To the Editor—Multidrug-resistant (MDR) infections are rapidly increasing worldwide, and, unfortunately, few new antimicrobials capable of treating these infections are under development [1, 2]. The emergence of infections for which there are limited treatment options represents a critical unmet medical need. In October 2011, we electronically surveyed the 1356 members of the Emerging Infections Network (EIN) about 3 areas of unmet medical need in the treatment of antibiotic-resistant infections.
Respondents ranked the severity of unmet medical need for different infections from 1 (least severe) to 5 (most severe). Respondents also ranked the importance of specific challenges related to the treatment of MDR infections from 1 (not important) to 5 (most important). Finally, they ranked 5 specific strategies designed to combat antibiotic-resistant infections in the order in which they felt would best aid in targeting these infections. Additional questions pertained to use of polymyxin B/E (colistin).
We received 562 responses (41.6%). The severity of unmet medical need was viewed as greatest for MDR gram-negative bacilli (mean score, 4.6), higher than for methicillin-resistant Staphylococcus aureus (MRSA), MDR tuberculosis, aspergillosis, and MDR gonorrhea (Figure 1A). The greatest challenge in the treatment of MDR infections was noted to be the limited number of new antimicrobials under development (mean score, 4.7) (Figure 1B). Respondents believed that the development of new antibacterials (mean score, 3.4) and more aggressive antimicrobial stewardship programs were the most important strategies in combating MDR infections (Figure 1C). Sixty-four percent of respondents reported using colistin during the previous year, 63% reported caring for a patient with an infection resistant to all available antibacterials, and 56% believe that the number of these untreatable infections is increasing.
Figure 1.
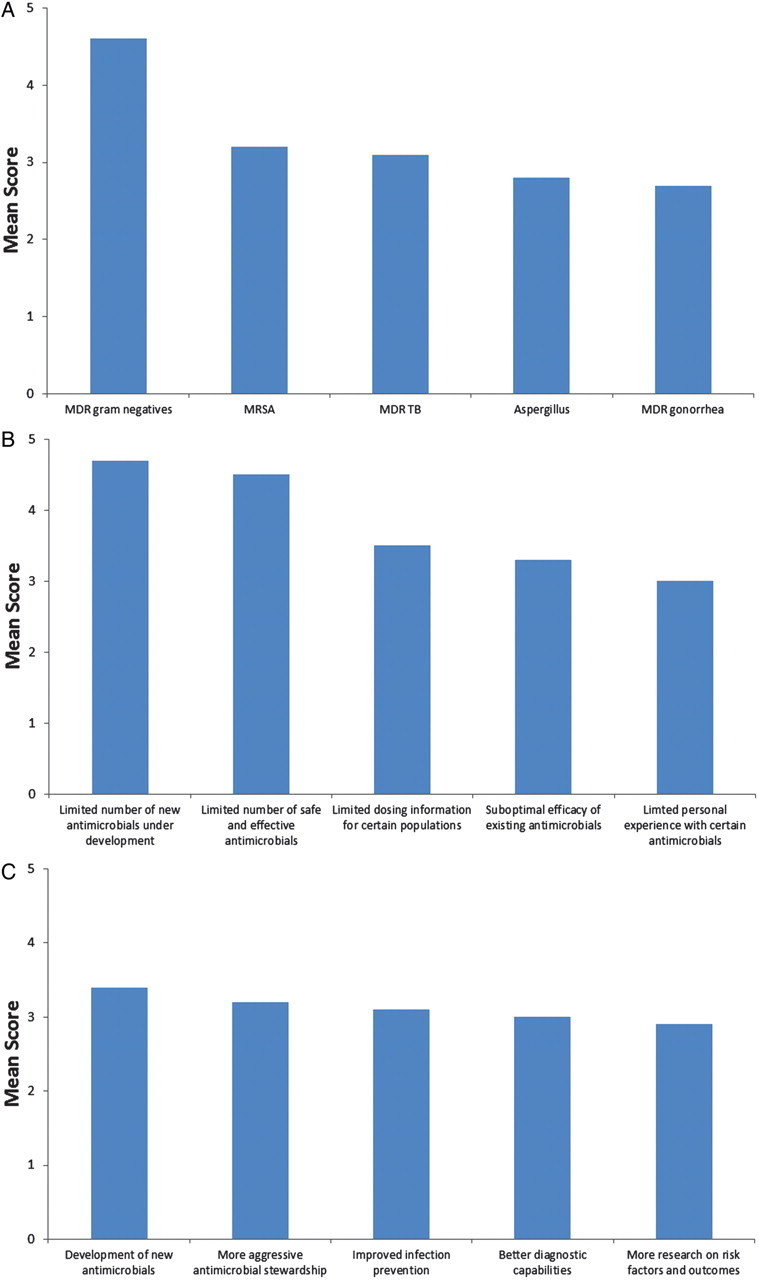
A, Mean score for rating severity of unmet medical need, ranging from 1 (least severe) to 5 (most severe). B, Mean score for rating importance of challenges in the treatment of multidrug-resistant infections, ranging from 1 (least important) to 5 (most important). C, Mean score for rating importance of various strategies in combating antibiotic-resistant infections, ranging from 1 (least important) to 5 (most important). Abbreviations: MDR, multidrug-resistant; MRSA, methicillin-resistant Staphylococcus aureus; TB, tuberculosis.
We found that management of infection due to MDR gram-negative bacteria represents the most severe unmet medical need in infectious diseases. In their practice, EIN members are experiencing an alarming increase in infections due to MDR gram-negative bacilli for which few and, in some cases, no effective therapies exist. In response, the Infectious Diseases Society of America has taken an active role in supporting national legislation that promotes control of antibiotic resistance and incentives for new drug development (the Generating Antibiotic Incentives Now Act). [3] Although MRSA and tuberculosis have drawn the attention of the public media, infectious diseases clinicians from the EIN believed that gram-negative bacilli represent a far greater unmet need. From the vantage of front-line physicians, the limited number of new antibacterials represents both the greatest limitation and the most important solution to combating this crisis.
Notes
Financial support. This work was supported by the National Institutes of Health and the Centers for Disease Control and Prevention (grants to P. M. P.).
Potential conflicts of interest. All authors: No reported conflicts.
All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1.Boucher HW, Talbot GH, Bradley JS, et al. Bad bugs, no drugs: no ESKAPE! An update from the Infectious Diseases Society of America. Clin Infect Dis. 2009;48:1–12. doi: 10.1086/595011. [DOI] [PubMed] [Google Scholar]
- 2.The Center for Disease Dynamics, Economics and Policy. Resistance Map. Available at: http://www.cddep.org/resistancemap . Accessed 28 January 2012. [Google Scholar]
- 3.Spellberg B, Blaser M, Guidos RJ, et al. Infectious Diseases Society of America (IDSA) Combating antimicrobial resistance: policy recommendations to save lives. Clin Infect Dis. 2011;(52(Suppl 5)):S397–428. doi: 10.1093/cid/cir153. [DOI] [PMC free article] [PubMed] [Google Scholar]


