Abstract
PURPOSE
In recognition of the impact of chronic diseases on mental health and the lack of research on Asian American subgroups, the present study examined subjective perceptions of health as a potential mediator in the association between diabetes and depressive symptoms in Korean American older adults.
METHODS
Multivariate analysis with data from 672 Korean American older adults in Florida explored the mediation model of health perceptions.
RESULTS
The presence of diabetes was associated with negative perceptions of health and elevated symptoms of depression. The proposed mediation model was also supported: negative perceptions of health served as an intervening step between diabetes and depressive symptoms.
CONCLUSIONS
The intervening role of health perceptions yields implications for developing health promotion interventions targeting older individuals with diabetes. Results suggest that even in the presence of chronic health conditions, mental well-being of older adults can be maintained by having optimistic beliefs and positive attitudes towards their own health.
Keywords: Diabetes, Depressive symptoms, Korean American older adults
Diabetes, one of the most common chronic diseases in older populations, is known to increase morbidity, mortality, and health care expenditure (1–3). The estimated prevalence of diabetes among older populations in the United States range from 15% to 23.5%, and this figure is expected to grow (4–6). It is notable that the annual health care cost among people with diabetes is more than twice higher than it would be in the absence of this condition (1). Given its projected increase in prevalence and burden in health care, diabetes has been portrayed as the most important epidemic of the 21st century (3).
Previous studies report a close connection between diabetes and depression (7,8). It is estimated that 11% to 31% of patients with diabetes manifest symptom profiles commensurate with a clinical diagnosis of depression (9). Moreover, prospective studies demonstrate that the comorbidity of depression may adversely affect the way people deal with their diabetes and has unfavorable consequences for other health outcomes and overall quality of life (10,11).
In the present study, we considered diabetes as a potential risk to mental health and explored a mediating factor in the relation between diabetes and depressive symptoms. Previous research has focused on behavioral and clinical factors as potential mediators (12,13). For example, Chou and Chi suggest (12) that diabetes-related complications such as heart disease, high blood pressure, stroke, and vision problems mediate the association between diabetes and depression.
However, the current study shifts the focus to the psychological realm: to the subjective perception of one's own health as a potential mediator. The orientation follows from studies suggesting that the adverse impact of physical morbidities may not only erode mental health but also prime people to harbor negative self-evaluation of health (14–18). Such findings suggest that subjective perception of health may serve as an intervening step between physical and mental health. In research on diabetics, health perception has been considered as an important psychosocial attribute (19,20); however, no study has conceptualized it as a mediator in the relation between diabetes and depressive symptoms. Assessment of the mediating role of health perceptions may help us better understand psychological mechanisms associated with chronic diseases and shed light on intervention strategies for chronic health management and health promotion.
Our choice of target population for the study is also intended to expand the knowledge base. It is widely known that diabetes is more common in Blacks and Hispanics than non-Hispanic Whites (3), but little is known about Asian Americans. It is notable that despite their low rates of obesity, Asian Americans have increased susceptibility to diabetes (21,22). This susceptibility has been attributed to a genetic predisposition towards high central adiposity (22). Given the heterogeneity of Asian Americans, the present study focused on one subgroup: Korean American older adults. Previous studies report the latter group's vulnerability to physical and mental health problems (21,23), prompting the need to more adequately address their health needs. Based on the aforementioned review, the current study explored (1) the relation between diabetes and depressive symptoms and (2) the mediating role of health perceptions in the relation between diabetes and depressive symptoms. Potential confounding variables including demographic information, medical comorbidity, and functional disability were controlled for the analysis.
Methods
Sample
After approval from the researcher's Institutional Review Board, surveys with community-dwelling Korean American older adults (aged 60 or older) were conducted from March to August 2008 in the Tampa and Orlando areas. The sources included local Korean churches, other religious groups, senior centers, elder associations, and a directory of Korean residents in Florida. The survey questionnaire was originally drafted in English; a Korean version was then developed using a back-translation method with reconciliation. In places where visits were made, surveys were self-administered but with trained Korean-speaking interviewers available for those needing assistance. For those who were recruited through means other than visits (e.g., via calling individuals listed in the directory of Korean residents and self-referrals), a mail survey approach was used. The resulting sample included 675 participants. Of the sample, 73% was recruited through visits and about 27% through mail surveys. We conducted a series of comparative analyses to check whether there was any difference in sample characteristics by recruitment method. No significant difference was found for the major study variables including health perceptions and depressive symptoms; however, compared to the individuals whose data were collected through mail surveys, participants recruited through visits were less educated (χ2= 10.3, p < .01). This finding suggests that a sole reliance on mail surveys would have excluded individuals with lower levels of education. Detailed information on sampling procedures and validation of the strategy of using multiple methods for recruitment is available elsewhere (24). After removing individuals who had more than 10% of missing information in their responses, the final sample consisted of 672 participants.
