Introduction
In recent years the management of brain AVMs has evolved both because of new materials and for the modification of treatment strategies. With regard to materials, newly developed improved microcatheters and microwires have allowed increasingly distal locations to be reached; N-Butyl-2-cyanoacrilate (Glubran 2) has recently substituted Isobutyl-2-cyanoacrilate (IBCA), and a completely new non-adhesive embolic agent (Onyx) is increasingly being used in many centres as a reliable alternative or as first choice agent.
Concerning treatment strategies it must be noted that radiosurgery, now available in many centres, is being used with increasing frequency as an alternative to surgery. Furthermore when associated with embolization, radiosurgery has allowed AVMs, which were previously considered untreatable, to be dealt with.
Methods
227 patients with cerebral AVMs treated over the last 5 years (from January 2000 to December 2004) in a national referral neurosurgical department provided with endovascular neuroradiology and gamma-knife radiosurgery facilities were evaluated (table 1).
Table 1.
Five Years AVMs Load in Department of Neurosurgery of Verona (2000-2004)
| Treatment Modality | N° of Patients | Percentage of Total |
|---|---|---|
| Direct radiosurgery | 113 | 49% |
| Direct surgery | 16 | 7% |
| Combined treatment * | 98 | 44% |
| Total | 227 | - |
| * endovascular treatment alone or in association with radiosurgery or surgery | ||
During this period 255 endovascular treatment sessions for cerebral AVMs were performed in 98 patients. In the present paper only the patients who started and completed their treatment sessions, consisting of embolization alone or combined with surgery and/or radiosurgery, were considered.
It is important to stress that during the same period of time 16 patients with cerebral AVMs were treated by means of surgery alone and 113 by stereotactic radiosurgery alone.
Out of the 98 patients treated by means of embolization, the following groups of patients were excluded:
- patients who completed treatment between January 2000 and December 2004 but who initiated treatment before 2000
- patients who started treatment after January 2000 and dropped out during treatment or were lost at follow-up
- patients still in treatment in December 2004.
For each patient the following data were reviewed:
A) Sex
B) Age at diagnosis
C) Clinical presentation:
-
a)
hemorrhage
-
b)
epilepsy
-
c)
focal neurological deficits
-
d)
cognitive/mental impairment
-
e)
headaches
-
f)
other symptoms (e.g. tinnitus)
-
g)
various combinations of points a to f
-
h)
asymptomatic, incidental finding
D) Location of the nidus, which was divided into two main groups depending on the presence of adjacent eloquent brain. The following locations were considered eloquent: sensory-motor area, language cortex (both Broca's and Wernicke's areas), visual cortex (occipito-mesial area), basal ganglia and hypothalamus; posterior fossa (including both brain stem and cerebellum)
E) Nidus size: the volume expressed in ml was calculated from the three MRI or angiographical main diameters (transverse, coronal and sagittal). In fact, as previously reported (A. Beltramello et Al, 1990), assuming that an AVM is similar to a sphere or an ellipsoid, its volume can be calculated by dividing the product of its 3 diameters by half According to their volume AVMs were divided into 3 main groups (A. Pasqualin et Al, 1991): 1) small: < 10 ml, 2) medium: 10-20 ml, 3) large: >20 ml
F) Number of endovascular procedures per patient and interval between procedures
G) Embolic agents used. The main agents were IBCA (recently substituted by Glubran 2) and Onyx in the last two years. Polylene threads and solid particles like PVA were sometimes used as secondary agents: the former to reduce the flux of a-v fistulae before IBCA injection, the latter for pre-surgical embolization of external carotid artery territories
H) Morphological results. Two different results were considered:
a) early result, at the end of the last endovascular procedure (total obliteration; subtotal obliteration with more than 90% obliteration of the nidus; more than 50% obliteration; less than 50% obliteration)
b) final result, evaluated by control angiography 3-6 months after the final treatment for patients who were embolized only or operated after embolization. For patients who underwent radiosurgery after embolization, final angiography was usually scheduled 24 months after treatment.
