Abstract
Accumulating evidence highlights the importance of using psychosocial approaches to intervention for children with ADHD that target the family and school, as well as the intersection of family and school.
Objective
This study was designed to evaluate the effectiveness of a family-school intervention, referred to as Family-School Success (FSS), designed to improve the family and educational functioning of students in grades 2 through 6 who meet criteria for ADHD combined and inattentive types. Key components of FSS were conjoint behavioral consultation, daily report cards, and behavioral homework interventions.
Methods
FSS was provided over the course of 12 weekly sessions, which included 6 group sessions, 4 individualized family sessions, and 2 school-based consultations. Families participating in the study were given the choice of placing their children on medication; 43% of children were on medication at the time of random assignment. Children (n=199) were randomly assigned to FSS or a comparison group controlling for non-specific treatment effects. Outcomes were assessed at post intervention and 3-month follow-up. The analyses controlled for child medication status.
Results
Study findings indicated that FSS had a significant effect on the quality of the family-school relationship, homework performance, and parenting behavior.
Conclusions
The superiority of FSS was demonstrated even though about 40% of the participants in FSS and CARE were on an optimal dose of medication and there were significant Time effects on each measure. This relatively brief intervention was able to produce effect sizes that were comparable to those of the more intensive MTA behavioral intervention.
Keywords: ADHD, intervention, behavioral, family, school
Evaluation of a Family-School Intervention for Children with ADHD: Results of a Randomized Clinical Trial of 199 Students in Grades 2 to 6
Children with attention-deficit/hyperactivity disorder (ADHD) generally have significant educational impairments (DuPaul & Stoner, 2003). Empirically supported treatments include stimulant medication and behavioral interventions (Fabiano, Pelham, Coles, Gnagy, Chronic-Tuscano, & O’Connor, 2009; MTA Cooperative Group, 1999). Behavioral interventions targeting educational problems have been based primarily in schools or summer camps. Research has shown that behavioral approaches applied in school are effective in reducing ADHD symptoms and related impairments, although the effects on academic functioning have been modest (DuPaul & Stoner, 2003). Numerous studies also have documented the effectiveness of psychosocial interventions for families coping with ADHD. These treatments typically have placed less emphasis on addressing educational problems, although there is evidence that these approaches have beneficial effects on school functioning (Fabiano et al., 2009).
Effect of Family Functioning on School Performance
Research indicates that family functioning can have an effect on school performance in at least two ways. First, parenting practices that promote strong parent-child attachments and child self regulation help children succeed in school (Pianta, 1997). Research on effective parenting practices strongly supports the use of behavioral parent training programs as a strategy to promote child success at both home and school (Fabiano et al., 2009). Second, family involvement in education has been shown to contribute to school success (Christenson & Sheridan, 2001). Family involvement can take the form of parental engagement in educational activities in the home, such as supporting children with homework, as well as effective collaboration between family and school, such as parent-teacher conferences to resolve problems arising at school (Fantuzzo, Tighe & Childs, 2000). Interventions for children with ADHD have placed less emphasis on promoting family involvement in education, although use of a daily report card, which involves ongoing parent-teacher communication (see Vannest, Davis, Davis, Mason, & Burke, 2010), is an exception to this rule. The parents of children with ADHD generally have significant concerns about their children’s schooling, but they have a low sense of self-efficacy in being able to resolve educational problems (Rogers, Wiener, Marton, & Tannock, 2009) and existing intervention models are not adequate in assisting parents in this role.
Multi-Modal Approaches to Psychosocial Intervention
In an effort to improve the functioning of children with ADHD in both home and school settings, several investigators have developed multimodal approaches to psychosocial intervention. A notable example is the Multimodal Treatment Study of Children with ADHD (MTA). The family behavioral component in the MTA addressed school issues by incorporating a daily report card and educating parents to become educational advocates (Wells, Pelham et al., 2000). Although the family intervention in the MTA was highly intensive, it was not possible to determine the unique effects of this treatment because it was bundled together with other components. Regardless, the multi-component behavioral intervention was superior to the community control condition on only two outcome variables: negative parenting and homework problems (Langberg et al., 2010; Wells, Epstein et al., 2000). One factor that may have limited the MTA’s ability to achieve significant outcomes, especially related to educational concerns, was that the MTA intervention had only a limited focus on homework performance. Systematic interventions that incorporate goal setting and contingency contracting are now available to improve homework and educational performance (Kahle & Kelley, 1994; Power, Karustis, & Habboushe, 2001). Second, the MTA attempted to improve the family-school relationship, but it did not employ a systematic model for doing so. Conjoint behavioral consultation, which involves the development of family-school partnerships and use of problem solving strategies to address school problems, is a promising method for improving the school performance of children with attention and behavior problems (Sheridan, Eagle, Cowan & Michelson, 2001).
Over the past several years, other examples of family-school interventions for children with ADHD have emerged (e.g., Abikoff et al., 2004; Owens, Murphy, Richerson, Girio, & Himawan, 2008; Pfiffner, Mikami, Huang-Pollock, Easterlin; Zalecki, & McBurnett, 2007). The program developed by Abikoff and colleagues included parent training, daily report cards, organizational skills training, and social skills training. Although this intervention was highly comprehensive and applied over the course of 2 years, the study was not designed to examine the effectiveness of the psychosocial treatment. Pfiffner and colleagues included behavioral parent training, child skills training, and teacher consultation. A noteworthy finding of this study was that the intervention resulted in improvements in organizational skills relative to the control group. The family-school intervention developed by Owens and colleagues included daily report cards, behavioral consultation to teachers, and parent training. This study demonstrated reductions in ADHD symptoms and impairments as well as an improvement in child relationships with parents and teachers in comparison to a control group. Although these programs are exemplars of multimodal treatment, limitations included: (a) a lack of focus on promoting family involvement in education and providing systematic homework interventions, (b) a lack of emphasis on promoting family-school, problem-solving partnerships, and (c) the use of a study design that did not evaluate psychosocial treatment in relation to a comparison group controlling for non-specific treatment effects.
Key Components of Family-mediated Educational Interventions
The Family-School Success (FSS) program addresses the limitations of existing multimodal treatments by focusing on building family-school partnerships through the use of components of conjoint behavioral consultation, and promoting family involvement in education through systematic homework interventions. In addition, similar to other multi-component interventions, FSS incorporates a daily report card. Unlike most previous investigations, FSS was evaluated in relation to a comparison group controlling for non-specific treatment effects.
Conjoint behavioral consultation (CBC)
Strengthening parent-teacher relationships is critical to creating a context to resolve students’ school problems (Sheridan & Kratochwill, 2008). CBC is a structured problem solving process in which parents and teachers work collaboratively through the stages of behavioral consultation. This model has been applied successfully with children who have a wide range of behavioral and educational problems, including youngsters with ADHD (Sheridan et al., 2001).
Homework interventions
Homework interventions focus on changing both antecedents and consequences (Power et al., 2001). School-based antecedents are the assignment of a reasonable amount of work and teacher checks to verify the accuracy of recorded assignments. A key home-based antecedent is establishing an optimal time for completing work. Contingency management programs, involving positive reinforcement for task completion, have been shown to be effective (DuPaul & Stoner, 2003). A particularly promising approach is goal setting with contingency contracting, which involves: (a) establishing realistic goals, (b) evaluating performance in relation to goals, and (c) administering reinforcers contingent upon goal attainment (Kahle & Kelley, 1994).
Daily report card (DRC)
DRC is a behavioral intervention that involves the delivery of contingencies at home based upon teacher reports of school performance. DRC requires that teachers evaluate students on one or more target behaviors at least once per day. At the end of the day, the student is instructed to take the note home for parental review. Parents are trained to set reasonable goals for performance and reinforce the child for goal attainment. Considerable evidence supports the effectiveness of the DRC (Vannest et al., 2010).
Study Hypotheses
In a large sample of children with ADHD in grades 2 through 6, this study evaluated the acceptability of FSS and the tested the hypothesis that FSS would be more effective than an active control group with regard to: (a) increasing family involvement in education and improving the quality of the parent-teacher relationship; (b) improving homework performance; (c) improving parent-child interactions; (d) reducing ADHD and ODD symptoms at home and school; and (e) improving academic performance. Outcomes were evaluated at post intervention and 3-month follow-up.
