Summary
The crucial question - treat or not a brain arteriovenous malformation - has been the object of many studies, sometimes contradictory. The authors analyse retrospectively, clinically and angiographically, the results of the intra-arterial embolization in the treatment of 106 patients with brain arteriovenous malformation. The endo-vascular therapy was palliative or curative in 46% of the cases, in 30% of the patients the embolization was pre-surgery and in 18% the intra-arterial occlusion was pre-radiosurgery. In 6% the therapeutic protocol included embolization with surgery and radiosurgery. Cyanocrylate was used in 89% of the cases, and in 10% of the patients the embolic material used was Ethylene - vinyl alcohol copolymer - EVOH (Onyx). In this series 11% of total morbidity occurred - transitory in 8% and settled with permanent neurological deficit in 3% of the patients. The mortality post-embolization was 2% and the total mortality post-embolization and surgery was 3%. Total angiographic exclusion immediately post-embolization was confirmed in 24% of the cases. The mean period for clinical and angiographic follow-up was 38 months. 72 patients - 77% of the cases discharged from hospital showed complete exclusion of the lesion after the different combined therapeutic strategy - embolization, surgery and radiosurgery. New retrospective and long-term prospective studies based on the actual therapeutic protocols and new embolic agents are necessary to be able to evaluate accurately a new therapeutic reality in the brain arteriovenous malformations.
Key words: endovascular treatment, intra-arterial embolization, follow-up, brain arteriovenous malformation, surgery, radiosurgery.
Introduction
The brain arteriovenous malformation (brain AVM) is the most frequent intra-cranial symptomatic vascular malformation, being the second most common cause of spontaneous cerebral haemorrhage in an adult1. It is usually diagnosed before the age of forty and according to Olivecrona and Yasargil, a higher occurrence in males is noticed. A brain AVM can show itself clinically in different ways, being the most frequent intra-cranial haemorrhage - 68% to 72% (parenchymatosis, intra-ventricular, subarachnoid or combined), epilepsy - 18% to 25%, neurological progressive deficit - 7% and headache with an incidence between 5% and 35% 2. The occurrence of intra-cranial haemorrhage in a brain AVM has been estimated between 2% to 4% yearly, increasing the risk of a re-haemorrhage to 6% yearly, with a mortality of 10% to 15% for each haemorrhagic accident3.
The problem - to treat or not a brain AVM - has been the object of countless studies, sometimes non-agreeable 4. It must be emphasised that is difficult to compare the results obtained in patients treated in a conservative manner with the ones submitted to invasive therapeutics, considering the fact that the great majority of the series are retrospective, including selected cases, not mentioning the time break that precedes or follows the diagnosis. In the cooperative study - Perret and Nishioka5 found a mortality of 5% in untreated cases and 12% in patients submitted to surgery. Under these circumstances, Perret and Nishioka defend that the validity of the surgery implies mortality inferior to 10% and post-operating morbidity better or comparable to patients treated in a conservative manner. The therapeutic approach of the brain AVM has known, in the last decades, profound alterations with fast progress as far as microneurosurgery techniques 1, endo-vascular therapy 6 and stereotactic radiosurgery 7,8. This new reality demands new long-term retrospective and prospective studies, based on the actual therapeutic protocols, used separately or associated in a way that results decurrent from the synergism of these various treatments can be obtained.