Measures
Diabetes
Diagnosed diabetes was assessed by asking participants if their medical doctor had informed them that they had diabetes. Responses were coded `yes' or `no'. Classification of diabetes into Type 1 or 2 was not assessed.
Medical comorbidity
Similarly, the presence of other medical conditions was assessed with an inventory of chronic diseases and conditions commonly found among older populations. The list included heart disease, liver disease, problems with digestive systems, arthritis, kidney disease, stroke, high blood pressure, and cancer. Each condition was coded using a yes/no format, and a summated score was used for the analysis.
Functional disability
Functional status was assessed with a composite measure of the Physical Activities of Daily Living (PADL; 25), Instrumental Activities of Daily Living (IADL; 25), Physical Performance Scale (26), and Functional Health Scale (27). The twenty items covered a wide range of activities including eating, dressing, traveling, managing money, carrying a bag of groceries, and ability to reach above the head with one's arms. Participants were asked whether they could perform each activity, and response was coded as 0 (without help), 1 (with some help) or 2 (unable to do). Total scores could range from 0 (no disability) to 40 (severe disability). Internal consistency for the measure in the present sample was .94.
Health perceptions
Subjective perception of health was measured with three items; “How would you rate your overall health at the present time?” “How is your present health compared to five years ago?” and “How much do your health troubles stand in the way of your doing the things you want to do?” The items form a subscale of the Older Americans Resources and Services (OARS; 25) questionnaire designed to assess individuals' subjective perceptions of their own health status. The summated scores could range from 3 to 10, higher scores indicating more negative health perceptions. Internal consistency of the scale in the present sample was .72.
Depressive symptoms
The Geriatric Depression Scale-Short Form (GDS-SF; 28) includes 15 items (e.g., “Are you satisfied with your life?”, “Do you feel happy?”, “Do you feel that your life is empty?” and “Do you feel helpless?”) with a yes/no response format. The total score was calculated by counting the number of endorsed symptoms of depression. The totals could range from 0 (no depressive symptoms) to 15 (severe depressive symptoms). The GDS-SF has been translated into Korean, and its psychometric properties have been validated (29,30). Internal consistency of the GDS-SF in the present sample was .82.
Demographic variables
Demographic information included age (in years), gender (1 = male, 2 = female), marital status (1 = married, 2 = not married), educational attainment (1 = < high school, 2 = ≥ high school), and perceived financial status (1 = below average, 2 = average, and 3 = above average). Given that all participants were immigrants, each was asked how long they had lived in the United States, with responses coded in years.
Analytic Strategy
In addition to descriptive and correlational analyses, hierarchical regression models of health perception and depressive symptoms were tested by entering independent blocks of predictors with (1) diabetes, (2) demographics (age, gender, marital status, education, and perceived financial status) and length of stay in the U.S.), and (3) health-related variables (medical comorbidity and functional disability). For the regression model for depressive symptoms, health perception was added as a potential predictor in the final step. Intercorrelations among study variables and variance inflation factors (VIF) were assessed to determine multicollinearity.
The mediating role of health perception was assessed with a series of regression analyses following Baron and Kenny's criteria for mediation (31): (a) there is a significant association between independent and dependent variables, (b) there is a significant association between independent variable and presumed mediator, (c) there is a significant association between presumed mediator and dependent variable, and (d) the link between independent and dependent variables should become non-significant or decrease when the mediator is controlled for. The Sobel test was used to assess the significance of any reduction in regression coefficients resulting from mediation (32).
Results
Descriptive Information of the Sample
Of the 672 participants, approximately 20% reported that they had diabetes. Table 1 presents comparative analysis between the individuals with diabetes (n = 133) and those without diabetes (n = 539). The two groups were quite similar in age, gender, marital status, perceived financial status, and length of stay in the United States, but those with diabetes were less likely to be educated and had more negative health profiles. For example, compared with their counterparts without diabetes, they had more medical comorbidity, greater functional disability, more negative perceptions of health and higher levels of depressive symptoms. The mean difference in the GDS-SF was small but significant. It is notable that 33% of the group with diabetes fell into the category of probable depression (GDS-SF scores greater than 5) whereas the corresponding figure in the group without diabetes was 20% (χ2 = 7.56, p < .005).
