Abstract
Background
The diffusion of antibiotics through the outer membrane is primarily affected by the porin super family, changes contribute to antibiotic resistance. Recently we demonstrated that the CpxAR two-component signaling system alters the expression of an uncharacterized porin OmpCKP, to mediate antimicrobial resistance in K. pneumoniae.
Principal Findings
In this study, functional characterization of the putative porin OmpCKP (denoted kpnO) with respect to antimicrobial susceptibility and virulence was evaluated by generating an isogenic mutant, ΔkpnO in a clinical isolate of K. pneumoniae. Estimation of uronic acid content confirmed that ΔkpnO produced ∼2.0 fold lesser capsular polysaccharide than the wild-type. The ΔkpnO displayed higher sensitivity to hyper osmotic and bile conditions. Disruption of kpnO increased the susceptibility of K. pneumoniae to oxidative and nitrostative stress by ∼1.6 fold and >7 fold respectively. The loss of the Klebsiella porin led to an increase in the minimum inhibitory concentration of tetracycline (3-fold), nalidixic acid (4-fold), tobramycin (4-fold), streptomycin (10-fold), and spectinomycin (10-fold), which could be restored following complementation. The single deletion of kpnO reduced the survival of the pathogen by 50% when exposed to disinfectants. In Caenorhabditis elegans model, the kpnO mutant exhibited significantly (P<0.01) lower virulence. To dissect the role of PhoBR signaling system in regulating the expression of the kpnO, a phoB KP isogenic mutant was constructed. The phoB KP mutant exhibited impaired gastrointestinal stress response and decreased antimicrobial susceptibility. The mRNA levels of kpnO were found to be 4-fold less in phoB KP mutant compared to wild type. A regulatory role of PhoBKP for the expression of kpnO was further supported by the specific binding of PhoBKP to the putative promoter of kpnO.
Conclusions and Significance
Loss of PhoBR regulated porin KpnO resulted in increased antimicrobial resistance, increased susceptibility to gastrointestinal stress, and reduced virulence in K. pneumoniae NTUH-K2044.
Introduction
The cell envelope of Gram-negative bacteria consists of three principal layers: the outer membrane (OM), the peptidoglycan cell wall, and the inner membrane [1]. The OM is punctuated by a family of proteins, called outer membrane proteins (OMP) or porins [2], [3]. In E. coli and related gamma-proteobacteria, the major OMPs are OmpF (∼35 kDa), OmpC (∼36 kDa) and PhoE, and they differ in their solute selectivity, porin activity and gene expression in response to many environmental factors, such as osmotic pressure, temperature and pH [4]. The OM of Gram-negative bacteria plays a significant role in a variety of functions; it serves as a diffusion barrier to extracellular solutes and interacts with the bacterial environment. Influx is largely controlled by porins that are represented in large amounts in the OM. They form water-filled open channels that span the OM and allow the passive penetration of small hydrophilic molecules (>600 Da), such as iron, nutrients, and clinically significant antibiotics, such as β-lactams, aminoglycosides, carbapenems and fluoroquinolones [5]. Porins also serve as receptors for bacteriophages and bacteriocins and, in conjunction with peptidoglycan and LPS, play a significant role in maintaining the integrity of bacterial cells. As the major components of the OM, pore-forming proteins play a role in bacterial pathogenesis, such as adherence, invasion, and serum resistance [6].
Alterations in OM permeability, including modification of porin expression, have emerged as the major multidrug resistant (MDR) mechanism in key Gram negative clinical pathogens, such as Escherichia coli, Salmonella spp., Enterobacter spp., Campylobacter spp., Acinetobacter baumannii, and Pseudomonas spp., including the notoriously extreme drug resistant Klebsiella pneumoniae [7], [8]. K. pneumoniae are opportunistic pathogens and can give rise to severe diseases such as septicemia, pneumonia, urinary tract infections, and soft tissue infections [9]. The hospitalized, immunocompromised patient with underlying diseases is the main target of these bacteria. Thus, Klebsiella infections may serve as a paradigm of hospital-acquired infections [10]. Their incidence of 5 to 7% of all hospital-acquired infections ranks them among the most important nosocomial pathogen. Klebsiella is well known to most clinicians as a cause of community-acquired bacterial pneumonia occurring particularly in chronic alcoholics and showing characteristic radiographic abnormalities [11]. Carbapenems and cephalosporins are the most common drugs of treatment for K. pneumoniae infection however prevalence of MDR strains have led to failures of drug therapy [12].
Similar to many enterobacterial pathogens, OmpK36 (OmpC homolog) and OmpK35 (OmpF homolog) are the two non-specific porins produced by K. pneumoniae through which nutrients and other hydrophilic molecules, such as carbapenems and cephalosporins, diffuse into the bacteria. Epidemiological studies indicate that porin loss in K. pneumoniae strains that produce ESBLs (Extended spectrum β-lactamases) display resistance to cefoxitin, oxyimino cephalosporins, monobactams, and fluoroquinolones [13]. A few studies have shown that strains producing CTX-M or AmpC type β-lactamases together with porin loss exhibit decreased susceptibility to carbapenems [14].
K. pneumoniae might express additional porins, such as PhoE, LamB, and OmpK37, which may be pivotal for normal cellular function in the absence of major porins OmpK36/35 [15]. In a previous study it was shown that absence of major porins OmpK35/K36 allows K. pneumoniae CSUB10S clinical isolate to exhibit high levels of resistance to various classes of antibiotics such as cefepime (8-fold), and cefotaxime (8-fold) and LamB deficiency in such OmpK35/K36 deleted background further increased the MICs of cefepime (16-fold) and cefotaxime (16-fold) respectively [16]. In another study, increased carbapenem resistance in OmpK36/K35 deficient clinical isolates has been correlated with down regulation of phoE in K. pneumoniae [17]. The alternative porin OmpK37 expressed at very low levels under standard laboratory conditions is known to have a minimal role in antimicrobial resistance [18]. Garcia-Sureda et al has recently reported that expression of the oligogalacturonate-specific porin OmpK26 compensated for the absence of OmpK35/36 in carbapenem resistant K. pneumoniae [19].
The K. pneumoniae NTUH-K2044 is hyper virulent clinical isolate with a thick capsule and has been isolated from a Taiwanese liver abscess patient, with magA and rmpA genes in its genome [20]. All these factors make this strain very suitable as a model organism for genomic studies. As for most bacterial pathogens, K. pneumoniae virulence is multifactorial, and there are many virulence factors that contribute to different disease syndromes. The success of this important pathogenic serotype in the varied ecological niches it can occupy depends on its ability to respond to the environment by differential regulation of its many virulence factors. Therefore understanding the biology of this human pathogen from the highly virulent serotype is critical to combat K. pneumoniae illness.
Previously we demonstrated that CpxAR two-component signaling system (TCS) alters the expression of a hypothetical porin (OmpK36 homolog) to mediate antimicrobial resistance in K. pneumoniae [21]. The current study was initiated to unravel the functions of the uncharacterized porin OmpCKP (denoted kpnO) with respect to bacterial physiology in general and antimicrobial susceptibility in particular in K. pneumoniae NTUH-K2044 for the first time. In silico analysis revealed PhoB binding sites in the kpnO regulatory region, therefore, a phoB null mutant was constructed to evaluate regulation of the porin by the PhoBR TCS in K. pneumoniae.
Results
Bioinformatic Analysis of KpnO
The nucleotide sequence deduced from 1098 bp DNA fragment obtained from K. pneumoniae NTUH-K2044 shared >80% identity with the OmpC porins from other Gram negative pathogens [20]. The protein sequence of KpnO exhibits the following identities (identities in brackets) with OmpC from other Klebsiella strains such as K. pneumoniae 342 (Accession no: NC_011283.1) (96%), K. pneumoniae MGH78578 (Accession no: NC_009648) (95%), K. pneumoniae HS11286 (95%) and other bacteria such as Enterobacter aerogenes (89%), E. coli (83%), Citrobacter youngae (83%), and Shigella dysenteriae (81%) respectively. Regulatory elements that have been defined for E. coli ompC, could be found upstream to the start codon of kpnO including Fnr (230–243 bp), OxyR (262–307 bp), OmpR (358–367 bp) binding sites, as analysed by virtual footprint promoter analysis www.prodoric.tu-bs.de.
