Summary
To report the embolization technique of using Onyx, a new liquid embolic agent, to treat cerebral arteriovenous malformations (AVMs) as well as its efficacy.
38 cases of cerebral AVMs located in eloquent area (motor, speech, visual nerve center), 9 in deep cerebral area, and another 3 cases in cerebellar hemisphere. The diameter of AVMs was smaller than 3cm in 10 cases, 3-6cm in 30 cases, and larger than 6cm in 10 cases. A 6F sheath was placed into the femoral artery after Selding's puncture. After a 6F guiding catheter was introduced into the internal carotid artery or vertebral artery, Ultraflow or Marathon microcatheter could be navigated into the nidus of AVMs. A long-slow injection of Onyx under fluoroscopic control was performed to embolize cerebral AVMs by adopting the "plug and push" technique.
10 AVM cases (20.0%) were considered to be totally occluded with Onyx in this group, 3 cases of which were found no regrowth by a 6-month follow-up. 25 cases (50%) were subtotally occluded while another 15 cases (30%) were partially embolized. Complications include: (1) severe cerebral hemorrhage occurred in three cases, two of them left hemiplegia after hematoma resection. (2) mild hemiplegia occurred in one lager frontal AVM patient. (3) mild visual deficit was left in one larger occipital AVM case. There was no severe complication in other 45 patients.
Onyx has unique and distinctive superiority in treating cerebral AVMs. Nonetheless, the correct embolization technique should be learned to achieve good clinical results and to avoid complications. The long-term efficacy of Onyx embolization needs to be followed up.
Key words: cerebral arteriovenous malformations (AVMs), endovascular therapy, Onyx copolymer
Onyx is a novel liquid embolization agent manufactured by MicroTherapeutics, Inc.. It is a mixture of ethylene-vinyl alcohol copolymer (EVOH), dissolved in Dimethyl Sulfoxide (DMSO), and micronized tantalum powder, which makes the mixture visible under fluoroscopy. It is nothing like glue, which is adhesive. When Onyx comes in contact with blood or any aqueous solution, EVOH copolymer precipitates and solidifies itself into a spongy cast from the outside in, like lava of volcano, as a result of rapid diffusion of DMSO solvent. Before the cast is completely solidified, its liquid center can still flow continuously. There are different concentrations of Onyx to be used for treatment of various diseases1. Since September 2003, we've been using Onyx 18 (6% EVOH and 94% DMSO) to embolize BAVMs in 50 patients. Here comes our preliminary experience.
Clinical Data
1) Population
Between September 2003 to May 2005, 50 patients with BAVMs were treated. There were 35 men and 15 female with a mean age of 28 years (range, 12-47 years). 16 patients presented with seizure, 14 patients with hemorrhage, 13 with headache and/or dizziness, and 7 with limb paralysis, loss of visual acuity and other neurological deficits. CT scan, MRI, and DSA revealed that 38 patients had BAVMs located in eloquent areas such as motor, speech, visual nerve center, 9 in deep cerebral area, and 3 in cerebellar hemisphere. 10 patients had BAVMs smaller than 3 cm, 30 between 3 cm and 6 cm, 10 larger than 6 cm.
2) Embolization Methods
1) A 6F sheath was placed into the femoral artery after Selding's puncture and catherization. After a 6F guiding catheter was introduced into the internal carotid artery or vertebral artery, a flow-directed microcathether compatible with DMSO (Ultraflow or Marathon, MTI, USA) was navigated into the nidus of AVMs with the help of blood flow and/or a guidewire (Mirage, MTI, USA). Angiography of the microcatheter was performed to confirm a stable distal tip position of the microcatheter, clear angioarchitecture of the nidus, and visible drainage vein.
2) A good working projection was found for operators to see the reflux clearly. An acceptable length of reflux was estimated and marked under fluoroscopy.
3) Onyx 18 (MTI, USA) could be injected after the microcatheter was flushed by 0.3 ml DMSO. The first 0.3 ml Onyx must be injected within a period of longer than 90 seconds. Afterwards the injection speed could be adjusted according to how well is the penetration of Onyx. Injection as slow as 0.10-0.15ml per minute was recommended to achieve full penetration of Onyx into the nidus. Injection should be stopped if there was reflux in feeding artery or penetration of Onyx into main drainage vein. Injection should be continued after a waiting period of 30 seconds to 2 minutes to ensure continuous penetration of Onyx into the nidus.
4) "Push and plug technique" is the key to improve penetration of Onyx into the nidus. After multiple rounds of injection, reflux, and waiting, a reflux as long as 1.0 cm to 1.5 cm could be formed at the tip of the microcatheter. Finally a plug could be created around the tip completely blocking the blood flow, resulting in distinctive change in pressure gradients within the nidus, till when, Onyx could penetrate into the nidus continuously to embolize the AVM subtotally or totally.