Table 1.
Descriptive Characteristics of the Sample (n = 672)
|
M ± SD (range) or % |
|||
|---|---|---|---|
| Variable | Individuals with diabetes (n = 133) | Individuals without diabetes (n = 539) | t (χ2) |
| Age | 71.2 ± 6.49 (60–91) | 70.6 ± 7.36 (60–98) | −1.22 |
| Gender (female) | 55.2 | 56.1 | (.06) |
| Marital status (not married) | 32.9 | 28.5 | (1.65) |
| Education (≥ high school) | 64.5 | 71.5 | (4.27*) |
| Perceived financial status (below average) | 20.5 | 18.2 | (.36) |
| Length of stay in the U.S. | 26.4 ± 10.7 (1–50) | 26.4 ± 11.4 (1–54) | .02 |
| Medical comorbidity | 1.67 ± 1.34 (0–8) | 1.18 ± 1.10 (0–6) | −5.59*** |
| Functional disability | 2.95 ± 5.96 (0–36) | 1.78 ± 4.34 (0–40) | −3.30** |
| Health perceptions | 7.23 ± 1.69 (4–11) | 6.31 ± 1.70 (3–11) | −7.30*** |
| Depressive symptoms | 4.80 ± 3.81 (0–15) | 4.05 ± 3.52 (0–15) | −2.70** |
p < .05,
p < .01,
p < .001
Hierarchical Models of Health Perceptions and Depressive Symptoms
Prior to multivariate analyses, bivariate correlations among all study variables were assessed. The variables were associated in expected directions, and all coefficients were below .46. The variance inflation factors in all regression models were below 1.52, indicating a lack of multicollinearity. Table 2 summarizes the results of hierarchical regression models for health perceptions and depressive symptoms. In the initial model (model 1), the presence of diabetes was significantly associated with negative perceptions of health. With the subsequent entry of demographic variables (model 2) and health-related variables (model 3), the predictability of diabetes became gradually reduced but remained significant. Each model contributed significant level of variance of health perceptions. In the final model, individuals who had diabetes, lower financial status, shorter stay in the U.S., more medical comorbidity and greater functional disability were more likely to report negative perceptions of health. In the initial model of depressive symptoms (model 1), the presence of diabetes significantly increased symptoms of depression. With the subsequent entry of demographic variables (model 2) and health-related variables (model 3), the predictability of diabetes again became reduced but remained significant until the entry of health perceptions (model 4), at which point of the influence of diabetes became non-significant. Each model made a significant contribution to accounting for variance of depressive symptoms. In the final model, individuals who were younger and not married, had greater functional disability, and reported more negative health perceptions were likely to have greater levels of depressive symptoms.
Table 2.
Hierarchical Regression Models of Health Perceptions and Depressive Symptoms
| Health perceptions, B (SE) |
Depressive symptoms, B (SE) |
||||||
|---|---|---|---|---|---|---|---|
| Predictor | Model 1 | Model 2 | Model 3 | Model 1 | Model 2 | Model 3 | Model 4 |
| Diabetes | .98 (.16)*** | .94 (.15)*** | .58(.14)*** | 1.00(.32)** | .90(.31)** | .67(.30)* | .29(.30) |
| Age | .02 (.01) | −.01(.01) | .00(.01) | −.05(.02)* | −.04(.01)* | ||
| Gender | .43 (.13)** | .23 (.12) | .17(.27) | −.16(.26) | −.31(.25) | ||
| Marital status | .22 (.16) | .17(.14) | 1.04(.33)** | 1.02(.31)** | .90(.30)** | ||
| Education | .01 (.15) | .10(.13) | −.39(.30) | −.23(.29) | −.31(.28) | ||
| Perceived financial status | −.60 (.11)*** | −.53(.10)*** | −.79(.24)** | −.68(.23)** | −.36(.22) | ||
| Length of stay in the U.S. | −.02 (.00)*** | −.02(.00)*** | −.03(.01)* | −.02(.01) | −.01(.01) | ||
| Medical comorbidity | .51(.05)*** | .24(.11)* | −.08(.12) | ||||
| Functional disability | .08(.01)*** | .22(.03)*** | .16(.03)*** | ||||
| Health perceptions | - | .63(.08)*** | |||||
|
| |||||||
| R2 | .05*** | .18*** | .34*** | .01** | .10*** | .18*** | .25*** |
Note. B = unstandardized coefficient, SE = standard error
p < .05,
p < .01,
p < .001
Mediating Roles of Health Perceptions in the Relation between Diabetes and Depressive Symptoms
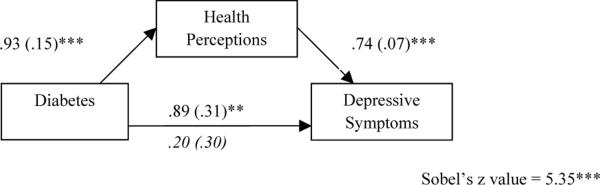
Employing criteria formulated by Baron and Kenny (31), the mediating model of health perception was tested next. The analysis was conducted after controlling for the effects of demographic variables (age, gender, marital status, education, perceived financial status, and length of stay in the U.S.). As presented in Figure 1, the independent paths among the independent variable (diabetes), the presumed mediator (health perceptions), and the dependent variable (depressive symptoms) showed significant levels of association. When health perceptions were controlled, the initially significant direct effects of diabetes on depressive symptoms (B = .89, p < .001) became non-significant (B =.20, p > .05). The Sobel test confirmed that the reduction in regression coefficients was statistically significant (z = 5.35, p < .001). A further test, using the equation by MacKinnon and Dwyer (32), indicated that 45% of the direct effect of diabetes on depressive symptoms was explained by subjective health perceptions.
