Abstract
Background
Interpersonal continuity of care is valued by patients, but there is concern that it has declined in recent years.
Aim
To determine how often patients express preference for seeing a particular GP and the extent to which that preference is met.
Design of study
Analysis of data from the 2009/2010 English GP Patient Survey.
Setting
A stratified random sample of adult patients registered with 8362 general practices in England (response rate 39%, yielding 2?169?718 responses).
Method
Weighted estimates were calculated of preference for and success in seeing a particular GP. Multilevel logistic regression was used to identify characteristics associated with these two outcomes.
Results
Excluding practices with one GP, 62% of patients expressed a preference for seeing a particular GP. Of these patients, 72% were successful in seeing their preferred GP most of the time. Certain patient groups were associated with more preference for and success in seeing a particular GP. These were older patients (preference odds ratio [OR]?=?1.7, success OR?=?1.8), those with chronic medical conditions (preference OR?=?1.9, success OR?=?1.3), those with chronic psychological conditions (preference OR?=?1.6, success OR?=?1.3), and those recently requesting only non-urgent versus urgent appointments (preference OR?=?1.4, success OR?=?1.6). Patient groups that had more frequent preference but less success in seeing a preferred GP were females (preference OR?=?1.5, success OR?=?0.9), patients in larger practices (preference OR?=?1.3, success OR?=?0.5), and those belonging to non-white ethnic groups.
Conclusion
The majority of patients value interpersonal continuity, yet a large minority of patients and specific patient groups are not regularly able to see the GP they prefer.
Keywords: continuity of patient care, England, general practice, primary healthcare
INTRODUCTION
There are a number of dimensions of continuity of care.1–6 A widely used classification identifies three types of continuity, namely informational, management, and interpersonal (or relational) continuity (Box 1).1
Box 1. Types of continuity of care1
Informational continuity: the use of information on past events and personal circumstances to make current care appropriate for each individual
Management continuity: a consistent and coherent approach to the management of a health condition that is responsive to a patient’s changing needs.
Interpersonal (relational) continuity: an ongoing therapeutic relationship between a patient and one or more providers.
Studies from different countries suggest that interpersonal continuity of care is highly valued by patients, especially by females, older patients, and those with chronic disease.7,8 Continuity of care is associated with improved patient outcomes9,10 and increased patient satisfaction.11–13 However, interpersonal continuity has declined in recent years in the UK and in other countries.14–16 This decline may reflect increasing emphasis on technical (clinical) aspects of primary care quality, as well as a reduction in doctors’ working hours, an increase in part-time working, and organisational changes in out-of-hours care.
METHOD
Data
Data from the 2009/2010 English General Practitioner Patient Survey (GPPS) were analysed; the GPPS is a national questionnaire survey covering different aspects of patient experience, sent by post to a stratified random sample of adult patients registered with an English primary care practice. In 2009/2010, the questionnaire was sent to 5.5?million individuals.17,18 Results of the survey are reported publicly for all practices. To ensure a minimum number of responses per practice, practices serving small populations and practices that were likely to have low response rates were oversampled.19
In the GPPS, continuity of care was assessed by two questions focusing on preference for and success in seeing a preferred doctor (Box 2).
Box 2. Questions on continuity of care as they appear in the 2009/2010 GPPS questionnaire20
Q15. Is there a particular doctor you prefer to see at your GP surgery or health centre?
-
■
Yes ….. Please go to Q16
-
■
No ….. Please go to Section F
-
■
There is usually one doctor in my GP surgery or health centre ….. Please go to section F
Q16. How often do you see the doctor you prefer to see?
-
■
Always or almost always
-
■
A lot of the time
-
■
Some of the time
-
■
Never or almost never
-
■
Not tried at this GP surgery or health centre
Using data provided by the survey responders, associations between these two measures of continuity of care and patient age, sex, ethnicity (16 categories as defined by the Office for National Statistics), and self-reported chronic medical or psychological/emotional condition were examined. Associations with patient deprivation (Index of Multiple Deprivation 2007, based on the patient’s postcode21) and the number of non-trainee GPs in each practice (as a marker of practice size) were also examined, using data from the 2009 GP census provided by the NHS Information Centre. Finally, associations with types of appointments requested in the previous 6?months, as reported by patients, were examined using a four-category classification; that is, whether the appointment(s) they had tried to make were urgent (within 2?working days) or non-urgent (after more than 2?working days), or both, or neither.
How this fits in
Previous studies suggest that patients value interpersonal continuity of care, but this preference varies in different patient groups. This study shows that 62% of primary care patients in England express a preference for seeing a particular doctor. Patients who were more likely to have such a preference were found to be females, older patients, those with chronic medical or psychological/emotional conditions, and patients of non-white ethnic origin. However, more than one-quarter of patients who prefer to see a particular doctor do not succeed in doing so most of the time. This study provides evidence that continuity of care is valued by the majority of patients. More needs to be done to meet these aspirations, especially in the light of evidence that continuity of care has declined in general practice in recent years.
Analysis
Responses to how often patients were able to see their preferred doctor (where they expressed a preference for doing so) were dichotomised into a yes (‘always or almost always’ or ‘a lot of the time’)/no (‘some of the time’ or ‘never or almost never’) measure.
Survey weights were developed by Ipsos MORI (the survey provider) and were used in the analysis to account for the complex survey design and non-response in prevalence estimates of preference for and success in seeing a preferred doctor. These weights employed rim weighting with two rims: (a) age-by-sex (8*2 levels), and (b) practice (8362 levels).19
Crude and multivariate logistic regression models were used to examine the association between various patient and practice characteristics and preference for and success in seeing a preferred doctor, separately. The data were adjusted for sex, age group, ethnicity, deprivation quintile, self-reported chronic medical or psychological/emotional condition, number of practice doctors, and type of appointments requested by the patient in the previous 6?months.