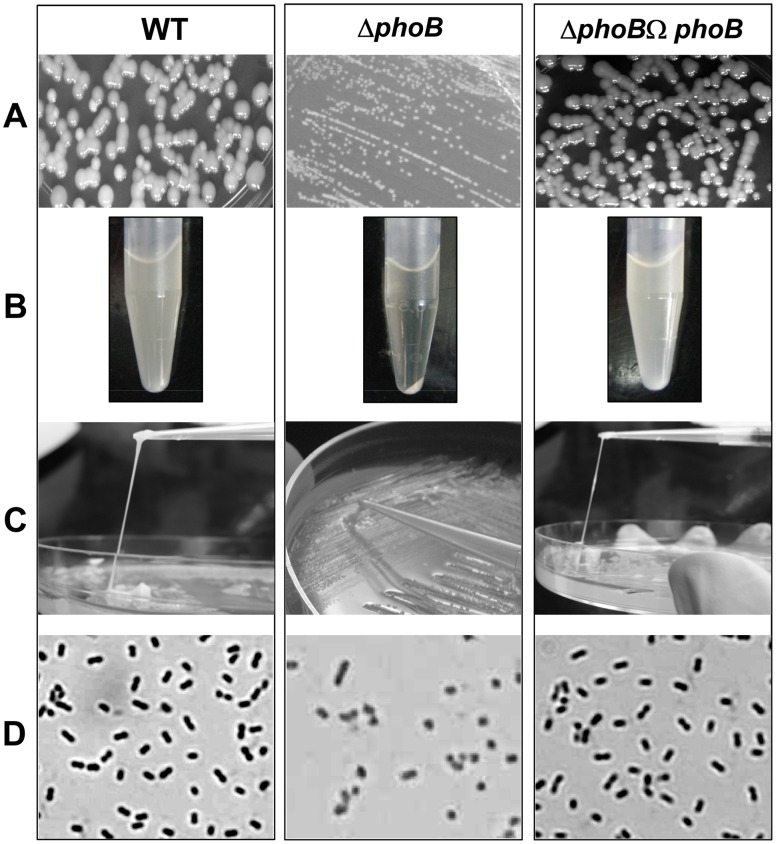
Deletion of kpnO Decreases Capsular Polysaccharide Production
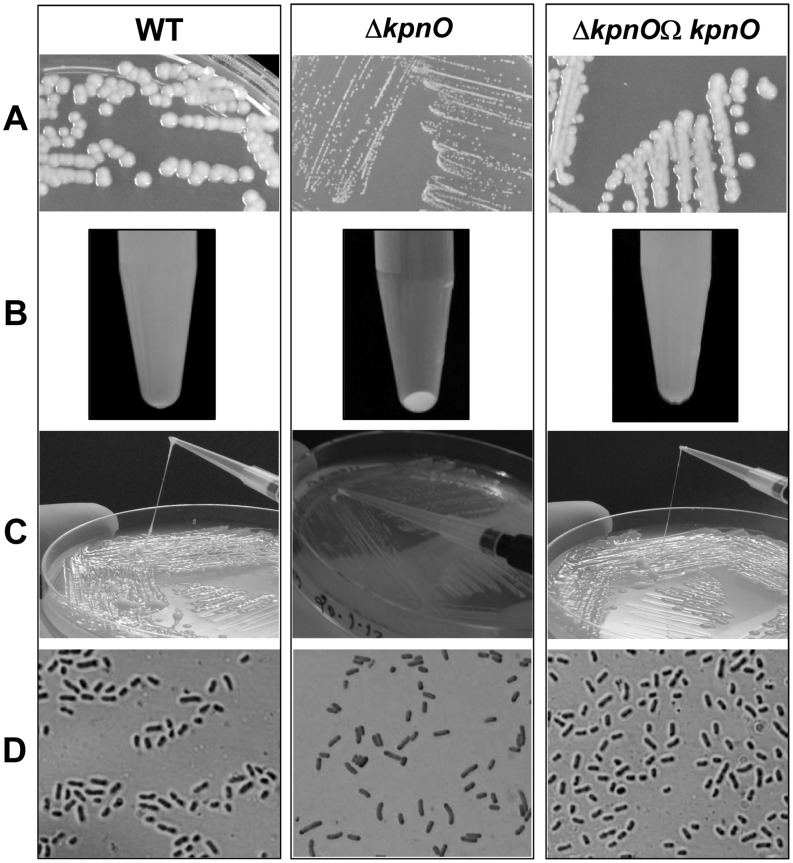
To determine the biological role of kpnO, a kpnO mutant was created by conjugation in the wild-type K. pneumoniae NTUH-K2044. We used insertion-duplication mutagenesis to interrupt kpnO, required for the synthesis of a functional porin. PCR followed by DNA sequencing was done to confirm the disruption of the gene in K. pneumoniae. RT-PCR analysis confirmed that mutations abolished the transcription of kpnO (data not shown). The kpnO mutant had a different colony morphology when compared to the wild type. The wild type (WT) strain produced bigger (3.0±0.5 mm) and heavily mucoid colonies while kpnO mutant (ΔkpnO) colonies were smaller (0.75±0.05 mm) and non-mucoid, indicating a direct decrease in capsular polysaccharides (CPS) production (Figure 1–A). To determine the role of kpnO in CPS production, the hypermucoviscosity string test was performed; this test assesses the formation of a viscous string. The length of the strings for WT and ΔkpnO were 5.0±0.5 cm and 0.51±0.02 cm respectively (Figure 1–B). The precipitation test was carried out on 12 h grown culture in LB broth at 37°C. The WT did not form a dense pellet after centrifugation at 4000rpm for 3 mins while the ΔkpnO formed compact pellet (Figure 1–C). Visualization of cultures using 20% CuSO4 as per Anthony's capsule staining methodology revealed distinct difference in the exopolysaccharide production around NTUH-K2044 and ΔkpnO (Figure 1–D), and complementation restored their morphology. Quantification of uronic acid content reconfirmed the same observation (Table 1). These data suggest that KpnO contributes significantly towards capsule production of K. pneumoniae NTUH-K2044.
Figure 1. Phenotypic characterization of kpnO mutant.
A) The kpnO mutant (ΔkpnO) had different colony morphology with smaller (0.75±0.05 mm on average) and less regular colonies than the wild-type (WT) (3.0±0.5 mm on average). B) The hypermucoviscosity string test was performed by measuring the formation of a viscous string stretched between the bacterial colony and the inoculation loop. The average lengths of WT, ΔkpnO were (5.0±0.5 cm) and (0.51±0.02 cm) respectively. C) The precipitation test was carried out on 12 h grown strains in LB broth at 37°C, and each pellet was evaluated after centrifugation at 4000rpm for 3 min. The WT and ΔkpnO showed profound difference in the compactness of the pellet. D) Cells were grown to late log phase in shaking culture and stained with crystal violet followed by treatment with 20% copper sulphate solution. The WT and ΔkpnO were visualized in Olympus microscope work station.
Table 1. Determination of capsular polysaccharides.
| Strain | Glucouronic acid content (µg/109 CFU)a | Mucoviscosityb |
| WT | 18.14±1.09 | +++ |
| ΔkpnO | 7.31±1.34 | – |
| ΔkpnO ΩkpnO | 15.07±1.26 | +++ |
| ΔphoB KP | 9.86±2.01 | – |
| ΔphoB KP ΩphoB KP | 17.24±0.98 | +++ |
Values are the averages of triplicate samples represented by mean ± standard deviation.
Confirmed by string test.
KpnO Contributes to Growth and Gastrointestinal Stress Tolerance in K. pneumoniae
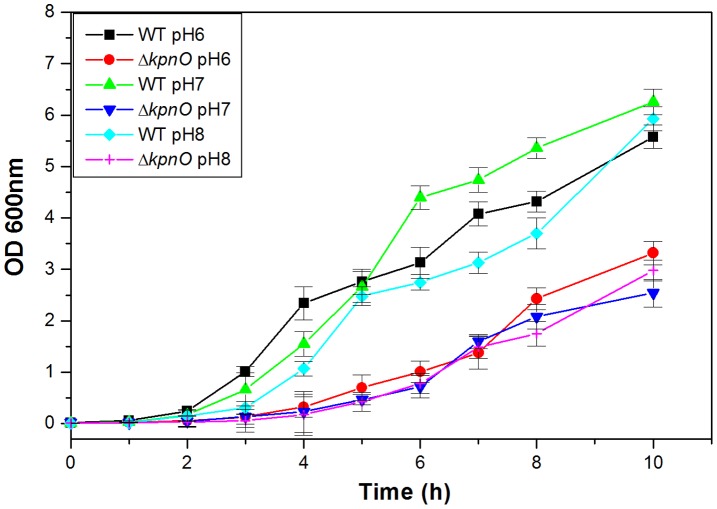
To decipher the involvement of KpnO in K. pneumoniae growth under conditions of different pH, the growth kinetics of ΔkpnO was compared with the wild type strain. Experimentally the growth characteristics of WT and ΔkpnO were determined over a period of ∼10 h in LB medium with different pH (3.0, 6.0, 7.0, 8.0 and 12.0) and subsequent data analysis revealed unique patterns. At pH 6.0, kpnO mutant exhibited reduced growth (>3.0 fold (±0.42) compared to the wild type after 6 h [WT/ΔkpnO mutant, P = 0.002]. The apparent density of ΔkpnO at pH 7.0 was 2.2 fold (±0.35) lower compared to wild-type after 10 h [WT/ΔkpnO mutant, P = 0.012]. At pH 8.0 ΔkpnO exhibited stunted growth (∼6 fold) compared to WT after 4 h and displayed a 2.0 fold density difference (Figure 2) [WT/ΔkpnO mutant, P = 0.004]. The other tested conditions of pH 3.0 and 12.0 were toxic to both the cultures. These results demonstrate that kpnO influences growth of K. pneumoniae under different pH conditions.
Figure 2. Growth kinetics.
Growth kinetics of WT, and ΔkpnO was assessed in LB medium pH 6.0, 7.0 and pH 8.0.
