Abstract
Background
We performed a systematic review and meta-analysis to determine the effect of suction with water seal, compared with water seal alone, applied to intrapleural chest tubes on the duration of air leaks in patients undergoing pulmonary surgery.
Methods
We searched MEDLINE, EMBASE and the Cochrane Central Register of Controlled Trials to find randomized controlled trials (RCTs) comparing the effect of the 2 methods on the duration of air leaks. Trials were systematically assessed for eligibility and validity. Data were extracted in duplicate and pooled across studies using a random-effects model.
Results
The search yielded 7 RCTs that met the eligibility criteria. No difference was identified between the 2 methods in duration of air leak (weighted mean difference [WMD] 1.15 days, favours water seal; 95% confidence interval [CI] −0.64 to 2.94), time to discharge (WMD 2.19 d, favours water seal; 95% CI −0.63 to 5.01), duration of chest tubes (WMD 0.96 d, favours water seal; 95% CI −0.12 to 2.05) or incidence of prolonged air leaks (absolute risk reduction [ARR] 0.04, favours water seal; 95% CI −0.01 to 0.09). Water seal was associated with a significantly increased incidence of postoperative pneumothorax (ARR −0.14, 95% CI −0.21 to −0.07).
Conclusion
No differences were identified in terms of duration of air leak, incidence of prolonged air leak, duration of chest tubes and duration of hospital stay when chest tubes were placed to suction rather than water seal. Chest tube suction appears to be superior to water seal in reducing the incidence of pneumothorax; however, the clinical significance of this finding is unclear.
Abstract
Contexte
Nous avons procédé à une revue systématique et à une méta-analyse dans le but de comparer l’effet de 2 méthodes de drainage thoracique intrapleural (la première, scellée sous eau avec succion et l'autre, scellée sous eau, mais sans succion) sur la durée des fuites d’air chez les patients soumis à une chirurgie pulmonaire.
Méthodes
Nous avons interrogé les bases de données MEDLINE, EMBASE et le registre central Cochrane des essais randomisés et contrôlés (ERC) pour recenser les ERC ayant comparé l’effet des 2 méthodes sur la durée des fuites d’air. Nous avons évalué de manière systématique l'admissibilité et la validité des ERC. Nous avons extrait en double les données des essais retenus et nous les avons regroupées selon un modèle à effets aléatoires.
Résultats
L'interrogation a permis de recenser 7 ERC qui répondaient aux critères d’admissibilité. Nous n’avons observé aucune différence entre les 2 méthodes quant à la durée des fuites d’air (différence moyenne pondérée [DMP] 1,15 j, favorisant le système scellé sous eau; intervalle de confiance [IC] à 95 % −0,64 à 2,94), durée du séjour hospitalier (DMP 2,19 j, favorisant le système scellé sous eau; IC à 95 % 0,63 à 5,01), la durée du drainage thoracique (DMP 0,96 j, favorisant le système scellé sous eau; IC à 95 % 0,12 à 2,05) ou l'incidence des fuites d’air prolongées (réduction du risque absolu [RRA] 0,04, favorisant le système scellé sous eau; IC à 95 % 0,01 à 0,09). Le système scellé sous eau a été associé à une augmentation significative de l’incidence des pneumothorax postopératoires (RRA 0,14, IC à 95 % 0,21 à 0,07).
Conclusion
Nous n’avons noté aucune différence sur le plan de la durée des fuites d’air, de l’incidence des fuites d’air prolongées, de la durée du drainage thoracique et de la durée du séjour hospitalier lorsque les drains thoraciques étaient placés sous succion plutôt que simplement scellés sous eau. Les drains thoraciques sous succion semblent supérieurs aux drains thoraciques scellés sous eau pour ce qui est de réduire l’incidence du pneumothorax. Toutefois, la portée clinique de cette observation reste à déterminer.