I) Technical complications during embolization procedures were considered as follows: glued catheter, hemorrhage, glue in venous sinuses, thrombo-embolic event, vessel perforation, normal vessel occlusion, vessel tearing, etc.
J) Morbidity and mortality, recorded for each endovascular procedure, distinguishing between transitory and permanent complications
K) Duration of treatment. This was considered to be the period elapsed between the time of the first embolization and the date of the final treatment (curative embolization, surgery, radio-surgery)
L) Follow-up period, considered from the date of final treatment to the date of the last clinical control
M) Final outcome at the time of the last clinical control.
Results
Over the 5-year period taken under consideration 98 patients underwent at least one endovascular procedure for the treatment of a cerebral AVM. 44 of these patients began and completed their endovascular or combined treatment within the period under consideration and are the object of this study. 54 patients were not included for the following reasons: a) first endovascular procedure performed before January 2000 (27 cases), b) patients still in treatment by the end of December 2004, for whom further embolization sessions have been scheduled (15 cases), c) patients who dropped out during treatment or were lost at follow-up (12 cases). The 44 patients studied included 27 males and 17 females, with a mean age at diagnosis of 30 years ± 15.1 (mean ± SD).
28 were treated by means of embolization combined with radiosurgery (64%); 12 were treated by means of embolization and surgical removal of the remaining nidus (27%) (two of these patients also underwent radiosurgery between embolization and surgery); 4 patients were treated by means of embolization alone (9%).
The data recorded are summarized in table 2. Only the most relevant data will be analysed in the following paragraphs, focusing on the largest groups. Patients treated by means of embolization followed by radiosurgery will be indicated as Group A (28 patients), while patients treated by means of embolization and surgery will be indicated as Group B (12 patients including the 2 who underwent radiosurgery before surgical removal). Group C identifies patients who underwent curative embolization (4 patients).
Table 2.
Patients Recorded Data
| GROUP A | GROUP B | GROUP C | TOTAL | ||
|---|---|---|---|---|---|
| (E + RS) | (E + S) and (E + RS + S) |
(E alone) | (GROUPS A + B + C) |
||
| (28 patients) | (12 patients) | (4 patients) | (44 patients) | ||
| Clinical presentation: | Hemorrhage | 10 (36%) | 4 (33%) | 2 | 16 (36.4%) |
| Epilepsy | 13 (46%) | 3 (25%) | 1 | 17 (38.6%) | |
| Focal deficit | - | 2 | 1 | 3 (6.8%) | |
| Headache | 5 | 3 | - | 8 (18.2%) | |
| Asymptomatic | - | - | - | - | |
| Location of The Nidus: | Non Eloquent | 11 (39%) | 7 (58%) | 2 | 20 (45.5%) |
| Eloquent | 17 (61%) | 5 (42%) | 2 | 24 (54.5%) | |
| Location of the nidus: | Language (Wernike's) |
5 | 2 | 2 | 9 (37.5%) |
| (when eloquent) | Rolandic | 5 | 1 | - | 6 (25%) |
| (24 patients) | Posterior Fossa | 3 | 1 | - | 4 (16.7%) |
| Basal Ganglia | 4 | - | - | 4 (16.7%) | |
| Other | - | 1 | - | 1 (4.1%) | |
| Location of the nidus: | Temporal | 10 | 6 | 1 | 10 (22.7%) |
| Frontal | 4 | 1 | 2 | 7 (15.9%) | |
| Temporo-Occipital | 3 | 3 | 1 | 7 (15.9%) | |