Patients and Method
The Neurovascular Pathology Section of the Department of Neurosciences at Hospital Sta. Maria - University of Lisbon - has treated, up to now, 112 patients with brain AVM. From this total, 6 cases of patients treated with our collaboration at other hospital units were excluded. Therefore, therapeutic protocols and results of 106 patients are analysed, from which 10 are still under treatment. As far as all these patients are concerned, the therapeutic orientation was decided in a joint meeting of Neuroradiology, Neurosurgery and Neurology - Neurovascular group. The endo-vascular interventions were performed under sedation and neuroanalgesia until 1998, this orientation being motivated by the systematic realization of Amytal Test in the intra-arterial embolizations. The abandonment of this neurofunctional evaluation test determined that presently, in our institution, the intra-arterial embolization in the brain AVM be performed under general anaesthesia. The pharmacological protocol during the endo-vascular occlusion includes steroids I.V., heparinization with 10.000 to 5.000 units in bolus, followed by 1.000 units/hour and when necessary, intra-arterial Nimodipine - vasospasm. With the exception of some cases where venous thrombosis is suspected, Heparine is reverted at the end of surgery. In deep and posterior fossa brain AVM, the intervention is performed with controlled arterial hypotension, which is maintained in the first 24 hours post-embolization. The diligences taken post-endovascular occlusion include 24 hours in the Intensive Care Unit and the great majority of patients are discharged on the fourth day post-embolization. In brain AVM's with larger dimensions - more than 3cms, it is our policy, whenever possible, to program various interventions - serial embolizations. Surgery and radiosurgery, when suggested, are usually performed between the 2 and 4 weeks post-embolization, when intense inflammatory reaction is no longer noticed and the haemodynamic alterations are stabilised. Most of our cases present themselves clinically with haemorrhage. The patients' age varied between 6 and 70 years and a discreet predominance of the male sex was identified. With regards to lesions treated, the majority is localised on the left cerebral hemisphere 50%, with a slight bigger incidence on the temporal lobe. The therapeutic strategy was the curative embolization in 33% of the patients. As embolic material we used Cyanocrylate in 95 of the cases. It is important to emphasize however that since 2003 Ethylene - vinyl alcohol copolymer - EVOH (Onyx) has been used more often - 10 patients. In our series the clinical and angiographic follow-up of the patients treated by endo-vascular approach has a mean period of 38 months.
Results
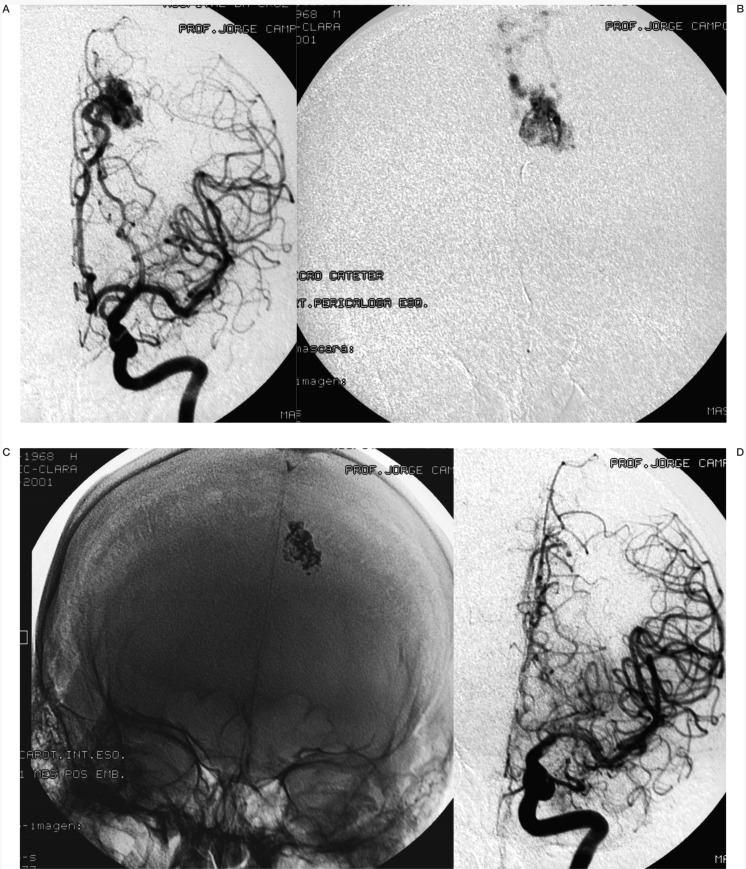
A complete angiographic exclusion of the brain AVM immediately after an intra-arterial embolization was observed in 24 patients (figure 1). As far as the follow-up - latter morphological angiographic results - this increases significantly, with emphasis on the complete exclusion of the lesion in 77% of the cases treated with different therapeutic protocols, namely embolization and surgery (figure 2), embolization and radiosurgery (figure 3) and embolization with surgery and radiosurgery (figure 4). During the endo-vascular therapy 9 technical complications occurred including 3 microcatheters glued or trapped in the arterial feeder, in all instances with no clinical problems. 2 arterial ruptures. 1 case of Cyanocrylate reflux to the parent artery and 3 cases of venous outflow occlusion must also be mentioned. With regards to morbidity - clinical complications - transitory symptoms in 8 patients are noticed - 3 cases of ischemic nature and 5 haemorrhagic events including 3 minor subarachnoid haemorrhages and 2 right temporal hematoma with complete recovery. Settled neurological deficit occurred in 3 patients - one ischemic with quadrantopsy, one right parietal venous haemorrhagic infarction and a severe left temporal hematoma. The post-embolization mortality was 2% and 1 patient died after surgery. The clinical outcome post-therapeutic protocol shows 93% of favourable cases - total or partial exclusion of the nidus with clinical improvement or without worsening of the symptoms.
