Abstract
Background
Blood centers rely heavily upon adolescent donors to meet blood demand, but pre-syncope and syncope are more frequent in younger donors. Studies have suggested administration of water prior to donation may reduce syncope and/or pre-syncope in this group.
Study design and methods
We conducted a randomized, controlled trial to establish the effect of pre-loading with 500ml of water on the rate of syncope and pre-syncope in adolescent donors. School collection sites in Eastern Cape Province of South Africa were randomized to receive water or not. Incidence of syncope and pre-syncope was compared between randomization groups using multivariable logistic regression.
Results
Of 2,464 study participants, 1,337 received water and 1,127 did not; groups differed slightly by gender and race. Syncope or pre-syncope was seen in 23 (1.7%) of the treatment and 18 (1.6%) of the control arm subjects. After adjusting for race, gender, age and donation history, there was no difference in outcome between the water versus no water arms (adjusted odds ratio (OR) = 0.80 (95% CI 0.42–1.53). Black donors had 7-fold lower odds of syncope or pre-syncope than their white counterparts (adjusted OR 0.14, 95% CI 0.04–0.47).
Conclusion
Preloading adolescent donors with 500ml of water did not have a major effect in reducing syncope and pre-syncope in South African adolescent donors. Our adolescent donors had a lower overall syncope and pre-syncope rate than similar populations in the USA, limiting the statistical power of the study. We confirmed much lower rates of syncope and pre-syncope among young Black donors.
Keywords: Blood Donors, Syncope, Randomized control trial, South-Africa, Adolescent
Introduction
As with all blood transfusion services throughout the world, it remains the mission of the blood transfusion services in South Africa to provide sufficient, safe blood for all the patients of the country. While the advances in blood banking have substantially improved the safety of the blood supply over the past decades1,2, the provision of a constant and sufficient blood supply remains a challenge. In South Africa, historical events resulted in poor representation of non-white donors in the donor pool. Correcting this imbalance in the face of the background HIV prevalence has placed the local blood services under pressure. Additionally, an aging population is increasing the blood dependency ratio3 and stricter deferral criteria4 on donors are shrinking the donor pool.5,6
The South African National Blood Service has therefore turned increasingly to the recruitment of young, school-aged donors who comprise 19.7% of collections in South Africa and up to 25% in the Eastern Cape region. This may be compared to 2006 data for the American Red Cross, in which blood donations by 16 to 19 year olds accounted for 14.5% of annual donations.7 The adolescent age group is especially prone to syncopal events.7–11 Syncope and pre-syncope increase the risk of serious injury8 and donors who suffer adverse events have a lower return rate12,13. In the Eastern Cape, we have anecdotally observed an increase in young donors sustaining serious injuries due to falls associated with syncope events, and future collections are reduced at sites where such injuries have occurred. Some studies have suggested that preloading young donors with water may reduce their syncope and/or pre-syncope rates, and the procedure has been introduced in some blood organizations.14–16
Currently, there are very little data on syncope and pre-syncope event rates among South African donors in general and high school students in particular. It is assumed that the rates will be similar to donor populations in the USA and Europe, but this needs to be confirmed. The South African donors’ genetic and ethnic background differs considerably from populations studied elsewhere and so it is not clear whether findings from studies in the USA and Europe can be extrapolated to the South African context. In considering an operational intervention to preload all adolescent donors with water to reduce the syncope and pre-syncope rate, we must first confirm the baseline rate and in addition determine whether water preloading will reduce the syncope and presyncope rate.
For these reasons, we conducted a randomized controlled trial to measure the efficacy of water preloading in reducing syncope and presyncope events among school-age donors in the Eastern Cape of South Africa, during October of 2009.
