Introduction
The first case of HIV in India was identified in 1986 in Chennai (1). Since that time, India’s National AIDS Control Organization (NACO) estimates that approximately 2.5 million Indians are now living with HIV/AIDS (2). Although recent reports suggest that HIV-incidence in India may be declining (3), persons already living with HIV/AIDS face a number of challenges, both in terms of the medical management of their disease and the psychosocial issues that accompany HIV-infection. Stigma is among the most pervasive of the psychosocial issues and has been described as one of the greatest barriers to dealing effectively with the epidemic worldwide (4). Stigma has been associated with depression, non-disclosure, and poor adherence to medications, subsequently contributing to increased morbidity and further spread of the disease (5–7). Initial studies of HIV-related stigma in India often used the Berger HIV Stigma Scale (8–11), yet despite this, the scale has not been adapted or validated for use in India’s unique cultural context.
The HIV Stigma Scale, developed by Barbara Berger and colleagues, measures stigma perceived and experienced by HIV-positive persons (12). Based on a conceptual model of perceived stigma, this 40-item scale yielded a four factor solution following exploratory factor analysis and measures four dimensions of HIV-related stigma: Personalized Stigma, Disclosure Concerns, Negative Self-Image, and Concern with Public Attitudes about People with HIV. While the Berger HIV Stigma Scale has been well-validated in other settings and used fairly extensively in many studies, it is also long (40 items) and its administration can be burdensome. In response to this concern, it has been shortened in both English and Spanish versions (13–15).
Despite the widespread use of the Berger HIV Stigma Scale in India and other contexts, several additional measures of HIV-related stigma have been developed and tested in Southern India, (16, 17). Notwithstanding this expansion of HIV-related stigma measures, there is increasing evidence that the construct of stigma and its possible impact are relatively consistent across different settings (18–21), suggesting that it may be more efficient to adapt and standardize existing instruments to different cultural settings rather than develop new ones specific to a given locale. The use of a common stigma scale would facilitate cross cultural comparisons and may enable a better appreciation of the phenomenon as it operates in different cultures and settings.
Furthermore, data from the original validation paper for the Berger HIV Stigma Scale suggest that the questionnaire can be shortened. Cronbach’s alpha for the 40-item scale in the US population within which it was developed was high, at 0.96 and ≥0.90 for each of the subscales, suggesting that even within subscales, items are redundant (22). Additionally, a number of items applied to more than one subscale (12), further suggesting redundancy in the 40-item scale. An abbreviated version of the scale is not only psychometrically necessary, but would greatly reduce patient burden.
Given the already widespread use of the Berger HIV Stigma Scale, its need to be shortened, and the need for comparative cross cultural studies on stigma, we conducted a study to adapt and standardize the Berger HIV Stigma Scale with the objective of creating a reliable, valid and abridged version of the scale that could be used to measure HIV-related stigma in the South Indian context.
Methods
Several different analyses commonly used in instrument development (23, 24) were carried out to adapt and evaluate the Berger HIV Stigma Scale to the South Indian context: (a) stakeholder and expert assessment of face and content validity of the entire scale, (b) assessment of convergent validity, (c) assessment of reliability (test-retest reliability and internal consistency/Cronbach’s alpha) of the entire scale, (d) confirmatory factor analysis based on the original subscale structure, (d) exploratory factor analysis to provide direction in abbreviating the scale; and (e) a second confirmatory factor analysis, convergent validity, and internal consistency/Cronbach’s alpha on the abridged version of the scale.
Study population, recruitment and consent
Men and women living with HIV/AIDS, aged 18–49 years and residing in and around the city of Chennai (urban) and Vellore town (semi-rural areas) in the state of Tamilnadu were recruited through support networks for HIV-positive individuals. Networks included the Tamilnadu chapter of the Indian Network of Positive Persons (INP+) with >75,000 members, the Tamilnadu chapter of Positive Women’s Network (PWN) with 4000 female members, and the Vellore-based Pushes Network with 1300 members. We sampled semi-purposively from these groups to obtain equal numbers of men and women.
Men and women affiliated with these networks were referred to study staff who described the study to them. Literate participants read the consent form themselves, while the interviewer read it out to those who were non–literate. Written informed consent was obtained from all since all were able to sign their names (many non-literate South Indians have learned to sign their names and all in this case were able to do so). All participants were given an opportunity to ask questions before signing the consent form.
Trained gender-matched interviewers/raters administered a questionnaire as a face-to-face interview in a private location after which individuals were compensated a nominal sum (Rs. 150/- or 3.50 USD) for their time. Individuals who participated in the test-retest portion of the study (n=50) provided contact information, were re-interviewed after 12–14 days and given the same nominal sum. Subsequently the questionnaire was administered to an additional sample of 200 HIV-positive men and women from support networks in Chennai and Vellore. Ethical committee clearance for this study was provided by the Institutional Review Boards of the Christian Medical College, Vellore and the University of Washington.
Instruments
Sociodemographic and Clinical Characteristics
General sociodemographic data collected included age, marital status, education and living situation (alone, with family or with friends). Self-reported information on respondents’ HIV infection was also collected, including mode of infection (e.g., sexual versus blood borne acquisition of HIV), timing of diagnosis, HIV-status disclosure, and any HIV-specific medications.
The Berger HIV Stigma Scale
The 40 items of the Berger HIV Stigma Scale were rated along a 4 point Likert scale (Strongly Disagree, Disagree, Agree, Strongly Agree) and measured stigma experienced by an HIV-positive person across the four domains of Personalized Stigma, Disclosure Concerns, Negative Self-Image and Public Attitudes. Questions such as “I have lost friends by telling them I have HIV” measured Personalized Stigma. Other items like, “I work hard to keep my HIV a secret”; “Having HIV makes me feel unclean” and “People with HIV are treated like outcasts” measured Disclosure Concerns, Negative Self-Image and Public Attitudes respectively. Although trained raters administered all questions to subjects irrespective of their literacy status, no changes were made to question phrasing (e.g., the pronoun “I” was not changed to “You”). The average time required to administer the 40-item version was 15–25 minutes, depending on subject literacy.
