Abstract
Background and Purpose
Post-traumatic stress disorder (PTSD) can be triggered by life-threatening medical events such as strokes and transient ischemic attacks (TIA). Little is known regarding how PTSD triggered by medical events affects patients’ adherence to medications.
Methods
We surveyed 535 participants, age ≥ 40 years old, who had at least one stroke or TIA in the previous 5 years. PTSD was assessed using the PTSD Checklist-Specific for stroke (PCL-S); a score ≥ 50 on this scale is highly specific for PTSD diagnosis. Medication adherence was measured using the 8-item Morisky scale. Logistic regression was used to test whether PTSD after stroke/TIA was associated with increased risk of medication non-adherence. Covariates for adjusted analyses included sociodemographics, Charlson comorbidity index, modified Rankin score, years since last stroke/TIA, and depression.
Results
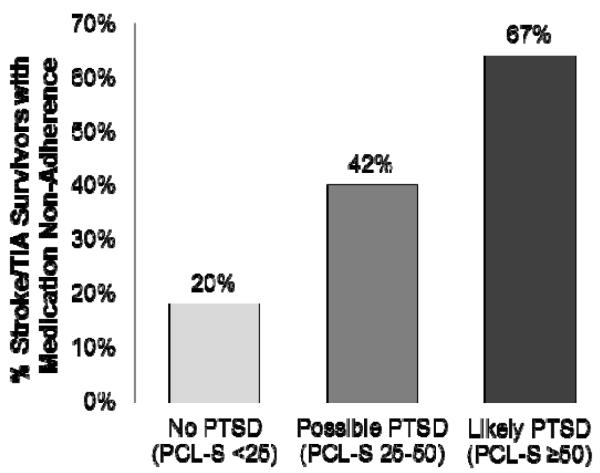
Eighteen percent of participants had likely PTSD (PCL-S ≥ 50), and 41% were non-adherent to medications according to the Morisky. A greater proportion of participants with likely PTSD were non-adherent to medications than other participants (67% versus 35%, p<0.001). In the adjusted model, participants with likely PTSD were nearly three times more likely (RR 2.7, 95%CI 1.7, 4.2) to be non-adherent compared to participants without PTSD (PCL-S <25) even after controlling for depression, and there was a graded association between PTSD severity and medication non-adherence.
Conclusion
PTSD is common after stroke/TIA. Patients who have PTSD after stroke or TIA are at increased risk for medication non-adherence.
Keywords: stroke care, TIA, psych & behavior
Introduction
Although exposures to violence and natural disasters represent common sources of trauma that lead to post-traumatic stress disorder (PTSD), a growing body of literature demonstrates that PTSD can also occur after acute, life-threatening medical events such as strokes and transient ischemic attacks (TIA).(1-3) Individuals with post-traumatic stress disorder (PTSD) due to non-medical traumatic events are at increased risk for poor physical health and prognosis.(4, 5) Less is known about the impact of PTSD on physical health when PTSD is triggered by acute medical events. There are many potential biological and behavioral explanations for the association of PTSD with poor outcomes(6); one of the most compelling is that PTSD may be associated with poor adherence to medications prescribed for primary and secondary prevention.
Survivors of strokes and TIAs may be at especially high risk for developing PTSD as stroke/TIA has many of the characteristics of events that are likely to trigger PTSD: namely, the onset of symptoms is unexpected, uncontrollable, and can be perceived as life-threatening.(7) Furthermore, in survivors of strokes/TIA, adherence to risk-reducing medications including antiplatelet agents, antihypertensives, and statins is especially important for preventing subsequent strokes.(8)
Prior research has shown an association between PTSD and lower adherence to medications for certain medical conditions such as HIV(9, 10) and coronary heart disease.(11, 12) Yet, depression is often comorbid in patients with PTSD, and some studies suggest that the association between PTSD and poor adherence is due to confounding by depression.(12) In contrast with PTSD, depression has been robustly associated with medication non-adherence in numerous studies.(13-15) However, the relationship between PTSD and adherence has been explored in very few medical conditions, and there may indeed be an important association between the two that merits investigation. Accordingly, we assessed whether PTSD after stroke/TIA is associated with medication non-adherence in stroke survivors even after accounting for depression and other established correlates of non-adherence.