Methods
Study Design and subjects
We conducted a randomized clinical trial on the effect of water preloading on syncope and presyncope among adolescent donors in the Eastern Cape during October of 2009. The study subjects included high school blood donors in the Eastern Cape of South Africa, who donated blood at mobile blood drives at their schools and who were 16 to 20 years old. Both first time and repeat donors were included in the study. Standard donor acceptance criteria applied and donors who were deferred in accordance with standard operating procedures were not included in the study. Donors are deferred if donating poses a risk to their health (e.g. cardiac conditions) or an infectious risk to the recipient (e.g. injection drug use or unsafe sexual practises). It was logistically impossible to randomize donors at the individual level, so we performed randomization at the school level. Recruitment commenced with verbal and or written consultation with the headmasters of the various schools, informing them of the planned study and requesting their permission to include data from their school blood drives in the study. All the headmasters contacted, agreed to participate. A random numbers table was used to assign each school to either the treatment or control arm of the study.
We were able to identify 79 high schools in the Eastern Cape which participate in regular blood drives (Fig 1). Only 75 schools were due for blood drives during October of 2011. Of these, 11 are located in the greater Mthatha region of the Eastern Cape. This area is located in the rural Eastern Cape and is logistically difficult to reach. As a result, they were excluded from the randomisation process. Finally, 64 schools were included in the randomization process.
Figure 1.
Flow chart showing participation and randomization status of schools and donors participating in the Water Intervention Study during October 2009 in the Eastern Cape, South Africa.
Intervention and outcomes
All donors at schools in the treatment arm were urged to consume 500ml of water shortly before donating between 475 to 575 mL of whole blood. A 500 mL plastic bottle of water at room temperature was given to the donor at the time of registration. The time-delay from registration to donation is between 15 and 30 minutes. At the schools randomized to receive water, the staff recorded whether water was administered and what portion of water was consumed, allowing analysis according to the “dose” of the fluid. No water was provided at schools randomized to the control arm, although refreshments were available after donation for both arms of the study. No refreshments were available during the donation process. Donor demographics and donation history were recorded in the blood center computer system for all donations, and extracted for later data analysis. Race was recorded as “White”; “Black”, “Coloured”, “Asian” and “Other”; the term “Coloured” is used in South Africa to denote persons of mixed race.
The primary outcome variable was a dichotomous variable of yes or no for syncope or pre-syncope. A secondary outcome was the severity of the events, which was recorded as an ordinal variable of none, mild, moderate or severe. Staff was retrained to ensure consistency in identifying and grading syncope and pre-syncope. Donors were actively monitored for all adverse events, including presyncope and syncope. They were asked about their general well-being but not specifically questioned as to the presence of presyncopal symptoms. A donor was marked as having had an event if he/she had a mild, moderate or severe event. Mild events are those where the donor feels dizzy, pales and becomes diaphoretic. The donor may also feel nauseous and vomit, but there is no loss of consciousness and the blood pressure remains stable. If the donor has any loss of consciousness, the event is recorded as being moderate. In addition, the blood pressure may drop from the pre-donation baseline, but recovers quickly. Severe events are those with sudden and even prolonged loss of consciousness with or without convulsions and prolonged low blood pressure.
Data analysis
We evaluated the success of the randomisation by assessing the distribution of the demographic characteristics of the study group. Standard summary statistics was used to characterise the study subjects by age, gender, race and donation history. The primary “intent to treat” analysis compared the outcome of syncope and pre-syncope between the randomization groups using unadjusted logistic regression. The secondary outcome analysis compared “Mild”, “Moderate” and “Severe” reactions, as defined above, between the groups. A “Per-Protocol” analysis, according to the proportion of water actually consumed (recorded as “none, ¼, ½, or ¾”) was also performed.
Multivariable logistic regression analysis was performed to assess the effect of the intervention on the primary outcome while controlling for potential imbalances between the groups. Subgroup analyses compared the effect of the water intervention in subgroups defined by age, gender and race. All statistical calculations were performed using STATA software, version 11.2 (StataCorp, College Station TX).
Power calculations were performed prior to the study. Because donor adverse events had not been recorded in the blood center computer system, the syncope and pre-syncope rate among our South African adolescent donors was unknown. We therefore used the results of Wiltbank et al., which described a syncope and pre-syncope rate of 3.9% in 17–18 year-olds. We felt that a reduction in the syncope and pre-syncope rate from the estimated 4% to 2% would be operationally significant. Using an event rate of 4.0% in controls and 2.0% in the treatment arm, a two-sided alpha of 0.05 and power (1-beta) of 0.80, we calculated the total sample size to be 1,237 per group, or 2,474 overall.