Chest tubes are placed postoperatively in patients undergoing thoracic surgery to prevent pneumothorax and to monitor for air leak and hemothoraces. Air leaks from resection margins are a common complication.1 Persistent air leaks can result in prolonged hospital stay and complications, such as empyema,2 in patients undergoing lung resection. Many surgeons keep chest tubes to −20 cm H2O suction postoperatively, whereas some use water seal to minimize the duration of postoperative air leaks. Placing the chest tube to suction has a theoretical advantage of improving apposition of the pleura to the chest wall; however, this negative intrathoracic pressure may also serve to maintain the flow of air through an alveolar pleural fistula, resulting in its persistence.2
A descriptive review,3 and more recently a systematic review,4 on this topic were published. The systematic review by Deng and colleagues,4 however, had some limitations. Its search was limited to MEDLINE, and only 1 reviewer selected studies for full assessment. Furthermore, no subgroup analysis was performed to explain heterogeneity among studies. We therefore felt it was worthwhile repeating this systematic review and meta-analysis with more rigorous methodology.
Methods
Study selection
We searched MEDLINE, EMBASE and the Cochrane Central Register of Controlled Trials for potentially relevant randomized controlled trials (RCTs) using the medical subject headings “pulmonary surgical procedures” and “respiratory tract fistula” as search terms. We then searched using the following keywords: “lobectomy,” “segmentectomy,” “lung resection,” “wedge resection,” “air leak” and “alveolar fistula.” Our search included foreign language publications. We reviewed the reference lists of all articles obtained as well as bibliographies of 2 major textbooks in thoracic surgery5,6 to identify any other missed articles. To uncover unpublished but potentially relevant trials, we searched 2 indices of conference proceedings (proceedingsfirst, papersfirst) and the database of registered trials at www.clinicaltrials.gov. Two reviewers assessed all articles obtained to determine whether they met our inclusion criteria. To be included, a study must have been an RCT comparing intrapleural chest tubes placed to suction versus water seal following pulmonary surgery. Outcomes of interest were duration of air leak, incicidence of prolonged air leak, duration of chest tubes, postoperative complications and length of hospital stay.
Agreement between reviewers was measured using the κ statistic. Any disagreements between reviewers were discussed and resolved by consensus when possible. A third reviewer adjudicated if consensus could not be obtained.
Validity assessment
Two independent reviewers assessed each eligible study to determine the risk of bias for each outcome. Six criteria were evaluated for each study. These were sequence generation, allocation concealment, blinding of outcome assessors, incomplete outcome data, selective outcome reporting and other sources of bias. For each criterion, each reviewer judged whether it was adequately addressed in the study based on the criteria for judging risk of bias in the Cochrane handbook’s “risk of bias” assessment tool.7 An overall assessment for risk of bias for each study was then made. Low risk of bias required that all categories of the risk of bias tool be adequately addressed. High risk of bias was assigned to any study with at least 1 category that was inadequately addressed. An unclear risk of bias was assigned to any study with at least 1 category assigned as unclear and no inadequately addressed categories.
Data extraction
Two investigators collected relevant information in duplicate regarding the population, intervention and outcomes from each selected article using standardized data extraction forms. When any of this information was missing from a study, an attempt was made to contact the authors to obtain these data.
Statistical analysis
We began the analysis with a visual inverted funnel plot of each study outcome with data from 5 or more trials, comparing the magnitude of the relative risk (including confidence intervals [CIs]) against the log standard error.8 An inverted, funnel-shaped, symmetric appearance suggests that no study has been left out, whereas an asymmetric appearance suggests the presence of publication or other systematic bias.
Data across studies were pooled using a random-effects model9 to calculate absolute risk reduction (ARR) for dichotomous outcomes and weighted mean differences (WMDs) for continuous outcomes. As part of our sensitivity analysis, data were also analyzed using a fixed-effects model. We tested homogeneity of the estimates using the Breslow–Day test with a significance threshold of p < 0.110 and the I2,11 which estimates the proportion of total variability that is owing to true between-study differences rather than chance alone. We explored heterogeneity (I2 > 0) with subgroup and sensitivity analyses based on predetermined hypotheses. Hypothesized sources of heterogeneity were length of time used to define prolonged air leak, presence of suction before random assignment of patients, indication for surgery and type of lung resection.