Methods
Participants
Participants were recruited between March 2010 and January 2012 as part of a clinical trial - Preventing Recurrence of All Inner City Strokes (PRAISE) - which tests the effectiveness of a peer-led educational workshop at improving risk factor control in community dwelling survivors of strokes and TIAs. Participants were eligible for the trial if they were at least 40 years of age and if they self-reported a history of stroke or TIA in the prior 5 years. Participants were excluded if they did not have capacity to provide informed consent, if they did not have the physical or mental capacity to participate in classes, if they were non-English and non-Spanish speaking, if they resided in nursing homes or other institutionalized settings, if they were pregnant, or if they were unable to meaningfully participate in the workshop as a result of aphasia or severe cognitive impairment.
Participants were identified through screenings at senior centers, churches and health fairs; by contacting patients with history of stroke on hospital registries of an academic medical center, a federally funded neighborhood health center, and the Visiting Nurse Service of New York; and through advertising the study in clinics and local organizations and newspapers in northern Manhattan and Southern Bronx, New York. The data collected for the analysis presented in this manuscript was collected as part of the baseline interview for the trial; no study-related interventions had occurred prior to collecting information for this analysis. Design of all study procedures was made with the input of a community action board comprised of individuals from East and Central Harlem. Ethics approval was obtained from the Institutional Review Board of the Mount Sinai School of Medicine. All participants provided written informed consent.
Outcome Measure
Adherence to overall medications was measured using the 8-item Morisky Medication Adherence Questionnaire (Morisky).(16) The Morisky is a self-report measure of adherence that has good internal validity. Each of the 8 items assesses specific medication-taking behaviors such as forgetting medications or stopping medications when one perceives one’s medical condition to be under good control. Summary scores on the questionnaire can be used to classify patients into low and high adherence groups and these groupings are concordant with objective measures of medication adherence including pharmacy refills.(17) To reduce social desirability effects, the questions related to medication adherence were preceded by the statement: “We want to know how you feel, not how you think doctors or other people you know feel.” According to the cutpoints recommended by the developers of the Morisky, participants who scored less than 6 points on the Morisky were categorized as non-adherent to medications and participants who scored 6 to 8 points on the Morisky were categorized as adherent to medications.(16)
Predictor Variables
PTSD symptoms were assessed with a modified version of the PTSD Checklist Specific for a stressor (PCL-S), using the stressor “stroke or mini-stroke.”(18) The PCL-S is an extensively validated 17-item scale that corresponds to DSM-IV criteria for PTSD. Participants were asked to rate whether they had specific PTSD symptoms as a result of their stroke or mini-stroke. To make the PCL-S more homogenous with the rest of the survey and easier to complete for participants of low health literacy, the instrument was modified from a 5-point (“not at all”, “a little bit”, “moderately”, “quite a bit”, “extremely”) to a 4-point response scale (“not at all”, “a little bit”, “somewhat”, “very much”). In addition, three items (loss of interest, trouble falling or staying asleep, difficulty concentrating) from the Patient Health Questionnaire (PHQ)(19) were used in place of PCL-S items as there was substantial content and wording overlap between these items on both instruments. Confirmatory factor analysis verified that these three PHQ items performed as predicted, loading on first-order PTSD symptom factors with standardized factor loadings equivalent to PCL-S items. To allow our scoring to be comparable to other studies using the PCL-S, we recoded PCL-S scores to reflect the standard 5-point response scale (1 = 1; 2 = 2.33; 3= 3.67; 4 = 5), so that the range of the total PCL-S score was the same as that used with the unmodified instrument. While studies of PTSD in civilian populations have used cutpoints from 30 to 44 for diagnosing PTSD, we used the more stringent cutpoint of 50 to categorize participants as having likely PTSD as recommended by the developers of the scale. This cutpoint has corresponded to a sensitivity of 60% and specificity of 99% in relation to a clinical diagnosis of PTSD due to breast cancer diagnosis.(20)
Depressive symptoms were measured using the 8-item PHQ (PHQ-8). The PHQ-8 has similar discriminant properties for diagnosing depression as the 9-item version(21), and the 9-item version has been validated for use in post-stroke patients(22) and in minority populations.(23) A score of 10 or higher on the PHQ-8 signifies at least mild to moderate depressive symptoms.