Crude models made use of the weights and adjusted standard errors to account for the survey design. Multivariate models did not make use of the weights but did include random intercepts for practice to account for clustering of patients within practices and to better distinguish the experiences and preferences of patient subgroups from general variation in continuity at practice level.
Although patient registration with a given practice is largely determined by geographical proximity, some patients might choose to register with a smaller practice specifically to get better continuity of care, in which case it would not have been appropriate to adjust sociodemographic associations for practice size. For this reason, a sensitivity analysis was performed, excluding the number of practice doctors. The results were very similar, so the data are not shown.
Stata (version 11) was used for the descriptive analyses and SAS (version 9.2) for the regression analyses.
RESULTS
The overall response rate was 39%, with 2?169?718 completed responses from patients in 8362 practices.17,18 The sociodemographic characteristics of responders are shown in Table 1.
Table 1.
Demographic characteristics of responders to the 2009/2010 General Practice Patient Survey
| Characteristic | n | % | |
|---|---|---|---|
| All survey responders | 2 169 718 | 100 | |
| Sex | |||
| Male | 897 326 | 42.4 | |
| Female | 1 218 009 | 57.6 | |
| Age group, years | |||
| 18-24 | 103 865 | 4.9 | |
| 25-34 | 230 654 | 10.9 | |
| 35-44 | 326 488 | 15.5 | |
| 45-54 | 376 472 | 17.8 | |
| 55-64 | 428 774 | 20.3 | |
| 65-74 | 357 022 | 16.9 | |
| 75-84 | 223 834 | 10.6 | |
| ≥85 | 66 621 | 3.2 | |
| Ethnic group (ONS 6) | Ethnic group (ONS16) | ||
| White | White British | 1 746 425 | 82 |
| Irish | 28 805 | 1.4 | |
| Any other white | 86 278 | 4.1 | |
| Mixed | White and Black Caribbean | 4345 | 0.2 |
| White and Black African | 2808 | 0.1 | |
| White and Asian | 4182 | 0.2 | |
| Any other mixed | 5046 | 0.2 | |
| South-Asian | Indian | 53 464 | 2.6 |
| Pakistani | 29 056 | 1.4 | |
| Bangladeshi | 9711 | 0.5 | |
| Any other Asian | 21 270 | 1 | |
| Black | Black Caribbean | 24 095 | 1.1 |
| Black African | 29 936 | 1.4 | |
| Any other black | 4750 | 0.2 | |
| Chinese | Chinese | 10 007 | 0.5 |
| Other ethnic group | Other ethnic group | 69 665 | 3.3 |
| Deprivation quintile | |||
| 1 (affluent) | 387 771 | 17.9 | |
| 2 | 418 707 | 19.3 | |
| 3 | 430 329 | 19.9 | |
| 4 | 446 263 | 20.6 | |
| 5 (deprived) | 483 594 | 22.3 | |
| Presence of self-reported chronic medical condition | |||
| No | 948 565 | 49.9 | |
| Yes | 951 323 | 50.1 | |
| Presence of self-reported long-standing psychological or emotional condition | |||
| No | 1 792 622 | 94.2 | |
| Yes | 110 507 | 5.8 | |
| Number of practice GPs | |||
| 1 | 259 957 | 12.1 | |
| 2 | 347 707 | 16.2 | |
| 3 | 285 727 | 13.3 | |
| 4 | 281 408 | 13.1 | |
| 5 | 257 185 | 11.9 | |
| 6-9 | 651 996 | 30.2 | |
| ≥10 | 72 390 | 3.4 | |
| Type of appointments sought in previous 6 monthsa | |||
| No appointments requested | 570 480 | 26.3 | |
| Urgent only | 554 818 | 25.6 | |
| Non-urgent only | 271 794 | 12.5 | |
| Both urgent and non-urgent | 772 626 | 35.6 | |
ONS = Office for National Statistics.
As reported by the patients (see Method).
Preference for seeing a particular doctor
Two per cent of patients reported that there was only one GP in their practice. After excluding those patients from further analysis, 62% of patients reported having a preference for seeing a particular doctor (Table 2). Such a preference varied across patient groups (Table 2) and was higher in females (68% versus 56% in males), older patients (52% for age group 18–24?years, increasing to 81% for the age group 75–84?years), those with chronic medical or psychological/emotional conditions (75% and 78% respectively) compared to those without chronic conditions (52% and 61% respectively), and those living in more affluent areas (from 60% to 64% for patients from the most to the least deprived areas).
Table 2.
