Abstract
Uncomplicated chronic rhinosinusitis (CRS) is generally treated with medical therapy initially and surgery is contemplated only after medical therapy has failed. However, there is considerable variation in the medical treatment regimens used and studies defining their efficacy are few. The aim of this study was to determine the proportion of patients treated medically who responded sufficiently well so that surgery was not required. Subgroup analysis to identify clinical features that predicted a favorable response to medical therapy was also performed. Eighty patients referred to the Otorhinolaryngology Clinic at North Shore Hospital were treated with a standardized medical therapy protocol (oral prednisone for 3 weeks, oral antibiotics and ongoing saline lavage and intranasal budesonide spray). Symptom scores were collected before and after medical therapy. Clinical features such as presence of polyps, asthma, and aspirin hypersensitivity were recorded. Failure of medical therapy was defined as the persistence of significant CRS symptoms, and those patients who failed medical therapy were offered surgery. Follow-up data were available for 72 (90%) patients. Of this group, 52.5%, (95% CI, 42.7%, 62.2%) failed to respond adequately to medical therapy and were offered surgery. The remaining patients (37.5%) were successfully treated with medical therapy and did not require surgery at the time of follow-up. The premedical therapy symptom scores were significantly higher than the postmedical therapy symptom scores (p < 0.01). The symptom scores of those patients postmedical therapy who proceeded to have surgery were significantly higher than the group who responded well to maximum medical therapy (MMT) and did not require surgery (p < 0.0001). There were no significant differences in the proportion of patients with asthma, aspirin sensitivity, or polyps between the groups failing or not failing MMT. In approximately one-third of patients with CRS, medical therapy improved symptoms sufficiently so that surgical therapy was avoided. Patients with more severe symptoms tended not to respond as well as those with less severe symptoms. Long-term follow-up is required for the group of responders to determine how many will eventually relapse.
Keywords: Antibiotics, chronic rhinosinusitis, corticosteroid, intranasal steroid, macrolides, maximal medical therapy, medical therapy, prednisone, saline irrigation, symptom
It is generally accepted that the treatment of chronic rhinosinusitis (CRS) should begin with medical therapy and that surgical procedure should be undertaken only after failure of medical therapy. There is no universally accepted protocol for medical therapy, and the success rates of various protocols have been reported to be between 50 and 95%.1
The goals of medical therapy are to reduce mucosal inflammation and swelling, control infection, and restore aeration of the nasal and sinus mucosa.2,3 Various combinations of medical therapy have been prescribed to achieve these goals. In a study of 145 patients, a combination of oral amoxicillin/clavulanate or clarithromycin for 4 weeks and a short course of high-dose prednisone, intranasal steroids, topical decongestant, and nasal saline irrigation were evaluated. Approximately one-third of the patients experienced poor or no response to medical therapy and surgery, 18% of patients experienced partial improvement of symptoms so that surgery was not required and just over one-half of the patients had complete resolution of their symptoms and signs of CRS.4 Overall, medical therapy was regarded as successful (surgery not required) in 69% of patients.