Ethical Considerations
Ethical approval to conduct the study, including a waiver of individual and parental consent, was obtained from the SANBS Research Ethics Committee. All the headmasters of the participating schools were contacted and informed of the study. Their permission was requested to use the data from their schools in the study. In South Africa parental consent is not required for donors 16 years and older to donate blood.
Results
Of the 64 schools included in the study, 33 were randomized to receive water and 31 were randomized to the control arm of the study (Figure 1). Due to scheduling conflicts between the dates allocated for the school blood drives and other large events at the schools, one school in the treatment arm and four schools in the control arm had to cancel their blood drives at short notice. Of the 32 schools remaining in the treatment arm, 28 (87%) were co-education schools, 4 (13%) were boys-only schools, and none were girls-only schools. In the 27 schools remaining in the control arm, 20 (74%) were co-education, 5 (18%) were boys only and 2 (7%) were small girls-only schools.
A total of 3,077 donors presented at the school blood drives. In accordance with standard operating procedures, 375 donors were deferred for a variety of reasons, included were 202 in the treatment arm and 173 in the control arm (Figure 1). All donors older than twenty years, including 234 teachers and staff at some of the schools, were excluded from the data analysis. Two donors were identified for whom parts of their data were missing and both were excluded from the analysis. Of the remaining 2,466 study participants, 1,339 were in the water arm and 1,127 were in the control arm (Table 1). The randomisation groups were similar with respect to age distribution and donor status, but differed in relation to gender and race. In the treatment arm, donors were more likely to be male and of White versus Black race than in the control arm.
Table 1.
Characteristics, by randomisation group, of the high school donors who participated in the Water Intervention Study during October 2009 in the Eastern Cape, South Africa.
| Water Arm | Control Arm | Chi squared P-value | |
|---|---|---|---|
| N=1339 | N=1127 | ||
| Gender | <0.001 | ||
| Male | 737 (55%) | 782 (69%) | |
| Female | 602 (45%) | 345 (31%) | |
| Race | <0.001 | ||
| White | 843 (63%) | 545 (48%) | |
| Coloured | 175 (13%) | 177 (16%) | |
| Black | 282 (21%) | 376 (33%) | |
| Asian/Other/Missing | 39 (3%) | 29 (3%) | |
| Age | 0.504 | ||
| 16 or under | 405 (30%) | 361 (32%) | |
| 17 | 515 (38%) | 421 (37%) | |
| 18 | 306 (23%) | 265 (24%) | |
| 19 and over | 113 (8%) | 80 (7%) | |
| Donation History | 0.503 | ||
| Repeat | 1016 (76%) | 842 (75%) | |
| First time | 323 (24%) | 285 (25%) |
Overall, out of the 2,466 scholars who donated, only 41 (1.7%) had any syncope or pre-syncope events (Table 2). Of these, the majority (76%) were minor, with only 9 moderate and 1 severe event; the latter occurred in the treatment arm. Syncope or pre-syncope occurred in 23 donors (1.7%) in the treatment arm compared to 18 (1.6%) donors in the control group (unadjusted OR=1.08, 95% CI 0.58 – 2.01). In the treatment arm, there was a significant trend towards fewer syncopal events in those who consumed all of their water compared to consumption of fractional amounts (p trend = 0.049). At eleven of the schools, more than one syncope or presyncope event occurred. Of these, six schools were in the treatment arm and involved 15 of the 26 events which occurred at these schools. No school had more than 3 events.
Table 2.
