs for persons within the same mobility transition group (no limitations, no change in limitations, worsening, becoming better, and death). The average and SD of those estimates are shown in table 5. Results show that transition to death in a given year has the highest average cost and variation within the group (as measured by the SD), followed by worsening of disability status. Persons with no mobility limitations had the lowest average cost and least variation.
Table 5. Estimated Cost of First Transition Including Individual Characteristics by Type of Mobility Transition.
| Transition | Type Cost* ($) |
|---|---|
| No limitation | 4231±2073 |
| No change in limitation | 9580±6445 |
| Worsening | 10,292±6578 |
| Becoming better | 7731±4645 |
| Death | 25,923±22,239 |
NOTE. Values are mean ± SD.
Estimates of cost from 2-part model controlling for age, sex, race, socioeconomic status, general health, living situation, comorbidities, and transition state.
DISCUSSION
Our findings reveal several interesting facts about adults in the United States, 65 years and older, who have mobility limitations. First, there is a great deal of stability and improvement in mobility. For any given initial mobility state, most respondents were most likely to either remain in the same state in the next year or actually improve. This fact even holds true when we examine the third year transitions for those whose mobility worsened between years 1 and 2, highlighting the dynamic nature of disability. Second, the probability of mobility disability transitions differs based on sex, education, and household income. At all age groups, women, those with less education, and those with less income were more likely to transition from no mobility limitation to some level of limitation.
Mobility transitions are also associated with significant health care costs. In our cohort, more than $133 billion in medical expenditures were recorded. Not surprisingly, per capita, the least expensive “transition” was from no limitation to no limitation. Although 40% of the entire cohort placed in this category, they only accounted for 19% of the total costs. In general, costs were lower for those who ended up with mild or moderate limitations, regardless of where they started. Those who ended up with severe limitations or who died had up to 10 times the costs of those with no mobility limitations. Fifty percent of the costs were borne by those who did not alter their status from one year to the next, 21% of costs were for those who got worse, 11% for those who got better, and 17% for those who died. Estimated costs based on individual characteristics provided additional support for the conclusion that highest costs are associated with worsening of disability and death.
Our results have certain policy implications. As the United States considers ways to reform its health care delivery system, our findings suggest 2 truths about disability. First, mobility limitation is an important predictor of health care costs even after controlling for many other patient characteristics. Thus it should be considered an essential factor when trying to design incentives for providers or estimate capitated payments. New health care delivery initiatives, such as the medical home, need to account for mobility limitations in their models or risk the creation of a selection bias against persons with disabilities. Second, mobility limitations may be reversible, but this comes at a cost. In our cohort, Medicare spent more than 7% ($9.4 billion) of its costs on those whose mobility improved. However, the costs of disability progression are high as well. If all the costs in our study could be attributable to mobility limitations, results show that Medicare could pay for approximately 10 adults for a year who do not have mobility limitations with the money it costs to pay for 1 adult who transitions to severe limitation. This suggests that prevention and reversing disability may be most cost-effective over time. We do realize that health care costs are complex and are not only generated by mobility limitations, but also other health conditions. However, comorbid health conditions can often lead to mobility limitations or develop secondarily as a result of mobility limitations. Even under these circumstances, a focus on prevention would be beneficial. In this study, we examined only costs that occurred during the transition. We recognize that a full analysis of costs, including those from the prior year, is important, but is beyond the scope of the current article.
Study Limitations
Our study has limitations. Our definition of mobility limitation was based on self-report and not on objective measures. Although this methodology is widely used in epidemiologic studies, the possibility exists that it could have biased our results if there were differential rates of inaccuracies between the persons in different mobility states. Second, we do not know exactly when a disability transition occurred, only that it happened at some point in the year before the person’s interview. This made it impossible to be precise about allocating specific costs to specific mobility transitions. The MCBS does not contain specific information to calculate a case mix. However, in the 2-part model, we included important patient characteristics (such as age and comorbidities) that have been shown to be important in explaining transitions. Finally, because MCBS only measured mobility limitation status once a year, transitions may have occurred in between our 2 measurements that are unaccounted for.
CONCLUSIONS
Our study has documented, for the first time, factors associated with mobility limitation transitions. Women, persons with less education, and those with less income are at risk for worse transitions after adjusting for other variables (including age). We have shown that substantial numbers of adults improve and that mobility limitation, an important predictor of health care costs, should play a role in health care reform both in designing payment systems and in ensuring against potential bias against persons with disability.
Acknowledgments
Supported by the National Institutes of Health Intramural Research Program.
List of Abbreviations
- MCBS
Medicare Current Beneficiary Survey
Footnotes
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the National Institutes of Health.
No commercial party having a direct financial interest in the results of the research supporting this article has or will confer a benefit on the authors or on any organization with which the authors are associated.
