Abstract
We analyzed alcohol involvement in 84,005 medically identified live discharges from hospitals in 20 states of the United States in 1997 for self-inflicted intentional injuries. Alcohol was involved in 27%. Men’s self-inflicted injuries involved alcohol significantly more often than women’s but men also drink more than women. Alcohol involvement rose and subsequently fell with age, with involvement above 30% for ages 30–55. Involvement fell precipitously by 27% below age 21, perhaps due to the 21-minimum legal drinking age.
Introduction
Suicide remains one of the leading causes of death in the United States (Heron et al., 2009). Alcohol abuse is considered a distal risk factor for suicide, with alcohol abuse patients having higher rates of suicide than both the general population and comparison clinical groups (Rossow et al, 2007; Potash et al., 2000; Moscicki, 1995). Alcohol use is also considered a proximal risk factor, in that alcohol use lowers inhibitions that may prevent suicidal behavior in individuals who are not alcoholics (Moscicki, 1995). A review of 37 studies from such varied sources as mortality data and psychological autopsies found alcohol involved in 10% to 69% of completed suicides, with a mean across studies of 37% (Cherpitel et al., 2004). An earlier meta-analysis (Smith et al., 1999) suggested that 29% of completed suicides involved alcohol intoxication (BAC ≥ 100 mg/dl).
Less is known about alcohol involvement in nonfatal suicide acts. Studies conducted in emergency rooms or trauma centers using both adult and pediatric populations and many types of suicide acts typically include modest numbers of cases. They suggest that perhaps 30% to 50% of hospital-admitted suicide acts involved alcohol (Borges et al., 2004; Cherpitel et al., 2004), with a range of 10% to 73% across studies. Powell et al. (2001) found a 26.5% alcohol involvement rate among 153 near-lethal suicide acts (76.5% of acts treated in the Emergency Department (ED)) in Houston TX, with an odds ratio of a suicide act given alcohol-positive of 8.0 relative to statistically matched community controls. Pooling data from seven case-crossover studies in four countries, Borges et al. (2004) find that 35.3% of 102 suicide acts treated in the ED were alcohol-involved, with recent alcohol consumption posing a relative risk of a suicide act of 9.6. In a case-control study, patients who recently consumed alcohol as measured with a breathalyzer upon admittance to an emergency room in Mexico City were at 90 times the relative risk of suicide attempt than a group of unintentional injury patients whose cause of trauma was not theoretically linked to alcohol consumption (Borges and Rosovsky, 1996). Further, recent alcohol consumption was a better suicide risk indicator than self-report of habitual alcohol consumption. Self-report of recent drunkenness has been associated with suicide attempts in youth (Brent, 1995; King et al., 2001) and alcohol abusers are more likely to attempt suicide (Gomberg, 1989; Rossow et al., 1999). These findings suggest that alcohol’s association with medically attended suicide attempts and with completions is similar.
Information is especially scarce on which demographic subgroups’ nonfatal suicide acts are most likely to involve alcohol. Although women more frequently attempt suicide, European ED data suggest that men are more likely to have used alcohol immediately prior to a poisoning or other suicide act then women (Prkacin et al., 2001). How alcohol involvement in suicide acts varies with age is also unclear. No published studies examining the relationship between ethnicity, alcohol consumption, and nonfatal suicide acts were found. In particular, no research has probed alcohol involvement in nonfatal suicide acts simultaneously by sex, age, and ethnicity.
This study examines the epidemiology of alcohol-related intentionally inflicted nonfatal injuries (hereafter, labeled suicide acts although the category is broader, as it was in most survivor studies cited above) in a large census of medically identified cases in the United States. The large case count allows us to isolate variations by sex, age, and ethnicity.
Birckmayer and Hemenway (1999) found youth suicide completions fell when the minimum legal drinking age rose to 21. If that association is causative, serious nonfatal suicide acts also should have declined. With recent advocacy to repeal the minimum drinking age, such buttressing evidence is increasingly important. This study adds to the correlational evidence.