Demographic information including age, gender, race/ethnicity, annual household income, and insurance status were also collected by patient interview. For cases when data was missing on annual household income (n=40), participants were categorized as having “low income” if they had Medicaid insurance. Three participants were missing information on both income and insurance status and were not included in the adjusted logistic regression models. Stroke severity was measured by asking patients the modified Rankin scale(24); a score of 3 or higher on this scale signifies at least moderate disability as a result of the stroke. Stroke timing was measured by asking the year of their most recent stroke or TIA.(25) Comorbidity was measured using the Charlson comorbidity index.(26)
Analysis Plan
PTSD was not normally distributed and was dichotomized into PTSD versus no PTSD using PCL-S score of 50 as a cutpoint for the primary analysis. Chi squared and t-tests were used to compare characteristics of participants according to whether or not they had PTSD. To determine whether there was a graded association between PTSD and medication adherence, PTSD was also divided into 3 groups: no PTSD (PCL-S <25), possible PTSD (PCL-S 25-50) and likely PTSD (PCL-S ≥ 50). We chose these cutpoints based on a review of predefined cutpoints in the literature.
We then used unadjusted and adjusted logistic regression to calculate the odds ratios and 95% confidence intervals of medication non-adherence associated with PTSD. We chose covariates for adjusted analyses based on a review of the literature for important patient-level predictors of poor adherence to cardiovascular medications.(27, 28) Given the high co-morbidity between depression and PTSD in prior samples and the potential for confounding by depression status, we tested separate models with and without depression. As there was a high non-adherence rate, we used GenMod procedure with a modified Poisson regression approach to estimate the adjusted relative risks (RR).(29) All analyses were performed using SAS statistical software, version 9.2 (SAS Institute, Inc., Cary, NC).
Results
We surveyed 535 participants for this study. The mean age of participants was 63 years, 59% were women, 80% were Black or Latino, 30% never completed high school, and 56% earned less than $15,000 yearly.(Table 1) Eighteen percent of participants had symptoms consistent with a diagnosis of PTSD, and 56% of participants had possible PTSD (PCL-S 25-50). Compared to participants without likely PTSD (PCL-S<50), those with PTSD were younger and were more likely to be women, minorities (Black and Hispanic), low-income, unmarried, and unable to work. Participants with PTSD also had a higher Charlson comorbidity score and higher stroke-related disability as measured by the modified Rankin. In addition, participants with PTSD were more likely to have elevated depressive symptoms (PHQ-8 ≥ 10) than those without PTSD (78% versus 19%, p<0.001).
Table 1.
Characteristics of Participants with Prior Stroke or Transient Ischemic Attack With and Without Elevated Symptoms of Post-Traumatic Stress Disorder*
| Characteristic | Overall (N=535) |
PTSD (PCLS≥50) (N=95) |
No PTSD (PCLS<50) (N=440) |
P-value |
|---|---|---|---|---|
| Age, mean ± SD | 63.0 ± 11.3 | 57.2 ± 8.5 | 64.2 ± 11.5 | <0.001 |
| Women | 317 (59) | 65 (68) | 252 (57) | 0.05 |
| Race/ethnicity | ||||
| Black | 210 (40) | 40(42) | 170 (40) | 0.002 |
| Hispanic | 212 (40) | 48 (51) | 164 (38) | |
| White | 76 (14) | 2 (2) | 74 (17) | |
| Other | 27 (5) | 5 (6) | 22 (5) | |
| Income ≤ $15,000/year | 300 (56) | 74 (79) | 226 (52) | <0.001 |
| Less than high school education | 157 (30) | 25 (27) | 132 (30) | 0.53 |
| Preferred language Spanish | 127 (24) | 22 (23) | 105 (24 ) | 0.88 |
| Married/live with a partner | 192 (36) | 21 (22) | 171 (39) | 0.002 |
| Live alone | 185 (35) | 40 (42) | 145 (33) | 0.09 |
| Employment status | ||||
| Full or part-time | 76 (14) | 7 (7) | 69 (16) | <0.001 |
| Unable to work | 205 (38) | 64 (67) | 141 (32) | |
