Summary
This retrospective study aimed to assess the percentage of complications in the daily practice of cerebral and spinal cord diagnostic angiography at our institution and to compare this with literature reports published in the last twenty years and guidelines for angiography.
From 1st December 1998 to 1st December 2003 2154 patients underwent digital angiography for a total of5996 vessels selected.
Three neurological complications arose during angiographic procedures in the five year period.
-
•
Focal neurological deficit resolving within 24h in two patients,
-
•
Permanent neurological deficit in one patient.
There were no adverse systemic reactions to contrast medium.
Retrospective analysis of our cohort disclosed a complication rate of 0.1% for transient neurological complications and 0.05% for permanent deficits.
Key words: cerebral angiography, spinal cord angiography, complications
Introduction
The gold standard in the diagnostic work up for vascular diseases of the nervous system remains digital arterial angiography. The increased use of newer, non-invasive vascular imaging methods including ultrasound, CT and MR angiography has led to increased scrutiny of the indications and complications rates of diagnostic angiography.
We concur with the diagnostic potential of CT angiography and MR angiography, but many literature reports have emphasized the invasive nature of traditional angiography2,15,18,19,22,23,24 and its complication rate. For this reason, we calculated the incidence of complications in patients undergoing angiography at our institution in the last five years, comparing it with literature reports published in the last twenty years8,9,12,16,25,26and guidelines for angiography1,4.
Material and Methods
From 1st December 1998 to 1st December 2003 2154 patients aged from 3 to 84, average age 53,2 years, underwent digital angiography for a total of 5996 vessels selected. 22% of patients underwent two or more angiographic procedures.
From 1st December 1998 to August 2002 angiography was carried out on a Philips Integris BV 3000 system and from September 2002 to December 2003 on GE Advantx biplane device.
2154 patients undergoing angiography in the period from 1st December 1998 to 1st December 2003 were referred in three different ways: 1731 patients admitted to wards in our institution (80%), 160 patients attending the Day Hospital of the Department of Neurosciences at our Hospital (8%) and 263 patients sent from other hospitals for angiograms performed at our Hospital (12%).
The main disorders requiring referral for angiography were: subarachnoid haemorrhage (30%), intraparenchymal haematoma (10%), arteriovenous malformations (6%), brain (35%) and spine-spinal cord (9%) tumours, and carotid atheromatous disease (5%).
The cerebral circulation and spinal nerve roots are examined by a standard procedure outlined in the operating instructions listed in our unit's quality control documentation certified ISO 9001/2000. This document plans, records and checks all diagnostic and interventional procedures undertaken in the Angiography Suite from informing and preparing patients to execution of the procedure, reporting and PACS data storage7.The documentation also describes the technique and materials to be used during the procedure from arterial puncture to the standard radiological views of each vascular axis.
Before the examination a venous catheter is inserted into all patients and heart rate, arterial pressure and capillary oxygen saturation are monitored throughout the procedure.
Diagnostic angiography is done with 4 Fr. catheters inserted by retrograde puncture of the femoral artery through an introducer continuously washed under pressure with saline solution. On average, half of the angiographic procedures required only one 4 Fr catheter whereas the other half needed two or more catheters. The hydrophilic guide wire is used on average once in every two examinations and is left in place within the catheter for less than 60 seconds.
Water soluble non-ionic iodate contrast agent is used (iopamidol 300) at a dosage related to the vascular axis under examination (common carotid artery 12 ml at 6 ml/s, internal carotid artery 8 ml at 4 ml/s, external carotid artery 5 ml at 2 ml/s, vertebral artery 6 ml at 3 ml/s) with a PSI of 300. These are standard values but the neuroradiologist performing the examination is entitled to adjust the study protocol adapting it the individual needs of each patient (table 1).
Table 1.
Distribution of vessels examined.
| Vascular axis | Number of vascular axes examined |
|---|---|
| Common carotid artery | 1529 |
| Internal carotid artery | 1595 |
| External carotid artery | 408 |
| Vertebral artery | 1710 |
| Spinal cord angiography | 302 |
| Other vessels | 452 |
| Total | 5996 |
Only saline solution and not heparinized saline solution is used either in infusion or to wash materials.