Prevalence and odds ratios for having a preference for seeing a particular doctor
| Characteristic | Weighted prevalencea (95% CI) | Crude weighted ORa (95% CI) | Adjusted ORb (95% CI) | |
|---|---|---|---|---|
| All survey responders | 62.2 (61.9 to 62.4) | N/A | N/A | |
| Sex | ||||
| Male | 56.3 (56.1 to 56.6) | Reference | Reference | |
| Female | 67.5 (67.2 to 67.7) | 1.60 (1.59 to 1.61) | 1.50 (1.49 to 1.52) | |
| Age group, years | ||||
| 18-24 | 51.7 (51.1 to 52.2) | 0.49 (0.48 to 0.50) | 0.65 (0.64 to 0.66) | |
| 25-34 | 51.0 (50.6 to 51.3) | 0.48 (0.47 to 0.48) | 0.55 (0.54 to 0.56) | |
| 35-44 | 56.0 (55.6 to 56.3) | 0.58 (0.58 to 0.59) | 0.66 (0.65 to 0.67) | |
| 45-54 | 61.4 (61.1 to 61.7) | 0.73 (0.72 to 0.74) | 0.79 (0.78 to 0.80) | |
| 55-64 | 68.6 (68.3 to 68.9) | Reference | Reference | |
| 65-74 | 76.0 (75.8 to 76.3) | 1.45 (1.44 to 1.47) | 1.36 (1.35 to 1.38) | |
| 75-84 | 81.1 (80.8 to 81.4) | 1.97 (1.94 to 2.00) | 1.71 (1.69 to 1.74) | |
| ≥85 | 80.0 (79.5 to 80.4) | 1.83 (1.78 to 1.88) | 1.54 (1.50 to 1.58) | |
| Ethnic group (ONS 6) | Ethnic group (ONS16) | |||
| White | White British | 62.9 (62.6 to 63.2) | Reference | Reference |
| Irish | 65.1 (64.2 to 65.9) | 1.10 (1.06 to 1.14) | 0.97 (0.94 to 1.00) | |
| Any other white | 57.5 (56.9 to 58.1) | 0.80 (0.78 to 0.82) | 1.03 (1.01 to 1.05) | |
| Mixed | White and Black Caribbean | 56.8 (54.8 to 58.9) | 0.78 (0.72 to 0.84) | 1.05 (0.97 to 1.14) |
| White and Black African | 52.2 (49.6 to 54.7) | 0.64 (0.58 to 0.71) | 0.92 (0.84 to 1.02) | |
| White and Asian | 56.7 (53.8 to 59.6) | 0.77 (0.69 to 0.87) | 1.07 (0.99 to 1.16) | |
| Any other mixed | 59.7 (57.7 to 61.7) | 0.88 (0.81 to 0.95) | 1.09 (1.02 to 1.18) | |
| South-Asian | Indian | 63.0 (62.2 to 63.9) | 1.01 (0.97 to 1.04) | 1.49 (1.45 to 1.53) |
| Pakistani | 61.4 (60.4 to 62.4) | 0.94 (0.90 to 0.98) | 1.49 (1.43 to 1.54) | |
| Bangladeshi | 61.7 (60.2 to 63.2) | 0.95 (0.89 to 1.01) | 1.74 (1.64 to 1.84) | |
| Any other Asian | 59.0 (57.9 to 60.1) | 0.85 (0.81 to 0.89) | 1.28 (1.23 to 1.33) | |
| Black | Black Caribbean | 61.9 (60.9 to 62.8) | 0.96 (0.92 to 1.00) | 1.14 (1.10 to 1.18) |
| Black African | 47.3 (46.4 to 48.2) | 0.53 (0.51 to 0.55) | 0.81 (0.78 to 0.83) | |
| Any other black | 59.1 (57.2 to 61.1) | 0.86 (0.79 to 0.93) | 1.08 (0.99 to 1.17) | |
| Chinese | Chinese | 48.5 (47.0 to 50.0) | 0.56 (0.52 to 0.59) | 0.86 (0.81 to 0.90) |
| Other ethnic group | Other ethnic group | 58.5 (57.9 to 59.1) | 0.83 (0.81 to 0.85) | 1.14 (1.12 to 1.17) |
| Deprivation quintile | ||||
| 1 (affluent) | 64.1 (63.7 to 64.5) | Reference | Reference | |
| 2 | 63.3 (62.9 to 63.6) | 0.96 (0.95 to 0.98) | 0.96 (0.95 to 0.97) | |
| 3 | 62.2 (61.8 to 62.6) | 0.92 (0.90 to 0.94) | 0.92 (0.91 to 0.93) | |
| 4 | 61.0 (60.6 to 61.3) | 0.87 (0.86 to 0.89) | 0.89 (0.88 to 0.90) | |
| 5 (deprived) | 59.5 (59.1 to 60.0) | 0.82 (0.81 to 0.84) | 0.84 (0.83 to 0.85) | |
| Presence of self-reported chronic medical condition | ||||
| No | 52.1 (51.7 to 52.4) | Reference | Reference | |
| Yes | 74.8 (74.5 to 75.0) | 2.73 (2.70 to 2.76) | 1.87 (1.86 to 1.89) | |
| Presence of self-reported long-standing psychological or emotional condition | ||||
| No | 61.3 (61.1 to 61.6) | Reference | Reference | |
| Yes | 78.3 (77.9 to 78.7) | 2.28 (2.23 to 2.33) | 1.59 (1.57 to 1.62) | |
| Number of practice GPs | ||||
| 1 | 56.4 (55.6 to 57.2) | 0.94 (0.90 to 0.97) | 1.01 (0.97 to 1.05) | |
| 2 | 58.0 (57.4 to 58.6) | Reference | Reference | |
| 3 | 61.9 (61.3 to 62.5) | 1.18 (1.13 to 1.22) | 1.20 (1.15 to 1.25) | |
| 4 | 63.5 (62.9 to 64.1) | 1.26 (1.22 to 1.30) | 1.29 (1.24 to 1.35) | |
| 5 | 63.6 (63.0 to 64.2) | 1.26 (1.22 to 1.31) | 1.31 (1.26 to 1.37) | |
| 6-9 | 63.0 (62.6 to 63.4) | 1.23 (1.19 to 1.27) | 1.30 (1.25 to 1.34) | |
| ≥10 | 62.2 (60.7 to 63.6) | 1.19 (1.11 to 1.27) | 1.28 (1.19 to 1.37) | |
| Type of appointments sought in previous 6 monthsc | ||||
| No appointments requested | 47.5 (47.2 to 47.8) | 0.65 (0.64 to 0.66) | 0.67 (0.66 to 0.68) | |
| Urgent only | 58.3 (58.0 to 58.6) | Reference | Reference | |
| Non-urgent only | 67.5 (67.1 to 67.9) | 1.49 (1.46 to 1.51) | 1.40 (1.39 to 1.42) | |
| Both urgent and non-urgent | 73.5 (73.2 to 73.7) | 1.98 (1.96 to 2.00) | 1.85 (1.83 to 1.87) | |
N/A = not applicable. ONS = Office for National Statistics. OR = odds ratio.
Estimated from weighted unadjusted analysis; P<0.001 for all association (joint tests for categorical variables).