Materials and Methods
A census of hospital discharge records from a geographically diverse convenience sample of 20 states was used to examine the relationships between sex, age, ethnicity, and alcohol-involved suicide attempts. This convenience sample included all states that made these data publicly available in 1997–1998 except Connecticut as its data were not affordable. The final sample included all 19 states where we could easily obtain deidentified 1997 cause-coded hospital discharge data, and where the data included victim age and sex as well: Arizona, California, Florida, Massachusetts, Maryland, Maine, Michigan, Nebraska, New Hampshire, New Jersey, New York, Pennsylvania, Rhode Island, South Carolina, Utah, Virginia, Vermont, Washington, and Wisconsin. Colorado data for 1998, the earliest year for which cause-coded hospital discharge data were available for that state, were also included. Using data from the 2000 U.S. Census, these 20 states represent an estimated 53.7% of the U.S. population. Similar to the 2000 U.S. Census, which was 49.1% male in the entire U.S. population and 49.0% male in the 20 states from which our data came, our sample of hospital discharges was 49.3% male. Validity checks were completed between states, and when needed, variables were recoded to produce uniform coding categories and value labels across states for variables such as discharge status and ethnicity. Analyses involving race/ethnicity excluded Maine, Nebraska, Utah, Washington, and Wisconsin. For these states, race/ethnicity data were either unavailable due to confidentiality concerns in states with a low census of minorities, or unusable for analysis due to inconsistencies in definition. Finally, re-admissions were identified when possible using information such as admission status or readmission codes, and were removed from the data set.
The 20-state Census included 84,005 records with ICD-9-CM diagnosis codes and external-cause-of-injury codes (E-codes) consistent with intentional self-inflicted nonfatal injury. In the United States, hospital admission for suicide acts is unique in that these cases are routinely screened for alcohol and other drugs, whereas other routine admissions are not. Toxicological data were available in the discharge record for at least 90.8% of the total sample. This includes virtually all poisonings, since toxicological screening is in the treatment protocol. However, positive toxicological screening was available for only 54.2% of traumatic injuries. For the remaining 45.8% of traumatic injuries, no mechanism existed to distinguish records with negative toxicological screenings from records without toxicological screenings, which suggests that reporting of alcohol involvement may be incomplete except for the poisonings. Of the 84,005 records with intentional self-inflicted nonfatal injury, the majority of the injuries were poisonings, with 70,120 records (83.5%) cause-coded as such; non-poisoning injuries accounted for 13,885 records, or 16.5% (with cutting or piercing accounting for 11.5%). Included in these 84,005 records with intentional self-inflicted nonfatal injury were 703 patients (0.83%) whose records listed both poisoning and trauma mechanisms. For purposes of analyzing suicide mechanisms, these patients were classified by the mechanism of the first-listed E code on the record. Ethnicity/race was available for 62,163 records, or 88.7% of those cases with hospital-admitted nonfatal poisoning suicide acts.
In addition to the 84,005 live discharges for suicide acts, 1,178 records indicated hospital admittance for suicide acts that resulted in death prior to discharge. Our analysis excludes those cases; they are unlikely to be representative suicide deaths. (Only 14.9% of 456 fatal poisonings and 8.2% of 722 fatal trauma cases were coded as alcohol-positive, but many of these crisis patients may not have been tested for alcohol).
All records having E codes consistent with intentional self-inflicted nonfatal injury were searched for diagnosis codes indicative of alcohol involvement. Records with ICD – 9 codes indicating alcohol intoxication (303.0, 790.3, V79.1), alcohol dependence (303.9), alcohol abuse (305.0), alcohol psychosis (291), alcohol poisoning (980.0), or alcohol deterrent poisoning (977.3) were flagged as cases that were alcohol involved. Additionally, records with E codes of E860.0 or E860.1, both indicative of unintentional alcohol poisoning were flagged. Flagged records were considered alcohol involved. Alcohol involvement was therefore a dichotomous variable (yes/no) indicating the presence or absence of alcohol on the medical record as indicated by ICD – 9 diagnosis or V or E codes.