Number (percent) of syncope/pre-syncope episodes by randomization group, by reaction severity and by volume of water drunk.
| Syncope or Presyncope Episodes | Treatment Water (N=1339) N (%) |
Control No Water (N=1127) N (%) |
|---|---|---|
|
|
||
| Events by severity | 23 (1.72%) | 18 (1.60%) |
|
| ||
| Mild | 20 (87%) | 11 (61%) |
| Moderate | 2 (9%) | 7 (39%) |
| Severe | 1 (4%) | 0 (0%) |
|
| ||
|
Events by water intake
| ||
| 25% (N=75) | 2 (3%) | |
| 50% (N=75) | 4 (5%) | |
| 75% (N=94) | 3 (3%) | |
| 100% (N=1072) | 14 (1%) | |
| p = 0.049 | ||
We performed multivariate logistic regression modelling to control for imbalances in the demographics of the two arms, and other potential confounding variables (Table 3). In the final model, the adjusted OR for the treatment arm with respect to syncope and pre-syncope was 0.83 (95% CI 0.43 – 1.57). Among female donors the odds for an event was almost twice that of their male counterparts, although not quite statistically significant (OR = 1.80, 95% CI 0.94 – 3.40). Black donors had a 7-fold smaller odds of having a syncopal event compared to white donors (adjusted OR 0.14, 95% CI 0.04–0.47). There was no significant association with age in the adjusted model. Finally, first-time donors were twice as likely to experience syncope or pre-syncope as were repeat donors (adjusted OR 2.08, 95%CI 1.11–3.87).
Table 3.
Multivariable logistic regression analysis of associations with syncope/pre-syncope episodes.
| Associations | Syncopal Event | No Syncopal Event | Unadjusted OR (95% CI) | Adjusted OR (95% CI) |
|---|---|---|---|---|
| Randomization Arm | - | |||
| No Water | 18 (2%) | 1109 (98%) | 1.00 (−) | 1.00 (−) |
| Water | 23 (2%) | 1316 (98%) | 1.08 (0.58 – 2.01) | 0.83 (0.43 – 1.57) |
| Gender | ||||
| Male | 18 (1%) | 1501 (99%) | 1.00 (−) | 1.00 (−) |
| Female | 23 (2%) | 924 (98%) | 2.08 (1.11–3.87) | 1.80 (0.94 – 3.40) |
| Race | ||||
| White | 34 (2%) | 1354 (98%) | 1.00 (−) | 1.00 (−) |
| Coloured | 3 (1%) | 349 (99%) | 0.34 (0.10–1.12) | 0.29 (0.09 – 0.95) |
| Black | 3 (0.5%) | 655 (99.5%) | 0.18 (0.06–0.60) | 0.14 (0.04 – 0.47) |
| Other/Missing | 1 (1%) | 67 (99%) | 0.59 (0.08–4.40) | 0.54 (0.07 – 4.11) |
| Age | ||||
| 16 & under | 20 (3%) | 746 (97%) | 1.00 (−) | 1.00 (−) |
| 17 | 14 (1%) | 922 (99%) | 0.57 (0.28 – 1.13) | 1.28 (0.59 – 2.78) |
| 18 –20 | 7 (1%) | 757 (99%) | 0.35 (0.14 – 0.82) | 0.94 (0.36 – 2.45) |
| Donation history | ||||
| Repeat | 16 (1%) | 1842 (99%) | 1.00 (−) | 1.00 (−) |
| First time | 25 (4%) | 583 (96%) | 4.94 (2.62 – 9.31) | 2.08 (1.11 –3.87) |
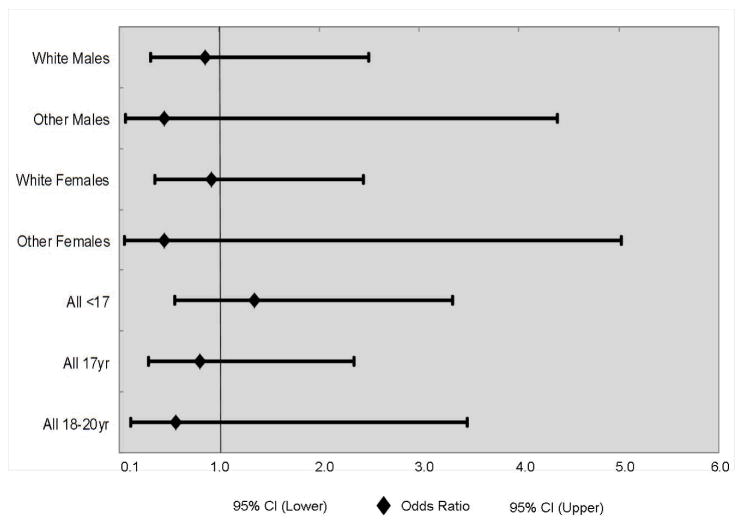
We next performed a subgroup analysis to assess whether the water intervention had differing effects in different demographic and donation history subgroups (Figure 2). Because of small numbers, donors were grouped into white and other race, and ages <17, 17 and 18–20 years. Confidence intervals on all of these subgroup estimates were wide, but most odds ratios clustered around one, and none were significantly different from one. In particular, there was no indication that White donors, who have highest a priori risk of syncope, had benefitted from the intervention. If anything, there was a suggestion that other race donors benefitted more. Thus, we have no real evidence for a particular subgroup of donors who might benefit from water intervention.