Estimated from a single multivariate logistic regression model including all variables that appear in the table, plus a random practice intercept; P<0.001 for all associations (joint tests for categorical variables).
As reported by the patients (see Method).
Patients’ preference for seeing a particular doctor ranged from 47% to 65% of responders across the 16 ethnic groups, and increased with the number of practice GPs (58% for practices with two GPs, increasing to 63% for practices with six to nine GPs). Preference for seeing a particular doctor was higher in patients who had requested only non-urgent appointments in the previous 6?months (68%) compared to patients who had requested only urgent appointments (58%). The crude odds ratios (Table 2) reflect the associations described above. All associations are stronger than would be expected by chance (P<0.001).
In multivariate analysis, there was strong evidence that differences exist in the preference for seeing a particular doctor across all sociodemographic groups after adjusting for other factors (P<0.001 for all variables) (Table 2). This preference was more common among females (odds ratio [OR]?=?1.50), older people (OR?=?1.71 for age group 74–85?years compared to age group 55–64?years), responders suffering from a chronic medical (OR?=?1.87) or psychological/emotional condition (OR?=?1.59), and those from more affluent areas (OR?=?0.84 for most deprived compared to most affluent areas). Patients from South-Asian ethnic groups (Bangladeshi, Indian, Pakistani and ‘any other Asian’) had substantially higher preference for seeing a particular doctor (OR?=?1.74, 1.49, 1.49, and 1.28 respectively, compared to white British). Patients were more likely to express such preference if they were registered with practices with a greater number of GPs (OR?=?1.3 for patients registered with practices with six to nine GPs compared to patients registered with practices with two GPs) and if they had sought non-urgent appointments (OR?=?1.4 patients seeking non-urgent appointments only compared to patients seeking urgent appointments only).
Success in seeing a preferred doctor
Subsequent analysis is restricted to patients with a preference for seeing a particular doctor. Of these patients, 72% were successful in seeing the doctor they preferred ‘always or almost always’ or ‘a lot of the time’: those two response categories are referred to using the term ‘most of the time’ hereafter (Table 3). The proportion of patients who were successful in seeing their preferred GP most of the time was higher in males (74% versus 70% in females), older patients (60% for age group 18–24?years, increasing to 87% for age group 75–84 years), and those with chronic medical or psychological/emotional conditions (77% and 75% respectively) when compared to those without (66% and 72% respectively). White patients were more likely to be able to see the doctor of their choice, compared to most other ethnic groups. More deprived patients were less successful in seeing the doctor they preferred most of the time (67% for the most-deprived, rising to 74% for the least-deprived patients). Success in seeing a particular doctor decreased as the number of practice GPs increased (77% for practices with two GPs compared to 69% for practices with 10 or more GPs). Success in seeing a particular doctor was least among patients requesting urgent appointments only (69%), where it was greatest for patients requesting only non-urgent appointments (79%). The crude odds ratios (Table 3) reflect the associations described above. All associations are stronger than would be expected by chance (P<0.001).
Table 3.
Prevalence and adjusted odds ratios for seeing a preferred doctormost of the time
| Characteristic | Weighted prevalencea (95% CI) | Crude weighted ORa (95% CI) | Adjusted ORb 95% CI) | |
|---|---|---|---|---|
| All survey responders | 71.8 (71.4 to 72.1) | N/A | N/A | |
| Sex | ||||
| Male | 73.6 (73.2 to 74.0) | Reference | Reference | |
| Female | 70.2 (69.9 to 70.6) | 0.85 (0.84 to 0.86) | 0.87 (0.86 to 0.88) | |
| Age group, years | ||||
| 18-24 | 59.8 (59.1 to 60.5) | 0.43 (0.42 to 0.44) | 0.43 (0.42 to 0.44) | |
