Summary
Carotid-vertebral anastomoses are commonly detected as incidental findings. But sometimes these channels are important for the clinical condition of the patient. Here a case of right thalamo-capsular arteriovenous malformation is described where a persistent primitive hypoglossal artery was the only route for embolization of the arteriovenous malformation.
Key words: hypoglossal artery, carotid-vertebral anastomoses, arterio-venous malformation, embolization
Introduction
Carotid-vertebral anastomoses develop during fetal life between the internal carotid and basilar arterial systems for the supply of the posterior cranial circulation. The channels include trigeminal, hypoglossal, otic and pro-atlantal segmental arteries. With the development of the posterior communicating artery, these channels regress and disappear but may rarely persist into adult life. The persistent trigeminal artery is the most common anomaly among the four, followed by the hypoglossal artery1. These channels are detected as incidental findings but may be associated with aneurysms, tumors, subarachnoid haemorrhage and arterio-venous malformations1-5. We describe a case of right thalamo-capsular arteriovenous malformation, for which embolization was done through persistent primitive hypoglossal artery.
Case report
This 47-year-old male patient presented with history of sudden onset left upper and lower limb dense hemiplegia associated with loss of consciousness, left focal seizures and left hemisensory dulling. CT scan showed an arteriovenous malformation (AVM) involving the right thalamus and posterior limb of right internal capsule with evidence of haematoma in the same regions. He was managed conservatively after that acute episode. Later digital subtraction angiography showed right thalamic and internal capsular AVM fed by perforating arteries from the right middle cerebral, anterior cerebral and posterior cerebral arteries along with right anterior and posterior choroidal arteries (figure 2A,B).
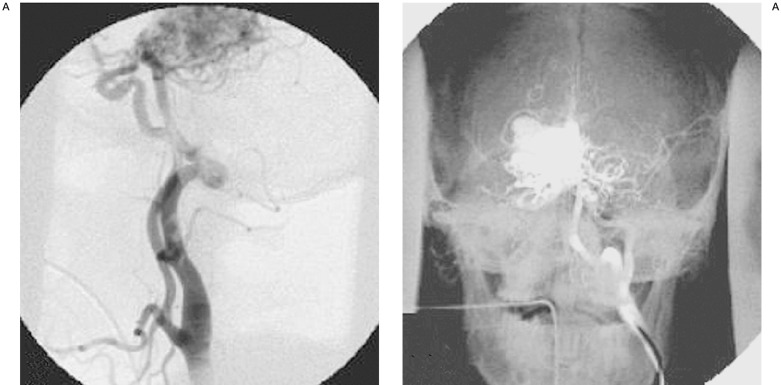
The AVM showed both superficial and deep venous drainage, but predominant drainage was through multiple superficial cortical veins due to significant stenosis of the straight sinus. The AVM nidus was compact, measured less than 3 cms in diameter without any intranidal aneurysm or venous ectasia. So it was in Spetzler Martin grade 3. On left common carotid (CCA) injection basilar artery (BA) was filling through a large anastomotic vessel between internal carotid artery (ICA) and intradural vertebral artery. ICA distal to this showed smaller in caliber and poor forward flow compared to the right side. The anastomotic vessel arose from the C2 vertebral body level and ascends posterosuperiorly and takes a dorsal loop at the level of basion (within the hypoglossal canal) then joins with the proximal part of the BA (figure 1).
Figure 1.
(A) Left common carotid lateral angiogram shows the persistent hypoglossal artery (PHA) arising from internal carotid artery (ICA) and entering through the hypoglossal canal and joining the proximal basilar artery. (B) Anteroposterior view of left ICA with bony landmark show the course of PHA posteromedial to ICA and filling of arteriovenous malformation (AVM).