Figure 1.
Left parietal AVM presented with seizures. A) Frontal left carotid artery angiogram pre-embolization. B) Microcatheterism of the nidus-frontal view. C) Frontal X-Ray without subtraction-cyanocrylate cast. D) Follow-up left carotid artery angiogram, one month post-embolization (glue).
Figure 2.
Right cerebellum AVM presented with hemorrhage. A) CT scan. B) Frontal left vertebral artery angiogram pre-embolization. C) Microcatheterism of the left PICA. D) Microcatheterism of the right AICA - shows a small intranidal aneurism. E) Frontal right vertebral artery angiogram postembolization (glue) and surgery. F) Frontal left vertebral artery angiogram post-embolization (glue) and surgery.
Figure 3.
Left parietal / temporal AVM with seizures. A) Frontal left carotid artery angiogram pre-embolization. B) Frontal X-Ray without subtraction - cyanocrylate cast. C) Frontal left carotid artery angiogram post-embolization (glue). D) Follow-up left carotid angiogram three years post-embolization and radiosurgery.
Figure 4.
Left temporal AVM presented with hemorrhage. A) CT scan. B) Frontal left carotid artery angiogram pre-embolization. C) Microcatheterism of the left anterior temporal artery. D) Follow-up left carotid artery angiogram six years post-embolization (glue), surgery and radiosurgery.
Discussion
A brain AVM is usually diagnosed before the age of 40, corresponding to 72% of the cases of our series. This lesion presents a cumulative risk of haemorrhage of 4% yearly 4, translated in its clinical presentation - 53% of our patients showed cerebral haemorrhage. In spite of some authors like Aminoff and Elstein having preconized a more conservative treatment, the age group and the haemorrhagic risk already referred to, have supported an invasive therapeutic indication, aiming at the surgical removal of the brain AVM or excluding it from the circulation by means of intra-arterial embolization or radiosurgery 6. The management of these vascular malformations can also involve various associated forms of these therapeutic modalities. In our series 32% of the patients were treated with curative embolization (figure 5), 30% with pre-operative embolization (figure 6), pre-radiosurgery embolization was performed in 17% of the cases (figure 7) and embolization with surgery and radiosurgery was done in 6% of the patients. A partial target embolization came to 13% of the series and it must be pointed out that stabilization of the symptoms occurred in most of the patients treated with palliative arterial occlusion. Although Cyanocrylate had been used as embolic material in 95 of the analysed cases, in the last 2 years the number of brain AVM treated with Ethylene - vinyl alcohol copolymer - EVOH (Onyx) - has increased significantly - 10 patients9. In one case the afferent artery of the vascular malformation was occluded presurgically with coils. In our institution other embolic materials such as PVA particles, silk and Ethanol are not used in brain AVM embolization10.
Figure 5.
Vermis AVM presented with headache. A) Frontal right vertebral artery angiogram pre-embolization. B) Lateral microcatheterism of the right PICA. C) Lateral microcatheterism of the right AICA. D) Frontal X-Ray without subtraction-Onyx cast. E) and F) Follow-up right and left vertebral artery angiograms one year post-embolization (Onyx).
Figure 6.
Left frontal AVM presented with hemorrhage. A) Lateral left carotid artery angiogram pre-embolization. B) Microcatheterism of the nidus-shows a proximal aneurysm in the feeder artery. C) Lateral X-Ray without subtraction-onyx cast. D) Lateral left carotid artery angiogram post-embolization (Onyx). E) and F) Lateral and frontal left carotid artery angiograms post-embolization and surgery.
Figure 7.
Right parietal AVM presented with hemorrhage. A) Lateral right carotid artery angiogram pre-embolization. B) Microcatheterism of the nidus. C) Lateral X-Ray without subtraction-cyanocrylate cast. D) Lateral right carotid artery angiograms post-embolization (glue). E) and F) Follow-up right and frontal carotid artery angiogram five years post-embolization and radiosurgery.