| 25-34 | 60.2 (59.7 to 60.8) | 0.44 (0.43 to 0.44) | 0.48 (0.47 to 0.49) | |
| 35-44 | 63.6 (63.1 to 64.0) | 0.50 (0.49 to 0.51) | 0.54 (0.53 to 0.55) | |
| 45-54 | 69.8 (69.4 to 70.3) | 0.67 (0.66 to 0.68) | 0.68 (0.67 to 0.69) | |
| 55-64 | 77.7 (77.3 to 78.1) | Reference | Reference | |
| 65-74 | 84.3 (84.0 to 84.7) | 1.55 (1.52 to 1.58) | 1.53 (1.50 to 1.56) | |
| 75-84 | 86.5 (86.1 to 86.8) | 1.84 (1.80 to 1.87) | 1.82 (1.79 to 1.86) | |
| ≤85 | 85.3 (84.8 to 85.7) | 1.66 (1.61 to 1.72) | 1.56 (1.51 to 1.61) | |
| Ethnic group (ONS 6) | Ethnic group (ONS16) | |||
| White | White British | 73.7 (73.4 to 74.1) | Reference | Reference |
| Irish | 74.1 (73.2 to 75.1) | 1.02 (0.97 to 1.07) | 0.90 (0.86 to 0.94) | |
| Any other white | 66.9 (66.2 to 67.5) | 0.72 (0.70 to 0.74) | 0.85 (0.83 to 0.88) | |
| Mixed | White and Black Caribbean | 61.8 (59.1 to 64.4) | 0.58 (0.52 to 0.64) | 0.90 (0.81 to 1.00) |
| White and Black African | 56.6 (53.4 to 59.8) | 0.46 (0.41 to 0.53) | 0.68 (0.60 to 0.78) | |
| White and Asian | 63.4 (60.7 to 66.1) | 0.62 (0.55 to 0.69) | 0.81 (0.72 to 0.90) | |
| Any other mixed | 62.4 (60.1 to 64.7) | 0.59 (0.54 to 0.65) | 0.74 (0.67 to 0.81) | |
| South-Asian | Indian | 60.7 (59.3 to 62.1) | 0.55 (0.52 to 0.58) | 0.73 (0.71 to 0.76) |
| Pakistani | 54.4 (52.9 to 55.9) | 0.43 (0.40 to 0.45) | 0.66 (0.63 to 0.69) | |
| Bangladeshi | 50.2 (48.1 to 52.3) | 0.36 (0.33 to 0.39) | 0.57 (0.53 to 0.61) | |
| Any other Asian | 56.8 (55.4 to 58.1) | 0.47 (0.44 to 0.49) | 0.59 (0.56 to 0.62) | |
| Black | Black Caribbean | 65.6 (64.2 to 67.0) | 0.68 (0.64 to 0.72) | 0.83 (0.79 to 0.87) |
| Black African | 52.3 (50.9 to 53.8) | 0.39 (0.37 to 0.42) | 0.55 (0.53 to 0.58) | |
| Any other black | 58.0 (55.3 to 60.6) | 0.49 (0.44 to 0.55) | 0.70 (0.62 to 0.78) | |
| Chinese | Chinese | 56.2 (54.1 to 58.4) | 0.46 (0.42 to 0.50) | 0.55 (0.51 to 0.59) |
| Other ethnic group | Other ethnic group | 60.6 (59.9 to 61.4) | 0.55 (0.53 to 0.57) | 0.66 (0.64 to 0.68) |
| Deprivation quintile | ||||
| 1 (affluent) | 74.3 (73.7 to 74.8) | Reference | Reference | |
| 2 | 74.1 (73.6 to 74.6) | 0.99 (0.97 to 1.02) | 0.99 (0.97 to 1.01) | |
| 3 | 72.3 (71.8 to 72.8) | 0.90 (0.88 to 0.93) | 0.95 (0.94 to 0.97) | |
| 4 | 69.6 (69.1 to 70.1) | 0.79 (0.77 to 0.82) | 0.91 (0.89 to 0.93) | |
| 5 (deprived) | 67.0 (66.4 to 67.6) | 0.70 (0.68 to 0.73) | 0.86 (0.84 to 0.88) | |
| Presence of self-reported chronic medical condition | ||||
| No | 66.3 (65.8 to 66.7) | Reference | Reference | |
| Yes | 76.8 (76.4 to 77.1) | 1.68 (1.66 to 1.70) | 1.29 (1.27 to 1.30) | |
| Presence of self-reported long-standing psychological or emotional condition | ||||
| No | 71.9 (71.5 to 72.2) | Reference | Reference | |
| Yes | 75.3 (74.8 to 75.8) | 1.19 (1.17 to 1.22) | 1.25 (1.22 to 1.27) | |
| Number of practice GPs | ||||
| 1 | 78.5 (77.3 to 79.6) | 1.10 (1.01 to 1.19) | 1.42 (1.33 to 1.52) | |
| 2 | 76.9 (76.0 to 77.7) | Reference | Reference | |
| 3 | 74.5 (73.6 to 75.4) | 0.88 (0.82 to 0.94) | 0.76 (0.71 to 0.81) | |
| 4 | 73.4 (72.6 to 74.3) | 0.83 (0.78 to 0.89) | 0.66 (0.61 to 0.70) | |
| 5 | 72.0 (71.1 to 72.9) | 0.77 (0.73 to 0.83) | 0.57 (0.53 to 0.61) | |
| 6-9 | 69.7 (69.2 to 70.3) | 0.69 (0.66 to 0.73) | 0.48 (0.45 to 0.51) | |
| ≥10 | 68.8 (67.0 to 70.7) | 0.67 (0.60 to 0.74) | 0.44 (0.40 to 0.49) | |
| Type of appointments sought in previous 6 monthsc | ||||
| No appointments requested | 73.6 (73.2 to 74.0) | 1.23 (1.21 to 1.25) | 1.17 (1.15 to 1.19) | |
| Urgent only | 69.4 (68.9 to 69.8) | Reference | Reference | |
| Non-urgent only | 78.8 (78.4 to 79.2) | 1.64 (1.60 to 1.68) | 1.59 (1.57 to 1.62) | |
| Both urgent and non-urgent | 70.3 (69.9 to 70.7) | 1.05 (1.03 to 1.06) | 1.12 (1.10 to 1.13) | |
N/A = not applicable. ONS = Office for National Statistics. OR = odds ratio.
Estimated from weighted unadjusted analysis; P<0.001 for all association (joint tests for categorical variables).
Estimated from a single multivariate logistic regression model including all variables that appear in the table, plus a random practice intercept; P<0.001 for all associations (joint tests for categorical variables).
As reported by the patients (see Method).