The Major Depression Inventory
To assess convergent validity, we measured depression using the Major Depression Inventory (MDI) (25, 26). This self-rating scale was developed by the World Health Organization and consists of 10 items rated along a 6 point Likert scale ranging from 0 (the symptom has not been present at all) to 5 (the symptom has been present all of the time). Individuals are categorized as having ‘mild, moderate or severe depression’ (25, 26). The MDI may be scored based on International Classification of Diseases-10 Revision (ICD-10) or Diagnostic Statistical Manual Fourth Edition (DSM-IV) diagnostic criteria to obtain diagnoses of major depressive disorder.
Translation
The instruments were translated into Tamil by members of the research team who were fluent in both English and Tamil (SK and RM), back translated into English by an independent person not involved in the project and checked for comparability with the original English questionnaire (27, 28). During translation into Tamil, the word “unclean” in the question, “Having HIV makes me feel unclean” was often misinterpreted to mean ‘personal hygiene’. There was no alternate phrasing in Tamil. Therefore, research assistants checked how each respondent interpreted the word “unclean” and asked subjects who misinterpreted the word to state what other interpretations came to mind. When they alluded to the concept of “feeling bad about oneself”, which was closest to the intended meaning of the question, we asked them to respond keeping this interpretation in mind.
Analyses of the 40-item Berger Stigma Scale
Face and Content Validity
To assess face validity, the Berger scale was simultaneously given to an expert panel, consisting of two English-speaking Indian psychiatrists and two members of our study team, who reviewed it for its relevance to the subject, its applicability to the Indian context, redundancy, and its comprehensiveness. The members of our study team who served as part of the expert panel are both social science researchers native to Tamilnadu (SK and RM). They are immersed in the local culture in ways that a Western researcher would not be and shared viewpoints similar to those of the two external experts, thus minimizing potential bias by including study team members on the expert panel. To determine content validity, we purposively recruited 5 persons (2 men and 3 women) from INP+ and PWN based on their willingness to spend about 45 minutes responding to questions about the scale. We held informal discussions with them about their perceptions on the relevance and adequacy of the concepts and language used in the scale as they related to the concept of stigma.
Two data entry operators independently entered the data into Epi- Info software Version 3.2. CDC, Atlanta, GA). The data files were then compared using the data compare options in Epi-Info. Any differences were resolved by a supervisor who referred back to the filled in schedule. Data analysis was done using SAS software, version 9.1 (SAS Corporation, Cary, NC).
Reliability
To assess test-retest reliability, the Berger HIV Stigma Scale was administered to 25 male and 25 female HIV-positive persons (a subset of the entire 250 participants for this study) at one point in time and then re-administered to the same sample after a gap of 12–14 days. The correlation of the measures taken at the two separate time points was determined using an intra-class correlation (ICC), where 0.60 was considered marginal, 0.70 acceptable and anything over 0.80 considered high (29). To assess internal consistency, we calculated Cronbach’s alpha for the scale overall and for each subscale, considering alpha values >0.70 indicative of good internal consistency (29).
Convergent Validity
Convergent validity was evaluated by assessing correlations of the scale to a theoretically related variable. Several studies have linked stigma and depression, or used measures of depression to assess concurrent validity with stigma measures (23, 30). Thus, we used a measure of depression (the MDI) and correlated depression scores with stigma scores to assess convergent validity. The reliability and internal consistency of the MDI, which has been used in other studies in India (31), were also assessed. The ICC was 0.7 (95% CI 0.5–0.8), suggesting acceptable reliability, and internal consistency was high (alpha=0.86).
Confirmatory Factor Analysis
Confirmatory Factor Analysis (CFA) of the original 40-item Berger HIV-stigma scale was performed on the entire sample of 250 participants, using the original 4 factor structure (Personalized Stigma, Disclosure Concerns, Negative Self-Image and Public Attitudes). A chi-square test for goodness of fit was used to assess model fit between the model and the sample. The root mean square error of approximation (RMSEA) was calculated, with a goal of 0.05 for good model fit (32). The Bentler’s Comparative Fit Index (CFI) was computed with a cut point of 0.95 set for good model fit (33, 34).
Exploratory Factor Analyses
After the initial CFA was conducted, an Exploratory Factor Analyses (EFA) using the principal-components factor extraction method with a non-orthogonal rotation (promax) was carried out to test the loading strength of the items on factors. The factor loading (lambda) was fixed at 0.6 in the EFA to guide item retention and shorten the scale. We then removed items with factor loadings <0.6 and items deemed redundant by our expert panel to produce the abridged scale.
Analyses of the Abridged Stigma Scale
A second CFA was conducted to assess the fit of the abridged scale. Cronbach’s alpha was calculated on the abridged scale overall and for each subscale. Convergent validity of the abridged scale was assessed and compared to that for the original 40-item scale.
Results
Face and content validity
Our expert panel reviewed the Berger HIV Stigma Scale and judged the instrument to be meaningful and relevant to the Indian cultural context. One psychiatrist noted that many questions were repetitive and suggested some items could be cut. Specifically, our expert panel judged two items to be highly redundant “I work hard to keep my HIV a secret” and “I never feel the need to hide the fact that I have HIV”, and suggested these be considered in the item reduction phase following the exploratory factor analysis. Five HIV-positive individuals subsequently responded to questions about the scale’s relevance and adequacy. They indicated that there was an element of repetitiveness in the questionnaire; specifically that similar questions were being asked in slightly different ways. Respondents also had difficulty understanding the 4 point “Strongly disagree----Strongly agree” response scale. Apart from their discomfort with selecting one of the two strongly worded end points, they also had difficulty in discerning the difference between ‘Strongly agree and Agree’ and ‘Strongly disagree and Disagree’. Further, the Berger scale comprises items worded as statements in the first person, ideally suited for a self-administered format. When the scale was administered by raters, respondents perceived some difficulty in understanding and applying the question to themselves.