5) The microcatheter would be withdrawn after the embolization or if the refux exceeded 1.5-2.0 cm. When the catheter was withdrawn, the microcatheter would be pulled straight first, then applied with gradually increased force, and either snapped out of Onyx cast or slowly pulled out.
6) Staged sessions of embolization were planned for partially occluded AVMs.
Results
Among these 50 BAVM patients, 12 patients underwent two-session treatment; 2 patients were treated with three sessions; all others were treated with one session. For each session, one to three feeding arteries were chosen to inject Onyx, and each injection took 15-85 minutes (on average 45 minutes), the volume of which ranged from 1 ml to 13.5 ml (on average 7.5 ml). 10 patients (20%) achieved total occlusion angiographically (Fig. attached) and no other therapeutic treatment was needed. Out of these 10 patients, 3 patients were followed up with angiography 6 months later and were found no recurrences. 25 patients (50%) had sub-total or majority embolization and were recommended to take stereotactic radiosurgery for treatment. 15 patients (30%) who received partial embolization were advised to take further embolizaiton 2 months after. Any patient who was unsuitable for another embolization session would be sent for stereotactic radiosurgery or surgery.
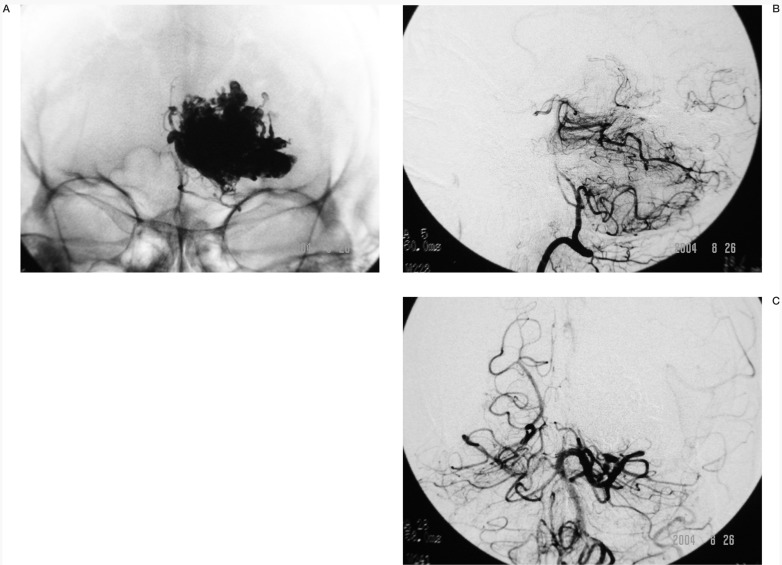
Figure A.
37-year-old male patient presented with persistent headache for 6 months. Cerebral angiogram revealed large BAVM in left occipital lobe. Onyx embolization was conducted. A) pre-operative lateral view of left vertebral angiogram (B) pre-operative AP view of left vertebral angiogram, revealing a large BAVM fed by left posterior cerebral artery. C) lateral view of Onyx cast after embolization (D) AP view of Onyx cast after embolization. A total of 13.5 ml Onyx by three injections. E) Post-operative lateral view of left vertebral angiogram, F) Post-operative AP view of left vertebral angiogram, revealing 100% occlusion of the large BAVM.
Severe brain hemorrhage occurred in three patients, who received emergency surgery removing hematoma. One was fully recovered when discharged. The other two were left with hemiplegia, but no death happened. There were some other complications: 6 patiens who had slight SAH or intraventricular hemorrhage were recovered after expectant treatment. Microcatheters were left in the body of 3 patients. These 3 patients were administered with lowmolecule heparin for one week (Fraxiparine, 0.4 ml, i.m., Bid). No adverse reaction was observed and these three patients were discharged without any problem. One patient with a large AVM located in anterior central gyrus suffered hemiplegia after embolization. Another patient with giant occipital AVM had visual field defect. Both underwent rehabilitation care after discharge.
Discussion
Onyx 18 is one type of low viscosity formula, suitable for AVM embolization. It has such main advantages as being non-adhesive but cohesive, suitable for slow, long injection, being able to penetrate into the whole AVM nidus while not easily drifting into draining vein and causing vein occlusion, and controllable in terms of reflux management. At present there were published articles reporting that the embolization effect was better with Onyx than with n-butyl-2-cyanoacrylate, NBCA2,3. However, there still existed a few problems in clinical applications, such as poor penetration with Onyx injection, catheter withdrawal, intracranial hemorrhage, and etc4,5. Therefore, like what we normally do to all new materials, we must carefully evaluate the material and use it cautiously to maximum its benefit while minimizing its risk.