CT angiogram showed that the anastomotic artery is entering through the enlarged left hypoglossal canal (figure 3). Both vertebral arteries at V4 segment and bilateral posterior communicating arteries were hypoplastic (figure 2C,D). Direct arteriovenous fistulae from two posterior cerebral artery perforating feeders were embolized using 50% Nbutyl cyanoacrylate. Since rest of the feeders too small for selective catheterization, it was decided to send him for steriotactic radiotherapy for further management.
Figure 2.
(A) Left PHA injection shows the connection to proximal basilar artery. (B) Left ICA injection lateral view shows the filling of AVM via perforators. Note the non-opacification of posterior communicating artery. (C,D) Right and left vertebral artery injections show the hypoplastic distal vertebral arteries.
Figure 3.
A) Plain CT of base of skull shows the enlarged left hypoglossal canal. B,C,D) Contrast enhanced CT scan shows the PHA coursing posteromedial to ICA and entering through the hypoglossal canal to join the basilar artery.
Discussion
The persistence of a primitive hypoglossal artery is a rare anomaly of Carotid-vertebral anastomoses. Reported frequency of persistent hypoglossal artery (PHA) is 0.02-0.1% which is lower than that of persistent trigeminal artery (0.1-0.6%), the most commonly found carotidvertebral anastomoses 6. At 4 mm embryo stage of development the internal carotid arteries extend from the paired dorsal aorta and anastomoses at three major sites with paired neural arteries in the hindbrain. These sites of communication are named for their relation to the trigeminal ganglion, otic vesicle and rootlets of the hypoglossal nerve forming the trigeminal artery, otic artery and hypoglossal artery. Otic is the first to disappear followed by the hypoglossal and lastly the trigeminal artery1. At the same stage there are seven transversely oriented arteries in the cervical region (cervical inter segmental arteries), the first of these has been designated as proatlantal intersegmental artery.
PHA originates from the internal carotid artery as a large extra cranial branch at C1 C3 level and enters the skull through the anterior condyloid foramen (hypoglossal canal) supplying the basilar artery7.
Initially the absence of posterior communicating artery was considered as an additional criterion for the presence of PHA. However Agnoli8 in a review of 80 cases, reported hypoplastic or angiographically absent posterior communicating arteries on both sides are present in 78% of cases and hypoplastic vertebral arteries in 79% of cases.
The characteristics which constitute the criteria for identification of the PHA are described as follows: a) the PHA arises from the cervical part of the internal carotid artery at the C1-C2 level, b) together with the XIIth cranial nerve enters the posterior cranial fossa via the hypoglossal canal, c) the basilar trunk arises from the branch of PHA and d) the ipsilateral vertebral artery may be hypoplastic9. In our case it exactly followed the typical course of a PHA. The ipsilateral ICA was smaller and bilateral vertebral vertebral arteries were hypoplastic distally.
Although conventional angiography has been considered as the reference standard for the detection and evaluation of vascular structures, there are diagnostic alternatives with different advantages. CT angiography is a noninvasive examination, which has the advantage of multiplanar demonstration of the PHA by the use of 3D reconstruction techniques. Therefore, CT angiography provides excellent anatomic localization of PHA in all its parts and depicts clearly its entrance to the hypoglossal canal6. In our case CT angiography showed the course of the artery through hypoglossal canal, not via foramen magnum, which is typically followed by proatlantal arteries.
MR imaging and MR angiography in particular is able to sufficiently demonstrate the PHA, without any contrast medium. MR angiography, by using a maximum-intensity-projection (MIP) program is able to show the complete carotid-vertebral anastomoses without superimposition of other vessels 6,10,11.
Both CT and MR angiography are diagnostic alternatives, which have already been reported in the literature in cases of PHA detection and evaluation of certain pathologic conditions. Thus, stenosis due to atherosclerotic plaque or aneurysm formation can be depicted by 3D CT or MR angiography 12,13.