Sociodemographic and Clinical Characteristics
Between December 2007 and July 2008 124 HIV-positive men and 126 women were enrolled, of whom 60% were from Chennai and 40% from Vellore (Table 1). The mean (±SD) age of male and female respondents was 37 (±5.2) and 33 (±6.1) years respectively, with women being younger than men by nearly five years (p<0.01). More men than women (75% vs 30%) were currently married while women were more likely to be widowed than men (51.6% vs. 4.8%, p<0.001). Most of the respondents were living with their families, be it extended or nuclear and nearly twice as many women as men (88% vs. 47%) reported sexual contact as the mode of infection. Notably, 28% of men, but only 7% of women reported that they did not know how they had contracted the disease (p<0.001). The large majority had been diagnosed with HIV over a year ago, with men somewhat more likely to have been recently diagnosed than women. While only slightly more than half (56%) of the women were on antiretroviral therapy (ART), this was true for three-quarters (78%) of the men (p<0.001). The group was predominantly literate, with more than 70% of all respondents having undergone primary to middle school education. The large majority had disclosed their HIV status to their sexual partner.
Table 1.
Characteristics of 250 male and female HIV-positive individuals from Chennai and Vellore, Tamil Nadu, enrolled from December 2007 to July 2008
| Characteristics | Male (n=124) | Female (n=126) | p-value (test statistic) | ||
|---|---|---|---|---|---|
|
| |||||
| n | % | n | % | ||
|
| |||||
| Site | 0.877 (0.02)3 | ||||
| Chennai (Urban) | 75 | 60.5 | 75 | 59.5 | |
| Vellore (Semi-rural) | 49 | 39.5 | 51 | 40.5 | |
|
| |||||
| Age (Years) | 36.78±5.21 | 32.92±6.1 | <0.001 (30.85)3 | ||
| 18 – 29 | 10 | 8.1 | 39 | 31.2 | |
| 30 – 34 | 30 | 24.4 | 40 | 32.0 | |
| 35 – 39 | 44 | 35.8 | 30 | 24.0 | |
| 40 + | 39 | 31.7 | 16 | 12.8 | |
|
| |||||
| Education | 0.068 (7.14)3 | ||||
| Illiterate | 6 | 5.0 | 12 | 9.5 | |
| Primary | 20 | 16.8 | 31 | 24.6 | |
| Middle | 67 | 56.3 | 68 | 54.0 | |
| High School & above | 26 | 21.9 | 15 | 11.9 | |
|
| |||||
| Marital Status | <0.001 (92.21)3 | ||||
| Married | 92 | 74.2 | 38 | 30.1 | |
| Single | 19 | 15.3 | 2 | 1.6 | |
| Separated/Divorced | 7 | 5.7 | 21 | 16.7 | |
| Widow/Widower | 6 | 4.8 | 65 | 51.6 | |
|
| |||||
| Living Situation | 0.0194 | ||||
| Alone | 14 | 11.3 | 9 | 7.1 | |
| With own family apart from parents or in-laws | 77 | 62.1 | 61 | 48.4 | |
| With parents or in-laws family | 31 | 25.0 | 55 | 43.7 | |
| With friends | 2 | 1.6 | 1 | 0.8 | |
|
| |||||
| HIV related characteristics | |||||
|
| |||||
| Mode of infection | <0.0014 | ||||
| Intravenous drug use | 23 | 18.9 | - | - | |
| Sexual intercourse | 57 | 46.7 | 111 | 88.1 | |
| Maternal to child transmission | 1 | 0.8 | 1 | 0.8 | |
| Contaminated blood products | 7 | 5.7 | 5 | 4.0 | |
| Don’t Know | 34 | 27.9 | 9 | 7.1 | |
|
| |||||
| When Diagnosed with HIV | 0.0114 | ||||
| In the past 3 months | 4 | 3.2 | - | - | |
| 3 months to 1 year ago | 15 | 12.1 | 8 | 6.4 | |
| 1–5 years ago | 66 | 53.2 | 58 | 46.0 | |
| >5 years ago | 39 | 31.5 | 60 | 47.6 | |
|
| |||||
| Disclosure to Romantic partner or Sexual partner | 0.290 (1.12)3 | ||||
| Yes | 88 | 71.5 | 96 | 77.4 | |
| No | 35 | 28.5 | 28 | 22.6 | |
|
| |||||
| Medication currently receiving | <0.0014 | ||||
| Antibiotics | 5 | 4.6 | 1 | 0.9 | |
| Vitamins | 14 | 13.0 | 52 | 43.3 | |
| Siddha-medicines2 | 5 | 4.6 | - | - | |
| Anti-retroviral therapy | 84 | 77.8 | 67 | 55.8 | |
Mean±SD;
South Indian Traditional medicine;
chi square test statistic;
Fisher’s exact test (no test statistic generated).