We conducted all analyses using Revman version 5. This paper adheres to the guidelines for reporting of systematic reviews proposed by the QUORUM Group.12
Results
Characteristics of included studies
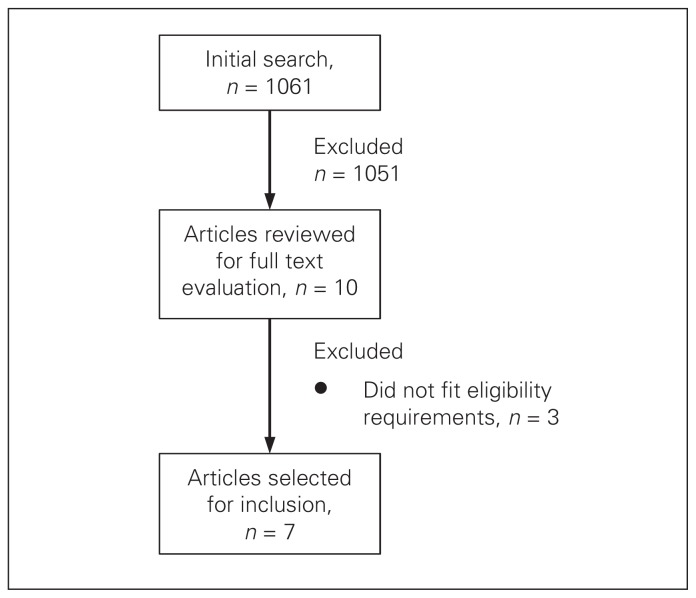
Our initial search yielded 1061 citations (Fig. 1). Of these, 1051 were excluded because they did not meet our eligibility criteria. This left 10 articles for full text evaluation. Three of these did not meet eligibility criteria, and 7 RCTs were ultimately included in our analysis (Table 1). All of the included studies were published in English. Reviewers achieved perfect agreement in the application of eligibility criteria (κ = 1).
Fig. 1.
Selection of randomized controlled trials comparing the effect of suction with water seal versus water seal alone on the duration of air leaks for inclusion in our systematic review and meta-analysis.
Table 1.
Characteristics of randomized controlled trials comparing the effect of suction with water seal versus water seal alone included in our systematic review and meta-analysis
| Study | Sample size | Eligibility criteria | Intervention | Outcomes |
|---|---|---|---|---|
| Alphonso et al.13 | 254 |
|
−20 cm suction v. water seal |
|
| Ayed14 | 100 |
|
−20 cm suction v. water seal |
|
| Brunelli et al.15 | 145 |
|
−20 cm suction v. water seal, random assignment of patients on POD 1 |
|
| Cerfolio et al.1 | 140 |
|
−20 cm suction v. water seal, random assignment of patients on POD 2 |
|
| Daneshvar et al.16 | 31 |
|
−10 to −18 cm suction v. water seal, random assignment of patients on POD 1 |
|
| Marshall et al.2 | 68 |
|
−20 cm suction v. water seal, random assignment of patients in recovery room |
|
| Prokakis et al.17 | 91 |
|
−15 to −20 cm suction v. water seal |
|
POD = postoperative day; VATS = video-assisted thoracic surgery.
All included studies were published between 2001 and 2008. Sample sizes ranged from 31 to 254 patients. Most studies included patients undergoing lung resections for lung cancer. One study included only patients with spontaneous pneumothorax.14 Six studies used −20 cm of water for the strength of intrapleural suction, whereas 1 used between −10 and −18 cm of suction.16 Four of the studies included a period of intrapleural suction postoperatively to expand the lung before random assignment of patients. These times ranged from the time required for patient transport to the recovery room to postoperative day 2.