To isolate the relative risk of alcohol involvement in medically identified poisoning suicide attempts by demographics, a logistic regression was used to examine the associations between alcohol involvement and sex, ethnicity/race, and age group. Because alcohol involvement in suicide attempts and suicide completions may differ and many fatalities never reach the hospital and are not alcohol-tested, fatalities were excluded. The large number of records supported a breakdown by sex within ethnic group. Age was grouped into 10-year increments except for the oldest and youngest groups. Ages 51 to 64 were grouped, as were ages 65 and up. The youngest age groups, 17 and under, and 18 to 20, were chosen because these groups have reduced alcohol access. Youth ages 18 to 20 are under the minimum legal drinking age; but because they potentially have greater alcohol access than youth under age 17, given drinking at college or with co-workers at day’s end, they were analyzed separately.
The sharp increase in alcohol involvement in poisoning suicide attempts between the ages of 20 and 21 suggested an impact of the minimum legal drinking age. A linear regression was used to estimate how lowering the minimum legal drinking age to 18 might impact alcohol involvement in suicide acts for youth ages 18 to 20 if the differential was caused by the age limitation. The regression trended the alcohol-involved rate of hospitalized suicide attempts by year of age for ages 21 to 30, then predicted the rates of alcohol involvement in suicide attempts for the 18–20 age group had the discontinuity at age 21 not occurred.
Results
As Table 1 shows, alcohol was involved in at least 22,707, or 27.0%, of the 84,005 hospitalized nonfatal suicide acts in these 20 states. Alcohol involvement for intentional nonfatal poisoning acts was 26.4%, and at least 30.3% for nonfatal non-poisoning suicide acts, based on the number of positive toxicological screenings available for non-poisoning suicide acts. Assuming all suicide survivors were screened, the percentage involving alcohol ranges from 23.6% for other/unspecified to 32.4% for cut/pierce. In 1,384 (1.65%) of the discharges, alcohol was listed as the primary poisoning substance.
Table 1.
Number of Live Hospital Discharges Resulting from Suicide Attempts and the Percentage that Were Alcohol Positive by Mechanism, 20 States
| Mechanism | Cases | Alcohol-Involved | % Alcohol-Positive of Those Definitely Tested | Drug-Involved, No Alcohol | % Alcohol-Positive Assuming All Were Tested |
|---|---|---|---|---|---|
| Total | 84,005 | 22,707 | 31.1% | 50,257 | 27.0% |
| Poisoning | 70,120 | 18,503 | 27.0% | 50,032 | 26.4% |
| Alcohol | 1,384 | 1,384 | 100.0% | 0 | 100.0% |
| Drug/medicine | 66,157 | 16,378 | 24.8% | 49,779 | 24.8% |
| Solid/liquid | 1,930 | 521 | 71.4% | 209 | 27.0% |
| Gas | 649 | 220 | 83.3% | 44 | 33.9% |
| Trauma | 13,885 | 4,204 | 94.9% | 225 | 30.3% |
| Strangle/suffocation | 768 | 209 | 94.6% | 12 | 27.2% |
| Submersion | 51 | 14 | 87.5% | 2 | 27.5% |
| Firearm/explosion | 953 | 257 | 93.8% | 17 | 27.0% |
| Cut/pierce | 9,613 | 3,111 | 94.6% | 177 | 32.4% |
| Jump – height | 620 | 169 | 97.7% | 4 | 27.3% |
| Other/unspecified | 1,880 | 444 | 97.2% | 13 | 23.6% |
Based on 1997 data for 19 States and 1998 data for Colorado
Admissions for nonfatal poisoning suicide acts with alcohol involvement varied modestly by day of the week and month of the year. Alcohol involvement was 28% on Saturday and Sunday but 25% on other days. A comparison of these percentages indicated statistically significant differences (z = 4.402, p < .0001). This difference may reflect an exposure differential. Similarly, alcohol involvement in nonfatal suicide acts peaked in the summer months of June, July, and August at 27% and was lowest in February and March at 23%. Again, these percentages were significantly different (z = 4.595, p < .0001).
Men’s nonfatal poisoning suicide acts involved alcohol 34.3% of the time, compared to 21.9% alcohol involvement in women’s acts (Chi-square = 1292.6, p < .0001). Alcohol involvement varied by ethnic/racial group, with Native Americans having the greatest percentage of alcohol-involved poisoning suicide acts (35.3%) and people of Asian/Pacific Island heritage having the lowest percentage (9.6%). As discussed below, exposure differences may cause this pattern.