Figure 1.
The Mediating Role of Health Perceptions in the Relation between Diabetes and Depressive Symptoms
Note. Numbers indicate unstandardized regression coefficients and standard errors in parentheses. The values italicized represent the indirect effect of diabetes on depressive symptoms after controlling for a mediating variable. All analyses were conducted with a control of demographic variables (age, gender, marital status, education, perceived financial status, and length of stay in the U.S). * p < .05, ** p < .01, *** p < .001
Discussion
In recognition of the public health challenges of diabetes (3) and the lack of research on Asian Americans (12,21,22), the present study examined the association between diabetes and depressive symptoms in Korean American older adults. Our focus was on exploring the mediating role of subjective perceptions of health in the relation between diabetes and depressive symptoms.
Among all participants, approximately 20% reported a diagnosis of diabetes. Consistent with previous findings (3), those individuals with diabetes showed adverse profiles in socioeconomic and health status. In multivariate analyses, diabetes was found to be associated with both health perceptions and depressive symptoms. People with diabetes not only perceived their own health in more negative ways (33) but also experienced elevated symptoms of depression (7,8,34). It is notable that functional disability was found to be a significant explanatory factor in models of health perceptions and of depressive symptoms. The association between diabetes and health perceptions remained significant throughout the series of hierarchical models whereas the diabetes-depressive symptoms association attenuated with the subsequent entry of control variables, suggesting a potential mechanism of mediation.
In a further analysis guided by Baron and Kenny (31), the proposed mediating role of subjective health perceptions in the relation between diabetes and depressive symptoms was supported. This finding, that the relation between diabetes and mental health was not only direct but also indirect through negative perceptions of health, yields implications for health promotions for older individuals with diabetes. This finding suggests that even in the presence of chronic health conditions, interventions can act to maintain or even enhance the mental health of older adults. Not only is this an important goal in and of itself, but such interventions may also act to arrest the negative spiral of depression leading to poor health management and subsequent exacerbation of the underlying diabetic condition. In addition to efforts for chronic disease prevention and health promotion, maintenance or enhancement of favorable perceptions and optimistic attitudes towards health have the potential to facilitate successful adaptation to challenges in later years of life and optimize physical and mental health outcomes.
Some limitations of the present study should be noted. The foremost concern is with our use of a geographically defined and nonrepresentative sample, which limits generalizability of the findings. Also, due to its cross-sectional design, caution must be made in drawing causal inference from the data. In particular, the present study conceptualized diabetes as a risk to mental health and health perceptions as an intervening step between them; however, the potential for a reversed or reciprocal relationship among the constructs should not be ignored. Symptoms of depression may also make individuals have negative perceptions of and attitudes toward health. In addition, the presence of diabetes was assessed based on self-reports, and the current study did not include specific information on the types of diabetes. Further studies need to employ comprehensive measures of diabetes including types of diabetes, attitudes towards diabetes, and self-knowledge on diabetes. Finally, the number of confounding variables made available in the present study was limited. Future studies need to consider adjusting analytic models for diabetes-related factors such as alcohol consumption, body mass index, and smoking.