All of the included papers used the incidence of prolonged air leak as one of the study outcomes. The definition of prolonged air leak, however, differed among studies. This varied from as little as 3 days in 1 paper, to more than 7 days in 3 papers.
The risk of bias was deemed unclear in 6 studies, whereas 1 study was deemed to have a high risk for bias owing to incomplete outcome data (Table 2). In all of the studies, there was blinding of surgeons; however, blinding of outcome assessors in each study was not reported. Reporting was generally poor in terms of concealment of allocation and sequence generation. Only 2 studies adequately described their method of random assignment. Three studies were deemed to be free of selective reporting, as they provided outcome data for all relevant patient outcomes addressed in this study, whereas the remaining 4 did not. The κ value for interobserver agreement for validity assessment was 0.70. All of the funnel plots demonstrated relative symmetry.
Table 2.
Risk of bias assessment
| Study | Concealment of allocation | Adequate sequence generation | Blinding of outcome assessors | Incomplete outcome data addressed | Free of selective reporting | Free of other bias | Overall risk of bias in study |
|---|---|---|---|---|---|---|---|
| Alphonso et al.13 | Yes | Yes | Unclear | No | Unclear | Yes | High |
| Ayed14 | Unclear | Unclear | Unclear | Yes | Yes | Yes | Unclear |
| Brunelli et al.15 | Unclear | Unclear | Unclear | Yes | Yes | Yes | Unclear |
| Cerfolio et al.1 | Unclear | Unclear | Unclear | Yes | Unclear | Yes | Unclear |
| Daneshvar et al.16 | Unclear | Unclear | Unclear | Yes | Unclear | Yes | Unclear |
| Marshall et al.2 | Unclear | Unclear | Unclear | Yes | Unclear | Yes | Unclear |
| Prokakis et al.17 | Unclear | Yes | Unclear | Yes | Yes | Yes | Unclear |
κ = 0.70.
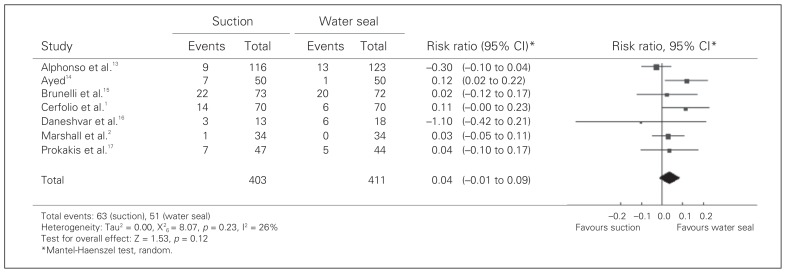
Duration of air leak
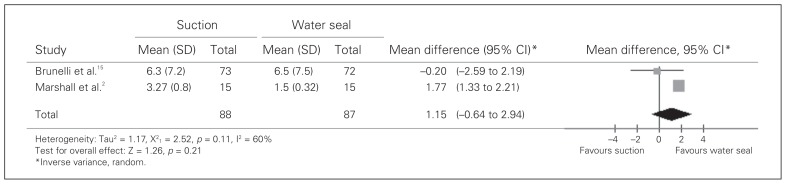
All 7 of the studies included incidence of prolonged air leak as an outcome (Fig. 2). There was a nonsignificant trend toward a decreased incidence of prolonged air leak in the water seal group (ARR 0.04, 95% CI −0.01 to 0.09). Only 2 of the 7 studies specifically included the duration of air leaks in their analysis. There was no statistical difference between suction and water seal identified (WMD 1.15 d, 95% CI −0.64 to 2.94; Fig. 3). Both of these studies reported the duration of air leak adjusted for the length of the staple line. When this adjustment was made, there was a statistically significant improvement in the duration of air leak in favour of water seal (0.07 d/cm, 95% CI 0.01–0.13). There was a trend toward decreased duration of chest tubes in the water seal group (WMD 0.96 d, 95% CI −0.12 to 2.05); however, this was not statistically significant. There was no significant difference in terms of length of hospital stay (WMD 2.19 d, 95% CI −0.63 to 5.01) despite a trend toward a shorter stay in the water seal group.
