Summary
The high risk cerebral AVM can do great harm to people in case of hemorrhage .The goal of aathis paper is to discuss the characters of images and the technical manipulate of endovascular embolization for high risk cerebral AVM with bleeding. Fifty-six cases of high risk cerebral AVM with bleeding were confirmed by CT?MRI?and approved by whole cerebral DSA. Depended on the nidus of AVM, the superselective endovascular embolization with NBCA or embolization combined with radiological surgery was chosen. The nidus was eliminated for 100% in 36 cases after embolization for 1 to 3 processes. The rebleeding was found in 2 cases with new growth and survival aneurysm in nidus during the following period and treatment with Y-knife, and cured by second embolization. These are the main causes of brain bleeding composed of aneurysm and aneurysm-like dilation beside and located at the nidus, fine draining veins, and growth in ventricles. It is the favourable for the preference to eliminate the aneurysm in AVM during embolization to prevent brain from bleeding.
Key words: cerebral arteriovenous malformations, angiography, digital subtraction, neuroradiology interventional
Introduction
Arteriovenous Malformation (AVM) is an important part of hemorrhagic cerebral vessel disease. Among them the high risk cerebral AVM which presented with onset of cerebral hemorrhage can often cause serious clinical symptoms, and the prognosis may be not well1. The analysis of all these cases indicates the characters of the disease while being diagnosed and treated.
Material and Methods
From 1996 to 2001, 56 patients (35 males, 21 females, median age 27 years, range 3-56 years) presenting with sudden headache and vomit were diagnosed as cerebral hemorrhage or intraventricular hemorrhage by CT or MRI scanning (11 of them had ever been performed craniotomy to remove the hematoma or both of craniotomy to remove the hematoma and decompression procedure), then underwent angiography and embolization. All record and angiographic examinations were analyzed retrospectively.
The cerebral AVM with bleeding of all the cases were confirmed by CT, MRI and approved by whole cerebral DSA. DSA can show the position, form, size, feeding artery, drainage vein and characters of the nidus of AVM. Depending on it, the superselective endovascular embolization with NBCA or/and liquid coils or embolization combined with radiological surgery were chosen.
All the cases underwent superselective endovascular embolization. Prior to embolization, cerebral DSA were performed by femoral artery or radial artery in routine to comprehend the information of the nidus of AVM. Then transguiding the Magic-STD microcatheter or Prowler-14 microcatheter (with assistance of microguidewire) were transmitted to the nidus. The tip of the microcatheter must be inside the nidus as far as possible. Superselective angiography injection is necessary. If it shows that there are arteriovenous fistulas in the nidus, the speed of local blood steam is fast, so something must be done to slow down it. In usual liquid microcoils were inject through the microcatheter to embolize the fistulas, then the AVM could be embolized with NBCA. If the speed of blood steam of the nidus is not fast, the embolization could be directly performed with NBCA. The concentration of NBCA is mixed according to the speed of blood steam of the nidus. Accurate concentration of NBCA and to pull out the microcatheter at the right moment can prevent the microcatheter from being glue in the target vessel.
If the nidus is in large size, it should be regarded to embolize in several times. But the aneurysms or sacked or aneurysmlik dilataltion inside or beside the nidus found should be thoroughly embolized to prevent it from bleeding again. If the remain of nidus is fed by fine perforating branches, Y-knife or X-knife can be chosen as the compensation of the therapy of embolization.
During and after the therapy of embolization, to control the blood pressure of systemic circulation at the level of 12.0/8.0 kPa can effectively prevent brain from bleeding because of the Normal Perfusion Break Syndrome.
Results
The characters of cerebral DSA in 56 cases of cerebral hemorrhage are: the diameters of the nidus are in the range 2-7 cm, there are aneurysms or sacked aneurysmlike dilataltion inside or beside the nidus in 16 cases and there were obvious retention of contrast medium in it. The drainage veins were Rothensal vein or Galen vein in 16 cases. And fine drainage veins were found in 11 cases and the circulation time was obviously elongated, the nidus was found in ventriclars in 13 cases. The nidus was eliminated for 100% in 36 cases after embolization for 1 to 3 processes, 90% in 10 cases and 60%-80% in 10 cases. The times of embolization are: once in 41 cases, twice in 12 cases, three times in 3 cases. The rebleeding was found in 2 cases. One occurred 1 year after embolization because of a new aneurysm beside the nidus and was cured by the second embolization (figures 1, 2, 3). The other occurred 3 months after X-knife treatment because of a survival sacked dilataltion inside the nidus and was cured by operation. 7 of 56 cases accepted treatment of, Y-knife or X-knife as a complement because the survival nidus were fed by fine arteries and without aneurysm or aneurysmlike dilataltion. 2 years later the review of DSA or MRI showed that no nidus was seen again in 5 cases. Only 1 patient had a disability in the lower limb on the other side after embolization, but 1 month later he recovered completely. No permanent complication occurred.