Figure 2.
Odds of syncope/pre-syncope reactions for water intervention, by demographic subgroups.
Discussion
During our randomized controlled study, we did not find a statistically significant difference in the number of syncope or pre-syncope events between the water and control arms of our study. The statistical power of the study to detect minor effects of water was limited due to a lower than anticipated syncope/pre-syncope incidence of 1.7% among adolescent donors in the Eastern Cape in South Africa, which is lower than reported in other adolescent donor populations. Furthermore, we noted a 7-fold lower risk of syncope and pre-syncope among our black adolescent donors as compared to the white adolescent donors. These data led us to conclude that there would be little operational or clinical benefit in introducing water preloading for adolescent donors in the South African setting.
Newman et al demonstrated in 2007 that preloading young donors with 473ml of water reduced syncope and pre-syncope reactions by 21%. Subsequently, a study in Japan showed that preloading at risk donors with a drink, may reduce the number of syncope/pre-syncope events in that group.17 Tomasulo et al also indicated that introducing water preloading in combination with other interventions, may reduce syncope/pre-syncope.16 More recently a small study in Ohio, USA, showed that consumption of 500ml water may reduce syncope and pre-syncope15 It is not certain why our study showed different results. First, our study was not powered to detect a 20% reduction, so we might have missed a small effect of water loading. Second, the lower than anticipated overall number of syncope and pre-syncope events we observed suggest population differences in susceptibility to syncope, perhaps explained by the relatively large number of black donors in our sample. Having fewer “at risk” donors, would not only reduce the number of events, but possibly diminish the effect of interventions aimed at reducing the risk.
The significantly lower than expected overall syncope and pre-syncope events among our scholars was surprising when compared to that noted in other studies18, and the generally higher incidence of complications and deferrals in younger compared to older donors.8–10,18–19 In 2006, Eder et al8, found that 10.7% of American Red Cross donors aged 16 to 17-years, and 8.3% of those aged 18 to 19 years experienced adverse events compared to 2.8% of those aged 20 and older. In a study of faint and prefaint reactions at 16 United Blood Services Centers, donors 17 to 18 years old had a reaction rate of 39.6/1,000 donation and an adjusted odds ratio of 2.75 for faint and prefaint reactions as compared to their 25 to 65 year old counterparts. Analysis of our unadjusted data demonstrated an almost linear reduction in syncope and pre-syncope with increasing age, but this effect was blunted after adjusting for gender, race and donation history.
It has been shown that donors who suffer adverse events have significantly lower return rates,12,13 with syncope and pre-syncope type symptoms having the biggest negative effect.12 In fact, those who do suffer adverse events may not donate again for as long as 5–6 years.20 Conversely, those who return soon after their first donation, were more likely to become habitual donors.21 Furthermore, very young donors have been shown to have higher return rates as long as their first donation experience was adverse event free.22 Finding interventions to minimize syncope and pre-syncope events is of great importance, but unfortunately, we confirmed that giving South African adolescent donors water to drink just prior to donating, will not reduce the number of vasovagal events in any meaningful manner. On the positive side, our lower than anticipated syncope/pre-syncope incidence suggests that this reaction should have less overall impact on donor return.