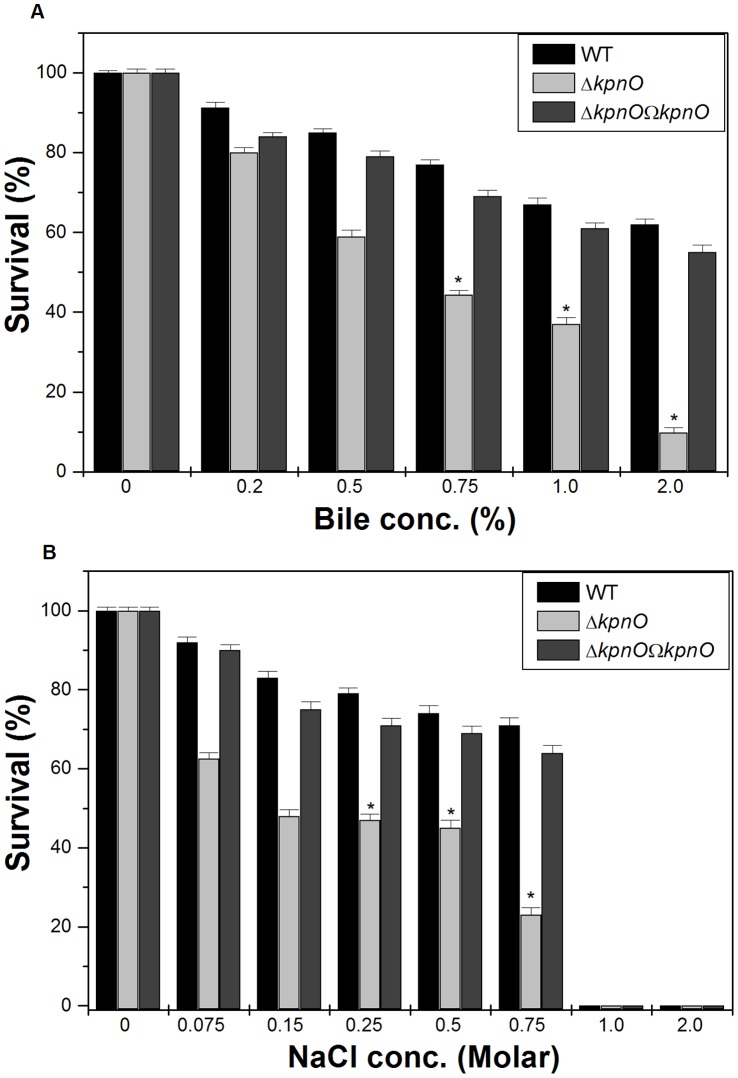
To determine the role of kpnO under conditions relevant to intestinal colonization, WT and ΔkpnO underwent specific gastrointestinal stress associated with bile and osmotic challenges. In the bile resistance assay, WT and ΔkpnO were exposed to different concentrations of bile (physiological concentration is 0.2% to 2%, [22]). The ability of WT to grow in the presence of 0.5% bile was 1.4 fold (±0.079), 0.75% bile was 1.7 fold (±0.017), 1% bile was 1.8 fold (±0.024) and 2% was 6.3 fold (±0.05) higher when compared to ΔkpnO, while transcomplemented ΔkpnOΩkpnO strain restored the ability to tolerate bile stress (Figure 3–A) [WT/ΔkpnO, P = 0.018; WT/transcomplemented, P = 0.004]. The ability of WT to grow in the presence of NaCl (physiological concentration being 150 mM, [23]) at 0.25 M was 1.7 fold (±0.014), 0.5 M was 1.6 fold (±0.055), and 0.75 M was 3-fold (±0.44), higher when compared to ΔkpnO regardless of the inoculum size (Figure 3–B) [WT/ΔkpnO mutant, P = 0.014; WT/transcomplemented, P = 0.022]. To deduce the role of kpnO in temperature tolerance, we performed the heat shock assay. The temperature dependent assay showed that the kpnO mutant displayed 10% reduced survival compared to the wild type at 60°C (data not shown), thereby demonstrating the role of kpnO during temperature stress. [WT/ΔkpnO mutant, P = 0.42]. Overall results described in this section indicate that kpnO influences the response towards bile, osmotic and heat shock stress in K. pneumoniae NTUH-K2044.
Figure 3. Bile and Osmotic challenge assays.
A) Stress sensitivity of the WT wild-type strain, the kpnO mutant. The percentage of resistance to bile (0.2%, 0.5%, 0.75%, 1.0%, and 2.0%) was calculated by comparison to the numbers of viable cells in LB medium alone. B) The percentage of resistance to different concentration of NaCl stress (0.075 M, 0.15 M, 0.25 M, 0.5 M, 0.75 M, 1.0 M and 2.0 M) for WT and ΔkpnO was calculated by comparison to the numbers of viable cells in control.
Role of KpnO in Modulating Oxidative and Nitrostative Stress Response
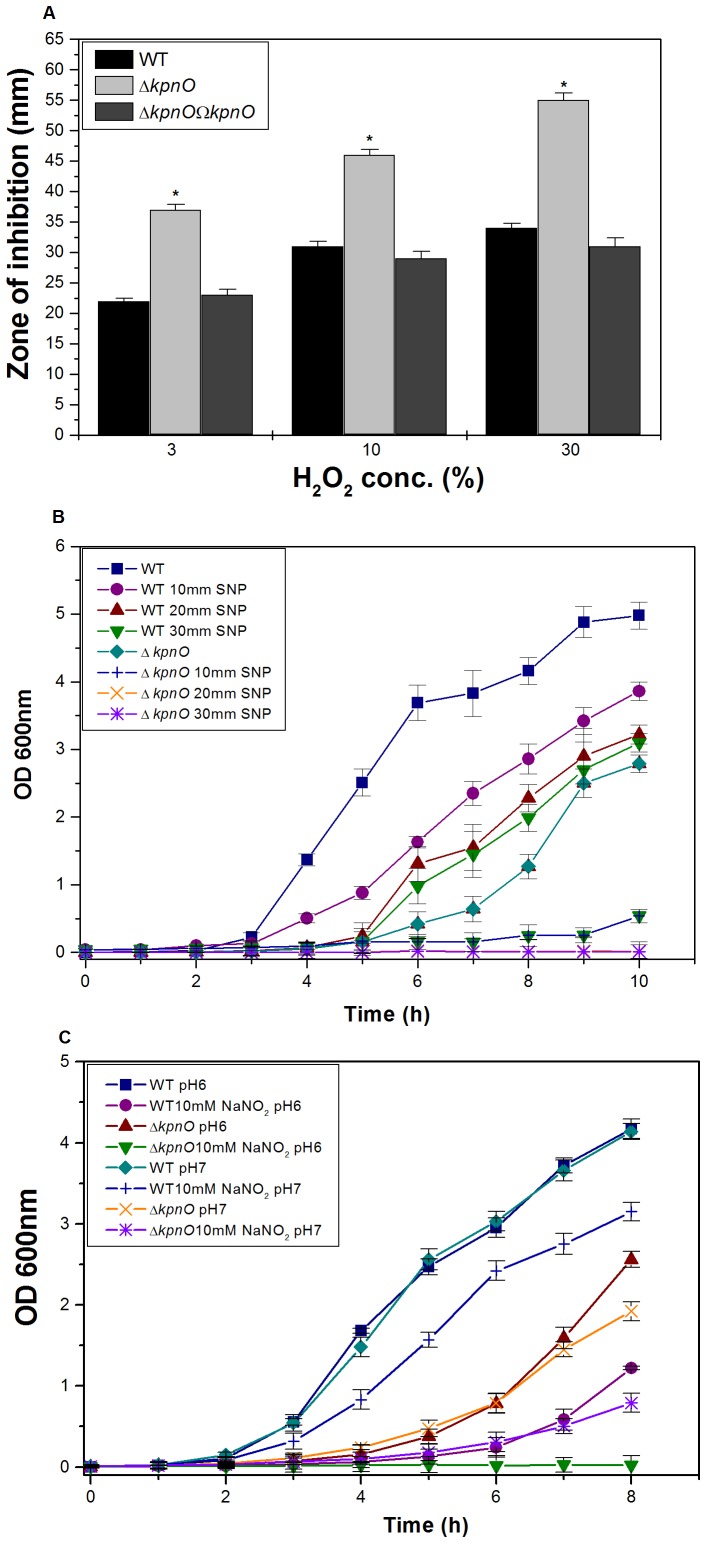
To deduce the role of kpnO in oxidative stress, we performed the hydrogen peroxide challenge assays. Oxidative disc assay showed that kpnO mutant exhibited 1.6 fold greater sensitivity to 30% H2O2 (inhibition zone = 55±2.0 mm) than the wild-type (inhibition zone = 34±0.0 mm) (Figure 4–A) [WT/ΔkpnO mutant, P = 0.013; WT/transcomplemented, P = 0.38]. The sensitivity of stationary-phase cultures to oxidative stress was tested by exposing them to a range of H2O2 concentrations for 1 h. Only 47% of the ΔkpnO cells survived upon treating with 0.07894 mM hydrogen peroxide in comparison to the 95% survival observed in wild-type cells (Figure S1).
Figure 4. Oxidative and nitrostative challenge assays.
A) Oxidative stress response of kpnO mutant. The ability of WT, ΔkpnO to combat different levels of hydrogen peroxide stress (3%, 10% and 30%) was measured by disc diffusion assay. The kpnO mutant displayed greater sensitivity to 30% H2O2 (inhibition zone = 55±2.0 mm) than the wild-type (inhibition zone = 34±0.0 mm). The data is the means of measurements made in triplicate and performed three times. *, Significant difference (P<0.05, Student t test). B) Effect of SNP at 10 mM, 20 mM and 30 mM concentration on growth of WT and ΔkpnO. Growth kinetics of ΔkpnO cells were ∼7 fold lower than the WT in the presence of 10 mM SNP, ΔkpnO exhibited ∼100 fold stunted growth at 20 mM and 30 mM SNP. C) Growth pattern of WT, ΔkpnO in the presence of sodium nitrite. In the presence of 10 mM NO donor, growth kinetics of ΔkpnO cells was ∼4.0 fold and ∼64.0 fold lower as compared to WT at pH 7.0 and pH 6.0 respectively.
To test whether the presence of K. pneumoniae KpnO provides any protection against NO donor and nitrostative stress, we compared the growth profiles of WT and ΔkpnO in the presence of different concentrations of the NO donor sodium nitroprusside (SNP). Growth kinetics of ΔkpnO cells were ∼7 fold lower than the WT in the presence of 10 mM SNP [WT/ΔkpnO mutant, P = 0.01], growth was ∼100 fold lower at 20 mM [WT/ΔkpnO mutant, P = 0.02] and 30 mM SNP [WT/ΔkpnO mutant, P = 0.02] respectively (Figure 4–B). To further evaluate the function of K. pneumoniae KpnO in conferring susceptibility to other reactive nitrogen species, we tested tolerance of ΔkpnO towards acidified sodium nitrite. Protonated nitrite quickly degrades to generate numerous species of nitrogen oxides, for example nitric oxide [24]. The growth kinetics of ΔkpnO in the presence of 10 mM NaNO2 at pH 7.0 was ∼4.0 fold lower compared to WT [WT/ΔkpnO mutant, P = 0.017], whereas in the presence of acidified LB the growth was >64 fold lower in the mutant [WT/ΔkpnO mutant, P = 0.115] (Figure 4–C). The growth kinetics of ΔkpnO in the presence of 30 mM NaNO2 at pH 7.0 was ∼7 fold lower compared to WT [WT/ΔkpnO mutant, P = 0.048], while presence of 30 mM NaNO2 in acidified LB was toxic to both the strains [WT/ΔkpnO mutant, P = 0.026] (Figure S2). Results clearly indicate the role of kpnO in affecting oxidative and nitrostative stress response in K. pneumoniae NTUH-K2044.