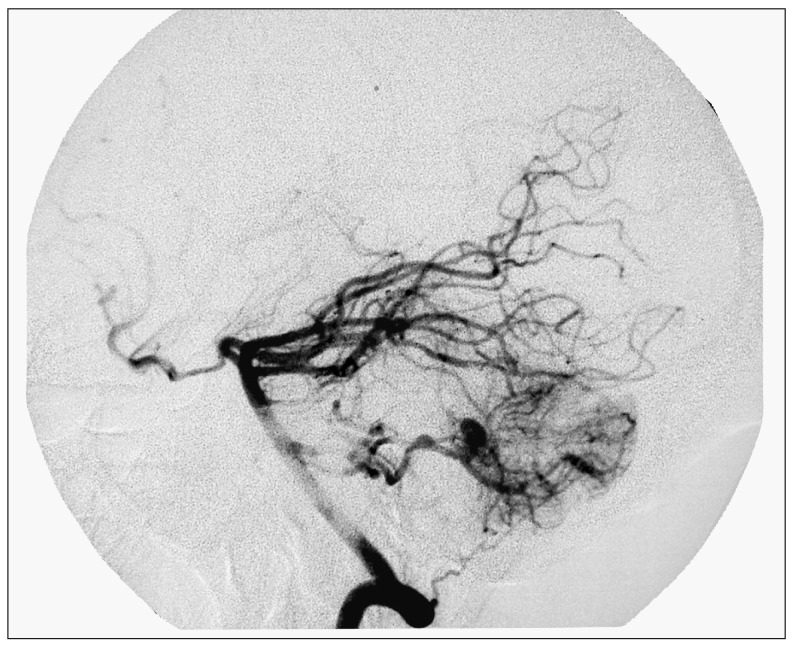
Figure 1.
male 32 years-old, cerebral hemorrhage in posterior fossa. DSA shows a nidus of AVM with an aneurysm beside the nidus feeding inferior posterior cerebellum artery.
Figure 2.
Superselective injection shows the nidus and the aneurysm clearly.
Figure 3.
The callback DSA shows that the nidus and the aneurysm have been eliminated completely after the injection of 2:1 NBCA through a Prowerl-14 microcatheter.
Discussion
The characters and prognosis of high risk cerebral AVM. The AVM presented with hemorrhge inside or beside the nidus was acute onset and did great harm to brain, it could easily lead to hemiplegia, coma, even death2. So it was regarded as high risk AVM. Usually the AVM which were easy to bleed possessed the characters in formation as follow3: there were aneurysms or aneurysmlik dilataltions inside or beside the nidus; the nidus were in the ventricles or grow near or into the ventricles; the drainage veins of the nidus were deep, long and fine, and this caused that the blood from the nidus could not be drained smoothly4. The series of cases accorded with above-mentioned characters in images.
The choice of therapeutic method and adaptation. Because the AVM with aneurysms or aneurysmlik dilataltions inside or beside the nidus or being in ventricles was easier to hemorrhge and the prognosi was worse than others, it indicated that the cases should be treated as soon as possible. There were many methods of therapy in usual, such as endovascular embolization, surgical operation and radiosurgery. But only endovascular embolization was simple and rapid in procedur, not only the patients suffered little, but also the effect were reliable. If Y-knife or X-knife was chosen firstly, more attention must be paid to the nidus with aneurysms or aneurysmlik dilataltions inside or beside the nidus. Because the elastic fibers in arterial walls were easier damaged by radiosurgery than the endothelial cells in constitution of arteries. In early period the wall of aneurysms would get weaker because of the break of the elastic fibers, so it would be possible that the aneurysm ruptured and hemorrhaged before the nidus got healed. And this would lead to deterioration. In this group of cases, hemorrhage occurred after the treatment with X-knife in 1 case because the aneurysmlik dilataltion inside the nidus was not embolized completely. On the other hand, DSA or MRI after 2 years of embolization in 7 cases without aneurysms or aneurysmlik dilataltions inside or beside the nidus.
The announcements of endovascular embolization In Process of endovascular em-bolization, floating series of microcatheter such as Magic and Spinnaker microcatheter were firstly chosen.
If the feeding arteries were often fine and the blood flow were less in the cases with small nidus, the microcatheter with micro-guide wire such as Prowler-10/14 or Excel-14 microcatheter should be chosen. Before the injection of NBCA5, the tip of the microcatheter must be put into the nidus. The aneurysms or aneurysmlik dilataltions inside or beside the nidus and the nidus inside the ventricle must be embolized firstly, and the drainage vein should be keep down if the nidus is too large to be embolized at one time. During and after the therapy of embolization, to control the blood pressure of systemic circulation at the level of 12.0/8.0 kPa could effectively prevent brain from bleeding because of the Normal Perfusion Break Syndrome.