| Rolandic | 5 | 1 | – | 6 (13.7%) | |
| Cerebellar | 3 | 1 | – | 4 (9.1%) | |
| Basal Ganglia | 4 | – | – | 4 (9.1%) | |
| Parieto-Occipital | 1 | 2 | – | 3 (6.8%) | |
| Other | 1 | 1 | 1 | 3 (6.8%) | |
| Nidus volume | <10 ml | 15 (53%) | 4 (34%) | 4 | 23 (52.3%) |
| 10-20 ml | 8 (29%) | 7 (58%) | - | 15 (34.1%) | |
| >20 ml | 5 (18%) | 1 (8%) | - | 6 (13.6%) | |
| Number of endovascular procedures per patient ± SD |
2 ±1.6 |
2.2 ± 1.8 |
1.5 ± 0.6 |
2 ± 1.6 |
|
| Interval in months ± SD | 5.4 ± 3.1 | 4.4 ± 1.8 | 4 ±2.8 | 5 ± 2.7 | |
| Embolic agents | IBCA | 16 | 5 | 2 | 23 (52.3%) |
| Glubran | 5 | 4 | 1 | 10 (22.7%) | |
| Onyx | 3 | - | 1 | 4 (9.1%) | |
| Onyx + Glubran | 4 | 3 | - | 7 (15.9%) | |
| Early morphological | <50% obliteration | 2 | - | - | 2 (4.5%) |
| result: | >50% obliteration | 16 | 10 | - | 26 (59.1%) |
| Subtotal obliteration | 10 | 2 | - | 12 (27.3%) | |
| Total obliteration | - | - | 4 | 4 (9.1%) | |
| Final morphological | <50% obliteration | 1 | - | - | 1 (2.3%) |
| result: | >50% obliteration | 2 | - | - | 2 (4.5%) |
| Subtotal obliteration | - | - | - | - | |
| Total obliteration | 11 | 12 | 4 | 27 (61.4%) | |
| Not yet available* | 14 | - | - | 14 (31.8%) | |
| Technical complications of embolization: |
Glued catheter | 3 | 3 | - | 6 (6.8%) |
| Perforation | 1 | 2 | - | 3 (3.4%) of total procedures |
|
| Embolization related | Transitory | 1 | 1 | 1 | 3 (3.4%) |
| morbidity: | Permanent | - | 2 | - | 2 (2.3%) of total procedures |
| Overall morbidity (Permanent) | 2 | 2 | - | 4 (9.1%) of total | |
| Duration of treatment | (months ± SD) | 12 ± 12.9 | 9.2 ± 7.4 | 1.5 ± 1 | 10.4. ± 11.3 |
| Follow-up period (30 patients) |
(months ± SD) | - | - | - | 29.6 ± 13.7 |
| Final outcome | Unmodified | 20 | 6 | 3 | 29 (66%) |
| Improved | 7 | 3 | 1 | 11 (25%) | |
| Worsened | 2 | 2 | - | 4 (9%) | |
| Legend: * Treatment completed but control angiography to be performed. | |||||
Clinical presentation: epilepsy was the most frequent symptom present in group A (46%), while hemorrhage was similar in the two groups (36% in group A; 33% in group B).
Location of the nidus was adjacent to eloquent brain in 61% of cases in group A and only in 42% of cases in group B.
All the basal ganglia AVMs (4/4) and almost all the AVMs located in the rolandic area (5/6) belonged to group A.
Nidus volume: the larger AVMs (5/6) belonged to group A, while medium sized AVMs (10-20 ml) were prominent in group B (almost all [6/7] located in non eloquent areas).
Volume was invariably small in those patients treated by means of curative embolization alone (4/4).
A total of 88 endovascular procedures were performed in the 44 patients considered in the period between Jan 2000 and Dec 2004.
Patients underwent an average of 2 ±1.6 endovascular treatment sessions and the interval between procedures was 5 ± 2.7 months. The variability of interval between different sessions often depended on non-medical factors (business commitments, family problems, etc.).
There was no significant difference among groups. It is interesting to note that the longest intervals were recorded in group A and this can be explained by the more challenging characteristics of these AVMs, both due to volume and size; nevertheless this delay did not affect negatively the final result (80% total occlusion).
Embolic agents used were IBCA in 23 (52.3%) and Glubran in 10 (22.7%).