Angiography is performed by experienced neuroradiologists. Staff in training are flanked by an expert neuroradiologist responsible for checking all actions and ready to intervene promptly if necessary. This organization largely abolishes the "learning curve" factor.
We adopted the following criteria to define the expertise required to undertake diagnostic angiography:
"those entitled to work independently in this sector must provided written evidence of have carried out and reported on at least 100 procedures in the past two years of which 50 as the first neuroradiologist. Maintenance of clinical skill after five years of continuous interventional neuroradiology activity entails the execution of at least 50 procedures a year as first or second neuroradiologist".
These criteria were officially implemented in our Region by regional law n° 594/00, subsequently referred to in regional law n° 327/04 defining the "General and specific requirements for accreditation in hospitals in the Emilia Romagna region".
At the end of the angiographic procedure patients are kept on the ward for at least an hour. Before being taken back to their refer-ring wards, patients' neurological status and puncture site are checked. Post-procedural recommendations are specified in the angiography report (bed rest for at least 24h, examination of the puncture site and ipsilateral dorsalis pedis artery pulse) together with information on 24 hour cover by a neuroradiologist in case of complications.
To assess the incidence of complications, data were collected from the electronic files storing radiological information in our neuroradiology unit. The radiology file contains two compulsory fields to be used for statistical purposes and two free fields for notes.
The information to be recorded for angiography includes: patient's personal details, degree of referral urgency, referring institution, doctors, technicians and nurses carrying out the procedure, vascular districts examined, material and drugs used, vital parameters on admission and any major changes arising during the procedure, time of the start and end of the procedure, reason for referral, examination report, ACR classification of angiography findings and onset of any complications. Moreover the medical personal files of the patients, form the different wards, have been reviewed.
We also did a MEDLINE search inserting the key words: cerebral angiography, adverse effects, and complication rates to compare our findings with those of leading studies published in the last twenty years 8,9,12,16,25,26,27 and guidelines for angiography1,4.
Results
We reviewed all complications arising during diagnostic angiography procedures at our institution from 1/12/1998 to 1/12/003. Our radiological filing system contains four broad groupings:
-
1.
Neurological complications
-
2.
Minor systemic complications caused by contrast administration
-
3.
Major systemic complications caused by contrast administration
-
4.
Local complications.
Each group contains a further breakdown of complications as listed in table 2.
Table 2.
Complications.
| 1. |
Neurological complications 1.1. transient focal neurological deficit 1.2. permanent focal neurological deficit |
| 2. |
Minor complications caused by contrast administration 2.1. nausea/vomiting 2.2. vagal seizures 2.3. headache 2.4. vertigo 2.5. skin rash |
| 3. |
Major complications caused by contrast administration 3.1. thromboembolism 3.2. cardiorespiratory seizures 3.3. cardiocirculatory seizures 3.4. hypertensive seizures 3.5. glottic oedema 3.6. anaphylactic shock 3.7. acute renal failure |
| 4. |
Local complications 4.1. inguinal haematoma 4.2. intimal dissection 4.3. arterial thrombosis 4.4. fragmented atheromatous plaque 4.5. vasospasm 4.6. pseudoaneurysm 4.7. arteriovenous fistula 4.8. nerve lesion 4.9. infection |
Table 3.
Results of leading studies on complications arising during neuroangiography.
| Author | Journal | Year | N° patients |
N° vascular axes examined |
Transient complications |
Permanent complications |
|---|---|---|---|---|---|---|
| Earnest F. et Al | AJR | 1984 | 1517 | 2.3% | 0.3% | |
| Dion J.E. et Al | STROKE | 1987 | 1002 | 1.3% | 0.1% | |
| Waugh J.R. et Al | Radiology | 1992 | 939 | \\ | 0.3% | |
| Heiserman J. et Al | AJNR | 1994 | 688 | 1000 | 1% | 0.5% |
| Leffers M. et Al | Acta Radiol | 2000 | 453 | 2.3% | 0.4% | |
| Willinsky R. et Al | Radiology | 2003 | 2899 | 0.9% | 0.5% | |
Group 1
Neurological complications are defined as the onset of a new neurological sign or worsening of a pre-existing sign during the angiographic procedure or in the following 24h. If the neurological deficit resolves the complication is deemed transient, if it persists it is termed permanent.