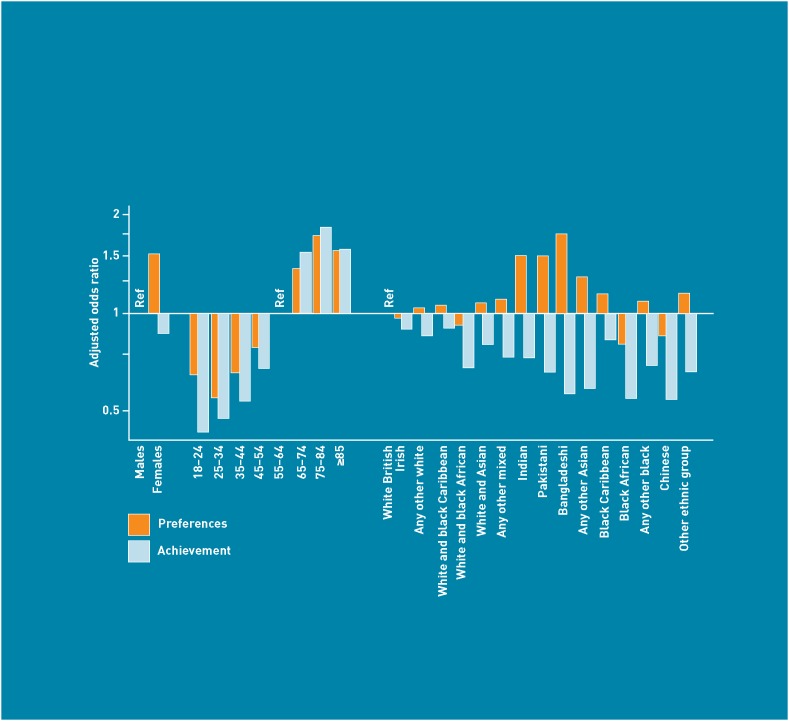
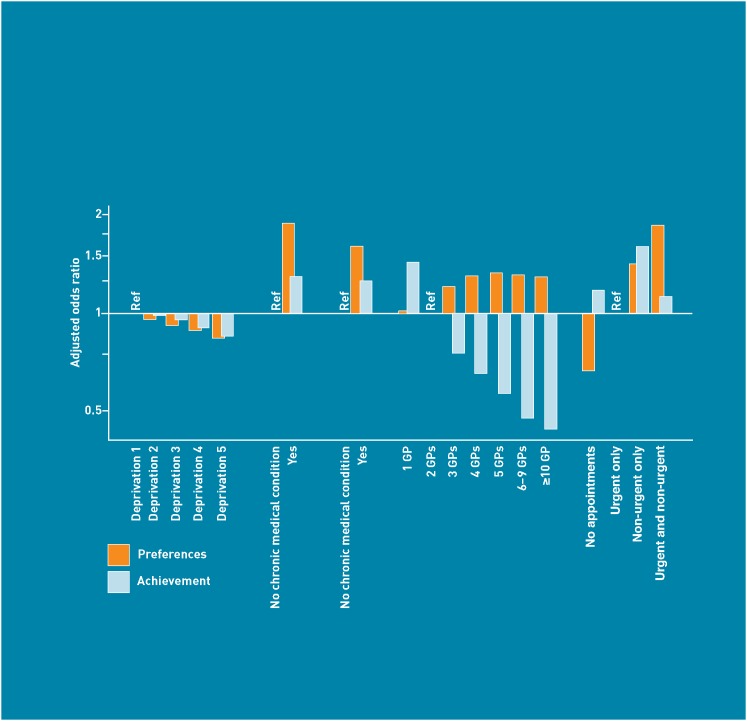
In multivariate analysis, there was strong evidence that differences in the success of seeing a preferred doctor persist after adjusting for other factors (P<0.001 for all variables) (Table 3). Female patients were less likely to be successful than males in seeing the doctor of their preference (OR?=?0.87). This contrasts with older patients (OR?=?1.82 for age group 74–85?years compared to age group 55–64?years), those with a chronic medical (OR?=?1.29) or psychological/emotional condition (OR?=?1.25), and white patients, all of whom were more likely to be successful compared to their respective reference groups. Success in seeing a preferred doctor was also less common in deprived areas (OR?=?0.86 for most deprived compared to most affluent). Patients registered with larger practices were less likely to report that they could see a doctor of their choice most of the time (OR?=?0.48 for patients registered with practices with six to nine GPs compared to patients registered with practices with two GPs). Patients who requested only non-urgent appointments were more likely to be successful in seeing the doctor they prefer (OR?=?1.59 compared to patients requesting only urgent appointments). The odds ratios from Tables 2 and 3 are summarised in Figures 1 and 2.
Figure 1.
Adjusted odds ratios of having preference for seeing a particular doctor, and success in achieving it most of the time (sex, age, and ethnicity).
Figure 2.
Adjusted odds ratios of having preference for seeing a particular doctor, and success in achieving it most of the time (deprivation, chronic conditions, practice size, and appointment type).
DISCUSSION
Summary
About two-thirds of English patients have a preference for seeing a particular doctor, and of these patients, about three-quarters succeed in seeing their preferred doctor most of the time. This figure reflects some success of English general practice in meeting patients’ preferences for continuity, but also represents an opportunity for improvement for more than one-quarter of patients who found it difficult to see the doctor of their choice most of the time.
The preference for and success in seeing a particular doctor varied across patient groups. Females, older people, patients with long-term conditions, and South Asian individuals were more likely to prefer to see a particular doctor. Males, older patients, those with long-term conditions, and white patients reported more success in seeing their preferred doctor. Patients requesting urgent appointments were less likely to want to see a particular doctor. This may reflect a greater value placed by patients on swift access to medical care in the context of acute/urgent conditions. However, patients making urgent appointments were also less likely to succeed in doing so if they did want to see a particular doctor, reflecting the difficulty for practices in offering speedy access and continuity of care simultaneously.
In spite of their higher preference for relational continuity, South Asian individuals (and to a lesser extent females and patients from large practices) were less likely to be successful in seeing a particular doctor. One possible reason why South Asian patients report such disadvantage in seeing their preferred doctor could be that, for some, their first language is not English, making them less able to negotiate with the receptionists in order to book an appointment to see their preferred doctor.
The findings suggest that relational continuity is preferred and achieved more frequently by older patients and those with chronic conditions. These patients are more likely to request appointments in advance (for example, for managing a chronic condition) compared to younger healthier patients (who are likely to request appointments for acute conditions). However, because the study analysis was adjusted for appointment type, it is not likely that the observed relation between age and health conditions on one side and preferring and achieving continuity on the other is confounded by the type of appointments sought.
Although the analysis was restricted to the 98% of responders who reported that their practice had more than one doctor, one in eight responders were registered with a practice recorded by the NHS Information Centre as being ‘single-handed’. It is likely that these patients were attending practices formally recorded as having just one practice doctor but in which other doctors also worked from time to time (for example, in assistant, salaried or locum capacity).
Strengths and limitations
Most previous evidence on variation in continuity of care comes from relatively small studies. The present study increases the evidence base substantially, with its large national sample of 2.2?million responders. This allowed the independent associations of a large number of different sociodemographic variables to be estimated robustly.