Onyx was used, alone or in combination with Glubran, in 7 patients (15.9%).
Early morphological results, assessed at the end of the last embolization session, were as following:
<50% obliteration in 4.5% of patients; >50% obliteration in 59.1%; subtotal obliteration in 27.3% and total obliteration in 9.1% of patients.
Satisfactory results, considered those with more than 50% obliteration, were recorded in 26 out of 28 patients in group A (93%), achieving sub-total obliteration in more than 1/3 of cases. Satisfactory results were obtained in all the patients in group B (12/12).
Obviously, total obliteration was obtained in all group C patients.
Final results, more than 6 months after the final treatment were as following: total obliteration in 27 cases (61.4%); more than 50% obliteration in 2 (4.5%); less than 50% obliteration in 1 (2.3%).
Radiosurgery after embolization (group A) achieved total obliteration of the AVM in 11 out of 14 patients (80%). AVMs which were not completely obliterated were the largest ones at the beginning of embolization treatment (mean volume > 20 ml in 3/3). For these patients a further angiographic control 3 years after treatment is scheduled. Should the AVM result incompletely occluded a second gamma-knife treatment would be advisable. By the end of Dec 2004, the remaining14 patients (31.8%) had already completed their endovascular treatment with subtotal obliteration in 4 cases (28.6%), and obliteration of more than 50% of the nidus in 9 (64.3%) and less than 50% in 1 (7.1%). Final angiographic follow-up will be performed 24 months after radiosurgery.
Technical complications during embolization procedures were observed in 10.2% of 88 procedures (6 glued catheters and 3 small perforations). No permanent clinical consequences were recorded.
Transitory complications occurred in 3 patients (3.4% of all endovascular procedures) and were evenly distributed among the three groups.
Permanent complications occurred in 2 patients - both belonging to group B: left hemianopia in one and left hemiparesis in the other (4.5% of all patients, 2.3% of 88 endovascular procedures).
No deaths were recorded.
Average duration of treatment was 10.4 months ± 11.3.
Follow-up period considered from the date of final treatment to the date of the last clinical control (available only for 29 patients) was 29.6 months ± 13.7.
At final outcome in 44 patients (groups A+B+C) clinical worsening was recorded in 4 (9% of the total), while the condition of 29 patients was unmodified (66%) and 11 had improved (25%).
Improvement was due to a decrease in intensity and frequency of headaches in 5 patients, and to better control of epileptic seizures in 6.
Discussion
Brain AVMs are often a challenging disease affecting young people for whom it is of prime importance to make every effort to improve materials and to employ all the available human resources.
In our opinion the best treatment can be obtained at multi-specialist well equipped centres that can offer all the technologies effective for this pathological entity (endovascular procedures, surgery, stereotactic radiosurgery).
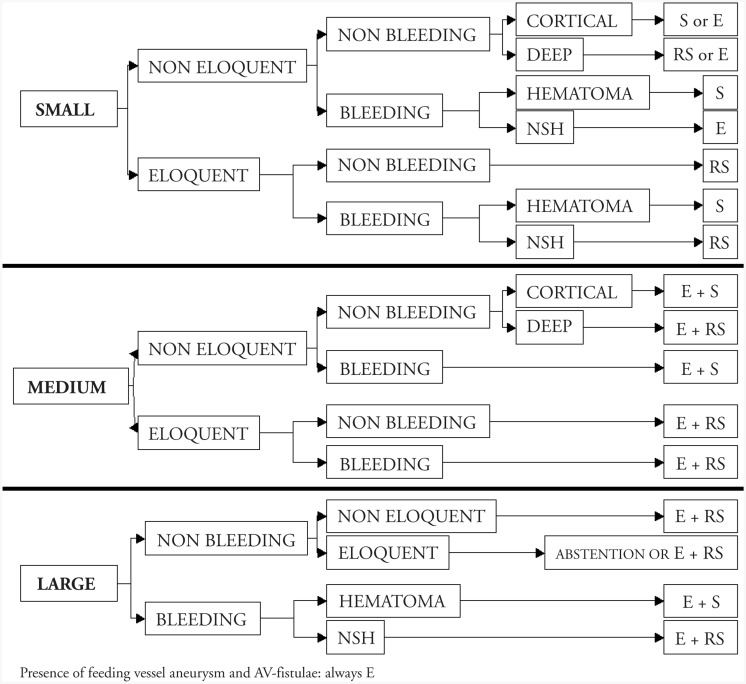
In our experience, the less-invasive therapy available for each specific type of AVM should be employed. The following specific factors should be considered when choosing the most suitable treatment strategy: nidus size, location (eloquent vs. non-eloquent) and presence or absence of previous hemorrhage (figure 1).