The Amytal Test11 was systematically used for pre-embolization neurofunctional evaluation until 1998. Since then, the non-significant results obtained with this physiologic testing associated with the implementation of intranidal microcatheterism and the necessity of general anaesthesia led to its progressive abandonment. With regards to the utilization versus non-utilization of Heparine during an endovascular intervention in brain AVM 12, it is still part of our protocol to perform the embolization under heparinization. With this orientation it must be pointed out that in our series only 3 transitory ischemic events occurred, all with no evidence of thromboembolic problems, and one case of post-embolization quadrantopsy also showed no evidence of inadverted arterial occlusion. When analysing the technical complications, the 3 cases of microcatheters trapped in the arterial feeder, as it was mentioned by other authors 13, did not condition clinical problems. In the 2 cases of post-embolization mortality, one was caused by Cyanocrylate reflux to the basilar artery and the other resulted from delayed left temporal haemorrhage - partial venous outflow occlusion14. Regarding morbidity, we also refer 2 cases of right temporal hematoma with favourable neurological evolution and which were also related to venous occlusion. These occurrences confirm the importance of an adequate time of Cyanocrylate polymerisation, as well as a strict control of its injection. As far as the clinical outcome, and in spite of being a small series, the 94% of cases considered of favourable evolution stand out, which seems to confirm the actual impact of intra-arterial embolization in the treatment of brain AVM.
Table 1.
Endovascular Therapy in Brain AVM
| 106 patients | |||
|---|---|---|---|
| 50 female 47% |
53 male 53% |
||
| Age | |||
| Up to 9 | 3 | 15% | |
| 10 up to 20 | 13 | ||
| 21 up to 30 | 29 | 57% | |
| 31 up to 40 | 31 | ||
| 41 up to 50 | 13 | 23% | |
| 51 up to 60 | 12 | ||
| 61 up to 70 | 5 | 5% | |
| University of Lisbon | |||
Table 2.
Endovascular Therapy in Brain AVM
| 106 patients - Presenting symptoms | ||
|---|---|---|
| Haemorrhage | 56 | 53% |
| Seizures | 35 | 33% |
| Progressive neurologic deficit |
9 | 8% |
| Headache | 13 | 6% |
| University of Lisbon | ||
Table 3.
Endovascular Therapy in Brain AVM
| Presenting symptoms Haemorrhage |
Age 56 patients |
|
| Up to 9 | 3 | 73 % |
| 10 up to 20 | 11 | |
| 21 up to 30 | 16 | |
| 31 up to 40 | 11 | |
| 41 up to 50 | 9 | 27 % |
| 51 up to 60 | 3 | |
| 61 up to 70 | 3 | |
| University of Lisbon | ||
Table 4.
Endovascular Therapy in Brain AVM
| Presenting symptoms Seizures |
Age 35 patients |
|
| 10 up to 20 | 4 | |
| 21 up to 30 | 13 | 83% |
| 31 up to 40 | 12 | |
| 41 up to 50 | 2 | 17% |
| 51 up to 60 | 4 | |
| University of Lisbon | ||
Table 5.
Endovascular Therapy in Brain AVM
| Presenting symptoms Progressive Neurologic Deficit |
Age 9 patients |
|
| 21 up to 30 | 2 | 83% |
| 31 up to 40 | 5 | |
| 41 up to 50 | 1 | 22% |
| 51 up to 60 | 1 | |
| University of Lisbon | ||
Table 6.
Endovascular Therapy in Brain AVM
| Presenting symptoms Headache |
Age 6 patients |
|
| 21 up to 30 | 1 | |
| 31 up to 40 | 1 | 50% |
| 41 up to 50 | 1 | |
| 51 up to 60 | 1 | 50% |
| 61 up to 70 | 2 | |
| University of Lisbon | ||
Table 7.
Endovascular Therapy in Brain AVM
| AVM Localization | 106 patients | ||
|---|---|---|---|
| Frontal | 21 | 20% | Right 6 Left 15 |
| Parietal | 21 | 25% | Right 12 Left 14 |
| Temporal | 36 | 34% | Right 17 Left 19 |
| Occipital | 9 | 8% | Right 4 Left 5 |
| Corpus callosum | 1 | 1% | |
| Basal ganglia | 1 | 1% | |
| Cerebellum | 12 | 11% | |
| University of Lisbon | |||
Table 8.
Endovascular Therapy in Brain AVM
| Therapeutic Strategy | 96 patients | |
|---|---|---|
| Pre operative embolization | 29 | 30% |
| Pre radiosurgery embolization | 17 | 18% |
| Pre operative and radiosurgery embolization |
26 | 25% |
| Curative embolization | 32 | 33% |
| Partial targeted embolization (palliative) |
12 | 13% |
| 10 patients remain in treatment | ||
| University of Lisbon | ||
Table 9.