Since the presence of PHA may be completely asymptomatic, it may appear as an incidental finding in a cerebral angiogram performed for another diagnostic purpose. However, its identification is clinically important for patient management, as for planning carotid endarterectomy or skull base surgery14. The existence of PHA has also been related with increased incidence of intracranial vascular abnormalities and atherosclerotic disease 12,13,15-21. The later may present as a plaque extending from the distal carotid artery into the internal carotid artery (ICA) or as an isolated stenosis near the PHA takeoff. The group of persistent primitive arteries, in which PHA belongs to, is implicated in cases of moyamoya and quasimoyamoya disease as well 22,23. Although some reports suggest higher frequency of intracranial arteriovenous malformations and aneurysms in the presence of a PHA, no statistically significant difference has been found6. PHA may provide pathway for cerebral embolism.
In contrast to PHA, the pro atlantal inter segmental artery curves sharply dorsally to course in the occipitoatlantal space like vertebral artery and then passes through the foramen magnum. Hypoglossal artery has a more vertical course than the proatlantal artery and lacks the horizontal sweep of vertebral and proatlantal artery24. This carotid-vertebral anastomosis is extremely rare. There were only six reported angiographic demonstrations until 197625.
This case was unique in the sense that the access to the AVM was possible only through the PHA as the V4 segment of both vertebral arteries and posterior communicating arteries were hypoplastic. To the best of our knowledge, there is no report of AVM embolization through the PHA.
References
- 1.Lie TA. Congenital anomalies of the carotid arteries. Amsterdam: Excerpta Medica Foundation; 1968. pp. 52–93. [Google Scholar]
- 2.Fantini GA, Reilly LM, Stoney RJ. Persistent hypoglossal artery: diagnostic and therapeutic consideration concerning carotid endarterectomy. J Vasc Surg. 1994;20:995–999. doi: 10.1016/0741-5214(94)90238-0. [DOI] [PubMed] [Google Scholar]
- 3.Hackett ER, Wilson CB. Congenital external carotid vertebral anastomosis: a case repor. Am J Radiol 1968; 1968;104:86–89. doi: 10.2214/ajr.104.1.86. [DOI] [PubMed] [Google Scholar]
- 4.Shapiro R. Enlargement of the hypoglossal canal in the presence of a persistent hypoglossal artery. Radiology. 1979;133:395–396. doi: 10.1148/133.2.395. [DOI] [PubMed] [Google Scholar]
- 5.Matsumara N, Nojiri K, Yumoto V. Persistent primitive hypoglossal artery associated with Arnold-Chiari Type I malformation. Surg Neurol. 1985;24:241–244. doi: 10.1016/0090-3019(85)90029-1. [DOI] [PubMed] [Google Scholar]
- 6.Oelerich M, Schuierer G. Primitive hypoglossal artery: demonstration with digital subtraction-, MR and CT angiography. Euro Radiol. 1997;7:1492–1494. doi: 10.1007/s003300050322. [DOI] [PubMed] [Google Scholar]
- 7.Brismar J. Persistent hypoglossal artery, diagnostic criteria. Report of a case. Acta Radiol. 1976;17:160–166. doi: 10.1177/028418517601700204. [DOI] [PubMed] [Google Scholar]
- 8.Agnoli Al. Vascular anomalies and subarachnoid haemorrhage associated with persisting embryonic vessels. Acta Neurochir. 1982;60:183–199. doi: 10.1007/BF01406306. [DOI] [PubMed] [Google Scholar]
- 9.Lasjaunias P, Doyon D. The ascending pharyngeal artery and the blood supply of the lower cranial nerves. J Neuroradiol. 1978;5:287–301. [PubMed] [Google Scholar]