Method
Participants
This study was conducted through an ADHD center within a pediatric hospital located in a large metropolitan area in the Northeast section of the U.S. Inclusion criteria were the following: (a) children enrolled in grades 2 through 6; (b) children meeting criteria for ADHD, Combined Type (ADHD/COM) or ADHD, Inattentive Type (ADHD/I) based upon parent-report on the Schedule for Affective Disorders and Schizophrenia for School Age Children - DSM IV (K-SADS-P IVR; Ambrosini, 2000); (c) children rated at or above the 85th percentile on the Inattention or Hyperactivity-Impulsivity factor of the ADHD Rating Scale-IV School Version (ADHD RS-IV; DuPaul, Power, Anastopoulos, & Reid, 1998), or the Attention Problems or Hyperactivity subscales of the Behavior Assessment System for Children, Second Edition - Teacher Rating Scales (BASC-2; Reynolds & Kamphaus, 2004); (d) children scoring at or above 0.75 of a standard deviation above the mean on the Homework Problem Checklist (HPC; Anesko, Schoiock, Ramirez, & Levine, 1987), which was considered an indicator of educational impairment; and (e) children scoring at or above an estimated IQ of 75 on the 2-subtest version of the Wechsler Abbreviated Scale of Intelligence (WASI; Psychological Corporation, 1999). For children on medication, decisions were based on responses to K-SADS items in the present or past state, and responses to ratings scales completed prior to the child being on medication.
Children meeting DSM-IV criteria for a psychotic disorder, bipolar disorder, chronic tic disorder or Tourette’s disorder, anxiety or mood disorder serious enough to warrant separate treatment, history of major neurological illness, and history of suicidal or homicidal behavior or ideation were excluded. Furthermore, children were excluded if they were currently receiving psychotropic medications, and their parents chose not to undergo a new medication trial as part of the study. Children with learning disabilities (as assessed using standardized tests administered for this study or as reported by school multidisciplinary evaluation teams), disruptive disorders (oppositional defiant disorder and conduct disorder), and internalizing disorders (anxiety and mood disorders, with the exception of bipolar disorder) were included.
Potential subjects for the study were identified in two ways: (a) parent-initiated referrals from the clinic within the hospital’s ADHD center; and (b) referrals from school and community providers (e.g., primary care and mental health professionals). Referrals from the clinic were obtained through a review of intake information for children whose parents requested a diagnostic evaluation. In addition, the medical records of children who completed diagnostic evaluations during the 6 months prior to the start of the study were reviewed to identify potential participants for the initial cohorts. In either case, if record review suggested that the child met initial eligibility criteria, a research assistant contacted the family by telephone to determine whether they were interested in study participation and to complete additional screening. Families referred by school professionals and community providers also were contacted by a research assistant, who completed the telephone screening.
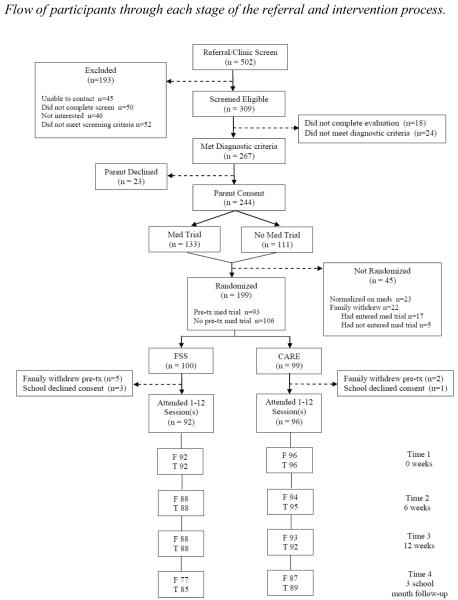
During the screening telephone call, the following information was obtained: (a) the child’s grade in school, (b) the child’s medication status at the time of referral, (c) name and dose of medication for children prescribed medication at the time of referral, (d) the parent’s preference for medication use during the study, and (e) parent ratings of child homework difficulties on the HPC. If the child met initial inclusion criteria based on this screening, the research assistant requested that the parent obtain teacher ratings of child behavior on the ADHD RS-IV School Version and the BASC-2 Teacher Rating Scales. Upon receipt of teacher ratings, the research assistant determined if the child met the screening criterion (i.e., inattention or hyperactive/impulsive ratings at or above the 85th percentile). If the child was taking medication at the time of screening and ratings were below the 85th percentile, scores from prior evaluations were reviewed. If screening ratings met eligibility criteria, the family was contacted, and a clinic visit was scheduled to conduct the diagnostic evaluation. At the diagnostic evaluation, the K-SADS-P IVR was completed by a licensed psychologist or advanced doctoral student supervised by a psychologist). Diagnostic interviews were audio recorded and 16.2% were selected at random for review by an independent clinician/doctoral trainee. Inter-rater agreement was 94% (κ = .87) for ADHD, Combined Type; 98% (κ = .96) for ADHD, Inattentive Type; 94% (κ = .74) for disruptive behavior disorders; and 98% (κ = .62) for mood and anxiety disorders. Figure 1 illustrates the screening and diagnostic process for referred families. Referrals were received for 502 children; 457 families were successfully contacted by telephone, and in 45 cases the study team was unable to reach the family to complete the screening process. Of the initial referrals, 309 completed telephone screening and met initial criteria, 291 of those families completed the diagnostic evaluation, and in 244 of these cases, the child was eligible for the study and the study team obtained parent consent. In 133 cases, the family elected to participate in the medication trial prior to randomization to treatment group. For those children, 93 were still eligible and interested in continuing in the study at the conclusion of the medication trial, and these cases were advanced to randomization to treatment group (see below for details about the medication trial). Of the consented families, 199 were randomly assigned to a treatment group.
Figure 1.
Flowchart of participation from screening to follow-up assessment 3 academic months after treatment. FSS = Family-School Success intervention; CARE = Coping with ADHD through Relationships and Education; F = Families completing measures; T = Teachers completing measures
Study Interventions
Family-School Success (FSS)
FSS is a 12-session family-school intervention designed to improve parenting skills, family involvement in education, family-school collaboration, and student academic engagement and productivity. In addition to components that are standard in behavioral parent training programs, FSS includes three educationally-focused intervention components: CBC, DRC, and homework interventions (Soffer & Power, 2005a).
FSS provides intervention using three formats: (a) parent group meetings (6 sessions) held simultaneously with separate child group sessions; (b) individualized family therapy (4 sessions), including the parents and child; and (c) family-school consultations (2 sessions) held at the school, including parents and teachers. While parents attend group sessions, their children participate in a group designed to introduce them to the strategies being taught to their parents. Child sessions are intended to be both educational and recreational (see Power, Karustis, & Habboushe, 2001). A behavioral management program (i.e., a token economy) was utilized during the child group sessions. An outline of program sessions is described in Table 1.
Table 1. Description of each session for Family School Success.
| Session Title | Session Type | Session Content |
|---|---|---|
| 1 - Introduction to Family School Success |
Group | Introduction to FSS Orientation to the CBC model Using attention to change child behavior |
| 2 - Preparing for Home-School Collaboration |
Individual Family |
Preparation for first school consultation Use of homework assignment books Use of DRC |
| 3 - Promoting Home- School Collaboration |
School Meeting |
Establishing collaborative home-school relationship Establishing use of assignment book & DRC |
| 4 - Understanding Basics of Behavior Management |
Individual Family |
Review school meeting Develop understanding of positive reinforcement and punishment |
| 5 - Introducing the Token Economy |
Group | Group discussion of school meetings Establishing a token economy |
| 6 - Understanding the Function of Behavior and Establishing the Homework Ritual |
Group | Functional assessment to define homework problems (antecedents and consequences) Establishing the homework routine Guidelines for giving effective instructions |
| 7 - Managing Time and Goal Setting |
Individual Family |
Time management strategies for homework completion Goal setting approach to homework completion |
| 8 - Managing Time and Goal Setting - 2 |
Individual Family |
Review goal setting strategies with clinician modeling and feedback |
| 9 - Using Punishment Successfully |
Group | Group discussion of experiences with goal setting Rationale for using punishment strategically Response cost and time-out Prepare for second school consultation |
| 10 - Collaborating to Refine Strategies |
School Meeting |
Review use of DRC and modify if needed Use of goal setting in the classroom |
| 11 - Developing Effective Study Skills |
Group | Strategies for effective study skills, including incremental rehearsal |
| 12 - Integrating Skills and Planning for the Future |
Group | Review and problem solve implementation difficulties Develop individual family “Formulas for Success” End of program celebration |
Note: CBC = Conjoint Behavioral Consultation; DRC = Daily Report Card
During this study one clinician was assigned to work with each cohort of parents. This clinician conducted parent group sessions and had responsibility for working with families in individualized family sessions and school-based sessions. In addition, three clinical assistants (graduate students in applied psychology) were assigned to work with each child group to ensure that children’s behavior was managed appropriately and safely during program sessions.