Endovascular Therapy in Brain AVM
| Intraarterial embolization - embolic material 106 patients | |
|---|---|
| Cyanocrylate | 95 cases |
| Coils | 1 case |
| Ethylene-vinyl alcohol copolymer-EVOH (Onyx) |
10 cases |
| University of Lisbon | |
Table 10.
Endovascular Therapy in Brain AVM
| Clinical and Angiographic Follow-up Period 96 patients | ||
|---|---|---|
| 3 months | 7 | 16% |
| 6 months | 8 | |
| 1 year | 19 | 44% |
| 2 years | 23 | |
| 3 years | 9 | 24% |
| 4 years | 9 | |
| 5 years | 5 | |
| 6 years | 2 | 16% |
| 7 years | 2 | |
| 8 years | 6 | |
| 9 years | 2 | |
| 11 years | 2 | |
| 14 years | 2 | |
| Mean follow-up period 38 month 10 patients remain in treatment | ||
| University of Lisbon | ||
Table 11.
Endovascular Therapy in Brain AVM
| Technical Complications (106 patients) |
9% |
|---|---|
| Microcatheters glued or trapped in the arterial feeder without clinical problems |
3 |
| Arterial ruptures | 2 |
| Cyanocrylate reflux | 1 |
| Venous outflow occlusions | 3 |
| University of Lisbon | |
Table 12.
Endovascular Therapy in Brain AVM
| Morphological Angiographic Results Immediately post embolization 106 patients | ||
|---|---|---|
| Complete angiographic exclusion | 24 | 23% |
| 90% exclusion | 42 | 39% |
| 80% exclusion | 14 | 13% |
| 70% exclusion | 11 | 10% |
| 60% exclusion | 7 | 7% |
| 50% exclusion | 3 | 3% |
| 40% exclusion | 5 | 5% |
| University of Lisbon | ||
Table 13.
Endovascular Therapy in Brain AVM
| Clinical Complications (106 patients) | ||
|---|---|---|
| Total Morbidity | 11% | |
| Transient neurologic defice with complete recovery |
8 patients 8% |
|
| Ischemic | 3 cases | |
| Haemorrhage | 5 cases | |
| Minor SAH | 3 cases | |
| Delayed right temporal hematoma | 2 cases | |
| Permanent neurologic defice | 3 patients 3% |
|
| Mild defice - ischemic | 1 cases | |
| Severe defice - haemorrhage | 2 cases | |
| University of Lisbon | ||
Table 14.
Endovascular Therapy in Brain AVM
| Intraarterial embolizations (106 patients) |
Mortality 2% |
|---|---|
| Related to embolizations | 2 patients |
| Reflux of cyanocrylate to the basilar artery |
1 case |
| Severe delayed hematoma caused by venous outflow occlusion |
1 case |
| University of Lisbon | |
Table 15.
Endovascular Therapy in Brain AVM
| Morphological Angiographic Results 93 patients |
Follow up | |
| Complete angiographic exclusion | 72 | 77% |
| Intraarterial embolization | 24 | 33% |
| Embolization and surgery | 28 | 39% |
| Embolization and radiosurgery | 14 | 20% |
| Embolization, surgery and radiosurgery |
6 | 8% |
| 10 patients remain in treatment and 3 patients don't have follow up | ||
| University of Lisbon | ||
Table 16.
Endovascular Therapy in Brain AVM
| Morphological Angiographic Results 93 patients |
Follow up | ||
| Partial angiographic exclusion | 21 | 23% | |
| Post embolization | 6 | ||
| 90% | Post embolization and surgery | 1 | |
| Post embolization and radiosurgery | 2 | ||
| 80% | Post embolization | 3 | |
| Post embolization and radiosurgery | 1 | ||
| 70% | Post embolization | 3 | |
| 60% | Post embolization | 2 | |
| ≤50% | Post embolization | 3 | |
| 10 patients remain in treatment and 3 patients don't have follow up | |||
| University of Lisbon | |||
Table 17.
Endovascular Therapy in Brain AVM
| Clinical outcome post therapeutic protocol 96 patients | ||
| Favourable | Morphological cure or partial exclusion with improvement or stable clinical condition |
94% |
| Unfavourable | Death or worsening of the symptoms (1 patient died after surgery) |
6% |
| 10 patients remain in treatment | ||
| University of Lisbon | ||
Conclusions
Nowadays, intra-arterial embolization holds a central position in the therapeutic protocol of the brain AVM. It can be used on its own - curative or palliative, and can be associated with surgery and radiosurgery.