Fig. 2.
Incidence of prolonged air leak. CI = confidence interval.
Fig. 3.
Duration of air leak (days). CI = confidence interval.
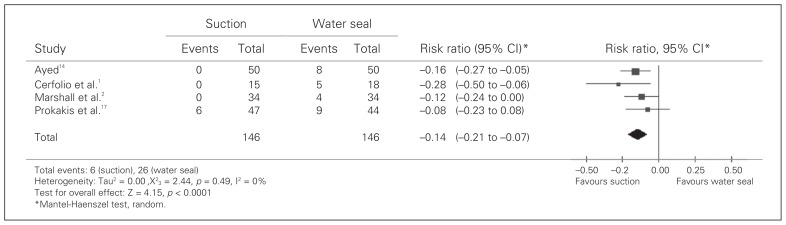
Complications
Four studies compared the incidence of postoperative pneumothorax. There was a significantly increased incidence in the water seal group (ARR −0.14, 95% CI −0.21 to −0.07; Fig. 4). For other complications, such as pneumonia (ARR −0.03, 95% CI −0.12 to 0.06), arrhythmia (ARR −0.04, 95% CI −0.15 to 0.08) and death (ARR −0.01, 95% CI −0.04 to 0.03), there were no differences identified between the suction and water seal groups.
Fig. 4.
Incidence of pneumothorax. CI = confidence interval.
Subgroup analysis
All of the above outcome measures, apart from death and the incidence of pneumothorax, demonstrated significant heterogeneity (I2 > 0). Subgroup analysis was performed in an attempt to eliminate both clinical and statistical heterogeneity. First, for the incidence of prolonged air leak, subgroup analysis was performed based on the definition of prolonged air leak. When only studies that defined this as greater than or equal to 6 days were used, heterogeneity was eliminated (I2 = 0). This also eliminated any trend in treatment effect for this outcome (ARR 0.00, 95% CI −0.05 to 0.05). Subgroup analysis based on the indication for lung resection (including only papers whose inclusion criteria was cancer) eliminated heterogeneity in the incidence of prolonged air leak but did not alter the failure to achieve statistical significance in the result (ARR 0.02, 95% CI −0.02 to 0.06). This analysis did not eliminate the statistical heterogeneity in any other outcomes. Our other hypothesized sources for heterogeneity did not reduce heterogeneity in any outcomes.
Sensitivity analysis
Sensitivity analysis was performed by reanalyzing the data using a fixed-effects model and by removing outlier studies. A fixed-effects model caused the time to discharge (WMD 1.76 d, 95% CI 1.20–2.32) and duration of air leak (WMD 1.71 d, 95% CI 1.28–2.14) to become significant in favour of water seal. For the time to discharge, there was 1 outlier study that was strongly in favour of water seal.2 A post hoc analysis removing this study caused this outcome to become significant in favour of water seal (WMD 1.02, 95% CI 0.41–1.62). This occurred as the CI for this outcome become much narrower following removal of this study. Removal of this study from the analysis also eliminated any statistical heterogeneity. There were no obvious methodological issues in this study that would explain why its results were so different from those of other studies in this group. As this analysis was performed post hoc, its results should be interpreted with caution.
Discussion
Intrapleural chest tubes are routinely placed following pulmonary surgery. Furthermore, postoperative air leaks are a common complication following lung resections. This systematic review was performed to determine if chest tubes placed to suction compared with water seal alone resulted in decreased duration of postoperative air leaks. We found no difference between suction and water seal alone in terms of duration of air leak, incidence of prolonged air leak, duration of chest tubes and duration of hospital stay. Placing chest tubes to suction was, however, superior with respect to the incidence of pneumothorax. The ARR of pneumothorax found in this meta-analysis translates into a number needed to treat of 7.14. This means that roughly 7 patients would need to be managed with suction to prevent 1 pneumothorax. Despite this significant improvement in the incidence of pneumothorax, suction did not decrease length of hospital stay or duration of chest tubes. This suggests that the pneumothoraces seen in the water seal group were not clinically important enough to affect these outcomes. This makes clinical sense given that these patients had chest tubes in place, which would make management of pneumothorax fairly simple. Subgroup analysis suggested that statistical heterogeneity could be partially explained by the definition of prolonged air leak used in various studies. When only those studies defining it as more than 6 days were included, heterogeneity was eliminated. No difference between the 2 groups in this analysis was identified.