1) Indications and Contraindications
Although some published articles and our experience proved that BAVM embolization with Onyx has distinctively better therapeutic effect than embolization with NBCA4,5,6,7, yet there were some complications as a result of unskillful practice. Furthermore, the long-term therapeutic effect of embolization needs to be followed up. Therefore we believe that small and medium-sized AVM located in non-eloquent areas should still be mainly treated with microscopic surgery8. Small AVM in deep brain area is more suitable for stereotactic radiosurgery 9. Onyx would be mainly used to treat large AVM cases which are larger than 3 cm, difficult for surgery (deep brain area), and highly risky (eloquent area). For giant BAVM, a multidisciplinary treatment will be adopted combining endovascular embolization, surgery, and stereotactic radiosurgery, among which pre-surgery or pre-radiosurgery embolization is considered essential for the treatment. Onyx is especially suitable for lump-shaped AVM cases with large feeding artery, for which cases not only the therapeutic effect of embolization is excellent, but also less risky it is for catheter withdrawal. There were occasions unsuitable for onyx embolization, such as 1) high flow AVF; 2) AVM with small deep perforating branch feeding artery, for example, brain stem AVM; 3) spinal AVM.
2) Treatment around Embolization
In general no special medication was applied before treatment. Patients who had seizures should take anti-epileptic medicine. Meanwhile, anti-epileptic medicine should be administered intravenously during and after the embolization. General anaesthesia was used to ensure the safety of long-time injection of Onyx. As some asymptomatic or minor brain hemorrhage was observed when Onyx was used to embolize AVM, we believe early reversal of heparin should be applied to prevent hemorrhage from a minor one turning into a fatal one. However, smooth pressurized dripping through coaxle catheter should be maintained at the same time. Heparinization and antiplatelet treatment were not required after the embolization. With majority or complete occlusion of large, high flow AVM nidus, low blood pressure should be maintained for one to two days after the embolization to prevent brain swelling and brain hemorrhage as a result of normal perfusion pressure breakthrough.
3) Precautions of Procedures
Whether BAVM embolization with Onyx can achieve great therapeutic result depends on how accurately the angioarchitecture of AVM nidus is understood and how well the technique is mastered. After 50 cases of BAVM embolization with Onyx, the following experience was gradually learned and summarized: 1) although BAVM normally has multiple feeding artery, yet one larger feeding artery will be chosen to achieve better embolization result. If there is only one large artery feeding the nidus while other feeders are small and tortuous, satisfactory embolization result should be strived to be obtained with the choice feeding artery, as there won't be second chance available for another embolization. 2) It should be emphasized that the tip of the microcatheter should enter the nidus for better result. If the tip is in the feeding artery instead of the nidus, no satisfactory penetration of Onyx can be achieved. What should be done under such occasion is to advance the tip of microcatheter into the nidus. Otherwise, Onyx shouldn't be used. 3) Slow injection should be adopted to enhance the penetration of Onyx while preventing too much reflux. 4) In most cases, "plug and push technique" must be adopted to have the majority or whole nidus embolized through one microcatheter: to allow little reflux around the tip the microcatheter, wait for 30 seconds up to 2 minutes for Onyx sodification, creating a complete blocking effect of blood flow, and then continue with slow injection so that Onyx can penetrate forward within the nidus. Such technique should be repeatedly used until sometimes the reflux is as long as 1.5cm to achieve better results. Thus the operator must have sufficient patience to observe and wait. 5) Catheter withdrawal technique is of vital importance to the success of the operation. Our experience is that quick catheter withdrawal should be easier for straight and large feeding artery; for tortuous feeding artery, slow catheter withdrawal should be recommended. The criteria is not to induce obvious shifting of the nidus. Otherwise, bleeding may occur.
1) Complications and Preventions
The severe complication for BAVM embolization with Onyx is mainly brain hemorrhage. We experienced 3 severe brain hemorrhage. One was caused by perforation of small tortuous feeder by microtheter during the operation; the other two were caused by obvious shifting of nidus when microcatheter was withdrawn at the end of embolization. 6 patients with higher percentage of embolizaiton were found asymptomatic or minor SAH or ventricular hemorrhage. Possible causes were following: 1) improper manipulation of microcatheter and guidewire to cause rupture of the nidus vessel. So gentle manipulation should be stressed and guidewire was recommended not to enter the nidus. NBCA should be prepared before the embolization started so that the bleeding legion could be occluded at once with NBCA in case there is one during the procedure. 2) Onyx reflux during the procedure played a role like a two-edged sword. On the one hand, proper reflux helps the continuous penetration of Onyx into nidus to achieve satisfactory embolization result; on the other hand, improper reflux makes it difficult to withdraw microcatheter, which may result in severe brain hemorrhage, causing patient death risk as well as severe sequela. We believe that the tortuosity of the feeding artery is the chief reason for difficult catheter withdrawal. Of course the length of the Onyx reflux as well as the time length of embolization are both important factors too. Onyx isn't the good embolic agent for obviously small tortuous feeding artery. If Onyx has to be used in such case, it is safer to leave microcatheter in the body after the procedure. If properly treated, the patient won't suffer any adverse effect with microcatheter left in the body. 3) Draining vein should be protected from being embolized during the case. If draining vein is no longer visible angiographically, the whole nidus should be completely occluded to avoid bleeding. 4) With giant high flow BAVM, due to the better penetration feature of Onyx, the volume of therapeutic embolization of one single session should be controlled. Meanwhile, post-operative depressurization treatment should be taken to avoid the risk of normal perfusion pressure breakthrough. For patients who underwent high percentage of embolization, depressurization treatment was taken as a rule during and after the operation.