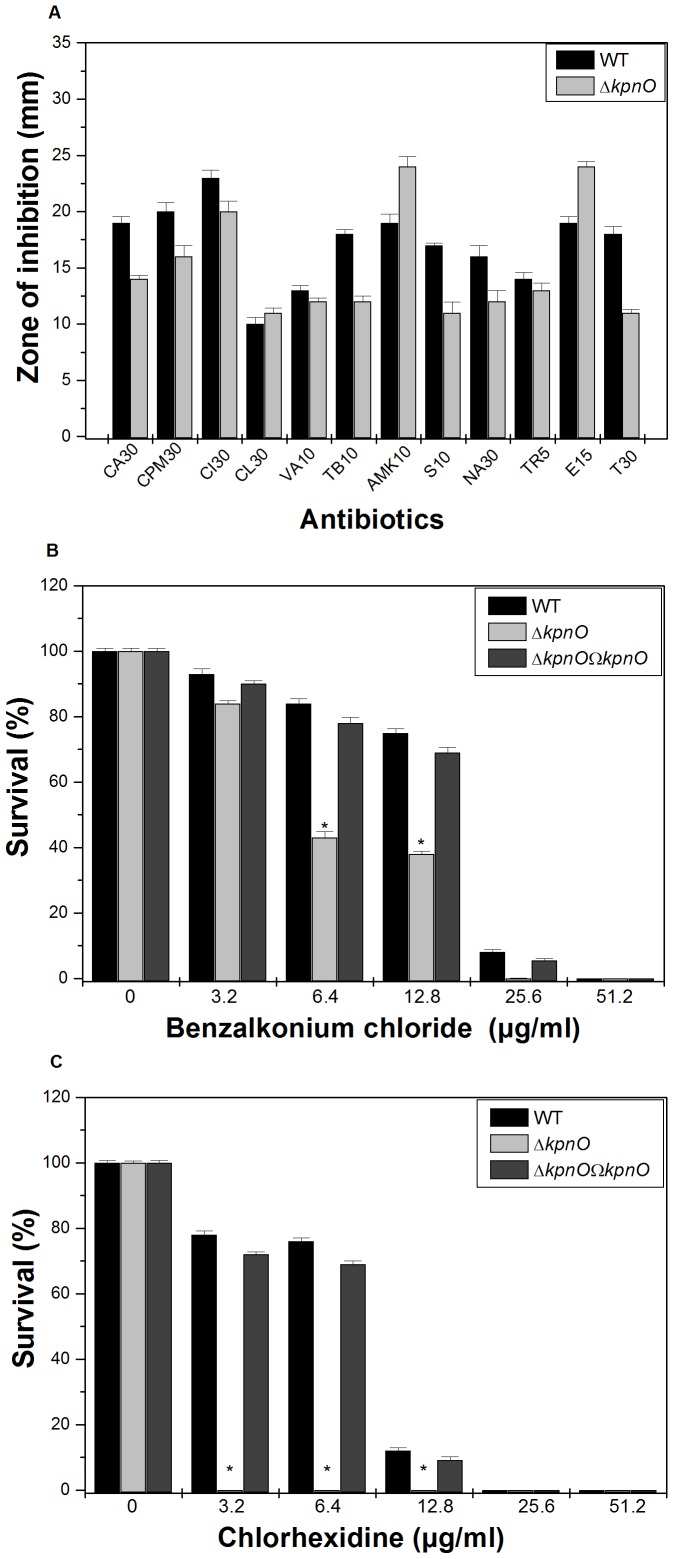
KpnO Mediates Antibiotic and Disinfectant Resistance by Altering Active Efflux
To evaluate the role of kpnO in drug resistance, antibiotic susceptibilities of WT and ΔkpnO were monitored. The results of disc diffusion assays indicated that upon deleting the porin, the bacterial cells displayed significantly altered susceptibility to ceftazidime, cefepime, ceftriaxone, tobramycin, amikacin, streptomycin, spectinomycin, nalidixic acid, erythromycin and tetracycline (Figure 5–A). The precise minimum inhibitory concentration (MIC) was further evaluated by following the guidelines of CLSI by E-test. The MIC of ΔkpnO was increased (fold increase in brackets); for different antibiotics namely nalidixic acid {4 fold}, tobramycin {4 fold}, streptomycin {10 fold}, spectinomycin {10 fold}, and tetracycline {3 fold} respectively compared to WT (Table 2). The MIC of erythromycin for ΔkpnO was 3-fold lower while compared to WT. In summary, deletion of kpnO altered the antibiotic susceptibility profile of K. pneumoniae belonging to K1 serotype.
Figure 5. Antibiotic susceptibility testing and disinfectant challenge assays.
A) The Kirby Bauer disc diffusion assay was performed with different antibiotics (CA30, CPM30, CI30, CL30, VA10, TB10, AMK10, S10, NA30, TR5, E15 and T30) using commercial discs. Data for representative drugs from each class have been shown here. B) Sensitivity towards benzalkonium chloride by WT and phoB KP mutant when cells were exposed to different concentrations of the disinfectant (3.2 µg/ml, 6.4 µg/ml, 12.8 µg/ml, 25.6 µg/ml, 51.2 µg/ml). C) Tolerance of WT and phoB KP to different concentration of chlorhexidine. The percent survival was calculated by comparison of viable cells in control. The datas are the means of measurements made in triplicate performed three times. *, significant difference (P<0.05, Student t test).
Table 2. Determination of MIC for WT, ΔkpnO, ΔkpnOΩkpnO, ΔphoB KP, and ΔphoB KPΩphoB KP.
| Antibiotics | WT | ΔkpnO | Fold changea | ΔkpnOΩ kpnO | ΔphoBKP | Fold changea | Δ phoBKPΩ phoBKP |
| Amikacin | 0.064 | 0.032 | 2 | 0.064 | 0.008 | 8 | 0.064 |
| Cefepime | 2 | 4 | 2 | 2 | 0.5 | 4 | 2 |
| Ceftazidime | 0.256 | 0.512 | 2 | 0.256 | 0.128 | 2 | 0.256 |
| Chloramphenicol | 0.1 | 0.1 | 1 | 0.1 | 0.01 | 10 | 0.1 |
| Colistin | 0.01 | 0.01 | 1 | 0.01 | 0.001 | 10 | 0.01 |
| Erythromycin | 30 | 10 | 3 | 30 | 5 | 6 | 30 |
| Nalidixic acid | 0.1 | 0.4 | 4 | 0.1 | 0.1 | 1 | 0.1 |
| Streptomycin | 0.1 | >1 | 10 | >0.05 | 0.01 | 10 | >0.05 |
| Spectinomycin | 0.1 | >1 | 10 | >0.05 | 0.1 | 1 | 0.1 |
| Tetracycline | 5 | 15 | 3 | 5 | 5 | 1 | 5 |
| Tobramycin | 0.1 | 0.4 | 4 | 0.1 | 0.1 | 1 | 0.1 |
| Trimethoprim | 0.1 | 0.1 | 1 | 0.1 | 0.01 | 10 | 0.1 |
E-strips were used to determine the precise MIC for different group of antibiotics such as ceftazidime, cefepime, ceftriaxone, nalidixic acid, streptomycin, tetracycline, trimethoprim, vancomycin, amikacin, erythromycin, tobramycin, chloramphenicol, ciprofloxacin, colistin, norfloxacin, ofloxacin, polymyxin, rifampicin, sparfloxacin, and spectinomycin following the CLSI guidelines. Complementation restored the MIC values. Units for MIC values are µg/ml.
Fold change is the ratio of MICs for WT and ΔkpnO or ΔphoB KP.
To decipher whether kpnO confers antibiotic resistance by affecting drug efflux, screening for a potential efflux phenotype was accomplished by determining the growth profile of WT and ΔkpnO in the presence of antibiotics and carbonyl cyanide 3-chlorophenylhydrazone (CCCP) (10 µg/ml) as described in methods section. The growth rate of ΔkpnO in the presence of 0.005 µg/ml ciprofloxacin was >16 fold lower than the WT [WT/ΔkpnO mutant, P = 0.007]. The addition of CCCP drastically reduced the growth in both strains as the action of antimicrobials was restored (Figure S3). In independent experiments, growth remained unaltered on the addition of reserpine. Results described here demonstrated that deletion of kpnO impaired the active efflux capacity in K. pneumoniae.