Three complications occurred during the five year period examined.
• In two patients the neurological deficit arose at the end of the procedure and resolved within 24h. One patient had upper limb paralysis which resolved spontaneously within six hours and the other had a hemiparesis which subsided around 12 hours later.
• One patient had permanent neurological deficit. This 64-year-old woman was admitted to our institution for subarachnoid haemorrhage and an initial angiogram was done within 24h after onset of symptoms to search for an aneurysm. Injection of contrast medium into the left subclavian artery at the origin of the vertebral artery disclosed severe narrowing of the entire cervical segment of the vertebral artery alternating with small filiform segments probably caused by arterial dissection or arteritis without aneurysms (figure 1). Injection of contrast medium into the controlateral vertebral artery displayed complete vascularization of the vertebrobasilar circulation with the antero-inferior cerebellar arteries highly developed bilaterally due to an anatomical variant with absence or hypoplasia of the postero-inferior cerebellar arteries (figure 2). Failure to detect an aneurysm and no clear-cut explanation for the subarachnoid haemorrhage led to follow-up cerebral angiography eight days after the acute event (figure 3). On this occasion the left vertebral artery was selectively injected, and angiographic findings remained unchanged. At the end of the procedure the patient complained of headache and some minutes later lost consciousness with stertorous respiration; GCS was five. Reanimation was performed immediately by endotracheal intubation and cerebral angiography repeated. Injection of contrast medium into the right vertebral artery disclosed a thrombosis in the middle third of the basilar artery sparing the antero-inferior cerebellar arteries (figure 4) interpreted as due to emboli from the left vertebral artery. Mechanical thrombolysis was undertaken by co-axial catheterization (Envoy 5F, Excel 14 e Dasher 0.14) inserting the micro-catheter into the thrombus and then injecting 800.000 IU of Urokinase initially in a bolus of 200.000 IU and then by slow infusion (90 minutes) of the remaining 600.000 IU (figure 5). At the end of the procedure the basilar artery appeared partially recanalized with injection of the superior cerebellar arteries and the apex and proximal portion of the left posterior cerebral artery (segment P1-P2) (figure 6). Injection of the posterior cerebral artery was seen from the carotid siphon whereas on the left there was a markedly delayed circulation of the temporooccipital territory of the posterior cerebral artery with late retrograde pial compensation. Sedation was then diminished for the purposes of neurological assessment which yielded a GCS of 9-10. The patient developed left mesial temporo-occipital ischaemia and a smaller ipsilateral cerebellar ischaemic lesion (figure 7) with persistence of a campimetric deficit and ideomotor slowing on discharge.