Sessions were held on a weekly basis. The initial session lasted 3 hours. Subsequent group sessions were 90 minutes in length. Individualized family sessions lasted 60 minutes. Each school session was approximately 45 minutes in duration. Two phone conferences between the clinician and the teacher (approximately 10 minutes each after sessions 5 and 7) were conducted to monitor the child’s progress and to refine interventions, if needed.
In this study, 13 FSS cohorts were conducted. The number of families per group ranged from 3 to 10, with a mean of 7. Seven clinicians (i.e., 6 post doctoral fellows in psychology and one doctoral level, non-licensed school psychologist with 15 years experience) conducted FSS groups: two conducted three groups each with a total of 18 and 20 families, respectively; a third conducted two groups with a total of 16 families; a fourth had two groups totaling 14 families; the fifth had one group of 9 families; the sixth had one group of 7 families; and the seventh had one group with 8 families. One of the FSS clinicians also conducted one cohort of the comparison treatment; in all other cases, the clinicians were assigned to either FSS or the comparison treatment. Eighty-eight teachers participated in the intervention; four teachers were involved in FSS for two children each. Two of the children (one teacher) were involved in the same cohort. The remaining six children (three teachers) were involved in separate cohorts.
Coping with ADHD through Relationships and Education (CARE)
CARE is a 12-session program designed to provide support and education to parents. There were three components of this program: (a) discussing children’s progress at home and school, (b) establishing a context within which parents can support each other in coping with their children’s difficulties, and (c) providing generic education to parents about ADHD. Education provided to parents focuses on ADHD, its associated features, and the challenges these children often encounter at home, in school, and with peers (Soffer & Power, 2005b).
The purpose of implementing CARE was to control for the non-specific effects of intervention. The content of CARE sessions did not address the primary components of FSS. Although parents were informed about potentially useful intervention strategies, they were not provided training in the use of empirically supported interventions. CARE did not involve parents and teachers in the process of problem solving, nor did it involve training parents in the use of contingency management strategies. During CARE, children met in groups while parents attended group sessions. Children in CARE received education on topics covered in the parent groups and engaged in fun, recreational activities. Similar to FSS, the child group clinicians utilized a token economy to support behavioral management during the child group sessions. One clinician was assigned to work with each cohort of parents, and three clinical assistants (graduate students in applied psychology) worked with each child group.
CARE included 11 group sessions and 1 family-school meeting, which were held on consecutive weeks. The initial session was conducted on a Saturday for 3 hours and subsequent meetings were 75 minutes (approximately the average amount of time spent with families in FSS sessions). The purpose of the school meeting was to acquire information about school functioning and not to engage in problem solving or behavioral consultation. The same procedures were used to obtain teacher consent and investment as were described for FSS.
In this study, 13 CARE cohorts were conducted. The number of families per group ranged from 5 to 10, with a mean of 7. Six clinicians (i.e., 1 pre-doctoral intern in psychology, 1 post doctoral fellow in psychology, 3 licensed psychologists, 1 doctoral level school psychologist with 4 years experience) conducted CARE groups: three conducted three groups each (25, 22, and 16 families, respectively); a fourth conducted two groups with a total of 18 families; a fifth had one group of 9 families; and the sixth had one group of 6 families. Ninety-four teachers participated in the intervention. Two teachers were involved in CARE for two children each; two children participated in the same cohort, and two were in separate cohorts.
Intervention Procedures
Program manuals were developed for both FSS and CARE. All clinical activities for FSS and CARE were supervised by a licensed psychologist with 10 years of experience working with the parents and teachers of children with ADHD. Prior to the start of each cohort, the FSS and CARE clinical teams reviewed the program manuals and met with the clinical supervisor to discuss program implementation. Throughout the intervention, parent group clinicians met with the supervisor weekly for 1 hour of individual supervision. To prevent contamination, clinicians for CARE received explicit, weekly instructions in the manual and from their supervisor not to: (a) engage in problem solving activities with parents, (b) discuss contingency management approaches, or (c) suggest strategies for building the family-school relationship. The supervisor directly observed approximately 80% of the CARE sessions to ensure adherence. Prior to group sessions, the clinical assistants met with the parent group leader to discuss implementation of the upcoming session and any specific issues that had arisen related to child behavior management during the previous child group. All parent group and individual family therapy sessions were videotaped for integrity monitoring purposes.
Several procedures were used to elicit teacher investment (for FSS and control group): (a) a letter briefly explaining the study was sent to teachers and their principals at the outset; (b) a phone call was initiated by the assigned clinician to the child’s teacher to introduce the study and schedule a face-to-face meeting; (c) the assigned clinician visited the school to obtain principal authorization and teacher consent, and provide the teacher with an explanation of the treatment being offered. Additional goals during the initial school meeting were for the clinician to establish rapport with the teacher and identify the teacher’s primary concerns about the child.
Integrity Monitoring and Session Attendance
For each FSS and CARE session, integrity checklists were created indicating all content to be delivered during the session, as specified in the manuals. External evaluators rated the extent to which each component was implemented (0 = not implemented, 1 = partially implemented, 2 = fully implemented). For group and individual family sessions, videotapes of randomly selected sessions were reviewed. For school sessions, an external evaluator conducted direct observations of selected meetings.
Integrity levels were high for both FSS and CARE. For FSS, integrity checks were conducted on 23% of individual, 30% of group, and 8% of school sessions. For FSS individual sessions, on average 86% of intervention components were fully implemented. For group sessions, clinicians fully implemented 90% of the intervention components. Finally, for school sessions, clinicians fully implemented 94% of the intervention components. For CARE, integrity checks were conducted on 18% of group and 14% of school sessions. For CARE group sessions, clinicians fully implemented 90% of the intervention components, and for school sessions 98% of the content was fully implemented.
On average, families who participated in FSS attended 10.4 (SD = 2.0) of the 12 regularly scheduled sessions, and 90% of the families attended at least 9 of 12 sessions. Attendance within each session format was equally high; for the 6 group, 4 individual family therapy, and 2 school sessions, mean session attendance was 5.1, 3.5, and 1.9 respectively. Make-up sessions were completed for 54% of all missed FSS sessions. Families who participated in CARE attended an average of 10.4 (SD = 1.9) regularly scheduled sessions; 88% of participants attended at least 9 of 12 sessions. CARE families were present for an average of 9.4 of the 11 regularly scheduled group sessions, and all except one family attended the school meeting. Make-up sessions were completed for 57% of all missed CARE sessions. Although attendance generally was high, adherence with parent-assigned homework activities in FSS was variable; of the six assignments given, 35% to 62% were partially or fully completed. No homework was assigned for CARE.
Medication Trial Procedures
Families were given the option to enroll in the study with or without pharmacological treatment. Children whose parents elected medication were managed by the study team, including two developmental pediatricians. The medication trial was completed before group assignment. The open-label titration of medication followed a modified version of the Texas algorithm (Pliszka et al., 2006), beginning with OROS-methylphenidate, and if necessary proceeding to mixed amphetamine salts extended release, and then atomoxetine. If the child did not respond well to these medications, alternative FDA-approved medications for ADHD were used. The medication trial was designed as a collaborative process between family and physician; if there was a compelling rationale to use an alternative sequence or medication, the physician and family collaborated to modify the protocol.
Prior to the trial, parent and teacher ratings on the MTA SNAP-IV (Swanson et al., 2001) were obtained. If the child was on medication at time of enrollment, they were taken off medication to obtain these ratings. During titration, ratings were obtained weekly. When atomoxetine was used, response was assessed after the child had been on a dose for 3 weeks. Norms from the ADHD RS-IV (DuPaul et al., 1998) were used to score the ADHD items from the SNAP-IV. A dose of medication was considered “effective” if parent or teacher ratings indicated a decrease of at least 15 percentage points on the relevant factor of the ADHD RS-IV and there were no significant side effects. Side effects were identified using parent responses to the Stimulant Drug Side Effects Rating Scale (Barkley, 1981). If response to a dose did not meet criteria for an “effective” response, the dose was increased to a maximum of 54 mg for OROS-methylphendate, 15 mg for mixed amphetamine salts, and 1.4 mg/kg/dose for atomoxetine. If a child completed a trial using all three medications and did not meet criteria for an “effective” response, one of three options were selected by the physician and family: (a) begin the psychosocial intervention on no medication, (b) select the best dose from among those tested; (c) continue medication trials until a stable medication and dose was found. When the most effective dose was identified, the parent completed the HPC to determine if educational impairment was still present (≥ .75 SD above mean). If so, the family was randomized to group. If not, the child was not advanced through the study and the family was offered a brief educational program.