The relatively high proportion of Black (25%) and Coloured (15%) donors among our study group allowed for further interpretation of the syncope and pre-syncope events among the various race groups in the Eastern Cape. The black donors had 5 to 7 times fewer syncope and pre-syncope events than the white donors. The New York Blood Center reviewed the syncope and pre-syncope reactions among first time teenaged donors and found an overall syncope/pre-syncope reaction rate of 8.2% but a 1.3% rate among African-American high school students.18 Wiltbank et al demonstrated similar findings11. Additionally, we demonstrated that the odds of syncope/pre-syncope events among coloured donors were intermediate between those of blacks and whites. Even though this was not statistically significant, it is in keeping with the theory that there is a genetic factor that offers donors of African origin protection against syncope and pre-syncope. Recently, Hinds et al, showed greater orthostatic tolerance among young black versus white females and noted greater sympathetic response to orthostatic challenges in the former group23. This echoes work done by others24–26 and is in keeping with unpublished observations from other African blood transfusion services of very low syncope and pre-syncope events among African donors (personal communication, Dr P. Knox, 2011).
Similar to other studies, we noted that the female adolescent donors had a two-fold higher number of syncope and pre-syncope events compared to the males9,11,18. However, the absolute incidence of events among the females was lower in our trial than other published studies. Others have noted that this higher faint rate is likely, at least in part, to be related to the proportionally smaller blood volume in female donors. Unfortunately, body weight was not recorded during this study.
Our study had several strengths. Study participants were blinded as they were not aware of the purpose of the intervention. Additionally, the intervention was well defined and delivered under controlled circumstances, with the students receiving the water at the time of being registered. The lag time between being registered and starting the donation process would range between 10 and 30 minutes. Seasonal effects were minimized by completing the entire study within one month. The outcome was also well-defined, well-known event with which the observers are familiar. As a result, we are of the opinion that the effects of observer bias and placebo effect were kept to the minimum.
Our study had some limitations. Initially, we used the syncope/pre-syncope event rate reported in the Wiltbank11 study to calculate our sample size, but with our rate being significantly lower, our study may not have been powered to detect minor differences in syncope and pre-syncope rates between the two arms. We calculate that with the available sample size, our study would have been sufficiently powered to detect only a 69% relative or 1.1% absolute decrease (i.e. 0.5% in the water arm and 1.6% in the control arm). For our study to have been robustly powered at 80 percent, we would have required a sample size of 2907 donors per arm to detect a 50% reduction (0.8% decrease), or 21,760 donors per arm to detect a 20% reduction (0.32% decrease). Although a study of 6000 might be feasible in the future, it is unlikely that a study of 43,000 high school donors will ever be accomplished.
As it was not possible to randomize the participants by individual, we had to apply randomisation by school and the “no water” arm ended with more male and black donors compared to the “water” arm. We attempted to correct for this imbalance by using multivariable logistic regression, but residual confounding could have affected our results. Finally, there may have been under-reporting of minor pre-syncope events but presumably this would have been similar in both arms of the study.
In conclusion, although we showed no benefit of pre-donation water administration in preventing syncope and pre-syncope symptoms, we were able to establish the incidence of syncope/pre-syncope rates for adolescent donors in the Eastern Cape, as well as variation by age, race and gender. We showed similar variation in syncope/pre-syncopel reactions within these subgroups as reported by other authors, but the overall incidence of reactions was much lower than in the USA. Thus, population differences in reaction rates illustrate the need for international blood services to conduct local research before implementing changes based upon findings from other countries. Finally, the experience gained with this study has resulted in improved processes for reporting and recording donor adverse events within the South African National Blood Service, paving the way for more detailed analysis of donor reactions within South Africa.