Caution should be applied when interpreting the results of the GPPS, due to its relatively low response rate (39%), with the mean response rate being lower than 25% in some primary care trusts. Significant sociodemographic differences in patterns of non-response have also been reported, with males, young adults, and people living in deprived areas being under-represented among responders.17 To minimise the effect of selective non-response bias, all prevalence estimates were weighted using weights accounting for oversampling from small practices and from practices with low response rates, as well as for individual non-response patterns (by age, sex, and practice). These weights, however, would not have accounted for any systematic difference in experiences of continuity between responders and non-responders that were not associated with these factors.
Given the wording of question 15 (‘Is there a particular doctor you prefer to see at your GP surgery or health centre?’), it is possible that some patients who value continuity might reply ‘No’ to this question, because they have no preference for seeing a particular doctor. This might apply, for example, to individuals with no recent encounters or those who value all doctors equally but still prefer to see the same doctor regularly. To that extent, it is possible that the true prevalence of preference for interpersonal continuity was underestimated in this survey. Some patients may also have a preference to avoid seeing a specific doctor (as opposed to seeing a particular one). Other patients may have a preference for seeing different doctors for different aspects of their care, for example, a particular doctor for the management of a mental health condition and another for a physical health problem. Such preferences could affect patients’ desire for and success in achieving relational continuity. The wording of the survey questions, however (Box 2), does not allow examination of such aspects of preference for relational continuity.
Comparison with existing literature
In a paper produced by The King’s Fund,22 Freeman and Hughes used the 2008/2009 GPPS results to assess patients’ and clinicians’ perspectives on continuity. Descriptive analysis was performed to identify the proportion of patients who want to see their preferred doctor and those who could achieve this. Variation by age, sex, ethnicity, chronic disease status, and practice size was in agreement with the findings of the present study. The present study took the analysis further by conducting multivariate analyses to adjust for potential confounding by sociodemographic variables and appointment type. In accordance with previous research, the present study indicates that interpersonal continuity of care is valued by the majority of patients, especially females, older patients, and those with chronic diseases.7,8 Previous studies similarly suggest that males, older patients, white patients, and those registered with small practices are more likely to receive continuity of care.22–28
Implications for research and practice
Continuity of care can be viewed from the perspective of the patient, the doctor, or the healthcare system.29 This study takes the patient’s perspective and confirms that interpersonal continuity of care is valued by patients. However, by no means all patients expressed this preference. Some patients will prefer rapid access to appointments, but in other situations they may trade off rapid access for better continuity.30,31 This underscores an important aspect of healthcare quality, which is the need to provide a system that is sensitive to the needs of individual patients. Practices need to provide flexible appointment systems that offer a choice between continuity of care and rapid access to appointments.
However, there is a substantial minority of patients, up to one-quarter, who, most of the time, are not successful in seeing their preferred doctor. This is particularly important, given the evidence that continuity of care has declined in recent years.14–16 There are a number of possible reasons for this, including a focus on access and rapid appointments in the 2004 GP contract, increasing part-time working among doctors, and an increase in salaried (and potentially transient) GPs. The larger medical teams now present in many general practices also make personal continuity more difficult to achieve.32
There are clear messages here for the organisation of general practice. Continuity of care is valued by patients, and is said to be highly valued by GPs as well.33 If interpersonal continuity of care is indeed a core value of general practice, then more needs to be done to ensure that continuity is reflected in the service that practices offer to patients. Government, the Department of Health, and commissioning groups, in turn, should work together to support and incentivise practices to improve patients’ experiences through fostering continuity of care.
Funding
The work in part relates to part-fulfilment (dissertation) of the MPhil in Public Health course of the Department of Public Health and Primary Care, University of Cambridge, by Ahmed Aboulghate, who was a beneficiary of the BP Cambridge Scholarship for Egypt in collaboration with the Cambridge Overseas Trust. The analyses form part of a larger programme of research on the GP Patient Survey funded by the Department of Health. Georgious Lyratzopoulos is on a post-doctoral fellowship funded by the National Institute for Health Research (NIHR).
Ethical approval
Ethical approval was not required for this study.
Provenance
Freely submitted; externally peer reviewed.
Competing interests
Martin Roland and John Campbell act as academic advisers to Ipsos MORI for the English GP Patient Survey.
Acknowledgements
We acknowledge the assistance of Isla Kuhn in the literature review and identifying the available evidence.
