Abstract
Chest pain is a common presenting symptom for emergency department (ED) patients, however a thorough cardiac evaluation can be difficult to complete within the ED setting. Implementation of a stand-alone unit for the evaluation of chest pain may improve care for chest pain patients. We designed a protocol for identifying patients without an acute coronary syndrome (ACS) and with low to intermediate likelihood of obstructive coronary artery disease (CAD). These patients were monitored in a stand-alone chest pain evaluation center (CPEC) staffed with a small group of providers and tested for CAD, if necessary. In the first six weeks of operation, 181 patients were evaluated in the CPEC. The prevalence of CAD risk factors was low. Of the 181 patients, 159 (88%) were discharged to home and 22 (12%) required admission to the hospital for further care. We compared the number of chest pain evaluations and admissions for first six weeks of operation to the same six week period from the two previous years. While ED chest pain evaluations increased 66% over the two year time frame, the proportion admitted to the hospital decreased from 53% to 42% (p < 0.0001). In conclusion, evidence-based evaluation of chest pain in patients without ACS and with low to intermediate likelihood of obstructive CAD can result in the significant majority of patients being discharged from the ED. Creation of a stand-alone CPEC in an academic hospital was associated with a significant reduction in hospital admissions.
Keywords: chest pain, emergency medicine, exercise tests, X-Ray Computed Tomography, clinical pathway
Introduction
Chest pain is an exceedingly common symptom for patients presenting to an emergency department (ED) setting. While scientific statements about the evaluation of chest pain have been published,1 solutions are varied and often dependent on the patient volumes and the institutional resources available at a given ED.2–5
In 2008 at the University of Florida, patients with chest pain discharged from the ED for outpatient follow-up were infrequently completing the testing as recommended. In response, the ED, Division of Cardiovascular Medicine, and Department of Radiology collaborated to develop an approach to offer computed tomography coronary angiography (CTCA) prior to discharge for suitable patients. Results of that study demonstrated not only low follow-up rates for outpatient treadmill testing, but a notable burden of coronary artery disease (CAD) diagnoses that were being missed by the outpatient follow-up strategy.6
Building on that approach, the interdisciplinary team from Emergency Medicine, Cardiology, and Radiology again collaborated to expand this CTCA based program into a stand-alone unit chest pain evaluation center (CPEC). We will describe the design of the CPEC, our initial patient experience, and future plans for the CPEC.
Methods
As previously noted, low-risk patients with chest pain infrequently complete recommended outpatient testing. Estimates of patient volume at our facility suggested that creating a stand-alone unit for the evaluation of chest pain would be a viable endeavor to address this limitation by offering cardiovascular testing on site in our ED. In addition to the CTCA program mentioned above, we have successfully used an interdisciplinary strategy with physicians, nurses, and technologists to optimize door-to-balloon care for patients with acute myocardial infarction. The collection of patient data related to this project was reviewed and approved by our institutional review board. Study data were collected and managed using REDCap electronic data capture tools hosted at the University of Florida.7 Data were analyzed using SPSS software version 20 (IBM; Armonk, NY).
Development of patient management strategy
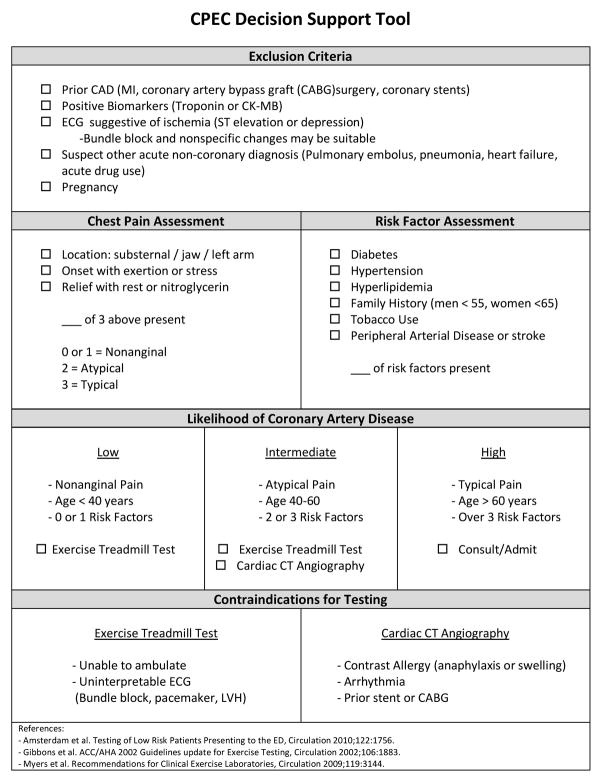
Because a primary goal of the CPEC is to improve the management of low-risk patients with acute chest pain, we selected this as the first patient population to focus on. Developing a strategy for managing these patients was built on three primary tasks: identifying patients most appropriate for the CPEC, selecting testing modalities most appropriate for this population, and directing management which should follow after testing is completed. (Figure 1)
Figure 1.
