New agents of liquid acrylic glue for embolization of brain vascular malformation have made their appearance in the therapeutic arsenal. Among those, we have change using previously Histoacryl" (Braun, Aesculap AG, Tuttingen, Germany) to choose Glubran" (GEM Srl, Viareggio, Italy) in 2003. Since this date, we have used Glubran for around 150 embolizations mostly in bAVM, dural arteriovenous shunt, direct fistulae and exceptionally aneurysms. The fact that Glubran bears the CE trademark with specific indication for neuroradiological endovascular use is very important on the legal point of view even if Histoacryl has been used worldwide by the most experience teams in cerebral vascular malformation endovascular field treatment3. To our experience, and in agreement with experimental works, Glubran does not produce bubbles and seems to diffuse more homogeneously and in a more predictable way than Histoacryl1.
The principle of intra nidal embolization with cyanoacrylate remains exactly the same and Glubran does not change the concept of treatment. It requires extensive experience which was acquired with Histoacryl and easily translates with Glubran.
All patients are treated under general anaesthesia, a 5 french guiding catheter is used to catheterize the main feeding trunk (flush with saline) and a bolus of 1000 UI of heparin is made intravenously. The heparin is reverse at the end of the embolization. On the technical point of view, there is no difference with Histoacryl except the color of the mixture. We always mixed Glubran with Lipiodol" (Guerbet, Aulnay s/s bois, France). The concentration is adapted to the nidus type angio architecture (the size of the nidus and the flow of the shunt). Commonly, we use a concentration between 25 and 50%. We think that experience is very important and that the neuroradiologist must master different concentrations of glue and the different kind of behaviour of the microcatheter 2.
Even if we try to control the flow during the injection, the situation of the tip of the microcatheter also influence the concentration of glue. For bAVM, most of the time we use a flow-dependant catheter (1,2 to 1,5 Fr). We try to navigate without guide wire to reach the nidus , and when it is possible in a wedge position. Before injecting the glue, we do a biplane superselective angiography in the "working projection". The working projection is chosen to allow visual control of the nidus penetration and arterial reflux when the glubran will be deposited. Then we flush the microcatheter with glucose and we inject the glue with a 3cc syringe during a biplane run. The quantity of glue depends of the size of the nidus (0,7 to 2cc), at the end of the injection the operator must aspirate back the glue and rapidly pull the microcatheter inside the guiding catheter. What are the main complications we have to avoid?
During the navigation, the operator must be very cautious when using guidewire to prevent any perforation. We preferred not to push the guidewire out of the tip of the microcatheter.
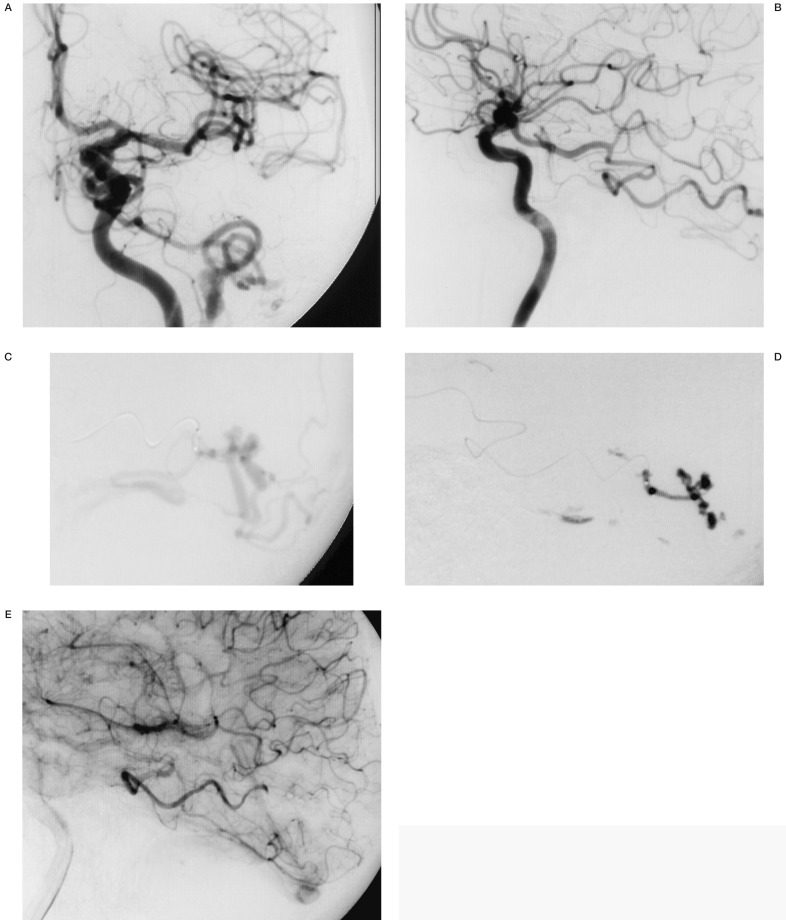
Figure 1.