We analyzed our data with a random-effects model and then later with a fixed-effects model as part of our sensitivity analysis. A fixed-effects model assumes that every study in the analysis is measuring the same treatment effect. The assumption is therefore made that if every study in the analysis were infinitely large, they would all have the same result. A random-effects model, on the other hand, assumes that there are differences in each study, such as differences in study design or patient population, that result in true differences in treatment effect.7 The random-effects model may perform better when there is statistical heterogeneity among studies, as was the case in our meta-analysis. Furthermore, the results using a random-effects model were more conservative than those using a fixed-effects model. For these reasons, the results using a random-effects model were favoured in this review.
A previous review examining chest tube suction following pulmonary surgery was performed by Sanni and colleagues;3 however, no meta-analysis was performed. This review included 5 RCTs, all of which were included in our paper. The authors concluded that water seal alone was a reasonable approach to managing postoperative air leaks, with the possible exception of large air leaks or in the presence of a large pneumothorax. The papers included in our study did not generally report data regarding the size of air leaks or pneumothoraces. We were therefore unable to perform any analysis regarding these possible subgroups.
Another systematic review on this topic has also been published.4 There are some notable differences between the present study and that review. The review by Deng and colleagues4 included only 6 trials. This is because they used a much more limited search strategy, including only studies from MEDLINE. Despite the inclusion of 1 extra study by Daneshvar,16 the results of this review and that by Deng had similar results. The 2 reviews differed significantly in the assessment of study quality. Deng and colleagues used the Jadad scoring system to assess quality and concluded that the studies were generally of high quality. The Cochrane handbook, however, specifically recommends avoiding the Jadad scale owing to its “strong emphasis on reporting rather than conduct” and its failure to address concealment of allocation.7 In the present review, a risk of bias assessment was performed based on the presence of adequate randomized sequence generation, blinding of outcome assessors, concealment of allocation, the presence of incomplete outcome data, selective outcome reporting and other sources of bias. We concluded that the overall risk of bias was unclear in 6 of the studies and high in 1. Although blinding of outcome assessors in these studies would be technically challenging, the lack of blinding does allow for the potential introduction of bias in any of the subjective outcomes addressed in these studies. The methods used in our review to assess risk of bias were in keeping with the recommendations of the Cochrane collaboration.7
Limitations
Strengths of our study include the systematic and explicit application of eligibility criteria, the careful consideration of study quality, the generation and testing of a priori hypotheses to explain heterogeneity, the standardized data extraction and the rigorous analytical approach. One weakness of this review is the heterogeneity found among studies. Subgroup analysis was performed based on our a priori hypothesis of possible sources of heterogeneity in an attempt to reduce it. The heterogeneity in the incidence of prolonged air leak and length of hospital stay could be explained and eliminated through subgroup and sensitivity analysis; however, this was not the case for any other outcomes. This review was also limited by incomplete reporting of methodology. For most of the studies concealment of allocation, patient blinding and outcome assessor blinding were not reported. This leaves the possibility of bias affecting the results of the studies.