The indication for brain AVM embolization and respective therapeutic protocol must be sensible, considering the risk/benefit and involves a multidisciplinary team dedicated to the Neurovascular Disease - Interventional Neuroradiologists, Neurologists, Neurosurgeons.
The enormous progress in microcatheter and microguiding systems, as well as the appearance of new embolic materials - Onyx, made possible that a higher percentage of patients with excellent clinical outcome and the reduction of morbidity and mortality in the endovascular intervention be achieved.
New long-term retrospective and prospective studies based on therapeutic arterial protocols are necessary to evaluate with rigour a new therapeutic reality in brain AVM.
References
- 1.Yasargil MG. AVM of the Brain, clinical considerations. In: Yasargil MG, editor. Microneurosurgery. Vol. III B. Stuttgart: George Thieme Verlag; 1988. [Google Scholar]
- 2.Rigamonti D, Spetzler RFM, et al. cerebral vascular malformations. BNI Quarterly. 1987;3 [Google Scholar]
- 3.Wilkins RH. Natural history of intracranial vascular malformations. A review. Neurosurgery. 1985;16:421–430. doi: 10.1227/00006123-198503000-00026. [DOI] [PubMed] [Google Scholar]
- 4.Crawford RM, West CR, et al. Arteriovenous malformations of the brain - Natural history in unoperated patients. Journal of Neurology, Neurosurgery and Psychiatry. 1986;49:1–10. doi: 10.1136/jnnp.49.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Perret G, Nishioka H. Arteriovenous Malformations. An analysis of 545 cases of craniocerebral arteriovenous malformations and fistulae reported to the cooperative study. J. Neurosurgery. 1966;25:467–490. doi: 10.3171/jns.1966.25.4.0467. [DOI] [PubMed] [Google Scholar]
- 6.Berenstein A, Lasjaunias P, et al. Cerebral Vascular Malformations. In: Berenstein A, Lasjaunias P, Ter Brugge KG, editors. Surgical NeuroAngiography. Vol. 2.2. Berlin: Springer; 2004. [Google Scholar]
- 7.Dawson RC, Tarr RH, et al. Treatment of arteriovenous malformations of the brain and stereotactic radiosurgery. Results after 1 and 2 years. Am J Neuroradiol. 1990;11:857–864. [PMC free article] [PubMed] [Google Scholar]
- 8.Pollock BE, Lunsford LD, et al. The Role of Embolization in combination with stereotactic Radiosurgery in the Management of Pial and Dural Arteriovenous Malformations. In: Connors J.J., Wojak J.C., et al., editors. Interventional Neuroradiology Strategies and Practical Techniques. Philadelphia: W.B. Saunders Company; 1999. [Google Scholar]
- 9.Florio F, Lauriola W, et al. Endovascular treatment of intracranial arteriovenous malformations with Onyx embolization. Preliminary Experience Radiol Med. 2003;106:512–520. [PubMed] [Google Scholar]
- 10.Marks MP. Endovascular Therapy for Arteriovenous Malformations. In: Marks M.P., Do H.M., editors. Endovascular and Percutaneous Therapy of the Brain and Spine. Philadelphia: Lippincott Williams & Wilkins; 2002. [Google Scholar]
- 11.Vinuela F. Update on intravascular functional evaluation and therapy of intracranial arteriovenous malformations. In: Vinuela F, Dion J, Duckwiller G, editors. NeuroImaging clinics of North America - Interventional Neuroradiology. Vol. 2. Philadelphia: Nº 2, W.B. Saunders Company; 1992. [Google Scholar]
- 12.Wikholm G, Pellettieri L, Karlsson B. Treatment of Arteriovenous Malformations of the Brain. In: Byrne J., editor. Interventional Neuroradiology. New York: Oxford University Press; 2002. [Google Scholar]
- 13.Aletich VA, Debrun G.M. Intracranial Arteriovenous Malformations. The Approach and Technique of Cyanocrylate Embolization. In: Connors J.J., Wojak J.C., editors. Interventional Neuroradiology Strategies and Practical Techniques. Philadelphia: W.B. Saunders Company; 1999. [Google Scholar]
- 14.Berenstein A, Lasjaunias P, et al. Endovascular Treatment of Arteriovenous Malformations of the Brain. In: Valavanis A, editor. Interventional NeuroRadiology. Verlag Berlin: Springer; 1993. [Google Scholar]