- 10.Chaljub G, Guinto FCJ, Crow WN. Persistent Hypoglossal Artery: MRI and MRA findings. JCAT. 1995;19:668–671. doi: 10.1097/00004728-199507000-00037. [DOI] [PubMed] [Google Scholar]
- 11.Hahnel S, Hartmann M, et al. Persistent hypoglossal artery: MRI, MRA and digital subtraction angiography. Neuroradiol. 2001;43:767–769. doi: 10.1007/s002340100566. [DOI] [PubMed] [Google Scholar]
- 12.Kanai H, Nagai H, et al. A large aneurysm of the persistent primitive hypoglossal artery. Neurosurg. 1992;30:794–797. [PubMed] [Google Scholar]
- 13.Wagner AL. Isolated stenosis of a persistent hypoglossal artery visualized at 3D CT angiography. Am J Neurorad. 2001;22:1613–1614. [PMC free article] [PubMed] [Google Scholar]
- 14.Megyesi JF, Findlay JM, Sherlock RA. Carotid endarterectomy in the presence of a persistent hypoglossal artery: case report. Neurosurgery. 1997;41:669–672. doi: 10.1097/00006123-199709000-00032. [DOI] [PubMed] [Google Scholar]
- 15.Katoh M, Kamiyama H, et al. Severe stenosis of internal carotid artery presenting as loss of consciousness due to presence of primitive hypoglossal artery; case report. Surg Neurol. 1999;51:310–312. doi: 10.1016/s0090-3019(98)00053-6. [DOI] [PubMed] [Google Scholar]
- 16.Huynh-Le P, Matsushima T, et al. Persistent primitive hypoglossal artery associated with proximal posterior inferior cerebellar artery aneurysm. Surg Neurol. 2004;62:546–551. doi: 10.1016/j.surneu.2004.03.018. [DOI] [PubMed] [Google Scholar]
- 17.Yokota N, Yokoyama T, Ryu H. Aneurysm of persistent primitive hypoglossal artery. Br J Neurosurg. 1999;13:608–610. doi: 10.1080/02688699943178. [DOI] [PubMed] [Google Scholar]
- 18.Al-Memar A, Thrush D. Unilateral hypoglossal nerve palsy due to aneurysm of the stump of persistent hypoglossal artery. J Neurol Neurosurg Psychiatry. 1998;64:405. doi: 10.1136/jnnp.64.3.405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kobayashi H, Munemoto S, et al. Association of persistent hypoglossal artery, multiple intracranial aneurysms, and polycystic disease. Surg Neurol. 1984;21:258–260. doi: 10.1016/0090-3019(84)90198-8. [DOI] [PubMed] [Google Scholar]
- 20.Shibata Y, Hyodo A, et al. Large arteriovenous malformation associated with persistent primitive hypoglossal artery-case report. Neurol Med Chir. 1991;31:804–808. doi: 10.2176/nmc.31.804. [DOI] [PubMed] [Google Scholar]
- 21.Nishida C, Ashikaga R, et al. Persistent hypoglossal artery associated with arteriovenous malformation: a case report. Eur J Radiol. 2000;33:59–62. doi: 10.1016/s0720-048x(99)00058-3. [DOI] [PubMed] [Google Scholar]
- 22.Komiyama M, Nakajima H, et al. High incidence of persistent primitive arteries in moyamoya and quasimoyamoya disease. Neurol Med Chir. 1999;39:416–420. doi: 10.2176/nmc.39.416. [DOI] [PubMed] [Google Scholar]
- 23.Katayama W, Eromoto T, et al. Moyamaya disease associated with persistent primitive hypoglossal artery: a case report. Ped Neurosurg. 2001;35:262–265. doi: 10.1159/000050433. [DOI] [PubMed] [Google Scholar]
- 24.Bashi YZ, Uysal H, et al. Persistent primitive proatlantal intersegmental artery (proatlantal artery I) results in 'top of basilar syndrome'. Stroke. 1993;24:2114–2117. doi: 10.1161/01.str.24.12.2114. [DOI] [PubMed] [Google Scholar]
- 25.Anderson RA, Sondheimer FK. Rare carotid-vertebrobasilar anastomoses with notes on differentiation between proatlantal and hypoglossal arteries. Neuroradiology. 1976;11:113–118. doi: 10.1007/BF00337545. [DOI] [PubMed] [Google Scholar]