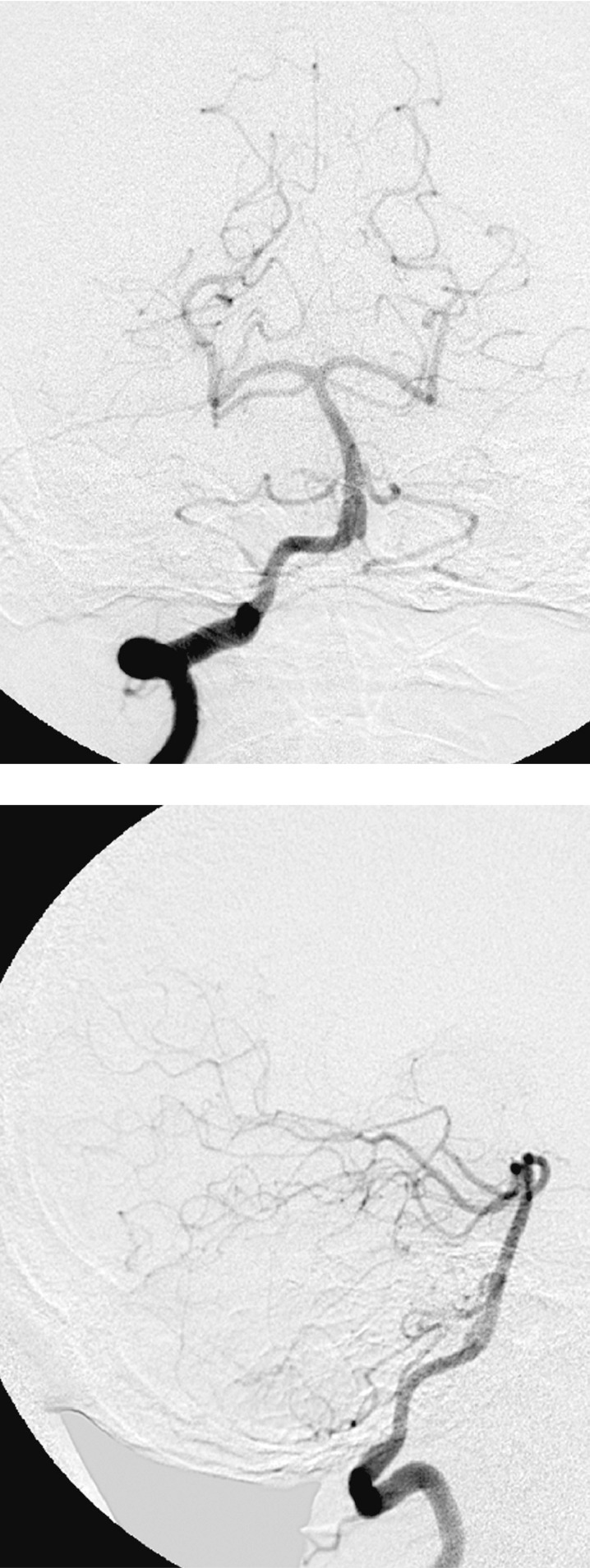
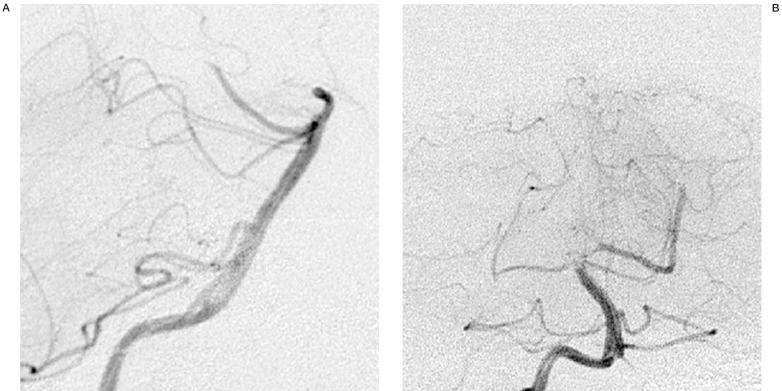
Figure 1.
A,B) First angiography: left vertebral artery with irregular morphology and filiform shape.
Figure 2.
First angiography: right vertebral artery showing compensation through the antero-inferior cerebellar arteries highly developed bilaterally due to an anatomic variant with absent or hypoplastic postero-inferior cerebellar arteries.