| Retired, in school, or other | 252 (47) | 24 (25) | 228 (52) | |
| Number of prior strokes and TIAs, mean ± SD | 1.7 ± 1.2 | 1.8 ± 1.3 | 1.6 ± 1.2 | 0.13 |
| Years since last stroke or TIA, mean ± SD | 1.9 ± 1.4 | 1.7 ± 1.4 | 1.9 ± 1.5 | 0.17 |
| Charlson score, mean ± SD | 3.7 ± 2.2 | 4.4 ± 2.3 | 3.5 ± 2.1 | <0.001 |
| Stroke impact severity | ||||
| Modified Rankin 0,1, or 2 | 287 (54) | 23 (24) | 264 (60) | <0.001 |
| Modified Rankin 3 or 4 | 248 (46) | 72 (76) | 176 (40) | |
| Depressed (PHQ-8 >10) | 159 (30) | 74 (78) | 85 (19) | <0.001 |
| Non-adherent to medications (Morisky 0-5) | 218 (41) | 64 (67) | 154 (35) | <0.001 |
Abbreviations: PTSD, post-traumatic stress disorder; PCL-S, PTSD Checklist Specific for Stroke; TIA, transient ischemic attack; PHQ-8, Patient Health Questionnaire-8 Item
Data are presented as number (%) unless otherwise specified
Forty-one percent of participants were non-adherent to medications according to the Morisky. Nearly twice as many participants with PTSD were non-adherent as compared to participants without PTSD (65% vs 33%, p<0.001). There was also a graded association between PTSD symptom severity and medication non-adherence. (Figure 1)
Figure 1.
Association between Post-Traumatic Stress Disorder Symptom Severity and Medication Non-Adherence Among Survivors of Stroke or Transient Ischemic Attack (N=535)
In both unadjusted and adjusted logistic regression analyses, PTSD was associated with medication non-adherence.(Table 2) In the model adjusted for demographic and clinical predictors of non-adherence, likely PTSD was associated with a nearly 3-fold increase in the risk for non-adherence [RR 2.90 (95% CI 1.92, 4.42)] as compared to stroke/TIA survivors with no PTSD. Although the addition of a depression measure (PHQ-8) into the model attenuated the relationship between PTSD and medication adherence, PTSD remained significantly associated with medication non-adherence whereas depressive symptom severity (PHQ-8 score) was not. In the fully adjusted model, participants with possible PTSD and with likely PTSD had increased odds of medication non-adherence compared to stroke/TIA survivors without PTSD [RR 1.86 (95%CI 1.26, 2.74) and 2.69 (95%CI 1.71, 4.23); respectively].
Table 2.
Unadjusted and Adjusted Relative Risks and 95% Confidence Intervals for Associations between Post-Traumatic Stress Disorder and Non-Adherence to Medications in Survivors of Stroke or Transient Ischemic Attack
| Characteristic | Model 1 (N=535) | Model 2 (N=532) | Model 3 (N=532) |
|---|---|---|---|
|
| |||
| PTSD | |||
| Likely PTSD (PCL-S>50) | 3.42 (2.36, 4.96) | 2.91 (1.92, 4.42) | 2.69 (1.71, 4.23) |
| Possible PTSD (PCL-S 25-50) | 2.10 (1.45, 3.04) | 1.92 (1.31, 2.80) | 1.86 (1.27, 2.74) |
| No PTSD (PCL-S <25) | Ref | Ref | Ref |
|
| |||
| Age | - | 0.99 (0.98, 1.00) | 0.99 (0.98, 1.00) |
|
| |||
| Gender | - | ||
| Female | - | 1.12 (0.91, 1.38) | 1.10 (0.90, 1.36) |
| Male | - | Ref | Ref |
|
| |||
| Race/ethnicity | - | ||
| Black/Hispanic/Other | 1.20 (0.79, 1.21) | 1.19 (0.77, 1.83) | |
| White | Ref | Ref | |
|
| |||
| Income | - | ||
| <$15,000/year | 0.98 (0.79, 1.21) | 0.97 (0.79, 1.20) | |
| ≥$15,000/year | Ref | Ref | |
|
| |||
| Charlson score | - | 1.04 (1.00, 1.08) | 1.04 (1.00, 1.08) |
|
| |||
| Stroke impact severity | - | ||
| Modified Rankin 3 to 4 | 0.92 (0.74, 1.14) | 0.92 (0.74, 1.14) | |
| Modified Rankin 0 to 2 | Ref | Ref | |
|
| |||
| Years since last stroke/TIA | - | 1.06 (1.00, 1.14) | 1.06 (1.00, 1.14) |
|
| |||
| Depressive symptoms (PHQ-8≥10) | - | - | 1.12 (0.88, 1.42) |
Abbreviations: PTSD, post-traumatic stress disorder; PCL-S, Post-Traumatic Stress Disorder Checklist-Specific for Stroke/Transient Ischemic Attack; PHQ-8, Patient Health Questionnaire-8 Item
Discussion