Figure 1.
Treatment policy for different types of AVMs. Legend: S = surgery, E = embolization, RS = radiosurgery, NSH = without significant haematoma.
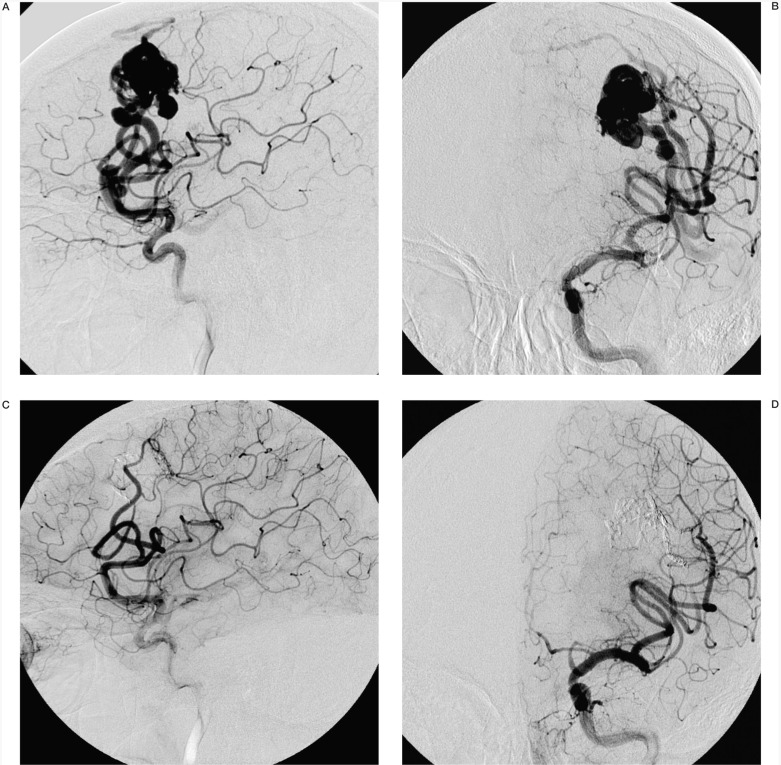
With these criteria in mind, in our experience most AVMs (113/227:49%) in the 5-year period considered underwent direct radiosurgery, which was preferred when the lesion was small, deep, eloquent and non-bleeding. Direct surgery (16/227:7%) was preferred for small or medium sized, cortical, non eloquent and bleeding lesions. Embolization was considered for all the other cases (98/227:44%), especially for large or medium-sized eloquent lesions, to decrease the lesion volume in order to render surgery or radiosurgery feasible. Embolization was curative in only a minority of lesions, mostly smaller ones (figure 2), but complete obliteration of the AVM by embolization alone was not intended as the goal of treatment according to our policy.
Figure 2.
A-D) Male, aged 60 presenting with sudden aphasia due to hemorrhage in the left frontal region. Left carotid angiography (A,B) showed a left frontal, pre-rolandic AVM with a volume of 9 ml fed by the most posterior of the prefrontal arteries and the precentral sulcus artery. Immediate post-embolization (Onyx) angiogram (C,D) showed complete obliteration of the AVM. A control angiogram, performed one year later, confirmed the stability of the result.