A 47-year-old man presenting with a left occipital haematoma. Left internal carotid angiography frontal (A) and lateral view (B): direct arteriovenous fistula fed by the posterior cerebral artery. Supraselective angiography of the fistula (C). Cast of glue injection (D). Control post embolization angiography, lateral view (E).
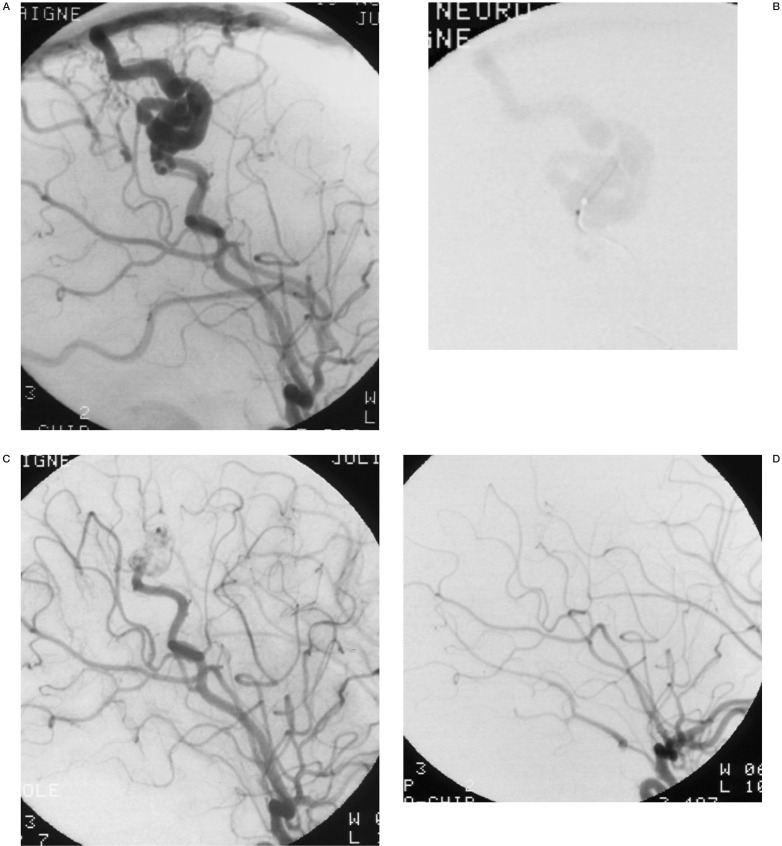
Figure 2.
A 3-year-old boy presenting an acute right hemiparesis with left frontal arteriovenous malformation. (A) left carotid artery angiography lateral view, direct arteriovenous fistula fed by the precentral artery. Supraselective angiography, lateral view, direct venous opacification (B). Immediate control post embolization with Glubran (C). One year control post embolization with remodelling of the feeding vessel which has now a normal size (D).
During the glue injection, venous penetration must be carefully recognized. In case of single draining vein, this is a dangerous situa-tion and the nidus has to be occluded totally to tion prevent haemorrhagic complication. In case of multiple draining veins, one of them can be occluded without any complication if the upstream nidus is already occluded.
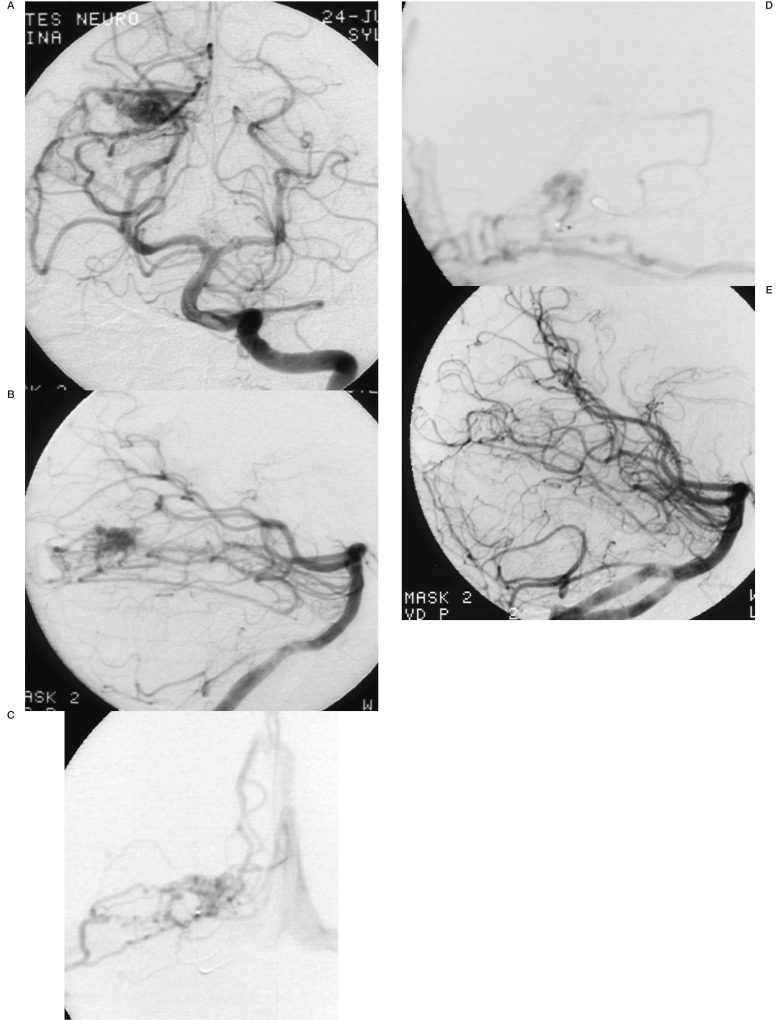
Figure 3.