To date, the understanding of PTSD’s association with medication adherence has been confounded by its association with depressive symptoms. We aimed to determine whether this would be the case for a group of individuals who were at high risk for PTSD and who had a strong need to adhere to medication to prevent future catastrophic health events, namely stroke and TIA survivors from diverse communities. We found that, indeed, elevated symptoms of PTSD were common in stroke or TIA survivors up to 5 years after their most recent stroke or TIA, with 18% of participants having symptoms consistent with a likely PTSD diagnosis and nearly 3 out of 4 participants with elevated symptoms of PTSD. Furthermore, stroke/TIA survivors with likely PTSD had nearly three times the risk of medication non-adherence in adjusted analyses, and the association between PTSD and medication adherence remained significant even after controlling for depressive symptoms. Furthermore, even participants with more modest elevations in PTSD symptoms were at increased risk of medication non-adherence, broadening the relevance of this risk factor for non-adherence to a large number of stroke/TIA survivors.
A large percentage of participants in our sample (41%) were non-adherent according to the Morisky questionnaire. For comparison, in the Adherence eValuation After Ischemic stroke–Longitudinal (AVAIL) Registry, only 14% of participants self-reported being non-adherent to medications.(30) In the AVAIL study, low socioeconomic status was associated with lower adherence. Hence, the high prevalence of patients from low socioeconomic background may help explain the higher prevalence of non-adherence in our sample.
Prior studies assessing the relationship between PTSD triggered by acute medical events and medication non-adherence have not always found an independent association after adjusting for covariates.(10, 12) There are several possible explanations for why our results differed. First, we had a relatively large sample size and a high proportion of participants were non-adherent to medications. These factors increased our statistical power to detect independent associations in multivariable analyses. However, the large magnitude of the relative risks we found suggest that power was not the only difference between our study and previous investigations.
The severity of PTSD may have been higher in our post-stroke/TIA sample as compared to other populations.(31) Our finding that symptom severity is associated with medication non-adherence suggests that greater PTSD severity in our sample may account for the difference between our findings and previous studies. Strokes and TIAs may be especially conducive to PTSD as a result of the acute, frightening nature of the stroke/TIA-related symptoms.
Finally, the fact that the triggering event for the PTSD symptoms was a medical event as compared to other sources of trauma may have resulted in a distinct association between PTSD and self-management of medical illness. For example, one of the defining clusters of PTSD symptoms is avoidance of reminders of the triggering event. Accordingly, when symptoms of PTSD are triggered by medical events, PTSD may cause patients to avoid stroke medications if they serve as reminders of the PTSD-inducing event.
A number of other potential mechanisms might explain the relationship between PTSD and medication non-adherence. PTSD has been directly associated with deficits in cognitive function both in patients with and without traumatic brain injury.(32, 33) Accordingly, cognitive dysfunction may be a mechanism linking PTSD with medication non-adherence due to forgetfulness or other cognitive factors. Some investigators have hypothesized that participants with elevated PTSD symptoms may hold different beliefs about treatment that may impact on medication adherence.(34) Wagner et al. showed that among African American HIV-infected individuals, perceived discrimination by the health care system partially mediated the relationship between PTSD and non-adherence to antiretroviral medications.(35) Given the high proportion of participants at risk for discrimination in our sample on account of their minority and low income status, it would be important to test this mechanism in future studies. This mechanism, however, may not be generalizable to other patient populations.