At the point of parent consent, 133 (54.5%) families opted to start a medication trial. Twenty-three (17.3%) of these children were ineligible after the trial because they no longer met HPC criteria. Seventeen (12.8%) other families dropped out during the medication trial for other reasons (e.g., time burden, psychiatric complications). Altogether, 93 (69.9%) of the 133 children were assigned to a group. Of these children, 81 (87.1%) entered the psychosocial intervention on medication, 8 (8.6%) chose to discontinue medication use prior to treatment group assignment, and 4 (4.3%) withdrew from the study before psychosocial treatment started. Only 5% of children demonstrated a change in medication status between baseline and post intervention involving a shift from off to on medication or a change in medication.
Outcome Measures
Intervention acceptability
The Treatment Acceptability Questionnaire (TAQ), an 8-item measure, was used to evaluate treatment acceptability from parents’ perspectives. The TAQ has demonstrated sound psychometric properties (Krain et al., 2005), and the coefficient alpha for the TAQ in the present study was .91. The Intervention Rating Profile - 10 Item Version (IRP-10; Power, Hess, & Bennett, 1995) was used to examine teacher perceptions of intervention acceptability. This scale was adapted from a measure developed by Martens, Witt, Elliott, and Darveaux (1985) and demonstrated adequate reliability in the present study (alpha = .93). Finally, the Children’s Intervention Rating Profile (CIRP), a 7-item measure, was used to evaluate child perceptions of acceptability. This scale is commonly been used in research (Witt & Elliott, 1985) and had an alpha of .69 in this study.
Family involvement in education
Parental self-efficacy was assessed using a 10-item version of the Parent as Educator Scale (PES). This measure assesses the extent to which caregivers perceive themselves as effective in assisting with their child’s education. Each item is rated on a five-point scale (1 = strongly disagree to 5 = strongly agree). In a prior study, the reliability of this scale was found to be high (alpha = .89; Hoover-Dempsey et al., 1992), and in the present study sample, the coefficient alpha was .83.
In addition, the Parent-Teacher Involvement Questionnaire (PTIQ; Kohl, Lengua, McMahon, & Conduct Problems Prevention Research Group, 2000) was used to assess the quality of the family-school relationship from the perspective of parents and teachers. A factor analysis of this measure uncovered an 11-item Quality of Parent-Teacher Relationship factor consisting of parent- and teacher-reported items. As in previous studies, parent and teacher reports on items pertaining to this factor were aggregated into a composite score for purposes of data analysis. Reliability in the present sample was high (alpha = .88).
Homework performance
The Homework Problem Checklist (HPC; Anesko et al., 1987) was used to assess parent perceptions of homework performance. The HPC measures two factors: Inattention/Avoidance (e.g., child is distractible and procrastinates) and Poor Productivity and Nonadherence with Rules (e.g., child does not know assignments and does not return assignments to class), which have demonstrated adequate validity (Power, Werba, Watkins, Angelucci, & Eiraldi, 2006). Coefficient alphas in the current study sample were .88 for Inattention/Avoidance and .78 for Poor Productivity.
The Homework Performance Questionnaire-Teacher Version (HPQ-T; Power, Dombrowski, Watkins, Mautone, & Eagle, 2007) is a teacher-rated measure of homework. Teachers completed the Student Responsibility factor (i.e., students take materials home and return assignments on time). The alpha coefficient in the current sample was .91. Research supports the concurrent and discriminant validity of this measure for children with ADHD (Mautone, Marshall, Costigan, Clarke, & Power, in press).
Parent-child interaction
The Parent-Child Relationship Questionnaire (PCRQ) assessed parent perceptions of the parent-child relationship. The validity of the Positive Involvement (22 items) and Negative/Ineffective Discipline (12 items) factors have been supported in research conducted by Hinshaw et al. (2000). The alpha coefficients in the present study sample were .89 for Positive Involvement and .84 for Negative/Ineffective Discipline.
ADHD and ODD symptoms
The MTA SNAP-IV (Swanson et al., 2001), completed by parents and teachers, was used to assess ADHD and ODD. To obtain a unitary index of child symptoms, mean item score for the 26 ADHD and ODD items combined was used in analyses (see Swanson et al., 2001). The coefficient alphas in the present sample for parent and teacher ratings were .92 and .94, respectively.
Academic performance
The Academic Performance Rating Scale (APRS) is a teacher-rated questionnaire used to assess academic performance. It includes a 12-item subscale that assesses students’ productivity related to academic tasks (i.e., Academic Productivity). The psychometric properties of the APRS are acceptable (DuPaul et al., 1991), and the coefficient alpha for this subscale in the current sample was .86.
Assessment Procedures
Data were collected at baseline, mid-point, post-treatment, and 3-month follow-up by research assistants who were not involved in intervention implementation and who were blind to group assignment and intervention procedures. As indicated, about 40% of children in each group were on medication during each assessment period. Parent-report baseline measures were collected during the first intervention session. Mid-point measures were distributed to parents during session 6, and parents either completed the measures during a session break or were asked to return completed measures at session 7. Post-treatment ratings were obtained in person at the conclusion of the final session, and families were invited to attend a reunion visit 3 school months after the final intervention session for follow-up data collection. If the family was unable to attend the reunion meeting, measures were mailed to the family with a self-addressed, stamped return envelope. Parents received a $20 cash stipend for completing measures at each assessment period.
Teacher-report measures were collected during each of the data collection periods. Teachers received the measures in the mail approximately 1 week prior to the scheduled data collection period. Teachers received a $20 cash stipend for completing measures at each period.
Statistical Analyses
A linear mixed-effects regression model was utilized to analyze outcomes at post intervention and follow-up. The analyses were based on an intent-to-treat approach, whereby participants were analyzed as a function of the treatment group to which they were assigned and medication status at baseline. The amount of missing data was relatively low; 95% of cases were missing two units of data or less on outcome measures at baseline and post intervention.
The SAS Proc Mixed procedure was used with the following general linear model: Y = Treatment Group + Medication Status + Time + Treatment Group × Medication Status + Treatment Group × Time + Time × Medication Status + Treatment Group × time × Medication Status. In this model Y = score on outcome measure; Treatment Group = FSS or CARE; Medication Status = on medication or off medication at baseline; and Time = baseline, mid intervention (1.5 months), post intervention (3 months), and follow-up (6 school months). In these models, only intercepts were defined as a random effect. The hypotheses were tested separately for effects at post intervention and follow up. The Treatment Group × Time interaction effect indicated whether there was a significant effect of intervention over time. However, the three-way interaction of Group × Time × Medication Status was examined to determine whether the effect of intervention varied as a function of medication status. Prior to conducting statistical testing, the distributions of each outcome measure were carefully examined to determine whether assumptions of normality were met and whether significant data outliers were present. The distributions of the outcome measures met assumptions of normality. SAS software version 9.2 and SPSS software version 19 were utilized to conduct the analyses.
The analytic model was based on the assumption that each domain of measures was independent of another domain. For this reason, each domain (aim) was evaluated using a p value of .05. However, within each domain, because multiple measures were tested, the p value was adjusted using the Bonferroni procedure. For domains with of two measures (all but the Homework Performance), the p value was set at .025. For the Homework Performance domain, consisting of three measures, the p value was set at .0167. Effect sizes (ESs) were computed by calculating the difference in change scores for FSS versus CARE between post intervention (follow-up) and baseline and dividing this amount by the pooled standard deviation of the change scores for FSS and CARE. Confidence intervals for ESs were computed using procedures delineated by Odgaard and Fowler (2010).