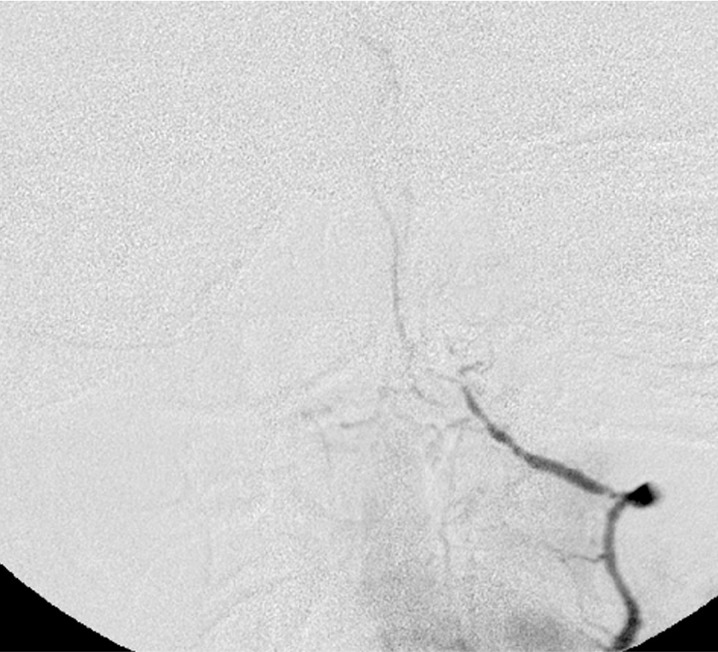
Figure 3.
Second angiography (eight days after the acute event): angiographic findings unchanged.
Figure 4.
Third angiography (undertaken immediately after the second due to onset of headache and loss of consciousness): thrombosis of the middle third of the basilar artery sparing the antero-inferior cerebellar arteries.
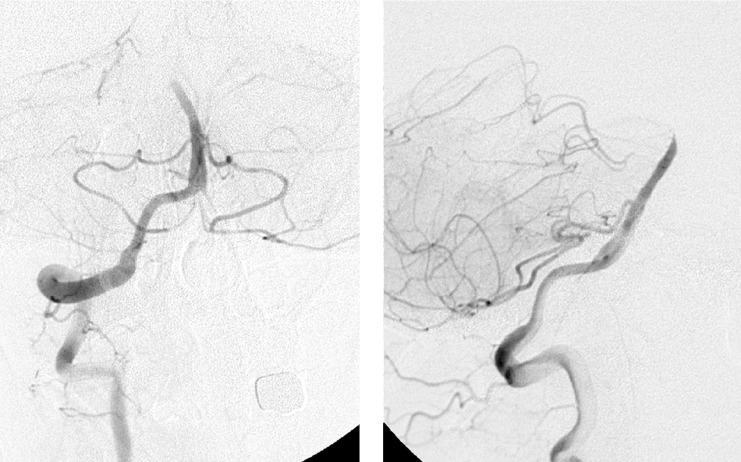
Figure 5.
Mechanical thrombolysis with insertion of the guiding catheter into the thrombus and injection of Urokinase.
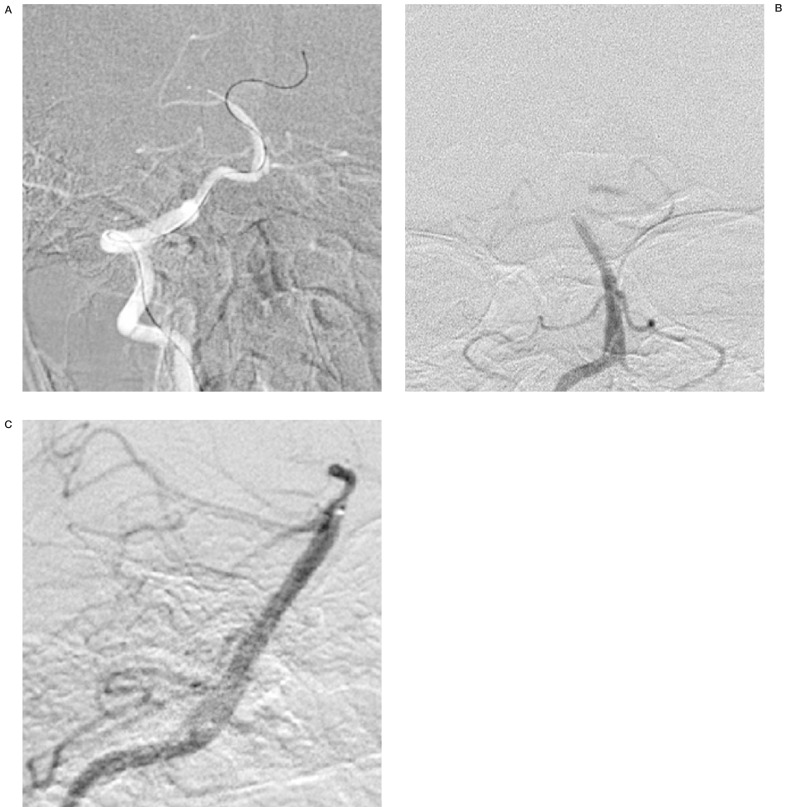
Figure 6.