Despite these limitations, the present study contributes to research and clinical practice by providing insights on approaches to chronic disease management and health promotion. Routinely assessing individuals' perceptions on their health and providing interventions that include efforts to reduce negative perceptions may help improving the mental health of older individuals with chronic health challenges.
Acknowledgments
The data used in the study were collected with support from the National Institute of Mental Health (R21MH081094).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest The authors declare that they have no conflict of interest.
References
- 1.American Diabetes Association Economic costs of diabetes in the U.S. in 2007. Diabetes Care. 2008;31:596–615. doi: 10.2337/dc08-9017. [DOI] [PubMed] [Google Scholar]
- 2.Meneilly GS, Tessier D. Diabetes in elderly adults. J Gerontol Med Sci. 2001;56:M5–M13. doi: 10.1093/gerona/56.1.m5. [DOI] [PubMed] [Google Scholar]
- 3.National Academy on an Aging Society . The most important epidemic of the 21st century? The Gerontological Society of America; Washington, DC: Winter. 2011. 2011. [Google Scholar]
- 4.Centers for Disease Control and Prevention . National diabetes fact sheet: General information and national estimates on diabetes in the United States, 2007. U.S. Department of Health and Human Services; Atlanta, GA: 2008. [Google Scholar]
- 5.Mokdad AH, Bowman BA, Ford ES, Vinicor F, Marks JS, Koplan JP. The continuing epidemics of obesity and diabetes in the United States. JAMA. 2001;286:1195–1200. doi: 10.1001/jama.286.10.1195. [DOI] [PubMed] [Google Scholar]
- 6.Trief PM. Depression in elderly diabetes patients. Diabetes Spectrum. 2007;20:71–75. [Google Scholar]
- 7.Blazer DG, Moody-Ayers S, Craft-Morgan J, Burchett B. Depression in diabetes and obesity: Racial/ethnic/gender issues in older adults. J Psychosom Res. 2002;53:913–916. doi: 10.1016/s0022-3999(02)00314-8. [DOI] [PubMed] [Google Scholar]
- 8.Talbot F, Nouwen A. A review of the relationship between depression and diabetes in adults: Is there a link? Diabetes Care. 2000;23:1556–1562. doi: 10.2337/diacare.23.10.1556. [DOI] [PubMed] [Google Scholar]
- 9.Anderson RJ, Freedland KE, Clouse RE, Lustman PJ. The prevalence of comorbid depression in adults with diabetes: A meta-analysis. Diabetes Care. 2001;24:1069–1078. doi: 10.2337/diacare.24.6.1069. [DOI] [PubMed] [Google Scholar]
- 10.Black SA, Markides KS, Ray LA. Depression predicts increased incidence of adverse health outcomes in older Mexican Americans with type 2 diabetes. Diabetes Care. 2003;26:2822–2828. doi: 10.2337/diacare.26.10.2822. [DOI] [PubMed] [Google Scholar]
- 11.Carnethon MR, Biggs ML, Barzilay JI, et al. Longitudinal association between depressive symptoms and incident type 2 diabetes mellitus in older adults: The cardiovascular health study. Arch Intern Med. 2007;167:802–807. doi: 10.1001/archinte.167.8.802. [DOI] [PubMed] [Google Scholar]
- 12.Chou KL, Chi I. Prevalence of depression among elderly Chinese with diabetes. Int J Geriatr Psychiatry. 2005;20:570–575. doi: 10.1002/gps.1328. [DOI] [PubMed] [Google Scholar]
- 13.Katon W, von Korff M, Ciechanowski P, et al. Behavioral and clinical factors associated with depression among individuals with diabetes. Diabetes Care. 2004;27:914–920. doi: 10.2337/diacare.27.4.914. [DOI] [PubMed] [Google Scholar]
- 14.Borawski EA, Kinney JM, Kahana E. The meaning of older adults' health appraisals: Congruence with health status and determinant of mortality. J Gerontol Soc Sci. 1996;51:S157–S170. doi: 10.1093/geronb/51b.3.s157. [DOI] [PubMed] [Google Scholar]
- 15.Bryant LL, Beck A, Fairclough DL. Factors that contribute to positive perceived health in an older population. J Aging Health. 2000;12:169–192. doi: 10.1177/089826430001200202. [DOI] [PubMed] [Google Scholar]