Embolization was performed in all the patients in whom the angio-architecture of the AVM increased the risk of bleeding. Regarding embolic agents, particulate embolization has been completely abandoned in favour of glues or Onyx; currently we prefer Onyx for high flow compact AVMs, while glue is preferred for dispersed lesions, fed by smaller vessels.
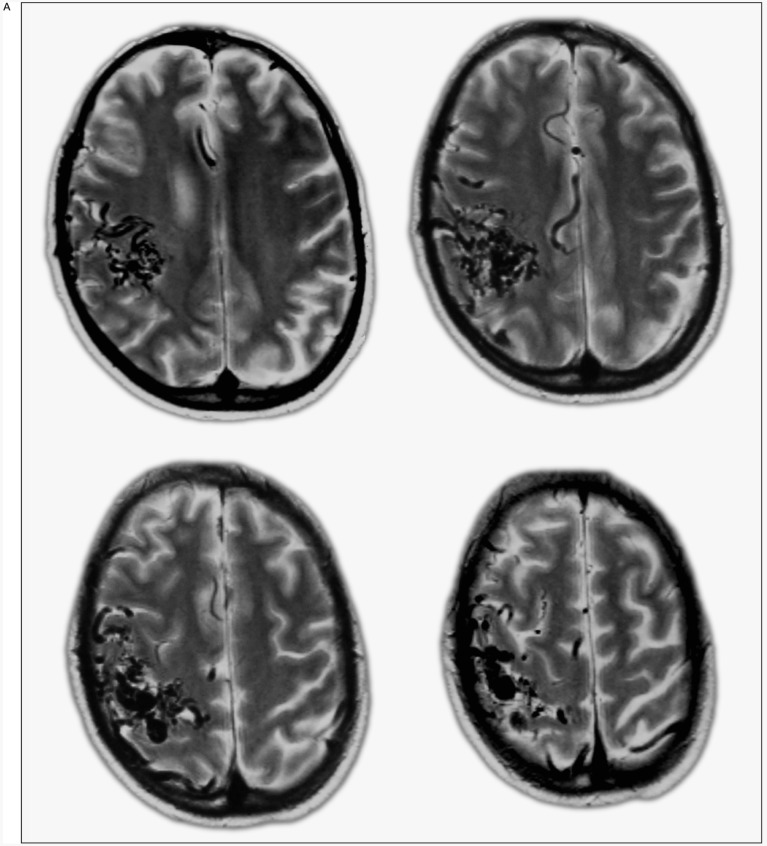
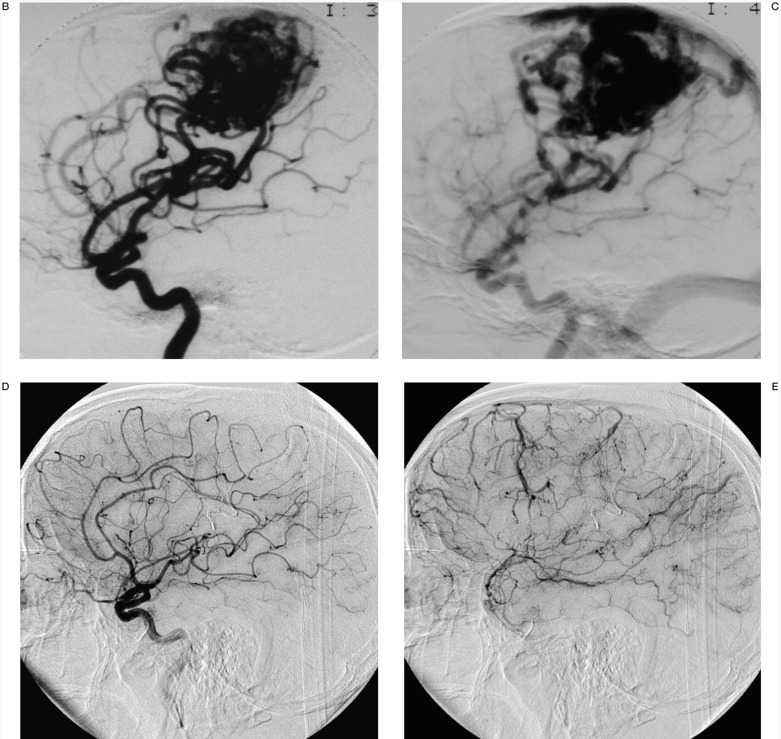
Satisfactory results (>50% obliteration of the lesion) were obtained by means of embolization in 93% of the cases that were subsequently addressed to radiosurgery, with subtotal obliteration before radiosurgery in more than one third of cases. Total obliteration of the lesion after radiosurgery was obtained in nearly 80% of cases, including the largest ones located in eloquent areas (figure 3), with a low rate of morbidity, which was not embolization related (2/28 permanent deficits: 7%).