Partial recanalization of the basilar artery with injection of the superior cerebellar arteries and the apex and proximal portion of the left posterior cerebral artery (segment P1-P2).
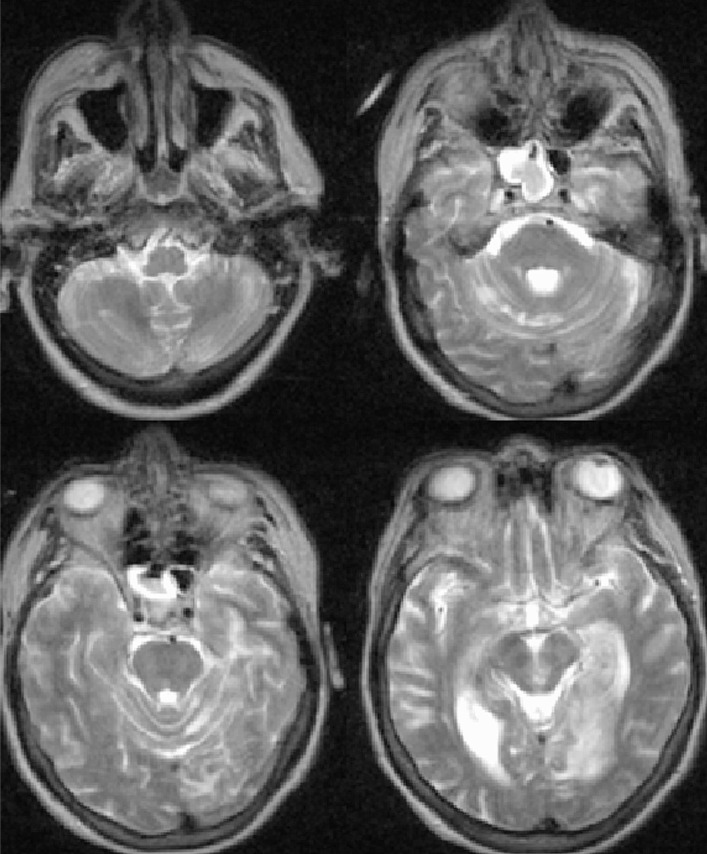
Figure 7.
Follow-up brain MR scan: left mesial temporo-occipital ischaemia and a smaller ipsilateral superior cerebellar ischaemic lesion.
Retrospective analysis of our cohort disclosed a complication rate of 0.1% for transient neurological complications and 0.05% for permanent deficits.
Groups 2 and 3
There were no major or minor adverse reactions to contrast medium.
Group 4
Follow-up of local complications was more difficult as onset of a small inguinal haematoma is not reported to us by the patient's referring ward as no local or systemic treatment is required.
No complication was reported by any of the 160 patients undergoing angiography in Day Hospital.
Discussion
Literature reports of neurological complications arising during diagnostic angiography vary from 0.4% to 12.2% for transient reversible neurological complications and from 0% to 5.4% for permanent deficits3,5,6,10,11,12,13,14,17,20,21.
A metanalysis by Cloft et Al in 1999 addressed three prospective studies reporting values between 0.9% and 2.3% for transient neurological complications and from 0.1% to 0.5% for permanent deficits.
The complication rates found in our study are lower than the average incidence reported in the literature but the reasons for this discrepancy are unknown. Possible factors influencing our low complication rate include:
1) Analysis of a more recent period than those of other studies.
2) A relatively young cohort average age 53,2 years with few cases of stenotic atheromatous carotid disease.