In a retrospective study of 40 patients, a regimen consisting of oral corticosteroids for 10 days, broad-spectrum antibiotics for 4–8 weeks, and topical therapy including intranasal steroids and nasal saline irrigations was used. Considerable symptomatic and radiological improvement was observed in the majority of the patients at 6–8 weeks postinitiation of medical therapy. However, 10% of patients required surgery because of inadequate response.5
A survey of American Rhinologic Society members was performed to determine which medical therapies were being used in CRS treatment. The most commonly treatments used were oral antibiotics, nasal topical steroids, oral steroids, and saline irrigation. The median length of antibiotic usage reported was 3–4 weeks and the median length of oral steroid use was 6–14 days.6
There is little consensus about the optimal choice of antibiotics for CRS or the duration of treatment. The efficacies of a number of antibiotics have been studied.7 Low-dose, long-term macrolides have been advocated for their combined antibiotic and anti-inflammatory actions, and improvements in symptom scores, nasal endoscopic appearance, and mucociliary function have been observed in patients with CRS.8
Although systemic corticosteroids are prescribed frequently for CRS, particularly for CRS with associated nasal polyposis, the evidence for their efficacy is surprisingly limited. A double-blind placebo randomized controlled trial reported improvement in nasal symptoms as well as nasal polyp size in symptomatic patients who have been treated with a short course of prednisolone (14 days of 50 mg) 9; however, short-term recurrence has been observed to often follow.10 A randomized controlled study investigating the efficacy of combined systemic and topical corticosteroid showed improvement in the nasal symptoms, polyp size, nasal patency, and reduction of CT scan scores. The study concluded that a short course (2 weeks) of oral prednisone was effective in alleviating nasal symptoms and that topical budesonide was capable of maintaining the effect of the oral steroid.11
Topical intranasal corticosteroid sprays are a mainstay long-term treatment of CRS, acting to reduce mucosal edema and inflammatory cell influx.2 Budesonide has been shown to have positive effects on symptom scores, nasal peak flow, and sense of smell,12 with associated reduction of tissue eosinophilia as well as polyp number and size.13
Intranasal saline is a safe and effective treatment modality, often used along with intranasal corticosteroid in the management of CRS.14 Improvements in quality of life, reduction in postnasal drip, and mediators within nasal secretions have been observed.15
It is the practice in our institution to use a regimen consisting of oral antibiotics for a minimum of 3 weeks, oral prednisone tapering over 3 weeks; intranasal corticosteroid; and saline lavage via sinus rinse device. We wished to determine how symptoms score improved with this regimen and how many patients were able to avoid surgery because of the symptom relief brought about by the regimen.
METHODS
The medical records of 80 patients with CRS who underwent treatment with medical therapy administered by two rhinologists in the Otorhinolaryngology Clinic at North Shore Hospital between January 1 and December 31, 2009 were reviewed. Diagnosis of CRS was consistent with the 2003 CRS Task Force diagnostic criteria.16 Patients in whom surgery was clearly indicated without a trial of medical therapy were excluded from the trial.
The demographic details, symptom scores, comorbidities, radiological, and endoscopic findings of each patient were collected. Symptom scores consisted of a simple visual analog scale from 0 to 5 with 0 being minimal severity and 5 being very severe. Symptoms of nasal obstruction, anterior and posterior rhinorrhea, facial pain and pressure, and hyposmia were scored at each clinic visit by the patients before their clinic review. Radiological findings derived from a paranasal CT that supports a diagnosis of CRS include isolated or diffuse mucosal thickening and presence of air–fluid levels involving the sinuses. The extent of these changes can be quantified by the Lund Mackay score. Positive endoscopic findings refer to signs of sinonasal inflammation observed with nasal endoscopy or anterior rhinoscopy; this includes presence of discolored nasal drainage, nasal polyps, polypoid swelling with nasal endoscopy, or anterior rhinoscopy, erythema or edema of the middle meatus, or ethmoid bulla.
A standard regimen of medical therapy was prescribed to 80 patients with CRS. All patients were treated with oral antibiotics, (roxithromycin or doxycycline for a minimum of 3 weeks): a tapering dose of prednisone consisting of 30 mg daily for 1 week, 20 mg daily for 1 week, and then 10 mg daily for 1 week. Patients were started on topical budesonide nasal spray at 200 μg twice daily to each nostril as well as nasal saline washes delivered by the sinus rinse device.
The patients' symptom scores were evaluated 3 months after the initiation of medical therapy. Whether patients progressed to surgery after this time was largely based on the degree of resolution of their symptoms. Sufficient resolution so that surgery could be avoided was regarded as successful medical therapy. The group in whom surgery was not required was reviewed again at an average of 5 months later to evaluate the longevity of the effect of the medical therapy.
Patients' demography was described. Ninety-five percent confidence intervals were calculated for the groups responding and not responding to medical therapy. Paired t-test and signed-rank sum test were used for the comparison of symptom scores. General linear and logistic regression model was also used for studying the predictive factors of symptom scores and success of medical therapy. SAS 9.1 was used for the analysis (SAS Institute, Inc., Cary, NC).
RESULTS
Eighty consecutive patients with CRS and without exclusions completed the study. There were 50 male and 30 female patients with a mean age of 45 years (range, 17–74 years). Within our study group, 2.5% of patients were Maori, 6.25% were Pacific Islanders, 14% were Asian, 10% were Middle Eastern, and 55% were European. Ten percent of the patients had aspirin sensitivity, 40% were asthmatic patients, and 35% had nasal polyps. A minority (23%) had previous nasal surgery and 80% had positive endoscopic findings suggestive of CRS such as nasal polyps or mucopus.