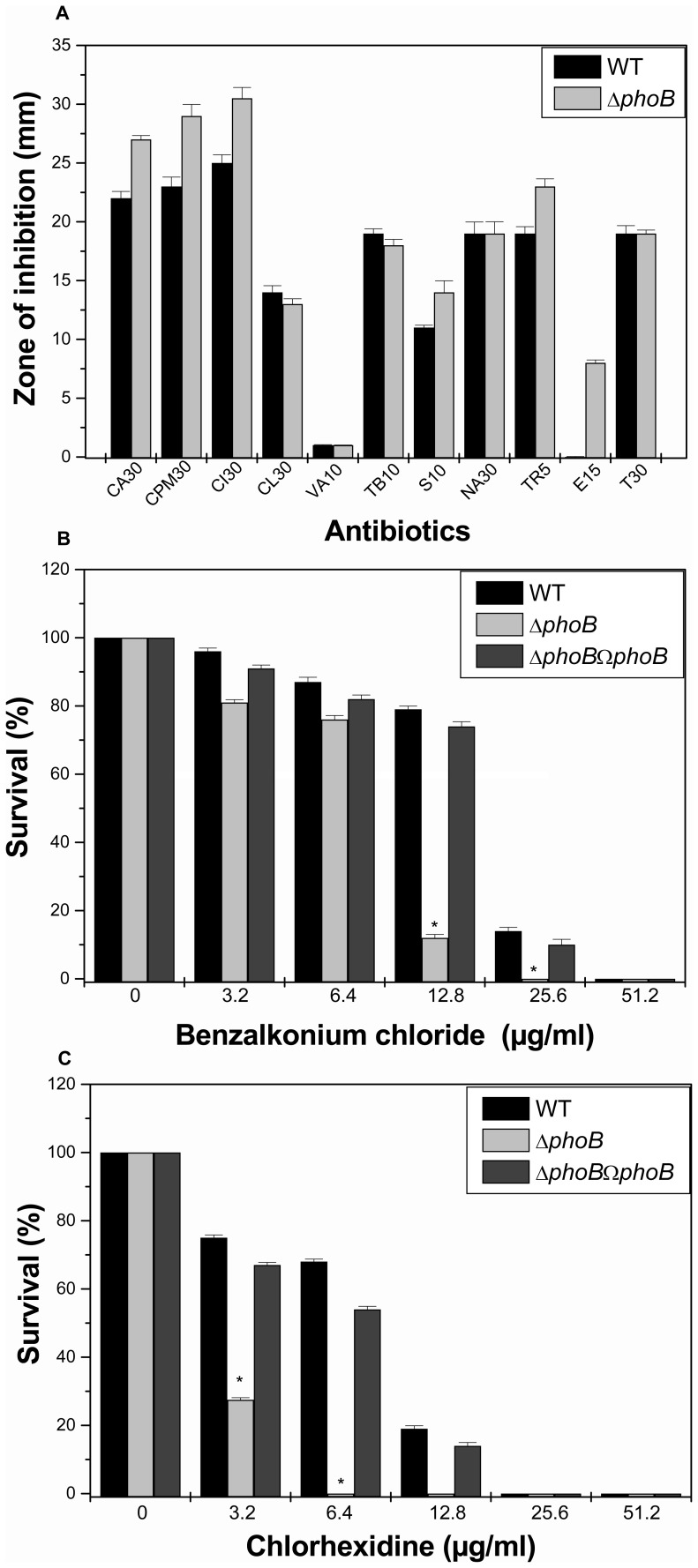
K. pneumoniae is a nosocomial pathogen and has an ability to remain viable on abiotic surfaces for long periods of time [25]; therefore we tested the susceptibilities of WT and ΔkpnO towards different concentrations of popularly used hospital based disinfectants such as chlorhexidine and benzalkonium chloride. The percent survival of ΔkpnO cells was reduced by 50% when exposed to 6.4 µg/ml of benzalkonium chloride [WT/ΔkpnO mutant, P = 0.08; WT/transcomplemented, P = 0.04] (Figure 5–B). The percent survival of ΔkpnO was reduced by 100% when exposed to 3.2 µg/ml chlorhexidine [WT/ΔkpnO mutant, P = 0.13; WT/transcomplemented, P = 0.09] (Figure 5–C), indicating the contributory role of kpnO in conferring disinfectant resistance in this nosocomial pathogen. In conclusion involvement of kpnO in mediating antibiotic resistance via efflux mechanism and its added contribution towards disinfectant tolerance has been demonstrated for the first time in K. pneumoniae.
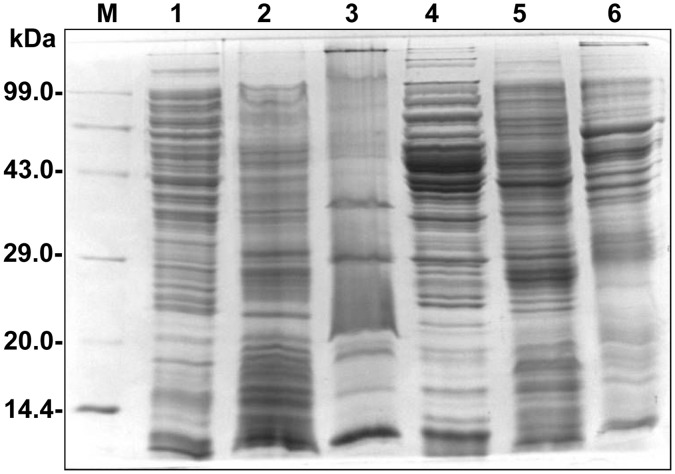
Alterations in OM Profile of the kpnO Deletion Mutant in K. pneumoniae
The cell envelope is the prime target for most outside stress conditions that may modify envelope components and thus cause an extra cytoplasmic stress response [26], [27]. A reduction in the permeation of antibiotics is generally related to a decrease in porin expression or an alteration in the porin structure [28]. Thus, we compared the OMP profiles of ΔkpnO with WT to find out whether a kpnO deleted mutant expresses alternative porins/OMPs to maintain normal cellular functions. It was interesting to note that there was a marked difference in the OMP profiles of mutant compared to wild type (Figure 6), and currently our lab is involved in deciphering the identity and function of these proteins.
Figure 6. Protein profiling of WT and kpnO mutant strain.
Membrane protein profiles were compared between the wild-type strain, and kpnO mutant. Total protein lysate of wild-type strain (lane 1), outer membrane fractions (lane 2), inner membrane fractions (lane 3), followed by total protein lysate of kpnO mutant (lane 4), outer membrane fractions (lane 5), inner membrane fractions (lane 6). Equal protein concentrations were separated by SDS-PAGE with a 5% stacking gel and a 12% separating gel and stained with coomassie brilliant blue. Lane M has molecular weight standards. The over expressed bands in outer membrane fractions of kpnO mutant are shown by arrow heads.
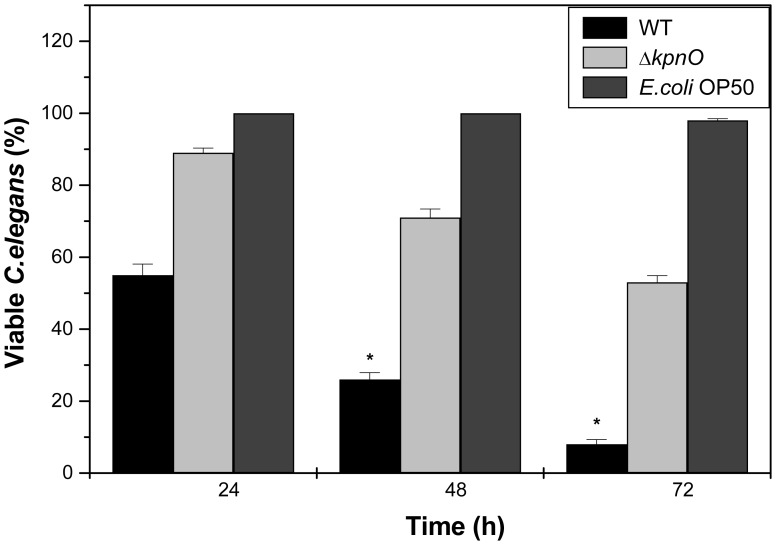
Role of KpnO in Virulence in K. pneumoniae NTUH-K2044
The Caenorhabditis elegans - K. pneumoniae infection model was employed to determine the involvement of kpnO in virulence. The wild type and mutant strains were examined for their abilities to kill C. elegans. The wild type strain displayed 80% and 90% killing at 48 and 72 h respectively. However, the mutant strain killed only 30% of the worms after 48 h (P<0.01) (Figure 7). Similar results were observed in liquid killing assay (data not shown). The E.coli strain OP50 was used as negative control. Thus, our findings demonstrate that the kpnO mutant kills C. elegans more slowly than wild type strain.
Figure 7. C. elegans killing assay.
The K. pneumoniae kpnO gene is required for virulence to the nematode C. elegans. Survival of C. elegans after infection with K. pneumoniae WT, kpnO mutant and E.coli OP50.
Prediction of PhoB Binding Sites in Regulatory Regions of kpnO
Deciphering transcriptional regulatory systems is a key step in understanding the regulation of bacterial biological processes, as a whole. Genome sequence analysis of K. pneumoniae NTUH-K2044 revealed the presence of >466 signalling proteins (http://mistdb.com) including many uncharacterized TCS. Recently, we demonstrated that the CpxAR TCS that senses envelope stress alters the expression of kpnO to mediate antimicrobial resistance in K. pneumoniae [21]. Different stress response pathways are induced in bacteria under different environmental assails and one such important system is the PhoBR TCS, where PhoR is the histidine kinase (HK) and PhoB is the response regulator (RR) [29]. It is interesting to state here that on performing genome-wide prediction of K. pneumoniae, we identified putative PhoB binding sites in the kpnO regulatory regions. Given the association of the PhoBR regulatory system with stress responsive pathways and the apparent presence of a PhoB binding site upstream of kpnO caused us to investigate the probable role of PhoBR in regulating kpnO. Therefore, to evaluate the role of PhoBR system in antimicrobial susceptibility and stress response, a phoB KP mutant was constructed and expression of kpnO in the ΔphoB KP was monitored.
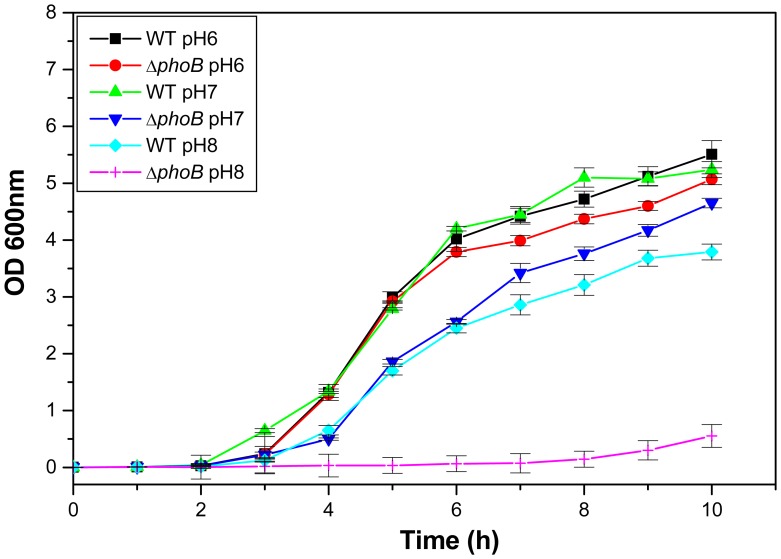
Deletion of phoB KP Affects Capsule Production and Cellular Growth
The colonies of WT were bigger (3.2±0.7 mm) with larger strings (4.5±0.5 cm) while the phoB KP mutant exhibited a reduction in colony size (1.0±0.15 mm) (Figure 8–A) with decreased mucosity by string test (0.75±0.02 cm) (Figure 8–B) and by centrifugation (Figure 8–C). Defects in exopolysaccharide production by ΔphoB KP were visually observed by Anthony's capsule staining (Figure 8–D) and reconfirmed by uronic acid quantification (Table 1). The phoB KP mutant exhibited stunted growth (∼6.8 fold) compared to WT in LB at pH 8.0 (Figure 9) [WT/ΔphoB KP mutant, P = 0.004]. The apparent density of ΔphoB KP was 1.6 fold (±0.35) lower compared to wild-type parent strain after 6 h, with no significant difference thereafter at pH 7.0 [WT/ΔphoB KP mutant, P = 0.001]. Results presented here demonstrate the role of phoB KP in capsule production and bacterial growth in K. pneumoniae.