Analyses of the 40-item scale
Convergent validity
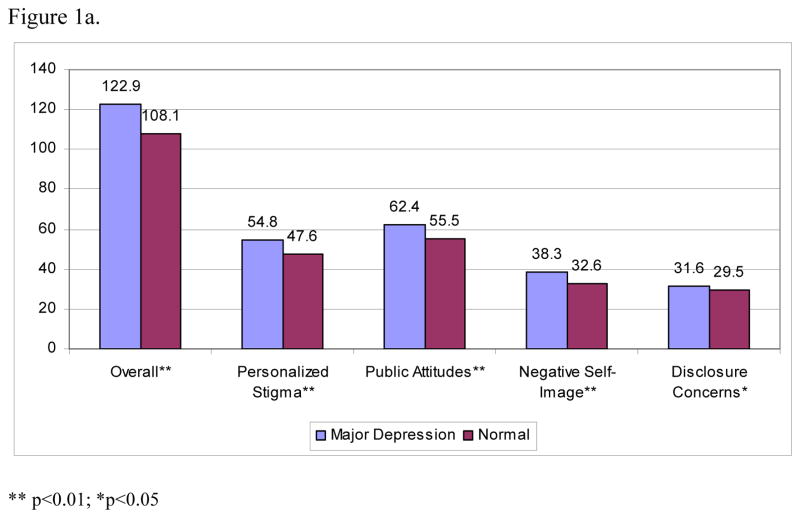
The overall mean stigma score as measured by the original 40-item version of the Berger scale was 109.6 (±16.2). Fifty-eight (24.2%) had scores in the top 25th percentile (e.g., those most severely stigmatized). Mean stigma scores were significantly higher among HIV-positive individuals with major depression than among those without major depression (122.9±12.3 vs. 108.1±15.9, p=<0.01) (Figure 1a). Similarly, stigma scores from all 4 subscales of the original scale were significantly higher among those with major depression than among those without a diagnosis of major depression (p<0.02 for all).
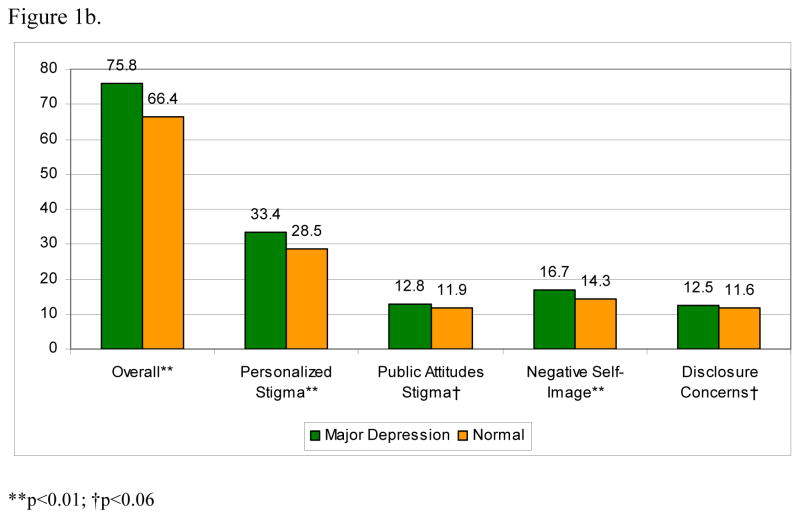
Figure 1.
Figure 1a. Relationship between major depression and stigma as a measured by the 40-item Berger HIV Stigma scale
Figure 1b. Relationship between major depression and stigma as a measured by the modified 25–item scale
Reliability
Among the first 50 men and women, the test-retest reliability of the original 40-item Berger scale was high (ICC=0.89; 95% CI 0.8–0.9) (Table 2). Test-retest reliability was also good for the initial three sub-scales (ICC=0.82 for Personalized Stigma, ICC= 0.85 for Negative Self-Image, and ICC=0.85 for Public Attitudes), but marginal (ICC=0.62) for the Disclosure Concerns subscale. Overall internal consistency for the entire 40-item scale was high with a Cronbach’s alpha of 0.91. It was similarly high for the Personalized Stigma (alpha=0.89) and Public Attitudes (alpha=0.86), but somewhat lower for the Negative Self-Image subscales (alpha=0.77). In contrast, the internal consistency for the Disclosure Concerns subscale was relatively low (alpha=0.62).
Table 2.
Reliability assessment of original 40-item Berger HIV Stigma scale and the abridged 25-item scale
| Berger Scale | Abridged Scale | |
|---|---|---|
|
| ||
| Overall | ||
| Number of items | 40 | 25 |
| Cronbach’s Alpha | 0.91 | 0.88 |
| Test retest reliability with 95% CI | 0.89(0.8 – 0.9) | - |
|
| ||
| Personalised Stigma | ||
| Number of items | 18 | 11 |
| Cronbach’s Alpha | 0.89 | 0.88 |
| Test retest reliability with 95% CI | 0.82(0.7 – 0.9) | - |
|
| ||
| Negative Stigma Sub Scale | ||
| Number of items | 13 | 6 |
| Cronbach’s Alpha | 0.77 | 0.80 |
| Test retest reliability with 95% CI | 0.85(0.7 – 0.9) | - |
|
| ||
| Public Attitude Stigma Sub Scale | ||
| Number of items | 20 | 4 |
| Cronbach’s Alpha | 0.86 | 0.68 |
| Test retest reliability with 95% CI | 0.85(0.7 – 0.9) | - |
|
| ||
| Disclosure Sub Scale | ||
| Number of items | 10 | 4 |
| Cronbach’s Alpha | 0.62 | 0.19 |
| Test retest reliability with 95% CI | 0.62(0.4 – 0.8) | - |
Promax rotation with Kappa=4.
Confirmatory Factor Analysis
Confirmatory Factor Analyses of the 40-item scale suggested poor model fit with the original subscale structure. The chi-square statistic had a p-value of <0.0001 with an RMSEA of 0.31, despite a Bentler’s CFI of 0.95. Bentler’s CFI was low for all of the subscales (ranging from 0.71–0.80), with the exception of the Disclosure Concerns subscale (CFI=0.94).