Acknowledgments
Funding for the research and manuscript were received from: Novartis; Blood Systems Research Institute; University of California, San Francisco, Center for AIDS Prevention Studies, US National Institute Mental Health (NIMH), P30 MH062246; International Society for Blood Transfusion and NHLBI Career Award K24-HL075036 to Dr. Murphy
The authors wish to thank the staff of the Eastern Cape Zone of the South African National Blood Service for their role in collecting the data, the headmasters of the various schools for participation in the study, the staff of the University of California, San Francisco’s International Traineeships in AIDS Prevention Studies (ITAPS), (U.S. NIMH, R25MH064712) for their valuable contribution to the development of the manuscript and Ms Susan Yuen for her assistance in submitting the manuscript.
Footnotes
The above author may be contacted for reprint requests.
The authors declare that they have no conflicts of interest relevant to the manuscript submitted to TRANSFUSION.
References
- 1.Glynn SA. Blood supply safety: an NHLBI perspective. Transfusion. 2008;48:1541–4. doi: 10.1111/j.1537-2995.2007.01754.x. [DOI] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention (CDC) Progress toward strengthening blood transfusion services--14 countries, 2003–2007. MMWR Morbidity And Mortality Weekly Report. 2008;57:1273–7. [PubMed] [Google Scholar]
- 3.Ali A, Auvinen M-K, Rautonen J. The aging population poses a global challenge for blood services. Transfusion. 2010;50:584–8. doi: 10.1111/j.1537-2995.2009.02490.x. [DOI] [PubMed] [Google Scholar]
- 4.Zou S, Musavi F, Notari EP, Rios JA, Trouern-Trend J, Fang CT. Donor deferral and resulting donor loss at the American Red Cross Blood Services, 2001 through 2006. Transfusion. 2008;48:2531–9. doi: 10.1111/j.1537-2995.2008.01903.x. [DOI] [PubMed] [Google Scholar]
- 5.Riley W, Schwei M, McCullough J. The United States’ potential blood donor pool: estimating the prevalence of donor-exclusion factors on the pool of potential donors. Transfusion. 2007;47:1180–8. doi: 10.1111/j.1537-2995.2007.01252.x. [DOI] [PubMed] [Google Scholar]
- 6.Custer B, Johnson ES, Sullivan SD, et al. Quantifying losses to the donated blood supply due to donor deferral and miscollection. Transfusion. 2004;44:1417–26. doi: 10.1111/j.1537-2995.2004.04160.x. [DOI] [PubMed] [Google Scholar]
- 7.Eder AF, Dy BA, Kennedy JM, et al. The American Red Cross donor hemovigilance program: complications of blood donation reported in 2006. Transfusion. 2008;48:1809–19. doi: 10.1111/j.1537-2995.2008.01811.x. [DOI] [PubMed] [Google Scholar]
- 8.Eder AF, Hillyer CD, Dy BA, Notari EPt, Benjamin RJ. Adverse reactions to allogeneic whole blood donation by 16- and 17-year-olds. JAMA: The Journal Of The American Medical Association. 2008;299:2279–86. doi: 10.1001/jama.299.19.2279. [DOI] [PubMed] [Google Scholar]
- 9.Reiss RF, Harkin R, Lessig M, Mascari J. Rates of vaso-vagal reactions among first time teenaged whole blood, double red cell, and plateletpheresis donors. Annals Of Clinical And Laboratory Science. 2009;39:138–43. [PubMed] [Google Scholar]
- 10.Newman BH, Satz SL, Janowicz NM, Siegfried BA. Donor reactions in high-school donors: the effects of sex, weight, and collection volume. Transfusion. 2006;46:284–8. doi: 10.1111/j.1537-2995.2006.00713.x. [DOI] [PubMed] [Google Scholar]
- 11.Wiltbank TB, Giordano GF, Kamel H, Tomasulo P, Custer B. Faint and prefaint reactions in whole-blood donors: an analysis of predonation measurements and their predictive value. Transfusion. 2008;48:1799–808. doi: 10.1111/j.1537-2995.2008.01745.x. [DOI] [PubMed] [Google Scholar]