Results
Characteristics of FSS and CARE Participants
The groups were compared on demographic variables, ADHD subtype status, and presence of comorbid conditions (see Table 2). The groups did not differ on any of these factors. Collapsing across groups, the mean grade level was 3.5. Thirty-two percent of participants were female, and 98% of families belonged to the three (of five) highest categories of the Hollingshead (1975) scale, reflecting that the sample was primarily in the middle and upper middle socioeconomic groups. With regard to ethnicity, 93% were non-Hispanic and 7% were Hispanic; with regard to race, 72% were White, 22% were Black/African American, 4% were multi-racial, and 2% were Asian. Children with ADHD, Inattentive Type comprised 52% of participants, and 48% had the Combined Type. The groups did not differ in ratings of ADHD severity. On the ADHD Rating Scale - IV, mean ratings were 85% for teacher-rated Inattention, 74% for teacher-rated Hyperactivity-Impulsivity, 95% for parent-rated Inattention, and 85% for parent-rated Hyperactivity-Impulsivity. The groups did not differ on WASI scores (M across groups = 105.9) or placement in special education (M across groups = 25%). Regarding comorbidities: 27% had a disruptive behavior disorder, 26% had learning disabilities, and 25% had a mood or anxiety disorder. Altogether, 43% of participants were on medication at baseline.
Table 2. Background Information About Participants in the FSS (n=100) and CARE (n=99) Groups.
|
|
|||
|---|---|---|---|
| FSS | CARE | Difference | |
| Gender (% female) | 33.0 | 30.3 | p=.761 |
| Grade level (M and SD)* | 3.5 (1.2) | 3.4 (1.2) | p=.602 |
| Single parent status (%) | 21.0 | 21.2 | p=1.000 |
| Hispanic (%) | 6.0 | 8.1 | p=.593 |
| Non-Hispanic (%) | 94.0 | 91.9 | — |
| African American (AA) (%) | 19.0 | 25.3 | p=.559 |
| White (%) | 74.0 | 70.7 | — |
| Asian (%) | 3.0 | 1.0 | — |
| Multiracial (%) | 4.0 | 3.0 | — |
| SES (% Levels III, IV, V on Hollingshead) | 98.0 | 98.0 | p=1.000 |
| Average percentage of students receiving subsidized lunch in the participating schools (M and SD)* |
20.7 (26.9) | 24.0 (31.2) | p=.436 |
| ADHD, Combined (%) | 45.0 | 51.5 | p=.396 |
| ADHD, Inattentive (%) | 55.0 | 48.5 | p=.396 |
| Learning disability status (% with LD) | 28.0 | 24.2 | p=.629 |
| Externalizing disorder (% with disorder) | 28.0 | 26.3 | p=.874 |
| Internalizing disorder (% with disorder) | 23.0 | 27.3 | p=.517 |
| Medication status at Baseline (% on medication) | 44.0 | 41.4 | p=.775 |
Note: SES refers to socioeconomic status, as assessed by the Hollingshead (1975) index of social status. Levels III, IV, and V reflect the middle to high levels of the scale. Subsidized lunch status refers to the average percentage of students who are eligible for free or reduced-price lunch across the schools represented in the FSS and CARE groups.
Independent samples t-tests were used to compute these comparisons. For all other comparisons, chi squared tests were used.
Treatment Acceptability
The hypothesis that FSS would be viewed as more acceptable than CARE was partially confirmed. On the parent-rated Treatment Acceptability Questionnaire (TAQ) mean item scores for FSS at post-treatment (M = 5.33, SD = 0.77) were significantly higher than scores for CARE (M = 4.98, SD = 0.92), t(179) = 2.79, p = .006, ES = 0.42. Given that mean item scores on the TAQ range up to 6.0, ratings for both groups reflected high levels of acceptability. On the teacher-rated Intervention Rating Profile (IRP), mean item scores for FSS at post-treatment (M = 4.96, SD = 1.02) were not significantly different from scores for CARE (M = 4.92, SD = 0.78). Mean item scores on the IRP, which range up to 6.0, were high for both groups. Mean item ratings for the Children’s Intervention Rating Profile, which range from 1.0 to 5.0, were high for both FSS (M = 4.48, SD = 0.62) and CARE (M = 4.47, SD = 0.56).
Overview of Outcome Findings
Means and standard deviations for each time point are presented in Table 3. There was a significant effect of Time on each measure at both post intervention and follow up; in all cases p < .05, but for a majority of measures p < .0001. There was a significant Group × Time effect on several measures; these results and associated effect sizes are presented in Table 4. The three-way interaction of Group × Medication Status × Time was significant only in two instances (out of 24). Only significant three-way interaction effects are described below.
Table 3. Means and standard deviations for primary outcomes across four data collection periods for FSS and CARE.
| FSS |
CARE |
|||||||
|---|---|---|---|---|---|---|---|---|
| Measure: |
Baseline M (SD) |
Midpoint M (SD) |
Post M (SD) |
Follow - up M (SD) |
Baseline M (SD) |
Midpoint M (SD) |
Post M (SD) |
Follow - up M (SD) |
| PES | 3.28 (0.62) | 3.68 (0.52) | 3.91 (0.52) | 3.88 (0.56) | 3.38 (0.57) | 3.63 (0.57) | 3.82 (0.46) | 3.89 (0.57) |
| PTIQ | 2.99 (0.57) | 3.06 (0.57) | 3.14 (0.58) | 3.15 (0.51) | 2.99 (0.59) | 3.08 (0.62) | 3.03 (0.63) | 3.04 (0.63) |
| HPC-IA | 2.04 (0.56) | 1.52 (0.56) | 1.18 (0.47) | 1.21 (0.56) | 2.09 (0.55) | 1.79 (0.67) | 1.51 (0.57) | 1.40 (0.60) |
| HPC-PP | 0.92 (0.51) | 0.64 (0.44) | 0.54 (0.42) | 0.55 (0.42) | 0.98 (0.54) | 0.73 (0.55) | 0.62 (0.39) | 0.64 (0.52) |
| HPQ-T | 2.77 (0.99) | 3.10 (0.73) | 3.09 (0.84) | 3.04 (0.86) | 2.80 (1.07) | 2.80 (1.08) | 2.85 (0.98) | 2.93 (1.08) |
| PCRQ - PI | 3.92 (0.44) | 3.96 (0.42) | 4.01 (0.41) | 4.02 (0.43) | 4.02 (0.40) | 4.03 (0.39) | 4.09 (0.36) | 4.11 (0.39) |
| PCRQ - N/ID | 2.93 (0.56) | 2.65 (0.50) | 2.41 (0.51) | 2.43 (0.57) | 2.95 (0.56) | 2.74 (0.59) | 2.71 (0.53) | 2.55 (0.59) |
| SNAP - P | 1.42 (0.55) | 1.22 (0.52) | 1.11 (0.53) | 0.96 (0.48) | 1.49 (0.51) | 1.31 (0.49) | 1.23 (0.47) | 1.13 (0.53) |
| SNAP - T | 1.18 (0.57) | 0.99 (0.54) | 1.04 (0.56) | 0.93 (0.59) | 1.15 (0.63) | 1.13 (0.66) | 1.09 (0.69) | 1.11 (0.79) |
| APRS | 3.07 (0.65) | 3.35 (0.63) | 3.32 (0.65) | 3.51 (0.64) | 3.08 (0.68) | 3.17 (0.77) | 3.20 (0.68) | 3.36 (0.76) |
Note. PES = parent as educator scale; PTIQ = parent-teacher involvement questionnaire; HPC-IA = Homework Problem Checklist, Inattention Avoidance factor; HPC-PP = Homework problem checklist, poor productivity factor; HPQ-T = homework performance questionnaire - teacher; PCRQ - PI = parent child relationship questionnaire - positive involvement; PCRQ - N/ID = parent child relationship questionnaire - negative/ineffective discipline; SNAP = Swanson, Nolan, and Pelham Questionnaire; APRS = Academic Performance Rating Scale
Table 4. Results of mixed effects analyses for the group x time interaction effects.