5) Therapeutic Effect and Evaluation
Jahan reported about 23 cases of BAVM treatment with Onyx embolization. After multiple treatments, the volumes of AVMs were shrunk by an average 63%. One permanent brain infarct after the treatment as well as 3 temporary neurological defects was reported. The initial clinical results we obtained revealed that 20% patients selected could be cured angiographically only by Onyx embolizaiton alone, yet the long-term results should be further monitored. For giant BAVM, one or two sessions of Onyx embolization can reduce the nidus to make it eligible for radiosurgery, which distinctively shortened the cycle of therapeutic treatment and lowered the treatment expenses. In addition, after following up by angiogram with patients who received Onyx embolization, we found that Onyx embolization was a true perfusion of nidus with embolic agent, which reduced the rate of recurrences and regrowth. Therefore, we believe that onyx is so far the better embolic agent to treat BAVM, which has expanded the indications of endovascular treatment of BAVM and hopefully enhanced the therapeutic effect of endovascular treatment of BAVM. However, a complication rate as high as 10% is still a major worrisome concern for most neuro-interventional physicians to opt for endovascular treatment of BAVM. To master the technique of Onyx embolization of BAVM while trying hard to minimize the complication rate will be what we consistently pursue.
References
- 1.Donglei Song. Application of Onyx in Interventional Treatment of Cerebral Vascular Disease, Chinese Contemporary Neuro Disease Magazine? 2004;4:15–18. [Google Scholar]
- 2.Duffner F, Ritz R, Bornemann A, et al. Combined therapy of cerebral arteriovenous malformations: histological differences between a non-adhesive liquid embolic agent and n-butyl 2-cyanoacrylate (NBCA) Clin Neuropathol. 2002;21:13–17. [PubMed] [Google Scholar]
- 3.Akin ED, Perkins E, Ross IB. Surgical handling characteristics of an ethylene vinyl alcohol copolymer compared with N-butyl cyanoacrylate used for embolization of vessels in an arteriovenous malformation resection model in swine. J Neurosurg. 2003;98:366–370. doi: 10.3171/jns.2003.98.2.0366. [DOI] [PubMed] [Google Scholar]
- 4.Donglei Song, Bing Leng, Yuxiang Gu, et al. Clinical Analysis of 28 BAVM Cases Embolized with Onyx, a Novel Liquid Embolic Agent. Interventional Radiology (Chinese)? 2004;12:105–108. [Google Scholar]
- 5.Florio F, Lauriola W, Nardella M, et al. Endovascular treatment of intracranial arterio-venous malformations with Onyx embolization: preliminary experience. Radiol Med. 2003;106:512–520. [PubMed] [Google Scholar]
- 6.Jahan R, Murayama Y, Gobin YP, et al. Embolization of arteriovenous malformations with Onyx: clinicopathological experience in 23 patients. Neurosurgery. 2001;48:984–995. doi: 10.1097/00006123-200105000-00003. [DOI] [PubMed] [Google Scholar]
- 7.Fournier D, Ter Brugge KG, Rodesch G, et al. Revascularization of brain arteriovenous malformations after embolization with bucrylate. Neuroradiology. 1990;32:497–501. doi: 10.1007/BF02426463. [DOI] [PubMed] [Google Scholar]
- 8.Deruty R, Pelissou-Guyotat I, Amat D, et al. Multidisciplinary treatment of cerebral arteriovenous malformations. Neurol Res. 1995;17:169–177. doi: 10.1080/01616412.1995.11740307. [DOI] [PubMed] [Google Scholar]
- 9.Gobin YP, Laurent A, Merienne L, et al. Treatment of brain arteriovenous malformations by embolization and radiosurgery. J neurosurg. 1996;85:19–28. doi: 10.3171/jns.1996.85.1.0019. [DOI] [PubMed] [Google Scholar]