There were several limitations to the interpretation of our findings. The cross-sectional nature of the data prevents us from ascribing causal attributions to the association of PTSD to medication adherence. The recruitment of a high proportion of minorities from low socioeconomic backgrounds and of individuals who were motivated to participate in an educational workshop may have limited the generalizability of the study’s findings to other populations. The PCL-S and PHQ-8 measure symptoms of PTSD and depression, respectively, but these do not replace diagnoses based on a psychiatric interview. Further, a modified version of the PCL-S was used and this may have influenced its discriminant properties. Nevertheless, we used the most conservative cutpoint for categorizing participants as having likely PTSD and may have underestimated the true prevalence of PTSD diagnosed by a psychiatric interview. Medication adherence was measured using self-report and no objective measures of adherence were available to confirm responses. Although the Morisky has been validated with objective adherence measures in other studies, patients tend to over-report how well they adhere to medications such that the prevalence of poor adherence to medications may be underestimated by this study.
Summary/Conclusions
The results of this study suggest that not only is PTSD common after strokes and TIAs, but that PTSD may be putting stroke/TIA survivors at increased risk for recurrent cerebrovascular events as a result of decreased medication adherence. Although the impact of PTSD on subsequent prognosis remains unknown, PTSD after acute coronary events has previously been associated with worse cardiovascular prognosis.(36, 37) Hence, the results of this study suggest that poor medication adherence may, at least in part, mediate the relationship between PTSD and poor medical outcomes in patients with cardiovascular disease. Future studies should seek to elucidate the mechanisms linking PTSD with poor adherence in stroke/TIA survivors and should test approaches to improving adherence in this population.
Acknowledgements
We gratefully acknowledge the East and Central Harlem Community Action Board and the study participants for their generous contributions.
Sources of Funding
Dr. Kronish received support from the National Heart, Lung and Blood Institute (K23 HL098359). Drs. Horowitz, Goldfinger and Ms. Fei received support from the National Institute of Minority Health and Health Disparities (P60MD00270) and Dr. Horowitz received funding from the National Center for Research Resources (UL1RR029887).
Abbreviations
- PCL-S
Post-Traumatic Stress Disorder Checklist-Specific for stroke/transient ischemic attack
- TIA
transient ischemic attack
Footnotes
Conflicts-of-Interest/Disclosures: None
This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Bruggimann L, Annoni JM, Staub F, von Steinbuchel N, Van der Linden M, Bogousslavsky J. Chronic posttraumatic stress symptoms after nonsevere stroke. Neurology. 2006;66:513–6. doi: 10.1212/01.wnl.0000194210.98757.49. [DOI] [PubMed] [Google Scholar]
- 2.Shemesh E, Koren-Michowitz M, Yehuda R, Milo-Cotter O, Murdock E, Vered Z, et al. Symptoms of posttraumatic stress disorder in patients who have had a myocardial infarction. Psychosomatics. 2006;47:231–9. doi: 10.1176/appi.psy.47.3.231. [DOI] [PubMed] [Google Scholar]
- 3.Tedstone JE, Tarrier N. Posttraumatic stress disorder following medical illness and treatment. Clin Psychol Rev. 2003;23:409–48. doi: 10.1016/s0272-7358(03)00031-x. [DOI] [PubMed] [Google Scholar]
- 4.Wisnivesky JP, Teitelbaum SL, Todd AC, Boffetta P, Crane M, Crowley L, et al. Persistence of multiple illnesses in World Trade Center rescue and recovery workers: a cohort study. Lancet. 2011;378:888–97. doi: 10.1016/S0140-6736(11)61180-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Beckham JC, Moore SD, Feldman ME, Hertzberg MA, Kirby AC, Fairbank JA. Health status, somatization, and severity of posttraumatic stress disorder in Vietnam combat veterans with posttraumatic stress disorder. Am J Psychiatry. 1998;155:1565–9. doi: 10.1176/ajp.155.11.1565. [DOI] [PubMed] [Google Scholar]