Exploratory Factor Analysis
Based on the poor fit of the 40-item scale and expert opinion indicating redundancy in the items, we conducted an EFA to abridge the scale and improve model fit. We examined factor loadings from the EFA (Table 3), and dropped items with factor loadings of 0.6 or lower. We also removed the previously identified redundant item with the lower factor loading (“I work hard to keep my HIV a secret”) and re-ran the CFA. This resulted in a 25-item version of the scale. Of the 15 removed items, five each were removed from the Disclosure Concerns, the Negative Self-Image, and the Public Attitudes subscales. Two items were deleted from the Personalized Stigma subscale, whereas three other items originally assigned to the Personalized Stigma subscale were moved to other subscales. The item “I regret having told some people that I have HIV” was incorporated into the Disclosure Concerns subscale, while two other items were incorporated into the Negative Self-Image subscale (“Some people act as though it’s my fault that I have HIV”, and “Since learning I have HIV, I feel set apart and isolated from the rest of the world”).
Table 3.
Factor Loadings from Exploratory Factor Analysis
| Items in Berger Scale | Factor Loadings | |||
|---|---|---|---|---|
| Personalized Stigma | Negative Self Image | Public Attitudes | Disclosure Concerns | |
| 31*. Some people close to me are afraid others will reject them if it becomes known that I have HIV. | 0.76 | 0.44 | 0.21 | 0.22 |
| 33. People have physically backed away from me when they learn I have HIV | 0.75 | 0.32 | 0.26 | 0.32 |
| 38. People who know I have HIV tend to ignore my good points | 0.73 | 0.33 | 0.28 | 0.33 |
| 28. Some people avoid touching me once they know I have HIV | 0.72 | 0.21 | 0.18 | 0.34 |
| 35. I have stopped socializing with some people because of their reactions to my having HIV | 0.70 | 0.26 | 0.37 | 0.23 |
| 29. People I care about stopped calling after learning I have HIV | 0.67 | 0.34 | 0.14 | 0.12 |
| 39. People seem afraid of me once they learn I have HIV. | 0.64 | 0.23 | 0.30 | 0.42 |
| 24. I have been hurt by how people reacted to learning I have HIV | 0.64 | 0.13 | 0.43 | 0.31 |
| 32. People don’t want me around their children once they know I have HIV | 0.61 | 0.49 | 0.26 | 0.31 |
| 36. I have lost friends by telling them I have HIV | 0.61 | 0.29 | 0.29 | 0.25 |
| 18. Some people who know I have HIV have grown more distant | 0.61 | 0.19 | 0.30 | 0.11 |
| 30. People have told me that getting HIV is what I deserve for how I lived my life | 0.42 | 0.33 | −0.08 | −0.10 |
| 12. Having HIV makes me feel unclean | 0.40 | 0.78 | 0.28 | 0.18 |
| 15.Having HIV makes me feel that I’m a bad person | 0.33 | 0.71 | 0.18 | 0.24 |
| 3. People’s attitudes about HIV make me feel worse about myself. | 0.23 | 0.71 | 0.29 | 0.18 |
| 7. I feel I am not as good a person as others because I have HIV. | 0.29 | 0.68 | 0.09 | 0.08 |
| 34. Some people act as though it’s my fault that I have HIV | 0.41 | 0.60 | 0.15 | 0.05 |
| 13. Since learning I have HIV, I feel set apart and isolated from the rest of world | 0.32 | 0.60 | 0.29 | 0.38 |
| 2. I feel guilty because I have HIV. | 0.15 | 0.55 | 0.15 | 0.27 |
| 23. Having HIV in my body is disgusting to me. | 0.41 | 0.55 | 0.25 | 0.34 |
| 1. In many areas of my life, no one knows that I have HIV. | −0.68 | 0.23 | 0.19 | 0.19 |
| 10. Most people believe that a person who has HIV is dirty | 0.29 | 0.27 | 0.68 | 0.37 |
| 16. Most people with HIV are rejected when others find out | 0.32 | 0.16 | 0.65 | 0.34 |
| 5. People with HIV lose their jobs when their employers find out | 0.14 | 0.17 | 0.64 | 0.14 |
| 14. Most people think that a person with HIV is disgusting | 0.26 | 0.17 | 0.61 | 0.17 |
| 4. Telling someone I have HIV is risky | 0.23 | 0.30 | 0.59 | 0.53 |
| 20. Most people are uncomfortable around someone with HIV | 0.49 | 0.13 | 0.58 | 0.45 |
| 19. Since learning I have HIV, I worry about people discriminating against me | 0.52 | 0.37 | 0.57 | 0.46 |
| 17. I am very careful who I tell that I have HIV | 0.13 | 0.12 | 0.55 | 0.51 |
| 9. People with HIV are treated like outcasts. | 0.35 | 0.13 | 0.50 | 0.23 |
| 40. When people learn you have HIV, they look for flaws in your character | 0.43 | 0.15 | 0.45 | 0.36 |
| 11. It is easier to avoid new friendships than worry about telling someone that I have HIV. | 0.13 | 0.29 | 0.41 | 0.27 |
| 21. I never feel the need to hide the fact that I have HIV | −0.01 | −0.17 | −0.14 | −0.68 |
| 25. I worry that people who know I have HIV will tell others | 0.35 | 0.14 | 0.43 | 0.68 |
| 26. I regret having told some people that I have HIV | 0.49 | 0.27 | 0.28 | 0.66 |
| 22. I worry that people may judge me when they learn I have HIV | 0.29 | 0.11 | 0.38 | 0.64 |
| 6. I work hard to keep my HIV a secret. | 0.21 | 0.23 | 0.55 | 0.62† |
| 27. As a rule, telling others that I have HIV has been a mistake | 0.54 | 0.16 | 0.25 | 0.57 |
| 37. I have told people close to me to keep the fact that I have HIV a secret | 0.32 | 0.19 | 0.18 | 0.32 |
| 8. I never feel ashamed of having HIV. | −0.18 | −0.20 | 0.19 | −0.29 |
| Eigen values‡ | 10.01 | 3.02 | 2.48 | 1.75 |
Number as provided in40-item Berger Scale,
Factor removed due to redundancy with Factor #21 “I never feel the need to hide the fact that I have HIV”,
Extracted eigenvalue >1.5 derived 4 factors.