After 3 months follow-up, 37.5% (95% confidence interval, 27.8%, 47.2%) of the patients reported sufficient improvement in their symptom score so that surgery was not required. Just over one-half (52.5%; 95% confidence interval, 42.7%, 62.2%) of the patients did not achieve satisfactory improvement in their symptom scores and therefore surgery was offered. Ten patients had incomplete data and were excluded from the analysis. Four patients had inadequate response to medical therapy but because of comorbidities or other extenuating circumstances (pregnancy) surgery was not offered.
The baseline symptom scores of the group who responded to medical therapy was 14 ± 2, which fell after a 3-month treatment period to 9 ± 2 (t-test, p < 0.002). The baseline symptom score of the group who failed to respond adequately to medical therapy was 16 ± 1, and after treatment this was 16 ± 2 (paired t-test, p = 0.91). After a mean of 5 months of additional follow-up (range, 1–10.4 months), the average symptom score of the medical treatment responding group was 8 ± 3, which was not significantly different from this group's symptom score at 3 months (signed-rank test, p = 0.24).
Relative younger ages, male gender, European ethnicity, presence of asthma, and positive endoscopic as well as CT findings were factors predictive of a need for surgery. Presence of polyps was not a predictive factor (Table 1).
Table 1.
Factors associated with outcome of surgery
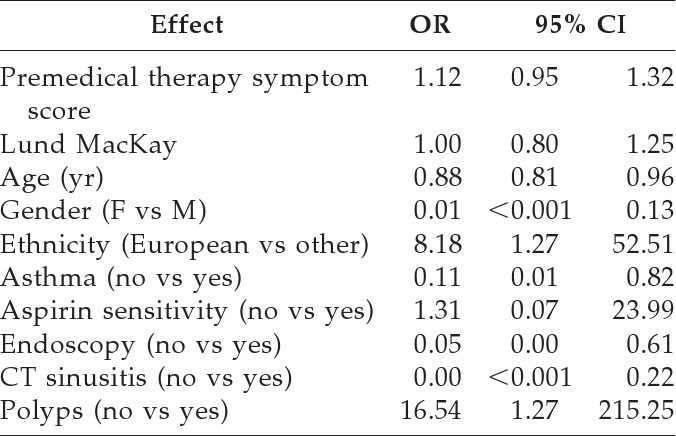
CI = confidence interval; OR = odds ratio.
DISCUSSION
It is generally accepted that CRS is treated initially with medical therapy with the aim of reducing symptoms, improving quality of life, and preventing disease progression or recurrence.3,17 Many different medical protocols have been used but none have been universally accepted.
The medical therapy prescribed for an individual patient may be influenced by previous treatments, patient referral patterns, and local bacterial sensitivities.1 In the present study, the standardized medical protocol consisted of doxycycline or roxithromycin for a minimum of 3 weeks, oral prednisone tapering over 3 weeks, and intranasal corticosteroid spray and saline lavage using the sinus rinse device continued until review. We found that medical therapy reduced symptoms sufficiently so that nearly 40% of patients felt they did not need surgical intervention after 3 months follow-up.
Other combinations of medical therapy have yielded variable results. In one series of 200 patients, with 9% <18 years of age, treated with 4 weeks of oral cefuroxime or amoxicillin/clavulanate, intranasal steroids, nasal irrigation, and topical decongestants, nasal mucosal swelling and purulent secretion were reduced markedly and only 6% of patients required surgery.18
In a retrospective study of 40 patients, symptoms and CT changes were assessed after oral prednisone for 10 days, (40 mg daily for 5 days followed by 20 mg daily for 5 days), broad-spectrum antibiotics for 4–8 weeks, nasal saline irrigation, and intranasal steroid. A relapse rate of 47.5% was observed at 3 months evaluation postmedical therapy requiring reinstitution of antibiotics and/or steroids. A 10% failure rate was reported, necessitating surgery.5 Association of nasal polyposis and previous sinus surgery were found to be linked with earlier relapse of sinusitis symptoms.5
A more recent study reported 145 patients treated with 4 weeks of clarithromycin or amoxicillin-clavulanate, a tapering course of oral steroids over 12 days, nasal saline irrigation, intranasal steroid, and topical decongestants. In just over one-half of the patients, there was complete resolution of symptoms at 2 months posttherapy, with no requirement for surgery in 69% of the patients.4 Facial pressure or pain, mucosal inflammation, and higher endoscopic severity grade were identified to be associated with failure of medical therapy.4
Several factors may contribute to the difference seen in our series and that of existing studies. The majority of our patients were referred by their primary care physicians, often with a long history of symptoms that had been resistant to previous trials of medical therapy. In this preselected group, the failure of medical therapy would be expected to be higher than self-referred patients.