The GRADE system was used to rate the overall quality of evidence. Using this system, RCTs are rated as high-quality evidence unless they have serious limitations in study quality, important inconsistency, uncertainty about directness, imprecise or sparse data or high probability of reporting bias.18,19 The data quality of the studies included in our review ranged from very low, as seen in the duration of air leak, incidence of arrhythmia and incidence of pneumonia, to moderate quality, as seen with the incidence of pneumothorax (Table 3). Very low-quality evidence suggests that we are very uncertain about the treatment effect estimates, whereas low-quality evidence indicates that further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate.20 Moderate quality evidence suggests that further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. The quality was limited in most outcomes by potentially high or unclear risk of bias in included studies and by inconsistency owing to substantial heterogeneity among studies. For the duration of air leak and the incidence of pneumonia, the data were limited both by inconsistent and by sparse data, resulting in low-quality evidence.
Table 3.
GRADE evidence summarizing the effectiveness of chest tubes placed to suction or water seal: positive values favour water seal, negative values favour suction
| Outcome | No. studies | No. participants | Results (95% CI) | Quality of the evidence |
|---|---|---|---|---|
| Duration of air leak, d | 2 | 175 | WMD 1.15 (−0.64 to 2.94) | Very low*†‡ |
| Duration of air leak/length of staple line, d/cm | 2 | 175 | WMD 0.07 (0.01 to 0.13)§ | Very low*†‡ |
| Incidence of prolonged air leak | 7 | 814 | ARR 0.04 (−0.01 to 0.09) | Low*‡ |
| Duration of chest tube, d | 4 | 404 | WMD 0.96 (−0.12 to 2.05) | Low*‡ |
| Duration of hospital stay, d | 4 | 404 | WMD 2.19 (−0.63 to 5.01) | Low*‡ |
| Incidence of pneumothorax | 4 | 292 | ARR −0.14 (−0.21 to −0.07)§ | Moderate‡ |
| Incidence of arrhythmia | 2 | 236 | ARR −0.04 (−0.15 to 0.08) | Very low*†‡ |
| Incidence of death | 2 | 191 | ARR −0.01 (−0.04 to 0.03) | Low†‡ |
| Incidence of pneumonia | 2 | 236 | ARR −0.03 (−0.12 to 0.06) | Very low*†‡ |
ARR = absolute risk reduction; CI = confidence interval; WMD = weighted mean difference.
Evidence limited by heterogeneity between studies.
Evidence limited by imprecise data (small sample size or event rate).
Evidence limited by high or unclear risk of bias in studies.
Statistically significant.
Conclusion
No differences were identified in terms of duration of air leak, incidence of prolonged air leak, duration of chest tubes and length of hospital stay when chest tubes were placed to suction rather than water seal. The quality of evidence for these outcomes was low or very low. There is moderate-quality evidence that chest tube suction is superior to water seal in the incidence of pneumothorax; however, the clinical significance of this finding is unclear. Based on the results of this analysis, we are unable to make any recommendations for the management of chest tubes following pulmonary resection. A future large, well-designed RCT would therefore be useful in addressing this clinical issue.
Footnotes
Competing interests: None declared.
Contributors: S.M. Coughlin and R. Malthaner designed the study. S.M. Coughlin and H.M.A. Emmerton-Coughlin acquired the data. S.M. Coughlin wrote the article. All authors analyzed the data, reviewed the article and approved its publication.
References
- 1.Cerfolio RJ, Bass C, Katholi CR. Prospective randomized trial compares suction versus water seal for air leaks. Ann Thorac Surg. 2001;71:1613–7. doi: 10.1016/s0003-4975(01)02474-2. [DOI] [PubMed] [Google Scholar]
- 2.Marshall MB, Deeb ME, Bleier JI, et al. Suction vs water seal after pulmonary resection: a randomized prospective study. Chest. 2002;121:831–5. doi: 10.1378/chest.121.3.831. [DOI] [PubMed] [Google Scholar]
- 3.Sanni A, Critchley A, Dunning J. Should chest drains be put on suction or not following pulmonary lobectomy? Interact Cardiovasc Thorac Surg. 2006;5:275–8. doi: 10.1510/icvts.2006.130559. [DOI] [PubMed] [Google Scholar]
- 4.Deng B, Tan QY, Zhao YP, et al. Suction or non-suction to the under-water seal drains following pulmonary operation: meta-analysis of randomized controlled trials. Eur J Cardiothorac Surg. 2010;38:210–5. doi: 10.1016/j.ejcts.2010.01.050. [DOI] [PubMed] [Google Scholar]
- 5.Shields TW, Iocicero R, Ponn RB, et al. General thoracic surgery. 6th ed. Philadelphia (PA): Lippcott Williams & Wilkins; 2005. [Google Scholar]
- 6.Selke FW, Del Midi PJ, Swanson SJ. Surgery of the chest. 7th ed. Philadelphia (PA): Saunders Elsevier; 2005. [Google Scholar]
- 7.Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions 4.2.6. [accessed 2012 May 9]. [updated September 2006]. Available: www.cochrane.org/resources/handbook/hbook.htm.