| Post Treatment | 3 Month Follow-Up | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
||||||||||
| Measure | df | F | p | ES* | ES:95% CI | df | F | p | ES* | ES: 95% CI |
| PES | ||||||||||
| Group X Time: | 1, 358 | 7.25 | .0074 | 0.37 | .07, .66 | 1, 521 | 2.9 | .0891 | 0.19 | −.12, .50 |
| PTIQ | ||||||||||
| Group X Time: | 1, 352 | 3.94 | .0478 | 0.29 | .00, .59 | 1, 507 | 6.34 | .0121 | 0.28 | −.03, .60 |
| HPC-IA | ||||||||||
| Group X Time: | 1, 359 | 15.40 | .0001 | 0.52 | .22, .81 | 1, 523 | 4.31 | .0384 | 0.19 | −.12, .50 |
| HPC-PP | ||||||||||
| Group X Time: | 1, 358 | 0.54 | .4633 | 0.06 | −.23, .35 | 1, 521 | 0.64 | .4230 | 0.05 | −.26, .35 |
| HPQ-T | ||||||||||
| Group X Time: | 1, 354 | 5.65 | .0180 | 0.34 | .05, .64 | 1, 525 | 1.01 | .3155 | 0.11 | −.19, .41 |
| PCRQ - PI | ||||||||||
| Group X Time: | 1, 352 | 0.06 | .8066 | 0.04 | −.25, .34 | 1, 513 | 0.01 | .9392 | 0.01 | −.31, .32 |
| PCRQ - N/ID | ||||||||||
| Group X Time: | 1, 352 | 17.27 | <.0001 | 0.59 | .29, .89 | 1, 513 | 10.70 | .0011 | 0.33 | .01, .64 |
| SNAP - P | ||||||||||
| Group X Time: | 1, 352 | 1.66 | .1984 | 0.16 | −.14, .45 | 1, 515 | 4.08 | .0439 | 0.19 | −.12, .50 |
| SNAP - T | ||||||||||
| Group X Time: | 1, 355 | 0.6 | .4384 | 0.07 | −.22, .37 | 1, 520 | 2.46 | .1171 | 0.20 | −.11, .50 |
| APRS | ||||||||||
| Group X Time: | 1, 352 | 3.49 | .0625 | 0.24 | −.06, .54 | 1, 522 | 2.75 | .0981 | 0.25 | −.05, .56 |
Note. ES = Effect size; PES = parent as educator scale; PTIQ = parent-teacher involvement questionnaire; HPC-IA = Homework Problem Checklist, Inattention Avoidance factor; HPC-PP = Homework Problem Checklist, Poor Productivity factor; HPQ-T = Homework Performance Questionnaire - Teacher; PCRQ - PI = Parent-Child Relationship Questionnaire - Positive Involvement; PCRQ - N/ID = Parent-Child Relationship Questionnaire - Negative/Ineffective Discipline; SNAP = Swanson, Nolan, and Pelham Questionnaire; APRS = Academic Performance Rating Scale.
ES were computed by comparing change scores between groups and dividing by the pooled standard deviation of change scores.
Parent Involvement in Education
At post intervention, the Group × Time interaction effect was significant for the Parent as Educator Scale (PES), ES = 0.37, indicating that FSS was superior to CARE. At follow up, there was a significant three-way interaction effect for Group × Time × Med Status on the PES. A post hoc covariate analysis was conducted, controlling for baseline scores, to determine whether there were differences between FSS and CARE in the subgroups who were medicated as well as those who were unmedicated. Neither of these contrasts was significant (p > .05), suggesting an attenuation of treatment effects on the PES at follow up.
At post intervention, differences between FSS and CARE on ratings of the quality of the parent-teacher relationship, assessed using the Parent-Teacher Involvement Questionnaire (PTIQ), failed to achieve significance using the adjusted p value. However, at follow up FSS was superior to CARE on the PTIQ (ES = 0.28).
Homework Performance
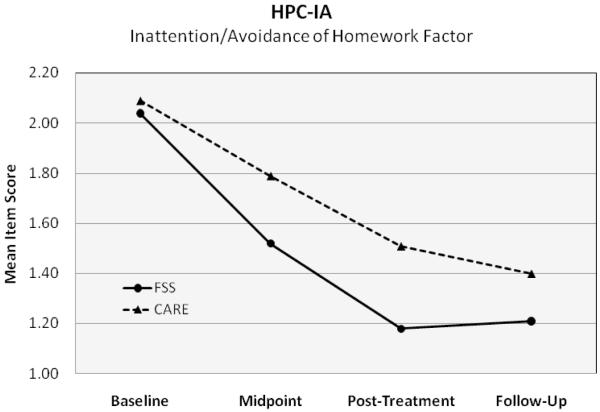
Based on parent ratings on the HPC, at post intervention children in FSS showed a significantly greater decrease in homework inattention/task avoidance (Factor I) than did their counterparts in the CARE condition (ES = 0.52), but this effect dissipated at follow up. Figure 2 depicts the change over time on Factor I of the HPC, showing the partial attenuation of the effect at the follow-up point. An intervention effect was not observed for parent ratings of poor productivity/nonadherence of the HPC (Factor II) at post intervention. Also, the difference between groups failed to reach significance using the corrected p value for student responsibility (Factor I) of the teacher-rated Homework Performance Questionnaire (HPQ).
Figure 2.
Improvement in parent ratings on Factor I (Inattention/Avoidance of Homework) of the Homework Problem Checklist (HPC). Points along each line represent the average of participants’ mean item scores on Factor I at each data collection period. Midpoint data collection occurred at Session 6 (1.5 months), Post-Treatment at Session 12 (3 months), and Follow-Up at 3 academic months after Session 12. FSS = Family-School Success. CARE = Coping with ADHD through Relationships and Education.
At follow up, there was a significant interaction of Group × Time × Med Status for Factor II of the HPC (Poor Productivity/Non-adherence). A subsequent covariate analysis controlling for baseline scores was conducted to determine whether there was a difference between FSS and CARE in the subgroups who were medicated as well as those who were unmedicated. Among children who were medicated, those receiving FSS performed better on Factor II of the HPC than those in CARE (ES = 0.56). There was no difference between FSS and CARE on this factor for the unmedicated group (p > .05).
Parent-Child Interaction
At post intervention, children in FSS demonstrated a significantly greater decrease in parent ratings of negative/ineffective discipline, as assessed by Factor II of the Parent-Child Relationship Questionnaire (PCRQ), than their counterparts in CARE (ES = 0.59), and this effect was maintained at follow up (ES = 0.33). An intervention effect was not observed for parent ratings of positive involvement (Factor I of the PCRQ).
ADHD and ODD Symptoms and Academic Performance
There was no intervention effect on ADHD and ODD symptoms, as assessed by parent and teacher ratings on the SNAP-IV. Also, the intervention did not have an effect on academic performance, as assessed by the teacher-rated Academic Performance Rating Scale.
Discussion
This study provides evidence of the effectiveness of FSS, a relatively brief behavioral intervention that promotes family involvement in education and family-school collaboration. FSS was shown to have a significant effect in the small to moderate range on family involvement in education, the quality of the family-school relationship, homework performance, and parenting behavior. The superiority of FSS was demonstrated even though about 40% of the participants in FSS and CARE were on an optimal dose of medication, and there was a significant effect of Time on all measures. This study replicates numerous investigations showing that behavioral interventions for children with ADHD are effective (e.g., Fabiano et al., 2009). Further, this study demonstrates that FSS is a highly acceptable approach to treatment.
This study demonstrated the effectiveness of a behavioral intervention designed to improve child functioning at both home and school. Like the MTA study, a significant improvement in homework performance and a reduction in negative/ineffective parenting were demonstrated at post intervention (Langberg, et al., 2010; Wells, Epstein, et al., 2000). In addition, similar to the MTA, the effects of intervention were demonstrated primarily in areas of functional impairment as opposed to DSM-IV symptoms pertaining to ADHD and ODD.
This study extends the findings of previous studies in numerous ways. First, this study is the first to demonstrate that a family-school intervention for children with ADHD can improve the quality of the parent-teacher relationship. Given the importance of the family-school relationship and the potential impact this relationship can have on student academic and social functioning (Christenson & Sheridan, 2001), improving this interaction may have considerable educational significance. Second, FSS was able to achieve effect sizes of comparable magnitude to those found in the MTA on variables related to homework performance and parenting behavior using a relatively brief intervention that is likely to be feasible for schools and clinics to implement. Third, unlike most previous studies, this investigation employed a comparison group (CARE) that provided a control for the non-specific effects of treatment. Even though families were highly engaged in CARE and viewed it as highly acceptable, FSS was perceived by parents to be more acceptable, and FSS was more effective than CARE on several measures. Further, in this study families had the choice of having children on medication while they were receiving the psychosocial interventions. In this sense, the present study was conducted under conditions similar to clinical practice. Nonetheless, there was a high level of control for medication status; a low percentage of children (5%) demonstrated a change in medication status during treatment.