A 12-year-old boy presenting with a temporo-occipital haematoma. Left vertebral angiography anteroposterior (A) and lateral view (B), arteriovenous malformation of the right occipital lobe. Supraselective injection frontal (C) and lateral (D) views. Control post embolization (E).
The arterial reflux during the glue injection must be mastered to prevent any normal brain artery occlusion.
During the withdrawing, we have not had catheter rupture while using Glubran nor gluing the microcatheter in place.
Conclusion
The concept of intranidal embolization for bAVM has not changed since we use Glubran. We have not modified our injection technique.
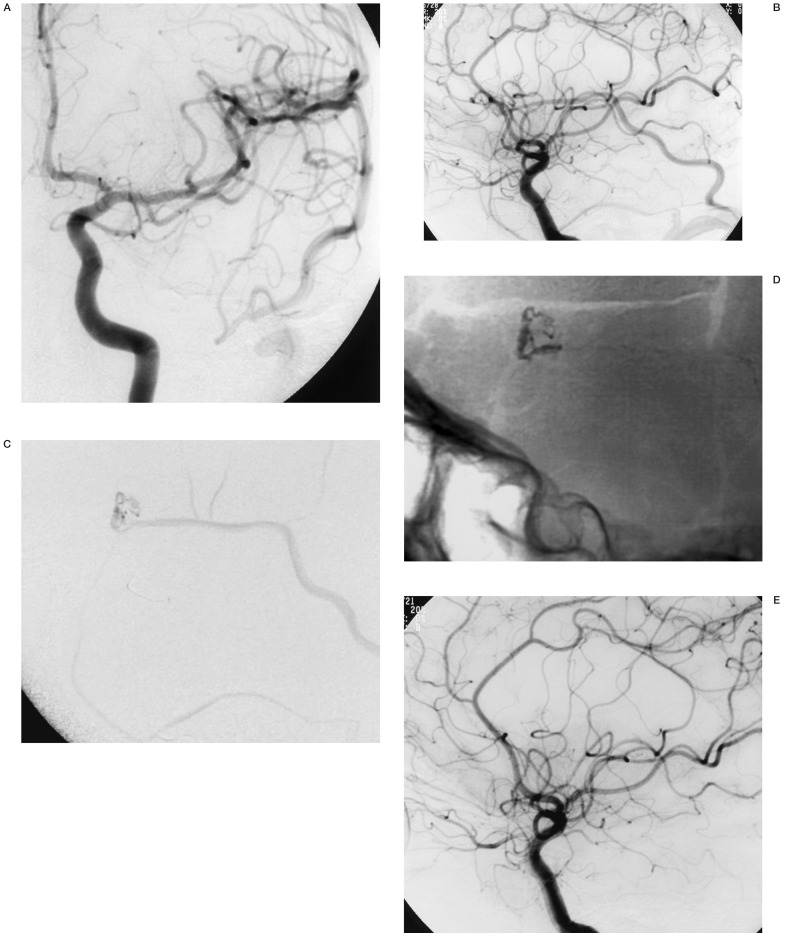
Figure 4.
A 37-year-old man presenting with a left frontal haematoma and aphasia. Left internal carotid artery frontal (A) and lateral (B) views. Small arteriovenous shunt with a single venous drainage (C) at the supraselective angiography. Cast of glue post embolization (D). Three months control angiogram of the left internal carotid artery angiogram, lateral view (E).
In our experience, Glubran polymerization is more reliable and predictable than other cyanoacrylate we used before. Even if new embolic agents (like Onyx) will probably be more widely used, Glubran will remains interesting for high flow single hole fistula occlusion.
References
- 1.Leonardi M, Barbara C, et al. Glubran 2: a new acrylic glue for neuroradiological endovascular use (experimental study on animals) Interventional Neuroradiology. 2002;8:245–50. doi: 10.1177/159101990200800304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wikholm G, Lunquist C, et al. Transarterial embolization of cerebral arteriovenous malformations: improvement of results with experience. Am J Neuroradiol. 1995;16:1811–7. [PMC free article] [PubMed] [Google Scholar]
- 3.Lasjaunias P, Berenstein A, et al. Surgical Neuro-angiography. vol 2.2. New York: Springer, Berlin, Heidelberg; 2003. pp. 695–735. [Google Scholar]