Flowsheet depicting the suggested strategy for guiding the selection of CPEC patients and testing modalities.
Many authors have developed and implemented a variety of strategies for identifying low-risk acute chest pain patients. For our CPEC, the goal was to identify patients not having an acute coronary syndrome to determine if their symptoms were due to obstructive coronary artery disease. We elected to use serial electrocardiograms and cardiac biomarker testing to establish a patient population at low risk of ACS. We used published guidelines and scientific statements to develop our strategy for test selection.1, 8–11 To estimate the likelihood that a patient’s symptoms were due to obstructive CAD, we constructed risk categories based on criteria developed by Diamond and Forrester.12 We incorporated known cardiac risk factors as additional criteria to stratify patients into low, intermediate, and high likelihood of having obstructive CAD.
With patients categorized by their likelihood of CAD, we next needed to determine which testing modalities would be most suitable for our population. Exercise treadmill testing (ETT) has been used for decades to expose cardiac ischemia, and is a cornerstone of many chest pain units. For patients who cannot exercise or those requiring most accurate testing, we needed to select at least one additional noninvasive method for diagnosing CAD. The physical plant, availability of personnel and established workflow patterns of our facility made both nuclear perfusion imaging and stress echocardiography unfavorable. We selected CTCA as the primary noninvasive imaging modality because the 320-detector computed tomography scanner at our facility is proximal to our CPEC and CTCA is an established method for rapid, accurate testing of acute chest pain patients.13–15
Staffing and Training
To achieve consistency in the application of our patient management strategy, we elected to train a small group of nurse practitioners and physician assistants to serve as the clinical leaders in our CPEC. Prior to opening the unit, the group went through three weeks of orientation and training focused on acute cardiac care and on the assessment of cardiac ischemia. These clinical leaders were supervised in performing at least 50 treadmill stress tests prior to performing them independently.16 Since opening the CPEC, we continue to hold regular in-service training for our clinical leaders where we debrief recent patient care scenarios as a group and review current literature in cardiac and emergency medicine.
Physical Plant
Our CPEC is located in the ED, in an area physically separated from the general patient care areas, with a total of 8 private and semi-private bed spaces. An exercise treadmill is located within the CPEC and studies are performed throughout normal business hours with immediate interpretation available by the Cardiology service. CTCA are performed on a scanner located within 100 yards of the CPEC.
Integration to existing patient workflow
The most typical route for a patient to take into the CPEC is as follows. After ambulatory arrival or via emergency medical services, patients go through a traditional triage process and are assigned a bed-space in the main ED. An electrocardiogram and point-of-care biomarker assays are promptly performed. If neither test shows evidence of ischemia, and the patient has low to intermediate pretest likelihood of obstructive coronary artery disease, the patient is transferred to the CPEC for further management. This opens a bed-space in the main ED for another patient and the remainder of the cardiac evaluation is performed in the CPEC, without need for direct involvement by the supervising ED attending physician. Serial biomarkers and electrocardiograms are performed at a time interval appropriate for the patient’s onset of symptoms, usually after six to eight hours after arrival. The clinical leader assesses the patient and selects, as needed, the appropriate modality to test for coronary artery disease. Once the additional testing and serial assessment of ischemia is completed, a disposition is determined and the patient is either admitted for further evaluation or discharged to home. Outpatient follow-up is arranged as needed.