3) Angiography was performed by highly experienced staff with a strong commitment to training younger physicians. This point must be stressed: during this period four young neuroradiologists were trained, two of them now regularly performing interventional procedures. The "learning curve" of these persons was eliminated by the ongoing supervision by the older experienced neuroradiologist continuously following every procedure and intervening whenever needed.
4) Examination times are kept as short as possible in view of the link between duration of angiography and the risk of complications.
5) Special attention was paid to haemostasis at the end of the procedure. The femoral artery is always compressed manually for a count of ten minutes with absent dorsalis pedis artery pulse, more lightly with a dorsalis pedis artery pulse present for about 20 minutes. Patients are then instructed to check and compress the puncture point themselves. It is significant that no complications were encountered in any of the 160 patients examined in the Day Hospital. Lastly, patients are kept in the neuroradiology unit for at least an hour after the procedure before being returned to their referring wards.
6) The angiography procedure follows a standard technical protocol (use of guiding catheters, careful washing of catheters to avoid empty spaces forming, etc.).
7) The contrast agent offers maximum tolerability and is administered at the minimal dose required for acquisition of a valid diagnostic image.
References
- 1.American College of Radiology. ACR standard for Cerebral Angiography. 1995:97–99. [Google Scholar]
- 2.Anderson GB, Findlay JM, et al. Experience with computed tomographic angiography for the detection of intracranial aneurysms in the setting of acute subarachnoid haemorrhage. Neurosurgery. 1997;41:522–527. doi: 10.1097/00006123-199709000-00003. [DOI] [PubMed] [Google Scholar]
- 3.Baum S, Stein GN, Kuroda KK. Complications of "arteriography". Radiology. 1966;86:835–838. doi: 10.1148/86.5.835. [DOI] [PubMed] [Google Scholar]
- 4.Citron SJ, co-chair Wallace RC, co-chair, ASITN, ASNR, et al. Quality improvement guidelines for adult diagnostic neuroangiography: cooperative study between ASITN, ASNR and SIR. I Vasc Interv Radiol. 2003;14:S257–S262. [PubMed] [Google Scholar]
- 5.Cloft HJ, Kallmes DF, Dion JE. Devil's advocate: a second look at the second look angiogram for subarachnoid haemorrhage. Radiology. 1997;205:323–325. doi: 10.1148/radiology.205.2.9356610. [DOI] [PubMed] [Google Scholar]
- 6.Cloft HJ, Joseph GJ, Dion JE. Risk of cerebral angiography in patients with subarachnoid haemorrhage, cerebral aneurysm, and arteriovenous malformation a meta-analysis. Stroke. 1999;30:317–320. doi: 10.1161/01.str.30.2.317. [DOI] [PubMed] [Google Scholar]
- 7.De Santi F, Agati R, et al. Il sistema filmless Pacs-Ris del Servizio di Neuroradiologia dell'Ospedale Bellaria di Bologna, tre anni di esperienza. Rivista di Neuroradiologia. 2001;14:113. [Google Scholar]
- 8.Dion JE, Gates PC, et al. Clinical events following neuroangiography: a prospective study. Stroke. 1987;18:997–1004. doi: 10.1161/01.str.18.6.997. [DOI] [PubMed] [Google Scholar]
- 9.Earnest F, Forbes G, et al. Complications of cerebral angiography: prospective assessment of risk. Am J Roentgenol. 1984;142:247–253. doi: 10.2214/ajr.142.2.247. [DOI] [PubMed] [Google Scholar]
- 10.Hankey GJ, Warlow CP, Sellar RJ. Cerebral angiographic risk in mild cerebrovascular disease. Stroke. 1990;21:209–222. doi: 10.1161/01.str.21.2.209. [DOI] [PubMed] [Google Scholar]