Analyses of the Abridged Scale
Confirmatory Factor Analyses
The 25-item version of the scale had substantially improved fit with an RMSEA of 0.07, p=0.10 and a Bentler’s CFI of 0.99 and was adopted as the abridged scale in subsequent analyses. We also assessed goodness of fit for each of the subscales. The Personalized Stigma subscale continued to have the greatest number of items (11 items in the abridged version) and demonstrated reasonable fit (RMSEA=0.08, p<0.0001; CFI=0.94). The abridged Negative Self-Image subscale contained 6 items and had slightly better RMSEA (0.06, p=0.06); and CFI (0.98). The abridged Public Attitudes subscale (4 items) had the best fit with RMSEA=0.00, p=0.65 and CFI=1.0. The reduced Disclosure Concerns subscale (4 items) had reasonable fit (RMSEA=0.09, p=0.05; CFI=0.973), similar to what was observed in the original scale.
Convergent Validity
The mean stigma score for the abridged 25-item scale was 67.4 (±11.2). Fifty-seven (23.7%) had scores in the top 25th percentile (e.g., those most severely stigmatized). Similar to the original 40-item version of the Berger scale, mean stigma scores were significantly higher among HIV-positive individuals with major depression than among those without major depression as diagnosed by the MDI (75.8±8.7 vs. 66.4±11.0, p<0.01) (Figure 1b). For all four of the abridged subscales, stigma scores were higher among those with major depression (p<0.05 for all). However, this was of borderline statistical significance for Public Attitudes and Disclosure Concerns (p<0.06).
Reliability
Overall internal consistency for the abridged scale remained high, although somewhat lower than the 40-item version (Cronbach’s alphas of 0.88 versus 0.91, Table 2). It was similar for both versions of the Personalized Stigma and Negative Self-Image subscales, but substantially lower for the revised subscale in the Public Attitudes and Disclosure Concerns domains.
Discussion
We sought to abridge, adapt and validate the Berger HIV stigma scale for use in South India, using a sample of HIV-positive persons drawn from HIV support networks in Tamilnadu State. Using sophisticated psychometric techniques, we assessed the reliability and validity of a commonly used stigma scale in India, and systematically reduced the number of items. The 40-item Berger scale in general was meaningful and relevant in the Indian context, but long and contained a number of redundant items, both of which resulted in significant patient burden. Although the response scale (strongly disagree, disagree, agree, strongly agree) did not translate well into Tamil and was difficult for participants to interpret, there was good correlation with major depressive disorder, suggesting that the scale captures the relevant construct. Reliability and validity were high and exploratory and confirmatory factor analysis resulted in an abridged 25-item version of the scale that possessed better psychometric properties than the original 40-item version.
Reliability for both the original 40-item scale and the abridged 25-item version was good. The Cronbach’s alpha we observed for the 40-item version in an Indian population was similar to that observed by Berger in the initial group of HIV-positive individuals in the U.S. in which the scale was developed (12). Although the alpha was somewhat higher for the Tamil 40-item version than the 25-item version, both were high, suggesting each had good internal consistency, irrespective of the number of items. In addition, the higher Cronbach’s alpha of the lengthier version confirmed the expert opinion that the scale items were redundant and certain items could be cut from the scale (22). Test-retest reliability, another important measure of overall reliability, indicated stability over time.
Our observation that HIV-positive persons with major depression had significantly higher scores in all stigma domains as compared to non-depressed HIV-positive persons indicates good correlation between the two constructs (stigma and depression) and attests to the theoretical validity of the Berger scale as a measure of stigma. This relationship between stigma and depression has been reported elsewhere (35, 36), demonstrating consistency with our results.
Others have sought to validate and abridge the Berger HIV Stigma Scale in diverse settings and observed similar findings. Among HIV-positive individuals in a rural U.S. setting, Bunn and colleagues reduced the scale from 40 to 32 items with virtually no change in Cronbach’s alpha (15). In contrast, Wright and colleagues reduced the 40-item version down to 10 items and tested their abridged scale among African American young adults (age 16–25). No overall alpha was calculated, but alphas for the subscales were generally similar to those we observed (0.72–0.84 vs. 0.68–0.88) (14), and similar to the subscale alphas in the original Berger 40-item version. Similarly, Franke and colleagues translated the scale into Spanish and reduced it from 40 to 21 items in Peru, with only a slight reduction in Cronbach’s alpha for the abridged version (13). In our analyses, the alphas for three subscales of the abridged 25-item version were good, but only moderate for the public attitudes subscale. This is likely attributable to the reduced number of items under this sub-scale (12 versus 4 items) (37). All four of the groups of researchers that have shortened the scale have studied different populations and arrived at different versions of the scale with varying numbers of items. This suggests that stigma differs as a construct across cultures, and that perhaps certain facets of stigma are more or less relevant from one population to another.
This study is characterized by a variety of strengths and limitations. Strengths include the iterative process involving exploratory factor analysis and validation based on confirmatory factor analysis that employed theoretically driven statistical methods. This allowed us to reevaluate the role of each question in the Berger scale, identify culture-specific items and reorient them to the relevant subscales. In an effort to respect the original structure of the scale, we did not adapt the response options or the first-person question phrasing, despite some confusion over their meaning. Therefore, some respondents may not have clearly understood the questions or may have provided responses that did not correctly reflect their perceptions, which may be a limitation. Further assessments of response scales that include visual analogs to aid understanding, using the same items, should be performed among South Indian populations. Interviewer administered versions of the scale may be more effective if the questions are rephrased using the second-person. Another limitation is the potential non-representativeness of our sample, despite an adequate sample size.. We enrolled a group of HIV-positive individuals from Southern India which is a somewhat different context from other areas of the country. Furthermore our participants were all involved in support networks and, given this affiliation, they likely experienced less stigma and/or depression than HIV-positive individuals who are more socially isolated. An additional limitation was our inability to confirm HIV-related clinical data (e.g., mode of infection, timing of diagnosis, status disclosure, and HIV related medications), potentially resulting in recall bias. Finally, although we succeeded in reducing the Berger Stigma scale from 40 to 25 items in an iterative process, the scope of this study did not include testing the abridged scale in a separate population and we could not determine the time required to administer it. Despite these limitations, given the widespread stigma experienced by people with HIV and its fairly consistent manifestations, we hypothesize that the validated and abridged 25-item scale will have relevance in a variety of settings in South India.