CPEC Registry
We have established an institutional review board approved prospective patient registry for patients evaluated using the management strategy described above. This registry includes a thorough assessment of the patient’s complaint and the effect on daily activity. Several standardized, validated survey instruments are self-administered by the patients. These instruments assess daily activity (Duke Activity Status Index),17 angina severity (Seattle Angina Questionnaire),18 depression (Patient Health Questionnaire-9),19 anxiety (Generalized Anxiety Disorder-7),20 gastroesophageal reflux disease (GERD Symptom Frequency Questionnaire),21 health literacy,22 and quality of life.23 Clinical outcomes including return ED visits, follow-up with a primary care physician, and myocardial infarction or hospitalization will be assessed by phone interviews conducted 30 days and 6 months after the index visit.
Results
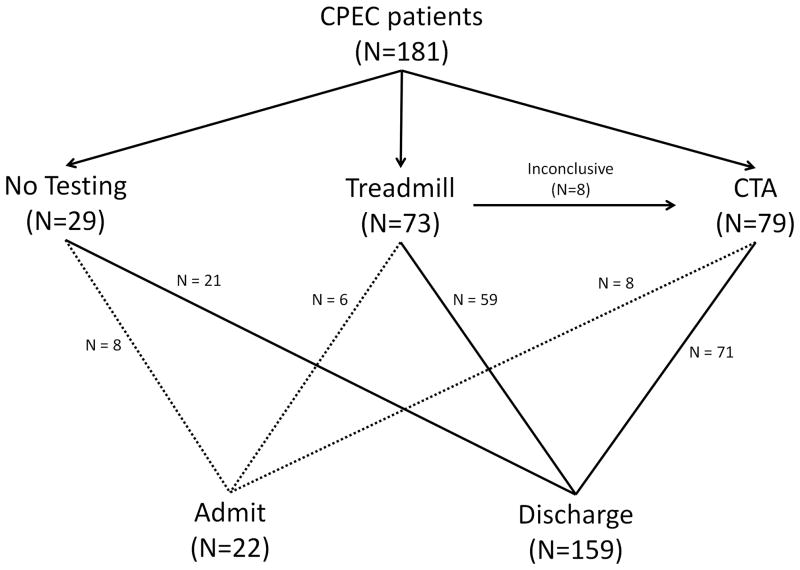
During the first six weeks of operation, 181 patients were seen in the CPEC. Subjects are categorized in Table 1 based on the initial testing strategy chosen, no test (n=29), ETT (n=73), or CTCA (n=79). Tobacco and alcohol use were common, however other cardiovascular risk factors were uncommon. For the no test group, the primary reasons that no test was ordered were presence of contraindications to both ETT and CTCA or having a noncardiac diagnosis made. No subjects were diagnosed as having an acute coronary syndrome. Disposition for each patient group is depicted in Figure 2. Ultimately, 159 patients (88%) were discharged from the unit while 22 (12%) required admission to the hospital.
Table 1.
| No Test (n=29) | Treadmill (n=73) | CTCA (n=79) | ||||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| Female | 15 | 51.7% | 34 | 46.6% | 45 | 57.0% |
| Alcohol use | 12 | 41.4% | 27 | 37.0% | 32 | 40.5% |
| Tobacco use | 11 | 37.9% | 15 | 20.5% | 27 | 34.2% |
| Depression | 2 | 6.9% | 3 | 4.1% | 4 | 5.1% |
| Anxiety | 3 | 10.3% | 2 | 2.7% | 5 | 6.3% |
| GERD | 1 | 3.4% | 4 | 5.5% | 10 | 12.7% |
| Diabetes | 0 | 0.0% | 7 | 9.6% | 7 | 8.9% |
| Stroke | 1 | 3.4% | 1 | 1.4% | 0 | 0.0% |
| Hyperlipidemia | 2 | 6.9% | 6 | 8.2% | 8 | 10.1% |
| Hypertension | 8 | 27.6% | 13 | 17.8% | 15 | 19.0% |
| Age, years (median) | 42 | 42 | 48 | |||
CTCA: computed tomography coronary angiography, GERD: gastroesophageal reflux disease
Figure 2.