Figure 8. Phenotypic characterization of phoB KP mutant.
A) Colony size of ΔphoB KP was smaller (1.0±0.15 mm) than the wild-type (3.2±0.7 mm). B) The phoB KP mutant produced smaller strings (0.75±0.02 cm) than wild-type (4.5±0.5 cm). C) Upon centrifugation at 4000 rpm for 3 min; ΔphoB KP formed dense pellet in contrast to WT. D) ΔphoB KP exhibited loss in capsular polysaccharide production as compared to WT.
Figure 9. Growth kinetics.
Growth kinetics of WT, and ΔphoB KP was assessed in LB medium pH 6.0, 7.0 and pH 8.0.
Impact of phoB Deletion on Gastrointestinal, Oxidative and Nitrostative Stress Tolerance
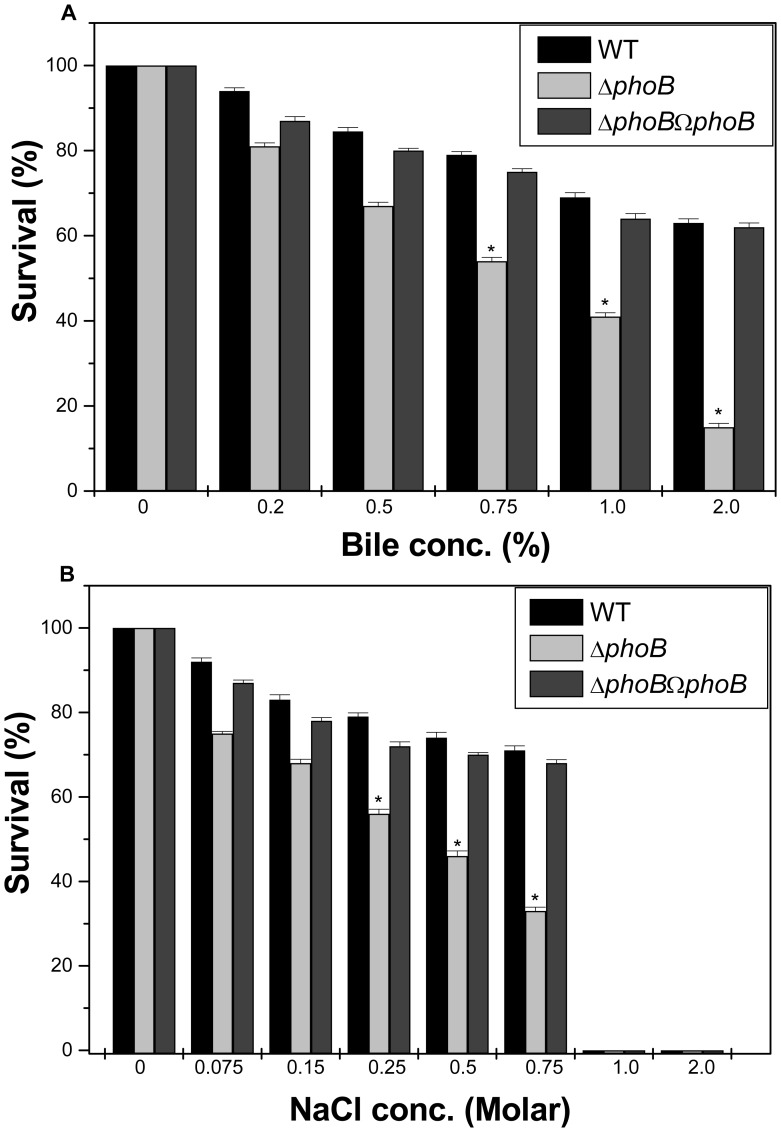
To determine the impact of the phoB deletion on general stress response, different stress challenge assays were performed. The ability of WT to grow in the presence of 0.75% bile was 1.5 fold (±0.027), 1% bile was 1.7 fold (±0.044) and 2% was 4.2 fold (±0.18) higher when compared to ΔphoB KP, while the transcomplemented strain restored the ability to tolerate stress (Figure 10–A) [WT/ΔphoB KP, P = 0.02; WT/transcomplemented, P = 0.02]. The ability of WT to grow in the presence of NaCl at 0.25 M was 1.4 fold (±0.033), 0.5 M was 1.6 fold (±0.076), and 0.75 M was 2 fold (±0.13), higher when compared to WTΔphoB KP regardless of the inoculum size (Figure 10–B) [WT/ΔphoB KP, P = 0.02; WT/transcomplemented, P = 0.017].
Figure 10. Bile and Osmotic challenge assays.
Sensitivity of WT and phoB KP mutant to varied gastrointestinal challenges such as bile (A) and NaCl (B). The percent survival was calculated by comparison of viable cells in control.
Oxidative stress tolerance remained unaltered in the phoB KP mutant of K. pneumoniae (inhibition zone = 32.5±0.5 mm) as compared to wild type (inhibition zone = 33±1.0 mm) [WT/ΔphoB KP mutant, P = 0.18] (Figure 11–A). The mutant remained unaffected when exposed to nitrostative stress conditions with 10 mM SNP [WT/ΔphoB KP mutant, P = 0.17] (Figure 11–B), 20 mM or 30 mM SNP respectively (Figure S4). The observation was the same upon using NaNO2 as the alternative NO donor (Figure 11–C). It is worthy to note that phoB KP deletion did not affect the capabilities of K. pneumoniae to tolerate oxidative and nitrostative stresses, but it displayed sensitivity to gastrointestinal like challenges.
Figure 11. Oxidative and nitrostative challenge assays.
A) Oxidative stress response of phoB KP mutant by disc assay. The phoB KP mutant displayed greater sensitivity to 30% H2O2 (inhibition zone = 32.5±0.5 mm) than the wild-type (inhibition zone = 33±1.0 mm). B) The data is the means of measurements made in triplicate. *, Significant difference (P<0.05, Student t test). B) Effect of SNP (10 mM) on growth kinetics of WT and ΔphoB KP. C) Effect of NaNO2 (10 mM) on growth profile of WT and ΔphoB KP.
Loss of PhoB Diminishes Antibiotic and Disinfectant Susceptibilities
To evaluate the role of phoB in drug resistance, antibiotic susceptibilities of WT and ΔphoB KP were monitored. The results of disc diffusion assay displayed that upon deleting the TCS, the bacterial cells displayed altered susceptibility to ceftazidime, cefepime, ceftriaxone, ertapenem, carbenicillin, and the quinolones (Figure 12–A). The ΔphoB exhibited reduced MICs (fold decrease in brackets) to amikacin {8 fold}, cefepime {4 fold}, ceftazidime {2 fold}, chloramphenicol {10 fold}, Colistin {10 fold}, erythromycin {6 fold}, streptomycin {10 fold} and trimethoprim {10 fold} (Table 2) in comparison to WT. To monitor the impact on active efflux, the growth rate of ΔphoB KP in the presence of 0.005 µg/ml ciprofloxacin was monitored and data reflect a 1.2-fold lower growth in the mutant than the WT [WT/ΔphoB KP mutant, P = 0.001]. The addition of CCCP drastically reduced the growth in both strains as the action of antimicrobials got restored (Figure S5). The impact of PhoB deletion on biocide susceptibilities was assessed by survival assays. The WT cells survived up to 79% on exposure with 12.8 µg/ml of benzalkonium chloride while percent survival was only 12% with the phoB KP mutant [WT/ΔphoB KP mutant, P = 0.14; WT/transcomplemented, P = 0.02] (Figure 12–B). Like wise the WT cells survived up to 75% on exposure with 3.2 µg/ml of chlorhexidine while percent survival was only 27% in the phoB KP mutant [WT/ΔphoB KP mutant, P = 0.11; WT/transcomplemented, P = 0.11](Figure 12–C). Results described here demonstrated the involvement of phoB in mediating antibiotic and disinfectant resistance in K. pneumoniae for the first time.
Figure 12. Antimicrobial susceptibilities of phoB KP mutant.
Kirby Bauer disc diffusion assay was performed with different antibiotics and data for representative drugs are shown (A). Measure of disinfectant tolerance by WT and phoB KP mutant when cells were exposed to different concentrations benzalkonium chloride (B) and chlorhexidine (C). The percent survival was calculated by comparison of viable cells in control. The datas are the means of measurements made in triplicate performed three times. *, significant difference (P<0.05, Student t test).
PhoB Regulates kpnO in K. pneumoniae
Inorganic phosphate is sensed and regulated in bacteria by the Pho regulon, which in turn is controlled by the PhoB-PhoR TCS [29]. PhoR, unlike other sensor HK, does not have a large periplasmic domain but has an extended cytoplasmic domain. The function of this extended cytoplasmic domain is proposed to sense internal signals that repress the kinase function of the PhoR. PhoB is the RR that binds to DNA and regulates transcription of genes, such as the high affinity phosphate-specific transport (pst) system, to acquire Pi [30]. Previous studies have reported that besides regulating the expression of the Pst system, Pho TCS also modulates the expression of other bacterial genes. PhoB binds to promoters that share an 18-bp Pho box of the sequence 5′-CTGTCATA(A/T)A(T/A) CTGT(C/A)A(C/T)-3′ [31].