HIV/AIDS is highly stigmatized in India and inhibits HIV-positive persons from disclosing their status, accessing medical care, and adhering to therapy (5–7). Validated and culturally relevant measures are essential to appropriately assess and quantify stigma and inform the downstream development of effective stigma interventions to address this psychosocial consequence of HIV infection. This culturally validated, 25-item stigma scale may reduce patient burden and could be used in busy Indian clinical settings to help identify individuals in need of support to encourage care seeking, status disclosure, and mental health services. It may also serve as a viable tool to assess reductions in stigma after interventions with patients with HIV in South India.
Acknowledgments
This project was funded by a grant from the Puget Sound Partners for Global Health (Award #26145) with additional support for LEM from the University of Washington Center for AIDS Research (National Institutes of Health P30 AI27757). The authors would like to thank Betsy Feldman for helpful statistical discussions and Katherine Murray for manuscript preparation assistance. The authors are also grateful to the leaders of the Indian Network of Positive Persons, the Positive Women’s Network and the Pushes Network for providing access to HIV-positive persons affiliated with their networks, and to the men and women who participated in this study.
References
- 1.Simoes EA, Babu PG, John TJ, Nirmala S, Solomon S, Lakshminarayana CS, et al. Evidence for HTLV-III infection in prostitutes in Tamil Nadu (India) Indian J Med Res. 1987 Apr;85:335–8. [PubMed] [Google Scholar]
- 2.National AIDS Control Organization. Facts and Figures. 2007 [cited Accessed on 28 march, 2007]; Available from: http://www.nacoonline.org/facts.htm.
- 3.Kumar R, Jha P, Arora P, Mony P, Bhatia P, Millson P, et al. Trends in HIV-1 in young adults in south India from 2000 to 2004: a prevalence study. Lancet. 2006 Apr 8;367(9517):1164–72. doi: 10.1016/S0140-6736(06)68435-3. [DOI] [PubMed] [Google Scholar]
- 4.UNAIDS. Stigma and discrimination. 2007 [cited Accessed on April 9, 2007]; Available from: http://www.unaids.org/en/Issues/Prevention_treatment/stigma.asp.
- 5.Simbayi LC, Kalichman S, Strebel A, Cloete A, Henda N, Mqeketo A. Internalized stigma, discrimination, and depression among men and women living with HIV/AIDS in Cape Town, South Africa. Soc Sci Med. 2007 May;64(9):1823–31. doi: 10.1016/j.socscimed.2007.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Leonard AD, Markham CM, Bui T, Shegog R, Paul ME. Lowering the risk of secondary HIV transmission: insights from HIV-positive youth and health care providers. Perspect Sex Reprod Health. Jun;42(2):110–6. doi: 10.1363/4211010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Curioso WH, Kepka D, Cabello R, Segura P, Kurth AE. Understanding the facilitators and barriers of antiretroviral adherence in Peru: a qualitative study. BMC Public Health. 10:13. doi: 10.1186/1471-2458-10-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chandra PS, Deepthivarma S, Manjula V. Disclosure of HIV infection in south India: patterns, reasons and reactions. AIDS Care. 2003;15(2):207–15. doi: 10.1080/0954012031000068353. [DOI] [PubMed] [Google Scholar]
- 9.Subramanian T, Gupte MD, Dorairaj VS, Periannan V, Mathai AK. Psychosocial impact and quality of life of people living with HIV/AIDS in South India. AIDS Care. 2009 Apr;21(4):473–81. doi: 10.1080/09540120802283469. [DOI] [PubMed] [Google Scholar]
- 10.Thomas BE, Rehman F, Suryanarayanan D, Josephine K, Dilip M, Dorairaj VS, et al. How stigmatizing is stigma in the life of people living with HIV: a study on HIV positive individuals from Chennai, South India. AIDS Care. 2005;17(7):795–801. doi: 10.1080/09540120500099936. [DOI] [PubMed] [Google Scholar]
- 11.Kumarasamy N, Safren SA, Raminani SR, Pickard R, James R, Krishnan AK, et al. Barriers and facilitators to antiretroviral medication adherence among patients with HIV in Chennai, India: a qualitative study. AIDS Patient Care STDS. 2005 Aug;19(8):526–37. doi: 10.1089/apc.2005.19.526. [DOI] [PubMed] [Google Scholar]
- 12.Berger BE, Ferrans CE, Lashley FR. Measuring stigma in people with HIV: psychometric assessment of the HIV stigma scale. Res Nurs Health. 2001 Dec;24(6):518–29. doi: 10.1002/nur.10011. [DOI] [PubMed] [Google Scholar]
- 13.Franke MF, Munoz M, Finnegan K, Zeladita J, Sebastian JL, Bayona JN, et al. Validation and abbreviation of an HIV stigma scale in an adult spanish-speaking population in urban Peru. AIDS Behav. Feb;14(1):189–99. doi: 10.1007/s10461-008-9474-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wright K, Naar-King S, Lam P, Templin T, Frey M. Stigma scale revised: reliability and validity of a brief measure of stigma for HIV+ youth. J Adolesc Health. 2007 Jan;40(1):96–8. doi: 10.1016/j.jadohealth.2006.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bunn JY, Solomon SE, Miller C, Forehand R. Measurement of stigma in people with HIV: a reexamination of the HIV Stigma Scale. AIDS Educ Prev. 2007 Jun;19(3):198–208. doi: 10.1521/aeap.2007.19.3.198. [DOI] [PubMed] [Google Scholar]