- 12.Newman BH, Newman DT, Ahmad R, Roth AJ. The effect of whole-blood donor adverse events on blood donor return rates. Transfusion. 2006;46:1374–9. doi: 10.1111/j.1537-2995.2006.00905.x. [DOI] [PubMed] [Google Scholar]
- 13.Olatunji BO, Etzel EN, Ciesielski BG. Vasovagal syncope and blood donor return: examination of the role of experience and affective expectancies. Behavior Modification. 2010;34:164–74. doi: 10.1177/0145445510362576. [DOI] [PubMed] [Google Scholar]
- 14.Newman B, Tommolino E, Andreozzi C, Joychan S, Pocedic J, Heringhausen J. The effect of a 473-mL (16-oz) water drink on vasovagal donor reaction rates in high-school students. Transfusion. 2007;47:1524–33. doi: 10.1111/j.1537-2995.2007.01293.x. [DOI] [PubMed] [Google Scholar]
- 15.France CR, Ditto B, Wissel ME, et al. Predonation hydration and applied muscle tension combine to reduce presyncopal reactions to blood donation. Transfusion. 2010;50:1257–64. doi: 10.1111/j.1537-2995.2009.02574.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tomasulo P, Kamel H, Bravo M, James RC, Custer B. Interventions to reduce the vasovagal reaction rate in young whole blood donors. Transfusion. 2011;51:1511–21. doi: 10.1111/j.1537-2995.2011.03074.x. [DOI] [PubMed] [Google Scholar]
- 17.Ando S-i, Kawamura N, Matsumoto M, et al. Simple standing test predicts and water ingestion prevents vasovagal reaction in the high-risk blood donors. Transfusion. 2009;49:1630–6. doi: 10.1111/j.1537-2995.2009.02189.x. [DOI] [PubMed] [Google Scholar]
- 18.Newman BH. Vasovagal reactions in high school students: findings relative to race, risk factor synergism, female sex, and non-high school participants. Transfusion. 2002;42:1557–60. doi: 10.1046/j.1537-2995.2002.00238.x. [DOI] [PubMed] [Google Scholar]
- 19.Newman BH. Blood donor complications after whole-blood donation. Current Opinion In Hematology. 2004;11:339–45. doi: 10.1097/01.moh.0000142105.21058.96. [DOI] [PubMed] [Google Scholar]
- 20.Schlumpf KS, Glynn SA, Schreiber GB, et al. Factors influencing donor return. Transfusion. 2008;48:264–72. doi: 10.1111/j.1537-2995.2007.01519.x. [DOI] [PubMed] [Google Scholar]
- 21.Ownby HE, Kong F, Watanabe K, Tu Y, Nass CC. Analysis of donor return behavior. Retrovirus Epidemiology Donor Study. Transfusion. 1999;39:1128–35. doi: 10.1046/j.1537-2995.1999.39101128.x. [DOI] [PubMed] [Google Scholar]
- 22.Notari EPt, Zou S, Fang CT, Eder AF, Benjamin RJ, Dodd RY. Age-related donor return patterns among first-time blood donors in the United States. Transfusion. 2009;49:2229–36. doi: 10.1111/j.1537-2995.2009.02288.x. [DOI] [PubMed] [Google Scholar]
- 23.Hinds K, Stachenfeld NS. Greater orthostatic tolerance in young black compared with white women. Hypertension. 2010;56:75–81. doi: 10.1161/HYPERTENSIONAHA.110.150011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zion AS, Bond V, Adams RG, et al. Low arterial compliance in young African-American males. American Journal Of Physiology Heart And Circulatory Physiology. 2003;285:H457–H62. doi: 10.1152/ajpheart.00497.2002. [DOI] [PubMed] [Google Scholar]
- 25.Goldstein IB, Shapiro D. The cardiovascular response to postural change as a function of race. Biological Psychology. 1995;39:173–86. doi: 10.1016/0301-0511(94)00958-Z. [DOI] [PubMed] [Google Scholar]
- 26.Parmer RJ, Cervenka JH, Stone RA. Baroreflex sensitivity and heredity in essential hypertension. Circulation. 1992;85:497–503. doi: 10.1161/01.cir.85.2.497. [DOI] [PubMed] [Google Scholar]