Diagram depicting the initial patient cohort, the testing modality selected, and the disposition for each patient. The dashed lines represent admitted patients while solid lines represent patients discharged from the CPEC.
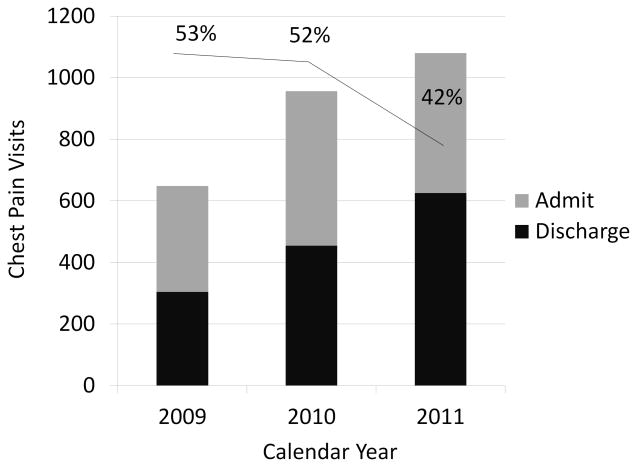
We reviewed data on all ED patients with chest pain to determine the effect of the CPEC on overall admission trends. We determined the number of patients seen by the entire ED for a chief complaint of chest pain and the proportion of those who were admitted during the first six weeks of CPEC operation during 2011. This was compared to data from the same six calendar weeks in 2010 and 2009. From 2009 to 2011, the number of chest pain evaluations increased by 66%. (Figure 3) In 2009 and 2010, the proportion of chest pain patients admitted was 53% and 52%, however for 2011, the proportion was reduced to 42%. (2010 vs. 2011, p < 0.0001)
Figure 3.
Each bar represents volume of patients with a primary symptom of chest pain for the same six week time frame from 2009, 2010, and 2011. The dark bars represent the proportion of patients who were discharged and the gray bars are the proportion admitted from the ER. The line at the top of the graph shows the percentage of patients admitted and the drop from 2010 to 2011.
Discussion
We have described the process and initial results of our experience opening a dedicated unit for the evaluation of chest pain in an academic ED. The observed reduction in hospital admissions was immediate and is promising for the future impact of the CPEC.
The use of dedicated units for the evaluation of chest pain in the ED is not a novel concept and descriptions of such units date back over many years. Chest pain units, however, are not warranted in every hospital setting and several challenges exist to their implementation. The utility of chest pain units requires having a large enough patient population to warrant a dedicated unit. ED’s differ from other hospital units in being open all day long. Hospital resources and cardiac testing are not always available for extended hours, and even less commonly available throughout the day. Cardiac testing modalities are usually under the control of departments other than the ED, and healthy cooperative relationships are necessary to be successful at interfacing across silos of patient care. Another hurdle is control of referrals to the unit and the selection of patients appropriate to the resources available. Creation of a stand-alone unit also creates divisions of labor that must be carefully considered in advance.
We have been pleased with the development that our clinical leaders have demonstrated in their short tenure in the CPEC. While none had prior experience with specialized cardiac care, they have rapidly acquired the skills necessary to independently supervise treadmill testing and to think beyond the proscribed patient management strategy to incorporate other cardiac testing as appropriate. Limited evidence exists regarding the appropriate training necessary for independent performance of ETTs. This topic warrants further study. Additionally, our leaders have been appropriately identifying patients who do not need any additional testing. Prior to opening the CPEC concerns were voiced about overuse and inappropriate testing. Anecdotally, this has not been a major concern and we will study it formally with our prospective registry.
Future Directions
Based on the CPEC experience and observing the adaptation of our clinical leaders, we are planning options for how to expand the eligible patient population for our dedicated unit. Organizations such as the Society for Chest Pain Centers have recognized the utility of providing other early, advanced cardiac care for arrhythmias and heart failure in the ED setting. We have explored these diagnoses as well as expanding the evaluation of chest pain beyond low to intermediate risk patients. The previously described prospective registry will provide ample opportunity for future publication and help guide interventions in the design and management of our CPEC. Formal cost-benefit analysis is beyond the scope of this manuscript, but is another topic we hope to address.