Figure 3.
A-E) Male, aged 42 with partial seizures. T2-weighted MR scans (A) reveal a large (21 ml) right rolandic AVM. At carotid angiogram (B,C) a rolandic AVM fed by several branches of anterior and middle cerebral arteries with draining veins directed to the superior sagittal sinus was evident. The patient underwent 5 endovascular procedures and radiosurgery. Control angiograms 3 years after completion of the combined treatment (D,E) show complete obliteration of AVM.
A higher morbidity rate was observed for embolized AVMs which then underwent surgery (2/12 permanent deficits:16%) which permitted the definitive cure of the lesion in all the cases.
No permanent deficit was observed in the 4 patients for whom endovascular treatment was curative.
Technical complications occurred in 10.2% of the total number of procedures, with no permanent sequelae.
In conclusion, overall morbidity rate was only 9%, with 90% total obliteration rate for 27 out of 30 patients who completed their treatment and follow-up in the 5-year period analysed. No deaths were recorded.
In our opinion these results should be considered encouraging enough to continue with the adopted treatment policy.
References
- 1.Benati A, Beltramello A, et al. Endovascular treatment of intracranial AVMs. Combined embolization with a multi-purpose mobile-wing microcatheter system. J. Neuroradiology. 1987;14:99–113. [PubMed] [Google Scholar]
- 2.Benati A, Beltramello A, et al. Endovascular treatment of intracranial AVMs by means of wing microcatheter: technique, clinical and pathological results; Proceedings of XVth Congress of European Society of Neuroradiology; Wurzburg. 1988. [Google Scholar]
- 3.Nadjimi M, editor. Berlin Heidelberg: Springer-Verlag; 1989. [Google Scholar]
- 4.Beltramello A, Benati A, et al. Interventional angiography in neuropediatrics. Child's Nerv Syst. 1989;5:87–93. doi: 10.1007/BF00571116. [DOI] [PubMed] [Google Scholar]
- 5.Benati A, Beltramello A, et al. Preoperative embolization of arteriovenous malformations with polylene threads: techniques with wing microcatheter and pathologic results. Am J Neuroradiol. 1989;10:579–586. [PMC free article] [PubMed] [Google Scholar]
- 6.Beltramello A, Benati A, et al. Neuroradiologic evaluation of intracranial angiomas. Rivista di Neuroradiologia. 1990;3:133–142. [Google Scholar]
- 7.Pasqualin A, Scienza R, et al. Treatment of cerebral arteriovenous malformations with a combination of preoperative embolization and surgery. Neurosurgery. 1991;29:358–368. doi: 10.1097/00006123-199109000-00004. [DOI] [PubMed] [Google Scholar]
- 8.Nicolato A, Foroni R, et al. Leksell gamma knife radiosurgery for cerebral arteriovenous malformations in pediatric patients. Childs Nerv Syst. 2005;21:301–7. doi: 10.1007/s00381-004-1049-5. [DOI] [PubMed] [Google Scholar]