References
- 1.Choi N, Schlichting-Ray L. Predictors of transitions in disease and disability in pre- and early-retirement populations. J Aging Health. 2001;13:379–409. doi: 10.1177/089826430101300304. [DOI] [PubMed] [Google Scholar]
- 2.Gill T, Allore H, Hardy S, Guo Z. The dynamic nature of mobility disability in older persons. J Am Geriatr Soc. 2006;54:248–54. doi: 10.1111/j.1532-5415.2005.00586.x. [DOI] [PubMed] [Google Scholar]
- 3.Gill T, Gahbauer E, Allore H, Han L. Transitions between frailty states among community-living older persons. Arch Intern Med. 2006;166:418–23. doi: 10.1001/archinte.166.4.418. [DOI] [PubMed] [Google Scholar]
- 4.Masala C, Petretto D. From disablement to enablement: conceptual models of disability in the 20th century. Disabil Rehabil. 2008;30:1233–44. doi: 10.1080/09638280701602418. [DOI] [PubMed] [Google Scholar]
- 5.Chan L, Doctor J, MacLehose R, et al. Do Medicare patients with disabilities receive preventive services? A population-based study. Arch Phys Med Rehabil. 1999;80:642–6. doi: 10.1016/s0003-9993(99)90166-1. [DOI] [PubMed] [Google Scholar]
- 6.Chan L, Beaver S, Maclehose R, Jha A, Maciejewski M, Doctor J. Disability and health care costs in the Medicare population. Arch Phys Med Rehabil. 2002;83:1196–201. doi: 10.1053/apmr.2002.34811. [DOI] [PubMed] [Google Scholar]
- 7.Jha A, Patrick D, MacLehose R, Doctor J, Chan L. Dissatisfaction with medical services among Medicare beneficiaries with disabilities. Arch Phys Med Rehabil. 2002;83:1335–41. doi: 10.1053/apmr.2002.33986. [DOI] [PubMed] [Google Scholar]
- 8.Bryant L, Shetterly S, Baxter J, Hamman R. Changing functional status in a biethnic rural population: the San Luis Valley Health and Aging Study. Am J Epidemiol. 2002;155:361–7. doi: 10.1093/aje/155.4.361. [DOI] [PubMed] [Google Scholar]
- 9.Mor V, Wilcox V, Rakowski W, Hiris J. Functional transitions among the elderly: patterns, predictors, and related hospital use. Am J Public Health. 1994;84:1274–80. doi: 10.2105/ajph.84.8.1274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hardy S, Allore H, Guo Z, Gill T. Explaining the effect of gender on functional transitions in older persons. Gerontology. 2008;54:79–86. doi: 10.1159/000115004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Diehr P, Patrick D. Probabilities of transition among health states for older adults. Qual Life Res. 2001;10:431–42. doi: 10.1023/a:1012566130639. [DOI] [PubMed] [Google Scholar]
- 12.Wolf D, Mendes de Leon C, Glass T. Trends in rates of onset of and recovery from disability at older ages: 1982-1994. J Gerontol B Psychol Sci Soc Sci. 2007;62:S3–S10. doi: 10.1093/geronb/62.1.s3. [DOI] [PubMed] [Google Scholar]
- 13.Hill S, Pylypchuk Y. Reports of fewer activity limitations: recovery, survey fatigue, or switching respondent? Med Care. 2006;44(5 Suppl):I73–81. doi: 10.1097/01.mlr.0000208199.13219.8b. [DOI] [PubMed] [Google Scholar]
- 14.Verbrugge L. Disability transitions for older persons with arthritis. J Aging Health. 1992;4:212–43. [Google Scholar]
- 15.Stuck A, Walthert J, Nikolaus T, Büla C, Hohmann C, Beck J. Risk factors for functional status decline in community-living elderly people: a systematic literature review. Soc Sci Med. 1999;48:445–69. doi: 10.1016/s0277-9536(98)00370-0. [DOI] [PubMed] [Google Scholar]
- 16.Iezzoni L, McCarthy E, Davis R, Siebens H. Mobility problems and perceptions of disability by self-respondents and proxy respondents. Med Care. 2000;38:1051–7. doi: 10.1097/00005650-200010000-00009. [DOI] [PubMed] [Google Scholar]
- 17.Hoffman J, Shumway-Cook A, Yorkston K, Ciol M, Dudgeon B, Chan L. Association of mobility limitations with health care satisfaction and use of preventive care: a survey of Medicare beneficiaries. Arch Phys Med Rehabil. 2007;88:583–8. doi: 10.1016/j.apmr.2007.02.005. [DOI] [PubMed] [Google Scholar]
- 18.Shumway-Cook A, Ciol MA, Yorkston KM, Hoffman JM, Chan L. Mobility limitations in the Medicare population: prevalence and sociodemographic and clinical correlates. J Am Geriatr Soc. 2005;53:1217–21. doi: 10.1111/j.1532-5415.2005.53372.x. [DOI] [PubMed] [Google Scholar]
- 19.Medicare Current Beneficiary Survey (MCBS) [Accessed February 15, 2010]; Available at: http://www.cms.hhs.gov/MCBS/
- 20.Karlin S, Taylor HM. A first course in stochastic processes. 2nd ed Academic Pr; New York: 1975. [Google Scholar]
- 21.Manning W, Duan N, Rogers W. Monte-Carlo evidence on the choice between sample selection and 2-part models. J Econom. 1987;35:59–82. [Google Scholar]
- 22.Madden D. Sample selection versus two-part models revisited: the case of female smoking and drinking. J Health Econ. 2008;27:300–7. doi: 10.1016/j.jhealeco.2007.07.001. [DOI] [PubMed] [Google Scholar]
- 23.Duan N. Smearing estimate—a nonparametric retransformation method. J Am Stat Assoc. 1983;78(383):605–10. [Google Scholar]
Suppliers
- a.PASW 18.0 for Mac, IBM Corp, Route 100, Somers, NY 10589.
- b.STATA/SE 11.0 for Mac, 4905 Lakeway Dr, College Station, TX 77845.