Direct comparison between studies is challenging because of different study design variables including doses, duration, and inclusion of additional agents; follow-up period; and definitions of what constitutes failure of medical therapy. The majority of American Rhinologic Society members surveyed (61.0%) consider that medical failure was disease on CT scan with persistent symptoms, and many (41.9%) regarded medical failure was disease with improved but persistent symptoms.
Nasal polyposis has been previously reported to be an important predictor of sinusitis relapse.5 We found a tendency toward polyp patients being more likely to require surgery after a trial of medical therapy (p = 0.06).4 In our study patient group there was no association between Lund-Mackay score and symptom score severity (p = 0.34), a finding consistent with several other reports.4,5,18 Relatively younger age, male gender, presence of asthma, and positive endoscopic and CT findings (Table 1) were correlated with severity of symptom scores and were predictive of a need for surgery.
Our study has some limitations. Compliance with medical therapy was not measured, and poor compliance would presumably reduce efficacy. Follow-up data were not available for 10% of patients.
The decision to proceed to surgery was largely based on the patients' perspective that their response to medical therapy was not adequate. It is very difficult to objectify the basis of this decision, and it is vulnerable to patient and surgeon biases. However, the framework of the consultation was similar in all cases and the patients were asked how they wished to proceed in an open manner.
A longer period of follow-up especially in patients whose symptoms have improved sufficiently after the medical therapy so that surgery was not indicated, would offer a superior insight into the longevity of the medical therapy effect. For practical reasons we were limited to a period of several months to maximize completeness of follow-up.
The majority of the study patients with Samter's triad had not been desensitized at the time of their taking medical therapy. Aspirin desensitization has been shown to improve nasal congestion, sense of smell, and reduction in sinus infections. This effect is independent of maximal medical therapy, and may confound the result.19
The majority (52.5%) of our patients failed to achieve what they regarded as adequate control of their symptoms with medical therapy and therefore required sinus surgery. The combination of medical therapy and surgery shares a synergistic relationship in providing long-term disease control.
The challenge is to offer a medical therapy regimen that is effective while remaining safe and well tolerated by patients. Medical therapy for CRS will continue to evolve as our understanding of the disease process and pharmacotherapy advances.
CONCLUSION
In this series, medical therapy improved symptoms sufficiently so that nearly 40% of patients felt they did not require surgery. After a follow-up at 3 months, those patients who showed good symptomatic response to medical therapy were maintained on intranasal steroid sprays and saline irrigation. The beneficial effect of the medical therapy was persistent up to an average of 8 months follow-up. Endoscopic findings and a history of asthma were a prognostic factor for failure of medical therapy. Demographic factors including being older and of female gender were associated with favorable response.
ACKNOWLEDGMENTS
The authors thank Jasmin O'Sullivan for her effort in facilitating access to clinical records.