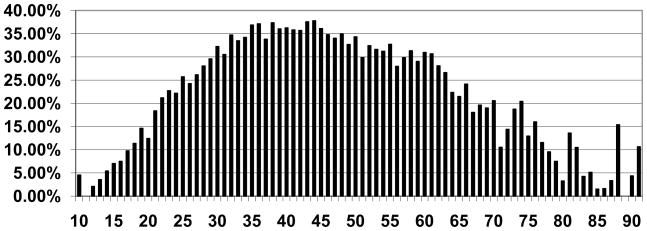
As Figure 1 shows, the percentage of alcohol involved hospital admitted poisoning suicide acts rose and subsequently fell with age, with involvement generally 30% and above for ages 30 through 61. The highest rate of alcohol involvement, above 35%, clustered in ages 35 to 45. Rates rose by 6 percentage points from age 20 to age 21 and decreased by 10 percentage points from age 70 to age 71.
Figure 1.
Percentage of Nonfatal Poisoning Suicide Hospital Admissions That Involved Alcohol by Year of Age
In the logistic regression examining nonfatal poisoning suicide acts, all sex/ethnic groups except Native American females were significantly different from the base group of white females ages 31 to 40 (max rescaled r2 = 0.092, percent concordant = 64.7; see Table 2). The 41 to 50 age group had the highest risk of alcohol involvement. Compared to white females, Native American males had the highest risk of alcohol involvement in poisoning suicide acts, followed by males of unknown or other ethnicity, white males, and Native American females. Asian Pacific females were least likely to be alcohol-involved, with Hispanic females and Asian Pacific males also at significantly lower risk than the base group of white females ages 31 to 40.
Table 2.
Alcohol Involvement in Hospitalized Nonfatal Suicide Attempts by Demographic Characteristics, 15 States
| Demographic Group | Suicide Discharges | % of Discharges Alcohol-Involved | Odds of Alcohol Involvement | 95% Confidence Limits |
|---|---|---|---|---|
| All | 62,163 | 26.0% | ||
| Female | 39,552 | 21.4% | ||
| White Female | 29,843 | 22.8% | 1.0 | -------- |
| Black, Non-Hispanic Female | 4,257 | 19.1% | 0.821a | 0.728 – 0.926 |
| Hispanic Female | 487 | 19.3% | 0.600b | 0.520 – 0.694 |
| Native American Female | 180 | 28.9% | 1.526 | 0.943 – 2.469 |
| Asian/Pacific Female | 843 | 7.1% | 0.296b | 0.202 – 0.433 |
| Other/Unknown Female | 3,942 | 16.7% | 0.795a | 0.688 – 0.919 |
| Male | 22,611 | 34.0% | ||
| White Male | 16,997 | 35.0% | 1.682b | 1.580 – 1.791 |
| Black, Non-Hispanic Male | 2,704 | 30.1% | 1.285b | 1.131 – 1.460 |
| Hispanic Male | 314 | 34.7% | 1.391b | 1.198 – 1.616 |
| Native American Male | 112 | 45.5% | 2.766b | 1.592 – 4.806 |
| Asian/Pacific Male | 308 | 16.6% | 0.688b | 0.443 – 1.068 |
| Other/Unknown Male | 2,176 | 32.7% | 1.687b | 1.444 – 1.971 |
| Ages 17 and under | 8,041 | 6.5% | 0.148b | 0.129 – 0.169 |
| Ages 18 to 20 | 4,610 | 12.4% | 0.278b | 0.243 – 0.318 |
| Ages 21 to 30 | 13,582 | 24.5% | 0.625b | 0.581 – 0.672 |
| Ages 31 to 40 | 17,041 | 34.6% | 1.0 | -------- |
| Ages 41 to 50 | 11,489 | 35.4% | 1.030 | 0.959 – 1.107 |
| Ages 51 to 64 | 4,617 | 30.1% | 0.804b | 0.726 – 0.890 |
| Ages 65 and older | 2,783 | 14.1% | 0.298b | 0.254 – 0.350 |
Significantly different from the base group (white females ages 31 to 40), p < .01
Significantly different from the base group (white females ages 31 to 40), p < .001
Based on 1997 data for 19 States and 1998 data for Colorado
From the linear regression trending alcohol involvement from age 21 to 30 (r2 = 0.942), the mean of the predicted values for ages 18 to 20, 16.3%, was 3.5% greater than the 12.8% mean for the rates for ages 18 to 20. Absent the minimum legal drinking age or other factors that caused alcohol involvement in suicide attempts to plunge below age 21, the alcohol involvement rate for ages 18 to 20 would increase by an estimated 3.5 percentage points. That means nonfatal alcohol-involved suicide admissions among this age group would rise by an estimated 27% (3.5/12.8). It is unclear if reducing the minimum drinking age would increase attempts or if those attempts would occur anyway but without alcohol involvement.