Although FSS achieved more favorable outcomes than CARE on several measures, the majority of between-groups comparisons did not reveal significant treatment effects. The emergence of additional treatment effects might have been attenuated by the strong Time effect observed across measures (mean ES for the Time effect across measures was 0.59 at post intervention and 0.59 at follow up). However, given that the study did not include a no-treatment control group, it was not possible to determine the extent to which the Time effect reflected improvements as a function of both FSS and CARE, as opposed to methodological factors (e.g., regression to mean, effects of history).
Although FSS demonstrated effects on homework performance, the findings were somewhat variable and teachers did not report a significant effect using the corrected p value. To further improve the effects of FSS on homework performance, additional treatment components may be needed. For example, recent studies have demonstrated the benefits of using behavioral strategies to improve the ability of students to organize homework planners and assignment binders (Langberg, Epstein, Urbanowicz, Simon, & Graham, 2008). The homework interventions used in the present study (i.e., using a homework book, following a homework routine, using a goal setting and time management strategy) did not target organizational skills in the classroom that could have an effect on homework performance. Although studies targeting organizational strategies generally have focused on students who were a little older than those in the current study, the intervention strategies likely can be adapted for use with younger students.
In this study the effectiveness of FSS generally did not vary as a function of whether children were on medication during behavioral treatment. The effect of FSS was essentially the same when children were medicated as when they were not. In contrast to other studies, behavioral intervention was examined in the context of a design in which families had a choice about medication. Although research has demonstrated some advantages of combined treatment over medication only and behavioral treatment over treatment as usual (e.g., Conners et al., 2001), previous research has not been clear about whether there is a differential response to behavioral treatment (in relation to a control group) based upon whether children are medicated using an optimal dose. Additional research is needed to examine the potential for medication to exert a moderating influence on response to behavioral treatment.
The rates of medication usage in this study are lower than those found in many clinical practices. At the outset of the study when parents were given the choice of a medication trial, only 55% of them selected the trial knowing that it did not commit them to actually prescribing medication to their child. Parents knew that the study would provide them with a psychosocial intervention, and this factor likely reduced the rate of medication selection. In many clinical practices, psychosocial interventions are often not available or are difficult to access, which may contribute to higher rates of selection of medication as a treatment option.
Several limitations should be noted. First, families participating in this study generally were highly motivated. For the most part, families were self-referrals to the study or our ADHD clinic. Further, families who were randomly assigned to treatment arms consisted of those who followed through with recruitment procedures by returning questionnaires, completing a diagnostic evaluation, and completing a medication trial when indicated. Families who are difficult to engage in treatment are likely to be underrepresented in this study.
Second, baseline levels of ADHD and ODD symptoms for participants in this study were lower than those assessed in the MTA study (mean item ratings were 0.3 lower for parent ratings, and 0.7 lower for teacher ratings). The lower level of severity may have been due in part to the fact that about 40% of children in each group were on medication at baseline. Also, children in this study included those with both the Combined and Inattentive subtypes of ADHD, whereas those in the MTA included only those with the Combined Type. It is possible that the sample in the present study was not as impaired as children in the MTA. Third, a high percentage of children on medication in this study were prescribed a long-acting stimulant or atomoxetine. Nonetheless, for many children the effects of medication may have abated by the time they were expected to complete homework. This factor may have contributed to the relatively low rates of medicated children who were normalized on the HPC after the medication trial (about 20%). Fourth, as indicated, children who received a medication trial and were normalized on the HPC were not assigned to the study interventions. As such, study findings do not pertain to those families who elect a medication trial and whose child demonstrates a normalization of homework performance according to parent ratings.
Fifth, this study was conducted primarily in a clinic setting. There are clear advantages to offering this treatment in schools with regard to improving access to care and affording opportunities for classroom interventions. It is strongly recommended that this intervention be adapted for use in school settings, so that both school- and clinic-based options are available. Sixth, this study was conducted with students in grades 2 to 6. The findings of this study are generalizable primarily to students in this grade range. Family-school interventions have been developed and tested for children below grade 2 (e.g., Kern et al., 2007). However, there is a dearth of research on family-school interventions for students in secondary school. Seventh, there were differences between FSS and CARE with regard to the experience level of the interventionists. However, it should be noted that in general CARE clinicians were somewhat more experienced than FSS providers, so any bias operating should have influenced the findings in favor of accepting the null hypothesis of no group differences.
In addition, this study examined follow-up effects only at 3 months after intervention. It is important to investigate longer term effects, as well as to explore the potential benefits of booster sessions. Further, outcome measures were assessed using parent and teacher reports. A limitation is that measures of primary outcome variables were not assessed using observational procedures and naturalistic measures (e.g., academic grades). Finally, data with regard to medication adherence were not collected systematically in this study, so the effect of medication adherence on outcomes could not be examined.
In conclusion, this study provided evidence of the effectiveness of FSS. Even though about 40% of children in each group were on medication and there were significant effects of Time on each measure, FSS was superior to the control group on measures of family involvement in education, the family-school relationship, homework performance, and parenting behavior. This study affirms the important role that parents can serve in improving variables related to student success in school. The effects of FSS were similar for children on and off medication. Additional research is needed to examine the effectiveness of an adapted version of FSS in clinic and school settings with families from a broad range of backgrounds.
Acknowledgments
This study was supported by research grant R01MH068290 funded by the National Institute of Mental Health and the Department of Education awarded to the first author. The authors wish to thank the participating families and schools as well as the clinicians and research assistants involved in the project, including Lisa Marie Angello, Michael Cassano, Terri Gaier, Rebecca Gullan, Heather Jones, Mia Khera, Elizabeth Lefler, Jennelle Nissley-Tsiopinis, Mark Scuitto, Katy Tresco, Maren Watkins, Jennifer Brereton, Elizabeth Gallini, Shawn Gilroy, Margaret Howley, Lauren Lee, Jessica Gresko, Brittany Lyman, Celeste Malone, Sean O’Dell, Lynn Panepinto, and Lauren Wilson.
References
- Abikoff H, Hechtman L, Klein RG, Gallagher R, Fleiss K, Etcovitch J, Pollack S. Social functioning in children with ADHD treated with long-term methylphenidate and multimodal psychosocial treatment. Journal of the American Academy of Child and Adolescent Psychiatry. 2004;43:820–829. doi: 10.1097/01.chi.0000128797.91601.1a. [DOI] [PubMed] [Google Scholar]
- Ambrosini PJ. Historical development and present status of the Schedule for Affective Disorders and Schizophrenia for School-age Children (K-SADS) Journal of the American Academy of Child and Adolescent Psychiatry. 2000;39:49–58. doi: 10.1097/00004583-200001000-00016. [DOI] [PubMed] [Google Scholar]
- Anesko KM, Schoiock G, Ramirez R, Levine FM. The Homework Problem Checklist: Assessing children’s homework difficulties. Behavioral Assess. 1987;9:179–185. [Google Scholar]