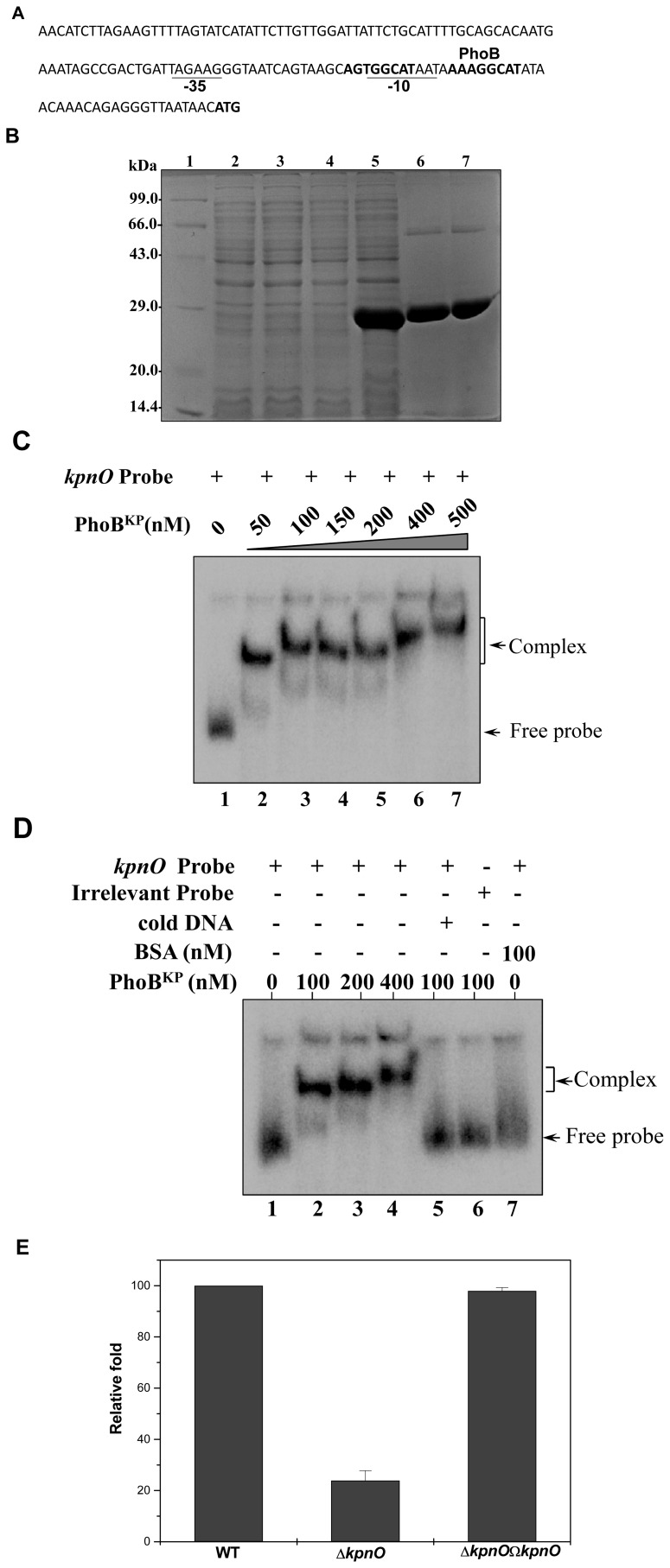
We assessed the promoter region of kpnO and analysis revealed the presence of a conserved putative PhoB binding site spanning the region between 24 to 43 bp from the first methionine of KpnO (Figure 13–A). The PhoBKP; KP1_2137, is a 714 bp gene that encodes a polypeptide of 237aa (27 kDa). To define the possible interaction of PhoBKP with the promoter of kpnO, we tested whether PhoBKP directly interacts with the promoter region of kpnO; the phoB KP gene was cloned and expressed. The phoB KP gene from K. pneumoniae was PCR amplified, cloned into pET-28c and after transformation in E. coli strain BL21 (DE3), expression of the His-tagged protein (PhoBKP) was monitored following IPTG induction. Cell lysates were purified on a Ni-NTA column, and resolved by SDS/PAGE, subsequent analysis yielded an expected induced band of ∼27 kDa (Figure 13–B).
Figure 13. PhoB regulates kpnO in K. pneumoniae.
A. Promoter region analysis of kpnO. The numbers in brackets represent the distance from the transcription start site. The −35 and −10 region in the promoter is underlined. Putative PhoB binding site has been shown in bold. B. SDS-PAGE profile of pET-phoB KP. Lane 1: medium size marker, Lane 2: pET28C/BL21DE3 uninduced, Lane 3: pET28C/BL21DE3 induced, Lane 4: pET-phoB KP/BL21DE3 uninduced, Lane 5: pET- phoB KP/BL21DE3 induced, purified PhoBKP-fractions E1 and E2 (lanes 6–7) respectively. Protein samples after induction were subjected to SDS/PAGE (15% gel) followed by coomassie brilliant blue staining. C. Gel shift assays demonstrating the binding of PhoB to promoter of outer membrane protein kpnO in K. pneumoniae in a concentration dependent manner. Lane 1 (shows free probe), lanes 2–7 with increasing concentrations of PhoB protein (50 nM to 500 nM) respectively. Slower moving bound complexes and free probe has been indicated by arrows respectively. The gels are representative of at least three independent experiments. D. Gel shift assays demonstrating the sequence-specific binding of PhoB to kpnO using different controls as in lane 1 (shows free probe), lanes 2–4 (labeled kpnO promoter with increasing amount (100 nM, 200 nM and 400 nM) of PhoB), lane 5 (labeled kpnO promoter and PhoB with specific competitive inhibitor: 10 fold excess of unlabeled kpnO promoter), lane 6 (labeled non-specific DNA: promoter of gyrA and PhoB, 100 nM), lane 7 (labeled kpnO promoter with non-specific protein: BSA, 100 nM) respectively. The gels are representative of at least three independent experiments. E. Relative transcriptional level of kpnO in ΔphoB KP and ΔphoB KPΩphoB KP strains determined using real time RT-PCR is showed in comparison with wild type. The wild type expression level is represented as one fold. Each bar represents the average value of three independent experiments. Error bars are standard deviations.
Thereafter, we carried out gel shift assays using the 32P-labeled kpnO promoter fragment. Protein-DNA complexes formed upon incubation of PhoBKP with 500 bp radiolabelled kpnO promoter in reaction buffer, resolved on 5% PAGE revealed a clear retardation which was directly proportional to the protein concentration (Figure 13–C). Lack of any binding/retardation upon using different controls such as competitive (specific: 10 fold excess of cold promoter and non-specific: poly dI-dC) and non-competitive inhibitor (bovine serum albumin, BSA) clearly demonstrated the specific DNA binding ability of PhoBKP to promoter region of kpnO in K. pneumoniae (Figure 13–D).
Expression Analysis of kpnO in phoB KP Mutant in K.pneumoniae
Quantitative real-time RT-PCR (qRT-PCR) was used to examine expression of kpnO in wild-type, phoB KP mutant, and complemented strains. Compared to the wild-type strain, expression of kpnO was decreased by ∼4 fold in the phoB KP mutant (ΔphoB KP and wild type: P<0.0003, Student’s t test) (Figure 13–E). Complementation of the phoB KP mutation almost restored expression of kpnO (P values <0.0001). Together these results provide evidence for the regulatory role of PhoBR system on OMP KpnO.
Discussion
OMPs allow for the passive diffusion of small molecules into the bacterial cell [32]. Passage of solutes through the cell envelope and control of this process are essential to cell survival when nutrients are scarce or when the cell is exposed to toxins or other adverse conditions [2]. In E. coli, there are three major OMPs, OmpA, OmpC, and OmpF, which function as passive diffusion channels for small molecules, such as nutrients, toxic salts, and antibiotics [26]. Changes in OMPs have been recognized to be very important in the development of clinical antibiotic resistance [28]. Mutations in OmpC have been dissected in E. coli and Enterobacter aerogenes that are isolated after drug treatment [33], [34].
In K. pneumoniae OmpK35 and OmpK36 are the two major porins [13]. Previous study has shown that combination of high-level production of AmpC β-lactamases such as ACT-1, CMY-4, DHA-1 or SHV-2 together with porin loss can result in resistance or reduced susceptibility to carbapenems in K. pneumoniae [35]–[37]. A separate study from Korea has shown that production of CMY-2 and DHA-1 together with loss of OmpK35 and OmpK36 resulted in an outbreak of K. pneumoniae, where strains remained mostly non-susceptible to imipenem [38]. In another study, the presence of CTX-M-1, together with loss of OmpK35 and OmpK36 was shown to result in resistance [39]. These findings suggest that OmpK36 plays an important role in resistance. The OmpK36 homolog is annotated in the genome sequence of hyper virulent and hyper mucoviscous strain, however its functions have remained completely unexplored so far. Thus experimental evidence for the biological functions of the OmpK36 homolog in K. pneumoniae NTUH-K2044 with respect to general bacterial stress response, antimicrobial resistance and virulence has been provided in this report for the first time.
The CPS of K. pneumoniae is complex acidic polysaccharide consisting of repeating units of 3–6 sugars. The type of sugars seems to correlate with the virulence, and untill now 78 capsule types have been identified [9]. The wild type strain was found to express a prominent capsule like structure surrounding the bacterial cell, while the kpnO mutant displayed a non-mucoid phenotype and lacked the well-defined capsule coat. In K. pneumoniae KpnO possibly functions as the auxiliary protein necessary for export of high molecular weight polysaccharides to the bacterial surface to form the capsule. Enteric bacteria are known to respond to hostile conditions in the host by altering the expression of genes whose products are involved in the resistance mechanism. The kpnO mutant displayed 1.5–3.0 fold higher sensitivity to varied gastrointestinal like stress irrespective of the inoculum size. Experimental evidence pinpointing the key role of KpnO in survival of the pleomorphic bacillus under conditions mimicking the upper parts of the GI, where they encounter hyper osmotic and bile salts condition in a microaerobic environment has been provided for the first time in K. pneumoniae. Impaired adaptation of kpnO during temperature stress reveals its key role in heat shock tolerance.