Discussion
The growth in accessible state hospital discharge censuses with injury cause codes offers a promising way to monitor the trend in alcohol involvement in hospitalized suicide acts. It suggests that 27% of hospitalized nonfatal suicide acts involve alcohol.
This study has several strengths. A 20-state census of roughly half of all live suicide discharges from US hospitals is analyzed. The large case count makes it possible to isolate the effects of different demographic characteristics; specifically, it allows simultaneous examination of sex and ethnicity. Additionally, because data are from hospital records, alcohol involvement is determined by toxicological screening, a more objective measure than self-report.
Still the study has limitations. Most importantly, the data are from 1997–1998. Because some people may be admitted for multiple suicide acts in a single year, the data cannot be used to compute accurate population-based rates. The likely readmission rate in six months (the average time post-attempt in one year of hospital discharge data) is probably 6%-8% (Beautrais, 2004, Conner et al., 2003, Owens et al., 2002) so our counts might be reduced by 1/16 to estimate rates. Hospitals also may fail to label some poisonings and injuries as self-inflicted, and alcohol involvement in those cases may differ from involvement in labeled cases. This problem is especially acute in the four states in the sample where more than 15% of injury discharges lacked cause codes: Florida, Maine, Michigan, and Virginia. Comparison between these four states and the remaining states in the sample revealed no statistically significant differences in rates of alcohol involvement in suicide acts. However, other states might have different alcohol involvement rates similar than the 20 geographically spread states studied. Moreover, the sample is somewhat thin in the Midwest.
Although the data are old, the pattern they describe seems to be stable over time and reasonably representative. On-line analysis of Drug Abuse Warning Network data from a nationally representative cluster sample of EDs (Ducharme et al., 2002), for example, reveals alcohol involvement rates of 30% in admitted suicide acts in both 1997 and 2006. That rate is consistent with the 27% rate reported here for 1997–1998.
The lack of routine alcohol and drug screening for admissions without intentional self-inflicted injury made a comparison between alcohol rates for hospital admitted suicide acts and other hospital admissions impossible. Consequently it is unclear how to interpret the observed differences. For example, the more frequent alcohol involvement in male than female suicide acts might occur simply because males drink more often than females. Similarly, mirroring the variation in alcohol involvement by ethnicity, on-line tabulation of the 1998 National Household Survey on Drug Abuse shows that Native Americans had the highest percentage of respondents reporting consuming 5 or more drinks in at least one drinking session during the past 30 days (41%), while people of Asian Pacific Island heritage reported the lowest percentage (14%). In contrast, alcohol involvement in hospitalized suicide attempts peaks at ages 30–60 while the number of people drinking five or more peaks at ages 18–30 and declines sharply by age 40. Furthermore, it is unclear how many of the alcohol-involved poisonings would not have occurred if alcohol had not been present, or how many that still occurred would have been less complex to manage.