- 6.Boscarino JA. Posttraumatic stress disorder and physical illness: results from clinical and epidemiologic studies. Ann N Y Acad Sci. 2004;1032:141–53. doi: 10.1196/annals.1314.011. [DOI] [PubMed] [Google Scholar]
- 7.Ehlers A, Clark DM. A cognitive model of posttraumatic stress disorder. Behav Res Ther. 2000;38:319–45. doi: 10.1016/s0005-7967(99)00123-0. [DOI] [PubMed] [Google Scholar]
- 8.Rothwell PM, Algra A, Amarenco P. Medical treatment in acute and long-term secondary prevention after transient ischaemic attack and ischaemic stroke. Lancet. 2011;377:1681–92. doi: 10.1016/S0140-6736(11)60516-3. [DOI] [PubMed] [Google Scholar]
- 9.Cohen MA, Alfonso CA, Hoffman RG, Milau V, Carrera G. The impact of PTSD on treatment adherence in persons with HIV infection. Gen Hosp Psychiatry. 2001;23:294–6. doi: 10.1016/s0163-8343(01)00152-9. [DOI] [PubMed] [Google Scholar]
- 10.Vranceanu AM, Safren SA, Lu M, Coady WM, Skolnik PR, Rogers WH, et al. The relationship of post-traumatic stress disorder and depression to antiretroviral medication adherence in persons with HIV. AIDS Patient Care STDS. 2008;22:313–21. doi: 10.1089/apc.2007.0069. [DOI] [PubMed] [Google Scholar]
- 11.Shemesh E, Yehuda R, Milo O, Dinur I, Rudnick A, Vered Z, et al. Posttraumatic stress, nonadherence, and adverse outcome in survivors of a myocardial infarction. Psychosom Med. 2004;66:521–6. doi: 10.1097/01.psy.0000126199.05189.86. [DOI] [PubMed] [Google Scholar]
- 12.Zen AL, Whooley MA, Zhao S, Cohen BE. Post-traumatic stress disorder is associated with poor health behaviors: Findings from the heart and soul study. Health Psychol. 2012;31:194–201. doi: 10.1037/a0025989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.DiMatteo MR, Lepper HS, Croghan TW. Depression is a risk factor for noncompliance with medical treatment: meta-analysis of the effects of anxiety and depression on patient adherence. Arch Intern Med. 2000;160:2101–7. doi: 10.1001/archinte.160.14.2101. [DOI] [PubMed] [Google Scholar]
- 14.Kronish IM, Rieckmann N, Halm EA, Shimbo D, Vorchheimer D, Haas DC, et al. Persistent depression affects adherence to secondary prevention behaviors after acute coronary syndromes. J Gen Intern Med. 2006;21:1178–83. doi: 10.1111/j.1525-1497.2006.00586.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rieckmann N, Kronish IM, Haas D, Gerin W, Chaplin WF, Burg MM, et al. Persistent depressive symptoms lower aspirin adherence after acute coronary syndromes. Am Heart J. 2006;152:922–7. doi: 10.1016/j.ahj.2006.05.014. [DOI] [PubMed] [Google Scholar]
- 16.Morisky DE, Ang A, Krousel-Wood M, Ward HJ. Predictive validity of a medication adherence measure in an outpatient setting. J Clin Hypertens (Greenwich) 2008;10:348–54. doi: 10.1111/j.1751-7176.2008.07572.x. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 17.Krousel-Wood M, Islam T, Webber LS, Re RN, Morisky DE, Muntner P. New medication adherence scale versus pharmacy fill rates in seniors with hypertension. Am J Manag Care. 2009;15:59–66. [PMC free article] [PubMed] [Google Scholar]
- 18.Weathers FWLT, Herman DS, Huska J, Keane T. The PTSD checklist: reliability, validity, and diagnostic utility; Annual Meeting of the International Society for Traumatic Stress Studies; San Antonio, TX. 1993. [Google Scholar]
- 19.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Andrykowski MA, Cordova MJ, Studts JL, Miller TW. Posttraumatic stress disorder after treatment for breast cancer: prevalence of diagnosis and use of the PTSD Checklist-Civilian Version (PCL-C) as a screening instrument. J Consult Clin Psychol. 1998;66:586–90. doi: 10.1037//0022-006x.66.3.586. [DOI] [PubMed] [Google Scholar]
- 21.Kroenke K, Spitzer RL, Williams JB, Lowe B. The Patient Health Questionnaire Somatic, Anxiety, and Depressive Symptom Scales: a systematic review. Gen Hosp Psychiatry. 2010;32:345–59. doi: 10.1016/j.genhosppsych.2010.03.006. [DOI] [PubMed] [Google Scholar]