Conclusion
An evidence-based patient management strategy focused on patients with low to intermediate cardiac risk factors and using on-site cardiac testing can immediately and significantly reduce hospital admissions. Future research on this patient population will provide insight on the relationship between noncardiac illnesses and the evaluation of chest pain.
Acknowledgments
Sources of support: Data collection was supported in part by the Clinical and Translational Science Institute (NIH grant 1UL1RR029890)
Sources of funding: none to disclose
Abbreviations
- CAD
coronary artery disease
- CPEC
chest pain evaluation center
- CTCA
computed tomography coronary angiography
- ED
emergency department
- ETT
exercise treadmill test
References
- 1.Amsterdam EA, Kirk JD, Bluemke DA, et al. Testing of low-risk patients presenting to the emergency department with chest pain: a scientific statement from the American Heart Association. Circulation. 2010 Oct 26;122(17):1756–1776. doi: 10.1161/CIR.0b013e3181ec61df. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rubinshtein R, Halon DA, Gaspar T, et al. Usefulness of 64-slice cardiac computed tomographic angiography for diagnosing acute coronary syndromes and predicting clinical outcome in emergency department patients with chest pain of uncertain origin. Circulation. 2007 Apr 3;115(13):1762–1768. doi: 10.1161/CIRCULATIONAHA.106.618389. [DOI] [PubMed] [Google Scholar]
- 3.Fesmire FM, Hughes AD, Fody EP, et al. The Erlanger chest pain evaluation protocol: a one-year experience with serial 12-lead ECG monitoring, two-hour delta serum marker measurements, and selective nuclear stress testing to identify and exclude acute coronary syndromes. Ann Emerg Med. 2002 Dec;40(6):584–594. doi: 10.1067/mem.2002.129506. [DOI] [PubMed] [Google Scholar]
- 4.Kirk JD, Diercks DB, Turnipseed SD, Amsterdam EA. Evaluation of chest pain suspicious for acute coronary syndrome: use of an accelerated diagnostic protocol in a chest pain evaluation unit. Am J Cardiol. 2000 Mar 9;85(5A):40B–48B. doi: 10.1016/s0002-9149(00)00755-4. discussion 49B. [DOI] [PubMed] [Google Scholar]
- 5.Goodacre S, Locker T, Arnold J, Angelini K, Morris F. Which diagnostic tests are most useful in a chest pain unit protocol? BMC Emerg Med. 2005 Aug 25;5:6. doi: 10.1186/1471-227X-5-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Winchester DE, Jois P, Kraft SM, Wymer DC, Hill JA. Immediate computed tomography coronary angiography versus delayed outpatient stress testing for detecting coronary artery disease in emergency department patients with chest pain. Int J Cardiovasc Imaging. 2011 Apr 19; doi: 10.1007/s10554-011-9870-x. [DOI] [PubMed] [Google Scholar]
- 7.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009 Apr;42(2):377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Budoff MJ, Achenbach S, Blumenthal RS, et al. Assessment of coronary artery disease by cardiac computed tomography: a scientific statement from the American Heart Association Committee on Cardiovascular Imaging and Intervention, Council on Cardiovascular Radiology and Intervention, and Committee on Cardiac Imaging, Council on Clinical Cardiology. Circulation. 2006 Oct 17;114(16):1761–1791. doi: 10.1161/CIRCULATIONAHA.106.178458. [DOI] [PubMed] [Google Scholar]
- 9.Taylor AJ, Cerqueira M, Hodgson JM, et al. ACCF/SCCT/ACR/AHA/ASE/ASNC/SCAI/SCMR 2010 Appropriate Use Criteria for Cardiac Computed Tomography. A Report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, the Society of Cardiovascular Computed Tomography, the American College of Radiology, the American Heart Association, the American Society of Echocardiography, the American Society of Nuclear Cardiology, the Society for Cardiovascular Angiography and Interventions, and the Society for Cardiovascular Magnetic Resonance. Circulation. 2010 Oct 25; doi: 10.1016/j.jcct.2010.11.001. [DOI] [PubMed] [Google Scholar]