Despite these limitations, these data increase knowledge about the relationship between demographic characteristics and alcohol involvement in nonfatal suicide acts. Age was strongly related to alcohol involvement in hospitalized attempts, increasing with age, hitting a plateau in mid-life, and then decreasing again with age. Although the rise in alcohol involvement rates to age 21 probably reflects increased access to alcohol, the continued rise in alcohol involvement after age 21 to the late 30s cannot be due to changes in the availability of alcohol. Because alcohol use disorders and heavy drinking (according to the NHSDA) are highest among adults aged 18 to 29 years (Grant, 1995), the continued rise in the number of alcohol-involved suicide acts after age 30 does not reflect increases in the number of alcoholic or heavy drinking adults. The different rates of alcohol exposure and alcohol involvement in suicide within age groups suggests that factors beyond alcohol exposure must be considered when trying to explain the high rates of alcohol involvement in suicidal acts for individuals aged 31 to 61. This continued increase may reflect, for some suicidal subgroups, alcohol abuse or dependence problems that continue and may be compounded over time. It also may reflect more serious consequences—financial, medical, and relational—that occur after longer periods of heavy alcohol use.
Access to alcohol appears to be a factor in limiting alcohol involvement in nonfatal poisoning suicide attempts for youth under the age of 21. This finding is consistent with prior research showing that the rise in minimum legal drinking age to 21 in 17 states was associated with an 8% reduction in suicide completions (Birckmayer and Hemenway, 1999). It buttresses that research and underlines the importance of retaining minimum drinking ages. Even among adults, reducing alcohol access and consumption is well-established as an effective approach to suicide prevention (Wasserman and Varnick, 1992).
In summary, alcohol involvement in hospital admitted nonfatal poisoning suicide acts is roughly double that of reported heavy alcohol consumption among the general population for all age groups over 30. The ratio between estimated alcohol exposure, as represented by reports of heavy alcohol use, and alcohol-involved suicide acts suggests that women of all ethnicities are more likely to have an alcohol-involved suicide act relative to their estimated alcohol exposure.
Acknowledgments
Funding: This study was supported in part by research grant 1 R01 MH60622-01 from the National Institute of Mental Health (NIMH), Bethesda, Maryland.
References
- Beautrais A. Further suicidal behaviour amongst medically serious suicide attempters. Suic Life-Threat Behav. 2004;34:1–11. doi: 10.1521/suli.34.1.1.27772. [DOI] [PubMed] [Google Scholar]
- Birckmayer J, Hemenway D. Minimum-age drinking laws and youth suicide, 1970–1990. Am J Pub Hlth. 1999;89:1365–1368. doi: 10.2105/ajph.89.9.1365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borges G, Rosovsky H. Suicide attempts and alcohol consumption in an emergency room sample. J Stud Alcohol. 1996;57:543–548. doi: 10.15288/jsa.1996.57.543. [DOI] [PubMed] [Google Scholar]
- Borges G, Cherpitel CJ, MacDonald S, Giesbrecht N, Stockwell T, Wilcox HC. A case-crossover study of acute alcohol use and suicide attempt. J Stud Alcohol Drugs. 2004;65:708–714. doi: 10.15288/jsa.2004.65.708. [DOI] [PubMed] [Google Scholar]
- Brent DA. Risk factors for adolescent suicide and suicidal behavior: Mental and substance abuse disorders, family environmental factors, and life stress. Suicide Life Threat Behav. 1995;25(Suppl):52–63. [PubMed] [Google Scholar]
- Cherpitel CJ, Borges GL, Wilcox HC. Acute alcohol use and suicidal behavior: a review of the literature. Alcohol Clin Exp Res. 2004;28(5 Suppl):18S–28S. doi: 10.1097/01.alc.0000127411.61634.14. [DOI] [PubMed] [Google Scholar]