- 16.Jang Y, Chiriboga DA, Borenstein A, Small BJ, Mortimer JA. Health-related quality of life in community-dwelling older Whites and African Americans. J Aging Health. 2009;21:336–349. doi: 10.1177/0898264308329001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kahana E, Redmond C, Hill GJ, et al. The effects of stress, vulnerability, and appraisals on the psychological well-being of the elderly. Res Aging. 1995;17:459–489. [Google Scholar]
- 18.Martin P, Rott C, Kerns M, Poon L, Johnson M. Autonomy versus dependence in the oldest old. Springer; New York: 2000. Predictors of depressive symptoms in centenarians; pp. 91–104. [Google Scholar]
- 19.Aalto A-M, Uutela A, Aro AR. Health related quality of life among insulin-dependent diabetics: Disease-related and psychosocial correlates. Patient Education and Counseling. 1997;30:215–225. doi: 10.1016/s0738-3991(96)00963-9. [DOI] [PubMed] [Google Scholar]
- 20.Linn MW, Linn BS, Skyler JS, Harris R. The importance of self-assessed health in patients with diabetes. Diabetes Care. 1980;3:599–606. doi: 10.2337/diacare.3.5.599. [DOI] [PubMed] [Google Scholar]
- 21.Kim MT, Han HR, Song HJ, et al. A community-based, culturally tailored behavioral intervention for Korean Americans with type 2 diabetes. Diabetes Educ. 2009;35:986–994. doi: 10.1177/0145721709345774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Oza-Frank R, Ali MK, Vaccarino V, Narayan KM. Asian Americans: Diabetes prevalence across U.S. and World Health Organization weight classifications. Diabetes Care. 2009;32:1644–1646. doi: 10.2337/dc09-0573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jang Y, Chiriboga DA. Living in a different world: Acculturative stress among Korean American elders. J Gerontol Psy Sci. 2010;65B:14–21. doi: 10.1093/geronb/gbp019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jang Y, Chiriboga DA, Allen J, Kwak J, Haley WE. Willingness of older Korean American adults to use hospice. J Am Geriatr Soc. 2010;58:352–356. doi: 10.1111/j.1532-5415.2009.02684.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fillenbaum G. Multidimensional functional assessment: The Duke older Americans resources and services procedure. Lawrence Erlbaum; Hillsdale, NJ: 1988. [Google Scholar]
- 26.Nagi SZ. An epidemiology of disability among adults in the United States. Milbank Q - Health Soc. 1976;54:439–467. [PubMed] [Google Scholar]
- 27.Rosow I, Breslau N. A Guttman Health Scale for the aged. J Gerontol. 1966;21:556–559. doi: 10.1093/geronj/21.4.556. [DOI] [PubMed] [Google Scholar]
- 28.Sheikh J, Yesavage J. Geriatric Depression Scale: Recent evidence and development of a shorter version. Clin Gerontologist. 1986;5:165–173. [Google Scholar]
- 29.Jang Y, Small BJ, Haley WE. Cross-cultural comparability of the Geriatric Depression Scale: Comparison between older Koreans and older Americans. Aging Ment Health. 2001;5:31–37. doi: 10.1080/13607860020020618. [DOI] [PubMed] [Google Scholar]
- 30.Mui AC, Kang SY, Chen LM, Domanski MD. Reliability of the Geriatric Depression Scale for use among elderly Asian immigrants in the USA. Int Psychogeriatr. 2003;15:253–271. doi: 10.1017/s1041610203009517. [DOI] [PubMed] [Google Scholar]
- 31.Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 32.MacKinnon DP, Dwyer JH. Estimating mediated effects in prevention studies. Evaluation Review. 1993;17:144–158. [Google Scholar]
- 33.Brown DW, Balluz LS, Giles WH, et al. Diabetes mellitus and health-related quality of life among older adults. Findings from the behavioral risk factor surveillance system (BRFSS) Diabetes Res Clin Pract. 2004;65:105–115. doi: 10.1016/j.diabres.2003.11.014. [DOI] [PubMed] [Google Scholar]
- 34.Gavard JA, Lustman PJ, Clouse RE. Prevalence of depression in adults with diabetes. An epidemiological evaluation. Diabetes Care. 1993;16:1167–1178. doi: 10.2337/diacare.16.8.1167. [DOI] [PubMed] [Google Scholar]