- 16.Steward WT, Herek GM, Ramakrishna J, Bharat S, Chandy S, Wrubel J, et al. HIV-related stigma: Adapting a theoretical framework for use in India. Soc Sci Med. 2008 Jul 1; doi: 10.1016/j.socscimed.2008.05.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zelaya CE, Sivaram S, Johnson SC, Srikrishnan AK, Solomon S, Celentano DD. HIV/AIDS stigma: reliability and validity of a new measurement instrument in Chennai, India. AIDS Behav. 2008;12(5):781–8. doi: 10.1007/s10461-007-9331-7. [DOI] [PubMed] [Google Scholar]
- 18.Van Brakel WH. Measuring health-related stigma--a literature review. Psychol Health Med. 2006 Aug;11(3):307–34. doi: 10.1080/13548500600595160. [DOI] [PubMed] [Google Scholar]
- 19.Rao D, Choi SW, Victorson D, Bode R, Peterman A, Heinemann A, et al. Measuring stigma across neurological conditions: the development of the stigma scale for chronic illness (SSCI) Qual Life Res. 2009 Jun;18(5):585–95. doi: 10.1007/s11136-009-9475-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Holzemer WL, Makoae LN, Greeff M, Dlamini PS, Kohi TW, Chirwa ML, et al. Measuring HIV stigma for PLHAs and nurses over time in five African countries. SAHARA J. 2009 Sep;6(2):76–82. doi: 10.1080/17290376.2009.9724933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nyblade LC. Measuring HIV stigma: existing knowledge and gaps. Psychol Health Med. 2006 Aug;11(3):335–45. doi: 10.1080/13548500600595178. [DOI] [PubMed] [Google Scholar]
- 22.Streiner D, Norman G. Health Measurement Scales A Practical Guide to Their Development and Use. New York: Oxford University Press, Inc; 1989. [Google Scholar]
- 23.Rao D, Choi S, Victorson D, Bode R, Heinemann A, Peterman A, et al. Measuring Stigma Across Neurological Conditions: The Development of the Stigma Scale for Chronic Illness (SSCI) Quality of Life Research. 2009;18:585–95. doi: 10.1007/s11136-009-9475-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lai J, Crane P, Cella D. Factor analysis techniques for assessing sufficient unidimensionality of cancer related fatigue. Quality of Life Research. 2006;15(7):1179–90. doi: 10.1007/s11136-006-0060-6. [DOI] [PubMed] [Google Scholar]
- 25.Bech P. The Major (ICD-10) Depression Inventory (MDI) 2007 [cited Accessed on April 11, 2007]; Available from: http://www.gp-training.net/protocol/psych/who/mdi.doc.
- 26.Olsen LR, Jensen DV, Noerholm V, Martiny K, Bech P. The internal and external validity of the Major Depression Inventory in measuring severity of depressive states. Psychol Med. 2003 Feb;33(2):351–6. doi: 10.1017/s0033291702006724. [DOI] [PubMed] [Google Scholar]
- 27.Cella D, Hernandez L, Bonomi A, Corona M, Vaquero M, Shiomoto G, et al. Spanish language translation and initial validation of the functional assessment of cancer therapy quality-of-life instrument. Medical Care. 1998;36(9):1407–18. doi: 10.1097/00005650-199809000-00012. [DOI] [PubMed] [Google Scholar]
- 28.Bonomi A, Cella D, Hahn E, Bjordal K, Sperner-Unterweger B, Gangeri L, et al. Multilingual translation of the Functional Assessment of Cancer Therapy (FACT) quality of life measurement system. Quality of Life Research. 1996;5(3):309–20. doi: 10.1007/BF00433915. [DOI] [PubMed] [Google Scholar]
- 29.Streiner DL. A checklist for evaluating the usefulness of rating scales. Can J Psychiatry. 1993 Mar;38(2):140–8. doi: 10.1177/070674379303800214. [DOI] [PubMed] [Google Scholar]
- 30.Alonzo AA, Reynolds NR. Stigma, HIV and AIDS: An exploration and elaboration of a stigma trajectory. Soc Sci Med. 1995;41:303–15. doi: 10.1016/0277-9536(94)00384-6. [DOI] [PubMed] [Google Scholar]
- 31.Barua A, Kar N. Screening for depression in elderly Indian population. Indian J Psychiatry. 2010 Apr;52(2):150–3. doi: 10.4103/0019-5545.64595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.McDonald RP, Ho MH. Principles and practice in reporting structural equation analyses. Psychol Methods. 2002 Mar;7(1):64–82. doi: 10.1037/1082-989x.7.1.64. [DOI] [PubMed] [Google Scholar]
- 33.Crowley SL, Fan X. Structural equation modeling: basic concepts and applications in personality assessment research. J Pers Assess. 1997 Jun;68(3):508–31. doi: 10.1207/s15327752jpa6803_4. [DOI] [PubMed] [Google Scholar]
- 34.Musil CM, Jones SL, Warner CD. Structural equation modeling and its relationship to multiple regression and factor analysis. Res Nurs Health. 1998 Jun;21(3):271–81. doi: 10.1002/(sici)1098-240x(199806)21:3<271::aid-nur10>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- 35.Goffman E. Stigma: Notes on the management of spoiled identity. New York: Simon and Schuster, Inc; 1963. [Google Scholar]
- 36.Laryea M, Gien L. The impact of HIV-positive diagnosis on the individual, Part 1: Stigma, rejection, and loneliness. Clin Nurs Res. 1993 Aug;2(3):245–63. doi: 10.1177/105477389300200302. discussion 63–6. [DOI] [PubMed] [Google Scholar]
- 37.Hattie J. Methodology review: assessing unidimensionality of tests and items. Applied Psychological Measurement. 1985;9:139–64. [Google Scholar]