- Conner KR, Langley J, Tomaszewski MS, Conwell Y. Injury hospitalization and risks for subsequent self-injury and suicide: a national study in New Zealand. American Journal of Public Health. 2003;93:1128–1131. doi: 10.2105/ajph.93.7.1128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ducharme L, McLeod C, Green J, Woodward A. DAWN Series M-4, (SMA) 02–3754. Rockville, MD: Substance Abuse and Mental Health Services Administration, Office of Applied Studies; 2002. Drug Abuse Warning Network: Development of a new design (methodology report) [Google Scholar]
- Foster SE, Vaughn RD, Foster WH, Califano JA. Alcohol consumption and expenditures for underage drinking and adult excessive drinking. JAMA. 2003;289:989–995. doi: 10.1001/jama.289.8.989. [DOI] [PubMed] [Google Scholar]
- Gomberg ES. Suicide risk among women with alcohol problems. Am J Public Health. 1989;79:1636–5. doi: 10.2105/ajph.79.10.1363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant B. Variations in the prevalence of alcohol use disorders and treatment by insurance status. Frontlines, Bethesda, MD: National Institute on Alcohol and Alcoholism and Foundation for Health Services Research; 1995. [Google Scholar]
- Heron M, Hoyert D, Murphy S, Xu J, Kochanek K, Tejada-Vera B. Deaths: Final data for 2006. National Vital Statistics Reports. 2009;57:14. [PubMed] [Google Scholar]
- King RA, Schwab-Stone M, Flisher AJ, Greenwald S, Kramer RA, Goodman SH, Lahey BB, Shaffer D, Gould MS. Psychosocial and risk behavior correlates of youth suicide attempts and suicidal ideation. J Am Acad Child Adoles Psychiat. 2001;40:837–846. doi: 10.1097/00004583-200107000-00019. [DOI] [PubMed] [Google Scholar]
- Moscicki EK. Epidemiology of suicidal behavior. Suicide Life Threat Behav. 1995;25:22–35. [PubMed] [Google Scholar]
- Owens D, Horrocks J, House A. Fatal and non-fatal repetition of self-harm. Systematic review. British Journal of Psychiatry. 2002;181:193–199. doi: 10.1192/bjp.181.3.193. [DOI] [PubMed] [Google Scholar]
- Potash JB, Kane HS, Chiu YF, Simpson SG, MacKinnon DF, McInnis MG, McMahon FJ, DePaulo JRJ. Attempted suicide and alcoholism in bipolar disorder: Clinical and familial relationships. Am J Psychiat. 2000;157:2048–2050. doi: 10.1176/appi.ajp.157.12.2048. [DOI] [PubMed] [Google Scholar]
- Powell K, Kresnow M, Mercy J, Potter L, Swann A, Frankowski R, Lee R, Bayer T. Alcohol consumption and nearly lethal suicide attempts. Suicide and Life-Threatening Behavior. 2001;32(1 Supplement):30–41. doi: 10.1521/suli.32.1.5.30.24208. [DOI] [PubMed] [Google Scholar]
- Prkacin I, Vujanic S, DAbo N, Palcic I, Naumovski-Mihalic S. Cases of acute poisoning admitted to Clinical Hospital Merkur in Zagreb in 1999. Arhiv Za Higijenu Rada I Toksikologiju. 2001;52:315–321. [PubMed] [Google Scholar]
- Rossow I. Suicide, alcohol, and divorce: Aspects of gender and family integration. Addiction. 1993;88:1659–1665. doi: 10.1111/j.1360-0443.1993.tb02041.x. [DOI] [PubMed] [Google Scholar]
- Rossow I, Ystgaard M, Hawton K, Madge N, van Heeringen K, de Wilde E, DeLeo D, Fekete s, Morey C. Cross-national comparisons of the association between alcohol consumption and deliberate self-harm in adolescents. Suicide and Life-Threatening Behavior. 37:605–615. doi: 10.1521/suli.2007.37.6.605. [DOI] [PubMed] [Google Scholar]
- Rossow I, Romelsjo A, Leigman H. Alcohol abuse and suicidal behaviour in young and middle aged men: Differentiating between attempted and completed suicide. Addiction. 1999;94:1199–1207. doi: 10.1046/j.1360-0443.1999.948119910.x. [DOI] [PubMed] [Google Scholar]
- Smith GS, Branas CC, Miller TR. Fatal nontraffic injuries involving alcohol: A meta-analysis. Ann Emerg Med. 1999;33:659–668. [PubMed] [Google Scholar]
- Varnick A, Wasserman D. Suicides in the former Soviet Republic. Acta Psychiatria Scandinavia. 1992;86:76–78. doi: 10.1111/j.1600-0447.1992.tb03230.x. [DOI] [PubMed] [Google Scholar]