- 11.Hankey JG, Warlow CP, Molyneux AJ. Complications of cerebral angiography for patients with mild carotid territory ischaemia being considered for carotid endarterectomy. J Neurol Neurosurg Psychiatry. 1990;53:542–548. doi: 10.1136/jnnp.53.7.542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Heiserman JE, Dean BL, et al. Neurologic complications of cerebral angiography.". Am J Neuroradiol. 1994;15:1408–1411. [PMC free article] [PubMed] [Google Scholar]
- 13.Kassell NF, Torner JC. Aneurysmal rebleeding: a preliminary report from the Cooperative Aneurysm Study. Neurosurgery. 1983;13:479–481. doi: 10.1227/00006123-198311000-00001. [DOI] [PubMed] [Google Scholar]
- 14.Kuhn J, Vehlen C, et al. Rupture of an internal carotid artery aneurysm during angiography with leakage ventricular drain. Neuroradiology. 2003;45:905–907. doi: 10.1007/s00234-003-1079-9. [DOI] [PubMed] [Google Scholar]
- 15.Le Roux PD, Dailey AT, et al. Emergent aneurysm clipping without angiography in the moribund patient with intracerebral haemorrhage: the use of infusion computed tomography scans. Neurosurgery. 1993;33:189–197. doi: 10.1227/00006123-199308000-00002. [DOI] [PubMed] [Google Scholar]
- 16.Leffers AM, Wagner A. Neurological complications of cerebral angiography: a retrospective study of complication rate and patient risk factors. Acta Radiologica. 2000;41:204. doi: 10.1080/028418500127345299. [DOI] [PubMed] [Google Scholar]
- 17.Louis TA. Findings for public health from meta-analysis. Ann Rev Public Health. 1985;6:1–20. doi: 10.1146/annurev.pu.06.050185.000245. [DOI] [PubMed] [Google Scholar]
- 18.Pollock BE, Kondziolka D, et al. Magnetic resonance imaging: an accurate method to evaluate arteriovenous malformations after stereotactic radiosurgery. J Neurosurg. 1996;85:1044–1049. doi: 10.3171/jns.1996.85.6.1044. [DOI] [PubMed] [Google Scholar]
- 19.Randoux B, Marro B, et al. Carotid artery stenosis: prospective comparison of CT, three-dimensional gadolinium-enhanced MR, and conventional angiography. Radiology. 2001;220:179–185. doi: 10.1148/radiology.220.1.r01jl35179. [DOI] [PubMed] [Google Scholar]
- 20.Saitoh H, Hayakawa K, et al. "Intracarotid blood pressure changes during contrast medium injection.". Am J Neuroradiol. 1996;17:51–54. [PMC free article] [PubMed] [Google Scholar]
- 21.Saitoh H, Hayakawa K, et al. Rerupture of cerebral aneurysms during angiography. Am J Neuroradiol. 1995;16:539–542. [PMC free article] [PubMed] [Google Scholar]
- 22.Schaller C, Schramm J. Arteriovenous malformations and magnetic resonance imaging. J Neurosurg. 1997;87:647. Comment. [PubMed] [Google Scholar]
- 23.Schuierer G, Huk WJ, Laub G. Magnetic resonance angiography of intracranial aneurysms: comparison with intra-arterial digital subtraction angiography. Neuroradiology. 1992;35:50–54. doi: 10.1007/BF00588279. [DOI] [PubMed] [Google Scholar]
- 24.Velthuis BK, Rinkel GJE, et al. Subarachnoid haemorrhage: aneurysm detection and preoperative evaluation with CT angiography. Radiology. 1998;208:423–430. doi: 10.1148/radiology.208.2.9680571. [DOI] [PubMed] [Google Scholar]
- 25.Waugh JR, Sacharias N. Arteriographic complications in the DSA era. Radiology. 1992;182:243–246. doi: 10.1148/radiology.182.1.1727290. [DOI] [PubMed] [Google Scholar]
- 26.Willinsky R, Taylor S M, et al. Neurologic complications of cerebral angiography: prospective analysis of 2899 procedures and review of the literature. Radiology 227 n. 2003;2:522–528. doi: 10.1148/radiol.2272012071. [DOI] [PubMed] [Google Scholar]
- 27.Yousem D, Trinh BC. Injection rates for neuroangiography: results of a survey. Am J Neuroradiol. 2001;22:1838–1840. [PMC free article] [PubMed] [Google Scholar]