- 10.Gibbons RJ, Balady GJ, Bricker JT, et al. ACC/AHA 2002 guideline update for exercise testing: summary article. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Update the 1997 Exercise Testing Guidelines) Journal of the American College of Cardiology. 2002;40(8):1531–1540. doi: 10.1016/s0735-1097(02)02164-2. [DOI] [PubMed] [Google Scholar]
- 11.Myers J, Arena R, Franklin B, et al. Recommendations for clinical exercise laboratories: a scientific statement from the american heart association. Circulation. 2009 Jun 23;119(24):3144–3161. doi: 10.1161/CIRCULATIONAHA.109.192520. [DOI] [PubMed] [Google Scholar]
- 12.Diamond GA, Forrester JS. Analysis of probability as an aid in the clinical diagnosis of coronary-artery disease. N Engl J Med. 1979 Jun 14;300(24):1350–1358. doi: 10.1056/NEJM197906143002402. [DOI] [PubMed] [Google Scholar]
- 13.Goldstein JA, Gallagher MJ, O’Neill WW, Ross MA, O’Neil BJ, Raff GL. A randomized controlled trial of multi-slice coronary computed tomography for evaluation of acute chest pain. Journal of the American College of Cardiology. 2007;49(8):863–871. doi: 10.1016/j.jacc.2006.08.064. [DOI] [PubMed] [Google Scholar]
- 14.Hoffmann U, Bamberg F, Chae CU, et al. Coronary computed tomography angiography for early triage of patients with acute chest pain: the ROMICAT (Rule Out Myocardial Infarction using Computer Assisted Tomography) trial. J Am Coll Cardiol. 2009 May 5;53(18):1642–1650. doi: 10.1016/j.jacc.2009.01.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Litt HI, Gatsonis C, Snyder B, et al. CT Angiography for Safe Discharge of Patients with Possible Acute Coronary Syndromes. N Engl J Med. 2012 Mar 26; doi: 10.1056/NEJMoa1201163. [DOI] [PubMed] [Google Scholar]
- 16.Rodgers GP, Ayanian JZ, Balady G, et al. American College of Cardiology/American Heart Association Clinical Competence Statement on Stress Testing. A Report of the American College of Cardiology/American Heart Association/American College of Physicians-American Society of Internal Medicine Task Force on Clinical Competence. Circulation. 2000 Oct 3;102(14):1726–1738. doi: 10.1161/01.cir.102.14.1726. [DOI] [PubMed] [Google Scholar]
- 17.Hlatky MA, Boineau RE, Higginbotham MB, et al. A brief self-administered questionnaire to determine functional capacity (the Duke Activity Status Index) Am J Cardiol. 1989 Sep 15;64(10):651–654. doi: 10.1016/0002-9149(89)90496-7. [DOI] [PubMed] [Google Scholar]
- 18.Spertus JA, Winder JA, Dewhurst TA, et al. Development and evaluation of the Seattle Angina Questionnaire: a new functional status measure for coronary artery disease. J Am Coll Cardiol. 1995 Feb;25(2):333–341. doi: 10.1016/0735-1097(94)00397-9. [DOI] [PubMed] [Google Scholar]
- 19.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001 Sep;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Spitzer RL, Kroenke K, Williams JB, Lowe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006 May 22;166(10):1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- 21.Pare P, Meyer F, Armstrong D, Pyzyk M, Pericak D, Goeree R. Validation of the GSFQ, a self-administered symptom frequency questionnaire for patients with gastroesophageal reflux disease. Can J Gastroenterol. 2003 May;17(5):307–312. doi: 10.1155/2003/530984. [DOI] [PubMed] [Google Scholar]
- 22.Peterson PN, Shetterly SM, Clarke CL, et al. Health literacy and outcomes among patients with heart failure. JAMA. 2011 Apr 27;305(16):1695–1701. doi: 10.1001/jama.2011.512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ried LD, Tueth MJ, Handberg E, Nyanteh H. Validating a self-report measure of global subjective well-being to predict adverse clinical outcomes. Qual Life Res. 2006 May;15(4):675–686. doi: 10.1007/s11136-005-3515-2. [DOI] [PubMed] [Google Scholar]