Discuss this article
Contribute and read comments about this article on the Discussion Forum: http://www.rcgp.org.uk/bjgp-discuss
REFERENCES
- 1.Haggerty JL, Reid RJ, Freeman GK, et al. Continuity of care: a multidisciplinary review. BMJ. 2003;327(7425):1219–1221. doi: 10.1136/bmj.327.7425.1219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wall EM. Continuity of care and family medicine: definition, determinants, and relationship to outcome. J Fam Pract. 1981;13(5):655–664. [PubMed] [Google Scholar]
- 3.Starfield B. Continuous confusion? Am J Public Health. 1980;70(2):117–119. doi: 10.2105/ajph.70.2.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Banahan BF, Jr, Banahan BF., III Continuity as an attitudinal contract. J Fam Pract. 1981;12(4):767–778. [PubMed] [Google Scholar]
- 5.Freeman G. Continuity of care in general practice: a review and critique. Fam Pract. 1984;1(4):245–252. doi: 10.1093/fampra/1.4.245. [DOI] [PubMed] [Google Scholar]
- 6.Freeman G, Hjortdahl P. What future for continuity of care in general practice? BMJ. 1997;314(7098):1870–1873. doi: 10.1136/bmj.314.7098.1870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Turner D, Tarrant C, Windridge K, et al. Do patients value continuity of care in general practice? An investigation using stated preference discrete choice experiments. J Health Serv Res Policy. 2007;12(3):132–137. doi: 10.1258/135581907781543021. [DOI] [PubMed] [Google Scholar]
- 8.Pandhi N, Saultz JW. Patients’ perceptions of interpersonal continuity of care. J Am Board Fam Med. 2006;19(4):390–397. doi: 10.3122/jabfm.19.4.390. [DOI] [PubMed] [Google Scholar]
- 9.Saultz JW, Lochner J. Interpersonal continuity of care and care outcomes: a critical review. Ann Fam Med. 2005;3(2):159–166. doi: 10.1370/afm.285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hsiao CJ, Boult C. Effects of quality on outcomes in primary care: a review of the literature. Am J Med Qual. 2008;23(4):302–310. doi: 10.1177/1062860608315643. [DOI] [PubMed] [Google Scholar]
- 11.Hjortdahl P, Laerum E. Continuity of care in general practice: effect on patient satisfaction. BMJ. 1992;304(6837):1287–1290. doi: 10.1136/bmj.304.6837.1287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Weyrauch KF. Does continuity of care increase HMO patients’ satisfaction with physician performance? J Am Board Fam Pract. 1996;9(1):31–36. [PubMed] [Google Scholar]
- 13.Wasson JH, Sauvigne AE, Mogielnicki RP, et al. Continuity of outpatient medical care in elderly men. A randomized trial. JAMA. 1984;252(17):2413–2417. [PubMed] [Google Scholar]
- 14.Emanuel EJ, Dubler NN. Preserving the physician–patient relationship in the era of managed care. JAMA. 1995;273(4):323–329. [PubMed] [Google Scholar]
- 15.Guthrie B, Wyke S. Does continuity in general practice really matter? BMJ. 2000;321(7263):734–736. doi: 10.1136/bmj.321.7263.734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Campbell SM, Kontopantelis E, Reeves D, et al. Changes in patient experiences of primary care during health service reforms in England between 2003 and 2007. Ann Fam Med. 2010;8(6):499–506. doi: 10.1370/afm.1145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Roland M, Elliott M, Lyratzopoulos G, et al. Reliability of patient responses in pay for performance schemes: analysis of national General Practitioner Patient Survey data in England. BMJ. 2009;339:b3851. doi: 10.1136/bmj.b3851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Campbell J, Smith P, Nissen S, et al. The GP Patient Survey for use in primary care in the National Health Service in the UK — development and psychometric characteristics. BMC Fam Pract. 2009;10:57. doi: 10.1186/1471-2296-10-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ipsos MORI. Technical annex for the GP Patient Survey 2009/10 annual report. http://gp-patient.co.uk/results/annual/technicalannex200910 (accessed 7 Jun 2012).
- 20.Ipsos MORI. The GP Patient Survey. http://www.gp-patient.co.uk (accessed 7 Jun 2012).
- 21.Noble M, McLennan D, Wilkinson K, et al. The English Indices of Deprivation 2007. London: Department of Communities and Local Government, 2008; http://www.communities.gov.uk/documents/communities/pdf/733520.pdf (accessed 12 Ju1 2012). [Google Scholar]
- 22.Freeman G, Hughes J. Continuity of care and the patient experience. London: The King’s Fund; 2010. [Google Scholar]
- 23.Baker R, Boulton M, Windridge K, et al. Interpersonal continuity of care: a cross-sectional survey of primary care patients’ preferences and their experiences. Br J Gen Pract. 2007;57(537):283–289. [PMC free article] [PubMed] [Google Scholar]
- 24.Boulton M, Tarrant C, Windridge K, et al. How are different types of continuity achieved? A mixed methods longitudinal study. Br J Gen Pract. 2006;56(531):749–755. [PMC free article] [PubMed] [Google Scholar]
- 25.Mead N, Roland M. Understanding why some ethnic minority patients evaluate medical care more negatively than white patients: a cross sectional analysis of a routine patient survey in English general practices. BMJ. 2009;339:b3450. doi: 10.1136/bmj.b3450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Campbell JL, Ramsay J, Green J. Age, gender, socioeconomic, and ethnic differences in patients’ assessments of primary health care. Qual Health Care. 2001;10(2):90–95. doi: 10.1136/qhc.10.2.90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Campbell JL, Ramsay J, Green J. Practice size: impact on consultation length, workload, and patient assessment of care. Br J Gen Pract. 2001;51(469):644–650. [PMC free article] [PubMed] [Google Scholar]
- 28.Kontopantelis E, Roland M, Reeves D. Patient experience of access to primary care: identification of predictors in a national patient survey. BMC Fam Pract. 2010;11:61. doi: 10.1186/1471-2296-11-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Salisbury C, Sampson F, Ridd M, Montgomery A. How should continuity of care in primary health care be measured? Br J Gen Pract. 2009;50(561):e134–141. doi: 10.3399/bjgp09X420257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Guthrie B, Wyke S. Personal continuity and access in UK general practice: a qualitative study of general practitioners’ and patients’ perceptions of when and how they matter. BMC Fam Pract. 2006;7:11. doi: 10.1186/1471-2296-7-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gerard K, Salisbury C, Street D, et al. Is fast access to general practice all that should matter? A discrete choice experiment of patient preferences. J Health Serv Res Policy. 2008;13(suppl 2):3–10. doi: 10.1258/jhsrp.2007.007087. [DOI] [PubMed] [Google Scholar]
- 32.Wagner EH, Reid RJ. Are continuity of care and teamwork incompatible? Med Care. 2007;45(1):6–7. doi: 10.1097/01.mlr.0000253165.03466.e3. [DOI] [PubMed] [Google Scholar]
- 33.Ridd M, Shaw A, Salisbury C. ‘Two sides of the coin’ — the value of personal continuity of GPs: a qualitative interview study. Fam Pract. 2006;23(4):461–468. doi: 10.1093/fampra/cml010. [DOI] [PubMed] [Google Scholar]