Footnotes
Presented at the 63rd Annual General and Scientific Meeting of the New Zealand Society of Otolaryngology–Head and Neck Surgery, Waitangi, New Zealand, March 2–5, 2010
The authors have no conflicts of interest to declare pertaining to this article
REFERENCES
- 1. Lund VJ. Maximal medical therapy for chronic rhinosinusitis. Otolaryngol Clin North Am 38:1301–1310, 2005 [DOI] [PubMed] [Google Scholar]
- 2. Gillespie MB, Osguthorpe JD. Pharmacologic management of chronic rhinosinusitis, alone or with nasal polyposis. Curr Allergy Asthma Rep 4:478–485, 2004 [DOI] [PubMed] [Google Scholar]
- 3. Glenis K, Scadding MA. Medical management of chronic rhinosinusitis. Immunol Allergy Clin North Am 24:103–118, 2004 [DOI] [PubMed] [Google Scholar]
- 4. Lal D, Scianna JM, Stankiewicz JA. Efficacy of targeted medical therapy in chronic rhinosinusitis and predicators of failure. Am J Rhinol Allergy 23:396–400, 2009 [DOI] [PubMed] [Google Scholar]
- 5. Subramanian HN, Schechtman KB, Hamilos DL. A retrospective analysis of treatment outcomes and time to relapse after intensive medical treatment for chronic sinusitis. Am J Rhinol 16:303–312, 2002 [PubMed] [Google Scholar]
- 6. Dubin MG, Liu C, Lin SY, Senior BA. American Rhinologic Society member survey on “maximal medical therapy” for chronic rhinosinusitis. Am J Rhinol 21:483–488, 2007 [DOI] [PubMed] [Google Scholar]
- 7. Sharp HJ, Denman D, Puumala S, Leopold DA. Treatment of acute and chronic rhinosinusitis in the United States, 1999–2002. Arch Otolaryngol Head Neck Surg 133:260–265, 2007 [DOI] [PubMed] [Google Scholar]
- 8. Yamada T, Fujieda S, Mori S, et al. Macrolide treatment decreased the size of nasal polyps and IL-8 levels in nasal lavage. Am J Rhinol 14:143–148, 2000 [DOI] [PubMed] [Google Scholar]
- 9. Hissaria P, Smith W, Wormald PJ, et al. Short course of systemic corticosteroids in sinonasal polyposis: A double-blind, randomized, placebo controlled trial with evaluation of outcome measures. J Allergy Clin Immunol 118:128–133, 2006 [DOI] [PubMed] [Google Scholar]
- 10. van Camp C, Clement PA. Results of oral steroid treatment in nasal polyposis. Rhinology 32:5–9, 1994 [PubMed] [Google Scholar]
- 11. Benitez P, Alobid I, De Haro J, et al. A short course of oral prednisone followed by intranasal budesonide is an effective treatment of severe nasal polyps. Laryngoscope 116:770–775, 2006 [DOI] [PubMed] [Google Scholar]
- 12. Tos M, Svendstrup F, Arndal H, et al. Efficacy of an aqueous and a powder formulation of nasal budesonide compared in patients with nasal polyps. Am J Rhinol 12:183–189, 1998 [DOI] [PubMed] [Google Scholar]
- 13. Holopainen E, Grahne B, Malmberg H, et al. Budesonide in the treatment of nasal polyposis. Eur J Respir Dis Suppl 122:221–228, 1982 [PubMed] [Google Scholar]
- 14. Harvey R, Hannan SA, Badia L, et al. Nasal saline irrigations of the symptoms of chronic rhinosinusitis. Cochrane Database Syst Rev 18:CD006394, 2007 [DOI] [PubMed] [Google Scholar]
- 15. Taccariello M, Parikh P, Darby Y, et al. Nasal douching as a valuable adjunct in the management of chronic rhinosinusitis. Rhinology 37:29–32, 1999 [PubMed] [Google Scholar]
- 16. Benninger MS, Ferguson BJ, Hadley JA, et al. Adult chronic rhinosinusitis: Definitions, diagnosis, epidemiology and pathophysiology. Otolaryngol Head Neck 129(suppl 1):S1–S32, 2003 [DOI] [PubMed] [Google Scholar]
- 17. Ragab SM, Lund VJ, Scadding G. Evaluation of the medical and surgical treatment of chronic rhinosinusitis: A prospective randomised controlled trial. Laryngoscope 114:923–930, 2004 [DOI] [PubMed] [Google Scholar]
- 18. McNally PA, White MV, Kaliner MA. Sinusitis in an allergist's office: Analysis of 200 consecutive cases. Allergy Asthma Proc 18:169–175, 1997 [DOI] [PubMed] [Google Scholar]
- 19. Stevenson DD, Hankammer MA, Mathison DA, et al. Aspirin desensitization treatment of aspirin-sensitive patients with rhinosinusitis-asthma: Long-term outcomes. J Allergy Clin Immunol 98:751–758, 1996 [DOI] [PubMed] [Google Scholar]