- 8.Dickersin K, Chan S, Chalmers TC, et al. Publication bias and clinical trials. Control Clin Trials. 1987;8:343–53. doi: 10.1016/0197-2456(87)90155-3. [DOI] [PubMed] [Google Scholar]
- 9.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177–88. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 10.Breslow N, Day N. Statistical methods in cancer research Volume 1 The analysis of case-control studies. Lyon (France): International Agency for Research on Cancer; 1980. Combination of results from a series of 2 × 2 tables; control of confounding; pp. 136–46. [Google Scholar]
- 11.Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–58. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 12.Moher D, Cook DJ, Eastwood S, et al. Improving the quality of reports of meta-analyses of randomised controlled trials: the QUOROM statement. QUOROM group. Br J Surg. 2000;87:1448–54. doi: 10.1046/j.1365-2168.2000.01610.x. [DOI] [PubMed] [Google Scholar]
- 13.Alphonso N, Tan C, Utley M, et al. A prospective randomized controlled trial of suction versus non-suction to the under-water seal drains following lung resection. Eur J Cardiothorac Surg. 2005;27:391–4. doi: 10.1016/j.ejcts.2004.12.004. [DOI] [PubMed] [Google Scholar]
- 14.Ayed AK. Suction versus water seal after thoracoscopy for primary spontaneous pneumothorax: prospective randomized study. Ann Thorac Surg. 2003;75:1593–6. doi: 10.1016/s0003-4975(02)04894-4. [DOI] [PubMed] [Google Scholar]
- 15.Brunelli A, Monteverde M, Borri A, et al. Comparison of water seal and suction after pulmonary lobectomy: a prospective, randomized trial. Ann Thorac Surg. 2004;77:1932–7. doi: 10.1016/j.athoracsur.2003.12.022. [DOI] [PubMed] [Google Scholar]
- 16.Daneshvar KA, Pooya M, Pejhan S, et al. Effect of chest tube suction on air-leak following lung resection. Tanaffos. 2006;5:37–43. [Google Scholar]
- 17.Prokakis C, Koletsis EN, Apostolakis E, et al. Routine suction of intercostal drains is not necessary after lobectomy: a prospective randomized trial. World J Surg. 2008;32:2336–42. doi: 10.1007/s00268-008-9741-3. [DOI] [PubMed] [Google Scholar]
- 18.Atkins D, Best D, Briss PA, et al. Grading quality of evidence and strength of recommendations. BMJ. 2004;328:1490. doi: 10.1136/bmj.328.7454.1490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Guyatt G, Gutterman D, Baumann MH, et al. Grading strength of recommendations and quality of evidence in clinical guidelines: report from an American college of chest physicians task force. Chest. 2006;129:174–81. doi: 10.1378/chest.129.1.174. [DOI] [PubMed] [Google Scholar]
- 20.Guyatt GH, Oxman A, Vist G, et al. GRADE guidelines: 4. Rating the quality of evidence — study limitations (risk of bias) J Clin Epidemiol. 2011;64:407–15. doi: 10.1016/j.jclinepi.2010.07.017. [DOI] [PubMed] [Google Scholar]