- Barkley RA. Attention deficit hyperactivity disorder: A handbook for diagnosis and treatment. 2nd ed. Guilford Press; New York: 1998. [Google Scholar]
- Christenson SL, Sheridan SM. Schools and families: Creating essential connections for learning. Guilford Press; New York: 2001. [Google Scholar]
- DuPaul GJ, Power TJ, Anastopoulos AD, Reid R. The ADHD Rating Scale - IV: Checklists, norms, and clinical interpretation. Guilford Press; New York: 1998. [Google Scholar]
- DuPaul GJ, Rapport MD, Perriello LM. Teacher ratings of academic skills: The development of Academic Performance Rating Scale. School Psychol. Rev. 1991;20:284–300. [Google Scholar]
- DuPaul GJ, Stoner G. ADHD in the schools: Assessment and intervention strategies. 2nd ed. Guilford Press; New York: 2003. [Google Scholar]
- Fabiano GA, Pelham WE, Jr., Coles EK, Gnagy EM, Chronis-Tuscano A, O’Connor BC. A meta-analysis of behavioral treatments for attention-deficit/hyperactivity disorder. Clinical Psychology Review. 2009;29(2):129–140. doi: 10.1016/j.cpr.2008.11.001. doi: 10.1016/j.cpr.2008.11.001. [DOI] [PubMed] [Google Scholar]
- Fantuzzo J, Tighe E, Childs S. Family Involvement Questionnaire: A multivariate assessment of family participation in early childhood education. Journal of Educational Psychology. 2000;92:367–376. [Google Scholar]
- Hinshaw SP, Owens EB, Wells KC, Kraemer HC, Abikoff HB, Arnold E, Wigal T. Family processes and treatment outcome in the MTA: Negative/ineffective parenting practices in relation to multimodal treatment. Journal of Abnormal Child Psychology. 2000;28:555–568. doi: 10.1023/a:1005183115230. [DOI] [PubMed] [Google Scholar]
- Hollingshead AB. Four factor index of social status. Yale University; New Haven, CT: 1975. [Google Scholar]
- Hoover-Dempsey KV, Bassler OC, Brissie JS. Explorations in parent-school relations. Journal of Educational Research. 1992;85:287–294. [Google Scholar]
- Kahle AL, Kelley ML. Children’s homework problems: A comparison of goal setting and parent training. Behavior Therapy. 1994;25:275–290. [Google Scholar]
- Kohl GO, Lengua LJ, McMahon RJ, Conduct Problems Prevention Research Group Parent involvement in school: Conceptualizing multiple dimensions and their relations with family demographic risk factors. Journal of School Psychol. 2000;38:501–524. doi: 10.1016/S0022-4405(00)00050-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krain AL, Kendall PC, Power TJ. The role of treatment acceptability in the initiation of treatment for ADHD. Journal of Attention Disorders. 2005;9:425–434. doi: 10.1177/1087054705279996. [DOI] [PubMed] [Google Scholar]
- Langberg JM, Arnold LE, Flowers AM, Epstein JN, Altaye M, Hinshaw SP, Jensen PS. Parent-reported homework problems in the MTA study: Evidence for sustained improvement with behavioral treatment. Journal of Clinical Child & Adolescent Psychology. 2010;39:220–233. doi: 10.1080/15374410903532700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Langberg JM, Epstein JN, Urbanowicz CM, Simon JO, Graham AJ. Efficacy of organization skills intervention to improve academic functioning of students with attention-deficit/hyperactivity disorder. School Psychology Quarterly. 2008;23:407–417. [Google Scholar]
- Martens B, Witt J, Elliott S, Darveaux D. Teacher judgments concerning the acceptability of school-based interventions. Professional psychology: Research and practice. 1985;16:191–198. [Google Scholar]
- Mautone JA, Marshall SA, Costigan TE, Clarke AT, Power TJ. Multidimensional assessment of homework: An analysis of students with ADHD. Journal of Attention Disorders. doi: 10.1177/1087054711416795. in press. [DOI] [PubMed] [Google Scholar]
- MTA Cooperative Group A 14-month randomized clinical trial of treatment strategies for attention-deficit hyperactivity disorder. Archives of General Psychiat. 1999;56:1073–1086. doi: 10.1001/archpsyc.56.12.1073. [DOI] [PubMed] [Google Scholar]
- Odgaard EC, Fowler RL. Confidence intervals for effect sizes: Compliance and clinical significance in the Journal of Consulting and Clinical Psychology. Journal of Consulting and Clinical Psychology. 2010;78:287–297. doi: 10.1037/a0019294. [DOI] [PubMed] [Google Scholar]
- Owens JS, Murphy CE, Richerson L, Girio EL, Himawan LK. Science to practice in underserved communities: The effectiveness of school mental health programming. Journal of Clinical Child & Adolescent Psychology. 2008;37:434–447. doi: 10.1080/15374410801955912. [DOI] [PubMed] [Google Scholar]
- Pfiffner LJ, Mikami AY, Huang-Pollock C, Easterlin B, Zalecki C, McBurnett K. A randomized, controlled trial of integrated home-school behavioral treatment for ADHD, Predominantly Inattentive Type. Journal of the American Academy of Child & Adolescent Psychiatry. 2007;46:1041–1050. doi: 10.1097/chi.0b013e318064675f. [DOI] [PubMed] [Google Scholar]
- Pianta RC. Adult-child relationship processes and early schooling. Early Education and Development. 1997;8:11–26. [Google Scholar]
- Pliszka SR, Crismon ML, Hughes CW, Conners CK, Emslie GJ, Jensen PS, Lopez M. The Texas children’s medication algorithm project: Revision of the algorithm for pharmacotherapy of attention-deficit/hyperactivity disorder. Journal of the American Academy of Child and Adolescent Psychiatry. 2006;45:642–657. doi: 10.1097/01.chi.0000215326.51175.eb. [DOI] [PubMed] [Google Scholar]
- Power TJ, Hess L, Bennett D. The acceptability of interventions for ADHD among elementary and middle school teachers. Journal of Developmental and Behavioral Pediatrics. 1995;16:238–243. [PubMed] [Google Scholar]
- Power TJ, Karustis JL, Habboushe DF. Homework success for children with ADHD: A family-school intervention program. Guilford Press; New York: 2001. [Google Scholar]
- Power TJ, Dombrowski SC, Watkins MW, Mautone JA, Eagle JW. Assessing children’s homework performance: Development of multi-dimensional, multi-informant rating scale. Journal of School Psychology. 2007;45:333–348. doi: 10.1016/j.jsp.2007.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Power TJ, Werba BE, Watkins MW, Angelucci JG, Eiraldi RB. Patterns of homework problems among ADHD-referred and non-referred children. School Psychology Quarterly. 2006;21:13–33. [Google Scholar]
- Psychological Corporation . Wechsler Abbreviated Scale of Intelligence (WASI) Author; San Antonio, TX: 1999. [Google Scholar]
- Reynolds CR, Kamphaus RW. BASC-2: Behavior Assessment System for Children. Second Edition AGS Publishing; Circle Pines, MN: 2004. [Google Scholar]
- Rogers MA, Wiener J, Marton I, Tannock R. Parental involvement in children’s learning: Comparing parents of children with and without attention-deficit/hyperactivity disorder (ADHD) Journal of School Psychology. 2009;47:167–185. doi: 10.1016/j.jsp.2009.02.001. [DOI] [PubMed] [Google Scholar]
- Sheridan SM, Eagle JW, Cowan RJ, Mickelson W. The effects of conjoint behavioral consultation: Results of a 4-year investigation. Journal of School Psychology. 2001;39:361–388. [Google Scholar]
- Sheridan SM, Kratochwill TR. Conjoint behavioral consultation: Promoting family-school connections and interventions. 2nd ed. Springer; New York: 2008. [Google Scholar]
- Soffer SL, Power TJ. Treatment manual for Family-School Success: A family-school intervention program for children with ADHD in grades 2 to 6. The Children’s Hospital of Philadelphia; Pennsylvania: 2005a. Unpublished manual, Department of Child and Adolescent Psychiatry and Behavioral Sciences. [Google Scholar]
- Soffer SL, Power TJ. Treatment manual for Coping with ADHD through relationships and education (CARE): A family intervention for children with ADHD in grades 2 to 6. The Children’s Hospital of Philadelphia; Pennsylvania: 2005b. Unpublished manual, Department of Child and Adolescent Psychiatry and Behavioral Sciences. [Google Scholar]
- Swanson JM, Kraemer HC, Hinshaw SP, Arnold LE, Conners CK, Abikoff HB. Clinical relevance of the primary findings of the MTA: Success rates based on severity of ADHD and ODD symptoms at the end of treatment. American Academy of Child and Adolescent Psychiatry. 2001;40:168–179. doi: 10.1097/00004583-200102000-00011. [DOI] [PubMed] [Google Scholar]
- Vannest KJ, Davis JL, Davis CR, Mason BA, Burke MD. Effective intervention for behavior with a daily behavior report card: A meta-analysis. School Psychology Review. 2010;39(4):654–672. [Google Scholar]
- Wells KC, Pelham WE, Kotkin RA, Hoza B, Abikoff HB, Abramowitz A, Schiller E. Psychosocial treatment strategies in the MTA Study: Rationale, methods, and critical issues in design and implementation. Journal of Abnormal Child Psychology. 2000;28:483–506. doi: 10.1023/a:1005174913412. [DOI] [PubMed] [Google Scholar]
- Wells KC, Epstein JN, Hinshaw SP, Conners CK, Klaric J, Abikoff HB, Wigal T. Parenting and family stress treatment outcomes in attention deficit hyperactivity disorder (ADHD). An empirical analysis in the MTA study. Journal of Abnormal Child Psychology. 2000;28:543–553. doi: 10.1023/a:1005131131159. [DOI] [PubMed] [Google Scholar]
- Witt JC, Elliott SN. Acceptability of classroom intervention strategies. In: Kratochwill TR, editor. Advances in School Psychology. Vol. 4. Lawrence Erlbaum; Hillsdale, NJ: 1985. pp. 251–288. [Google Scholar]