- 22.Schmid AA, Kroenke K, Hendrie HC, Bakas T, Sutherland JM, Williams LS. Poststroke depression and treatment effects on functional outcomes. Neurology. 2011;76:1000–5. doi: 10.1212/WNL.0b013e318210435e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Huang FY, Chung H, Kroenke K, Delucchi KL, Spitzer RL. Using the Patient Health Questionnaire-9 to measure depression among racially and ethnically diverse primary care patients. J Gen Intern Med. 2006;21:547–52. doi: 10.1111/j.1525-1497.2006.00409.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wilson JT, Hareendran A, Grant M, Baird T, Schulz UG, Muir KW, et al. Improving the assessment of outcomes in stroke: use of a structured interview to assign grades on the modified Rankin Scale. Stroke. 2002;33:2243–6. doi: 10.1161/01.str.0000027437.22450.bd. [DOI] [PubMed] [Google Scholar]
- 25.Banks JL, Marotta CA. Outcomes validity and reliability of the modified Rankin scale: implications for stroke clinical trials: a literature review and synthesis. Stroke. 2007;38:1091–6. doi: 10.1161/01.STR.0000258355.23810.c6. [DOI] [PubMed] [Google Scholar]
- 26.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–83. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 27.Mann DM, Woodward M, Muntner P, Falzon L, Kronish I. Predictors of nonadherence to statins: a systematic review and meta-analysis. Ann Pharmacother. 2010;44:1410–21. doi: 10.1345/aph.1P150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;353:487–97. doi: 10.1056/NEJMra050100. [DOI] [PubMed] [Google Scholar]
- 29.McNutt LA, Wu C, Xue X, Hafner JP. Estimating the relative risk in cohort studies and clinical trials of common outcomes. Am J Epidemiol. 2003;157:940–3. doi: 10.1093/aje/kwg074. [DOI] [PubMed] [Google Scholar]
- 30.Bushnell CD, Olson DM, Zhao X, Pan W, Zimmer LO, Goldstein LB, et al. Secondary preventive medication persistence and adherence 1 year after stroke. Neurology. 2011;77:1182–90. doi: 10.1212/WNL.0b013e31822f0423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Shemesh E, Rudnick A, Kaluski E, Milovanov O, Salah A, Alon D, et al. A prospective study of posttraumatic stress symptoms and nonadherence in survivors of a myocardial infarction (MI) Gen Hosp Psychiatry. 2001;23:215–22. doi: 10.1016/s0163-8343(01)00150-5. [DOI] [PubMed] [Google Scholar]
- 32.Qureshi SU, Long ME, Bradshaw MR, Pyne JM, Magruder KM, Kimbrell T, et al. Does PTSD impair cognition beyond the effect of trauma? J Neuropsychiatry Clin Neurosci. 2011;23:16–28. doi: 10.1176/jnp.23.1.jnp16. [DOI] [PubMed] [Google Scholar]
- 33.Nelson LA, Yoash-Gantz RE, Pickett TC, Campbell TA. Relationship between processing speed and executive functioning performance among OEF/OIF veterans: implications for postdeployment rehabilitation. J Head Trauma Rehabil. 2009;24:32–40. doi: 10.1097/HTR.0b013e3181957016. [DOI] [PubMed] [Google Scholar]
- 34.Spoont M, Sayer N, Nelson DB. PTSD and Treatment Adherence: the role of health beliefs. J Nerv Ment Dis. 2005;193:515–22. doi: 10.1097/01.nmd.0000172474.86877.2b. [DOI] [PubMed] [Google Scholar]
- 35.Wagner GJ, Bogart LM, Galvan FH, Banks D, Klein DJ. Discrimination as a key mediator of the relationship between posttraumatic stress and HIV treatment adherence among African American men. J Behav Med. 2012;35:8–18. doi: 10.1007/s10865-011-9320-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Edmondson D, Rieckmann N, Shaffer JA, Schwartz JE, Burg MM, Davidson KW, et al. Posttraumatic stress due to an acute coronary syndrome increases risk of 42-month major adverse cardiac events and all-cause mortality. J Psychiatr Res. 2011;45:1621–6. doi: 10.1016/j.jpsychires.2011.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.von Kanel R, Hari R, Schmid JP, Wiedemar L, Guler E, Barth J, et al. Non-fatal cardiovascular outcome in patients with posttraumatic stress symptoms caused by myocardial infarction. J Cardiol. 2011;58:61–8. doi: 10.1016/j.jjcc.2011.02.007. [DOI] [PubMed] [Google Scholar]