The effect of embolization for high risk cerebral AVM. There are the main causes of brain bleeding in high risk cerebral AVM?aneurysm and aneurysmlike dilation beside and located at the nidus, fine draining veins, and growing in ventricles. The high risk cerebral AVM can do great harm to brain by the onset of cerebral hemorrhage and often cause serious clinical symptoms and bad prognosis. Endovascular embolization is an important method to reduce the factors of hemorrhage by the embolization of aneurysms or aneurysmlik dilataltions inside or beside the nidus and the nidus inside the ventricles or growing near or into the ventricles 3, (figures 4-6).
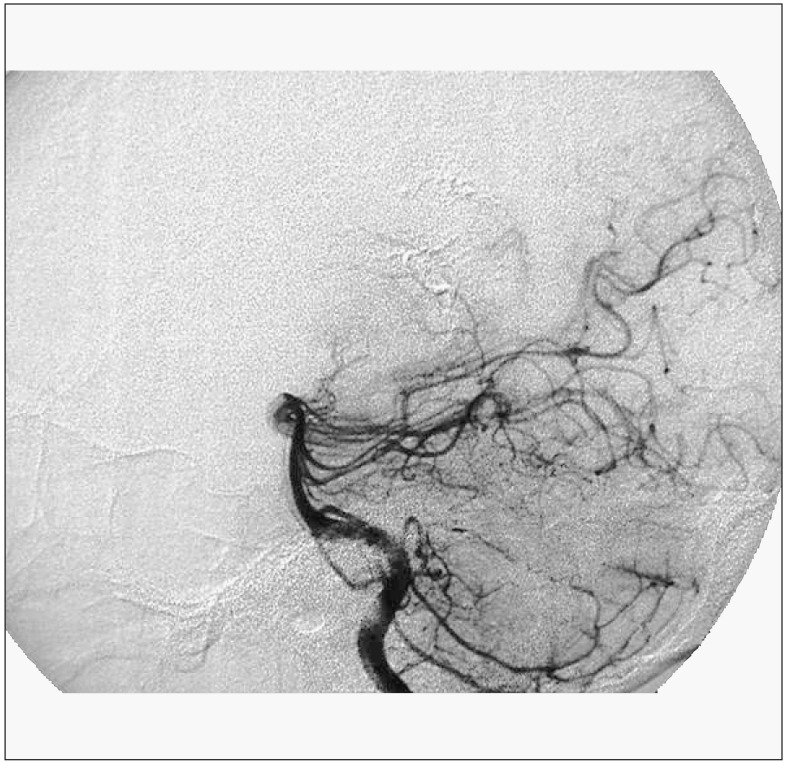
Figure 4.
male 23-years-old, hemorrhage in right ventricle. DSA shows a nidus of AVM in right ventricle (Right CCA injection AP View).
Figure 5.
DSA shows a nidus of AVM in right ventricle (Left DSA shows a nidus of AVM in right ventricle (Right CCA VA injection Lateral View). injection AP View).
Figure 6.
DSA (post-embolization) shows the nidus of AVM in right ventricle has disappeared (Right CCA injection AP View).
Figure 7.
DSA (post-embolization) shows the nidus of AVM in right ventricle has disappeared (Left VA injection LateralView).
Figure 8.
CT (post-embolization) shows the cast of NBCA in View). right ventricle.
Conclusions
There are the main causes of brain bleeding: aneurysm and aneurysmlike dilation beside and located at the nidus, fine draining veins, and growthing in ventricles. It is the favourable for the preference to eliminate the aneurysm in AVM during embolizing to prevent brain from bleeding. Endovascular embolization is a minimal traumatic, secure and effective method of treatment for high risk cerebral AVM. Embolization combined with Y-knife or X-knife in the cases without aneurysm and aneurysmlike dilation and low blood stream can improve healing ratio.
References
- 1.Hayashi K, Takahata H, et al. A case of cerebral arteriovenous malformation complicated with intracerebral hemorrhage after endovascular embolization. No Shinkei Geka. 2001;29:353–358. [PubMed] [Google Scholar]
- 2.Norbash M, Marks MP, et al. Correlation of pressure measurements with angiographic characteristics predisposing to hemorrhage and steal in cerebra arteriovenous malformations. Am J Neuroradiol. 1994;15:809–810. [PMC free article] [PubMed] [Google Scholar]
- 3.Li Sheng, Li Baomin, et al. The Characters of Images and Endovascular Embolization for Cerebral AVM with Bleeding[J] Chin J Radiol. 2002;36:994–996. [Google Scholar]
- 4.Mine S, Hirai S, et al. Risk factors for poor outcome of untreated arteriovenous malformation. J-Clin-Neurosci. 2000;7:503–506. doi: 10.1054/jocn.2000.0743. [DOI] [PubMed] [Google Scholar]
- 5.Li Baomin, Wang Jiayu, et al. The clinic research of the embolization of cerebral AVM with homemade N-Butylcyanoacrylate[J] Chin J Neurosurg. 1999;15:167–169. [Google Scholar]