Antimicrobial therapy for K. pneumoniae is often ineffective as members of the Klebsiella spp. are highly resistant to most clinically relevant antimicrobial agents [12]. Multidrug resistance in K. pneumoniae is defined as resistance to all of the agents belonging to at least two of three classes of antibiotics, such as quinolones, aminoglycosides, and β-lactam agents [40]. A study in S. Typhimurium has shown that loss of porins STM1530 and OmpD were important for ceftriaxone resistance [41]. A recent study by Tsai et al in K. pneumoniae strain NVT2001 belonging K2 serotype has demonstrated that deletion of ompK36 results in resistance to a group of β-lactams such as cefazolin, cephalothin, and cefoxitin [13]. Current study on the porin kpnO from the K1 serotype reflects its broad spectrum antibiogram. Loss of kpnO rendered cells resistant not only to β-lactams such as ceftazidime, cefepime, ceftriaxone, but also to aminoglycosides such as tobramycin, streptomycin, spectinomycin, including quinolone such as nalidixic acid and polyketide such as tetracycline.
In previous years, the possibility that widely-used disinfectants might co-select for antibiotic resistance has been suggested to pose a potential risk to the successful treatment of hospital acquired infections [42]. A few studies have shown that disinfectants induce resistance determinants thereby reducing susceptibility to antibiotics in bacteria [43]. Therefore, it is plausible that antibiotic sensitive K. pneumoniae commonly found in hospitals (where there is heavy use of disinfectants), when exposed to such continued selective pressure might transform to exhibit antibiotic resistant phenotypes. Besides, we found that kpnO mutant exhibited a reduced ability to kill the nematode C. elegans demonstrating its key role in virulence. Hence, these studies implicate an important role for kpnO in antimicrobial resistance and virulence.
Signal transduction systems are intracellular information processing pathways that translate external stimulus to an adaptive cellular response [44]. In our previous study, we showed that CpxR modulates the expression of kpnO to mediate antimicrobial resistance in K. pneumoniae [21]. The current study was expanded by decoding the regulation of kpnO in K. pneumoniae NTUH-K2044. In E. coli anaerobiosis is known to up regulate the expression of OmpC [32]. Previous reports have shown that acidic pH and presence of chemicals such as bile salts in the environment also induce expression of OmpC [45]. Another study has shown that OmpC is expressed under high osmolarity conditions in animal intestine at 37°C [46]. Thus one common signal transducing system that can sense all these varied signals is the PhoBR TCS in bacteria [30], [31]. Given that PhoBR TCS is a stress responsive signaling system and that the presence of PhoB binding site was detected upstream of kpnO, these observations suggested that PhoBR was a potential regulator of kpnO. Therefore, understanding the regulation of OmpC homolog by PhoB is quite intriguing as both the proteins are highly conserved in bacterial species. The constructed phoB KP mutant displayed impaired sensitivity to gastrointestinal stress similar to that of ΔkpnO. A significant reduction in kpnO mRNA level in phoB KP mutant, together with the binding of PhoB on the regulatory fragments of kpnO provide strong evidence for the involvement of PhoBR system in regulating the expression of kpnO. Interestingly, deletion of kpnO rendered the bacteria resistant to different classes of antibiotics, in contrast to the behaviour of Δ phoB KP where cells became sensitive. The well characterized TCS in bacteria EvgSA, BaeSR, CpxAR and PhoBR are capable of inducing efflux pumps which leads to decreased antibiotic susceptibility [8], [22]. The positive regulation of efflux genes mdtABC and acrD in E. coli and S. Typhimurium by TCS leading to increased resistance of β-lactams, novobiocin and deoxycholate has been reported previously [47]. With such documented observations, the possibility of altered/decreased efflux pump expression reducing antibiotic susceptibility/tolerance in ΔphoB KP cannot be ruled out. A study relating to the impact of phoB KP on efflux pump expression/activity in K. pneumoniae is highly warranted. To our knowledge, this is the first evidence showing that general bacterial porin kpnO regulated by PhoBR is involved in mediating resistance against GI stresses, affecting antibiotic/disinfectants susceptibilities in K. pneumoniae NTUH-K2044; hyper virulent K1 serotype.
Materials and Methods
Bacterial Strains, Plasmids and Media
K. pneumoniae NTUH-K2044 (This strain came from the blood of a previously healthy individual who was diagnosed with a community-acquired primary liver abscess and metastatic meningitis) was kindly provided by Dr. Jin Town Wang of the National Taiwan University Hospital, Taipei, Taiwan [20], [48]. E. coli S17-1λ pir which carries the F plasmid and encodes π protein essential for replication of pUT-Km was used for cloning experiments. Bacteria cultures were grown in Luria-Bertani (LB) broth or on LB agar (Difco, Becton-Dickinson, Sparks, MD) at 37°C with constant shaking (220 rpm) and supplemented with Kanamycin (100 µg/ml) where required.
DNA Methods
Restriction digestion, ligation, transformation, and agarose gel electrophoresis were done according to standard protocols. Plasmids were prepared from E. coli using a QIAprep Spin miniprep kit from Qiagen according to the manufacturer's protocol. Mobilization of plasmids into K. pneumoniae cells was performed as previously described [21]. Genomic DNA of K. pneumoniae was extracted using the Gene Aid DNA purification kit according to the manufacturer's instructions. DNA fragments used for cloning were extracted from agarose gels using a QIA quick gel extraction kit from Qiagen. PCR products were purified using a QIA quick PCR purification kit (Qiagen) and, when cloned, sequenced to confirm the correct sequences (Applied Biosystems). Primers used in the present study were custom-synthesized (Eurofins MWG operons, Germany).
Construction of Deletion Mutants in K. pneumoniae Strain NTUH-K2044
The MisT2 database (www.mistdb.com) shows the presence of 5262 proteins in the 5,472,672 bp (GC content: 57.4%) genome sequence of the K1 serotype (Accession No: AP006725.1). The putative OmpC homolog, KP1_3869 (denoted kpnO) is located starting from nucleotides 3698768 bp to 3699865 bps (kpnO: 1098 bp, 365aa) in the genome sequence of K. pneumoniae NTUH-K2044 [20]. To construct knock out, a 540 bp internal fragment was amplified by PCR using ΔkpnO-F and ΔkpnO-R primer from its genomic DNA (Table 3). The PCR product was ligated into an EcoRI digested plasmid pUT-Km which was blunted by klenow reaction that contained the kanamycin resistance gene, transformed into E. coli S17-1λ pir and the resulting recombinant plasmid harbouring the internal fragment of kpnO was designated as pUT-kpnO. The plasmid pUT-kpnO was mobilized into recipient K. pneumoniae NTUH-K2044 from donor E. coli S17-1λ pir.
Table 3. Primers used in this study.
| Primer name | Primer sequences (5′-3′) |
| ΔkpnO-F | TTGGCGACGCGGGCTCTTTCGACTACGGTC |
| ΔkpnO-R | AAGCGCAGAACTTCGAAGTGGTTGCTCAGT |
| Primer NT-1 | GAGTACATATGAAAGTTAAAGTACTGTCCCTCCTG |
| Primer CT-2 | TACTAGGATCCTTAGAACTGGTAAACCAGGCC |
| phoB-F | GGTACATATGAGCGTCAGACTACTATCGAA |
| phoB-R | TCTAGGATCCTCAGCGCAGTTCGAACAGAT |
| prom kpnO-F | GGCCTAATTGATTGATTAATAGTCGTTAGGGAAT |
| prom kpnO-R | GTTATTAACCCTCTGTTTGTTATATGCCTTTTAT |
| ΔphoBKP-F | GGAAGCGGACTACTATCTGGGCGAACATCTCC |
| ΔphoBKP-R | TCAGGGTTTCCATAATGGTGTATTCAAAGGCG |
| Primer NT-3 | GAGTACATAATCACCAACCCGCTCGCCGTTCGCA |
| Primer CT-4 | TACTAGGATCCATGCCGTAGGCCAGGGAGAGCA |
| RT-kpnO KPNT | ACCCAGACCTACAACGCAAC |
| RT-kpnO KPCT | ATTTCAGGATGTCCTGGTCG |
| RT-rpoB KPNT | GCGGTTGGTCGTATGAAGTT |
| RT-rpoB KPCT | TGGCGTTGATCATATCCTGA |
Briefly, K. pneumoniae was inoculated into 10 ml LB and was incubated for 2–3 h till OD600 nm reaches 0.2. For matings, recipient and donor culture were mixed in a ratio of 1∶2 respectively, pelleted and spotted onto the centre of an LB agar plate. After 3 h of growth at 37°C the cells were plated on Klebsiella selective agar (HiMedia HiCrome Klebsiella Selective Agar Base cat# M1573; Klebsiella Selective Supplement cat# FD225) containing Kanamycin 100 µg/ml and 5 µg/ml chlorhexidine to select for colonies. It is expected that colonies that appear on the selective plate would be transconjugants that resulted from one DNA exchange event in which the whole suicidal plasmid gets incorporated in the K. pneumoniae genome. The disruption at kpnO gene was confirmed with selected transconjugant by PCR and DNA sequencing using gene specific and genome flanking primers and deleted mutant was denoted as ΔkpnO. Intact kpnO gene was amplified along with its promoter using primer NT-1 and primer CT-2 and cloned into a pCRIITOPO-CAT plasmid (Table 3). The selected recombinant plasmid harbouring the intact kpnO gene was transformed into the kpnO isogenic mutant strain by electroporation. The complementation strains were selected on LB agar plates supplemented with 50 µg/mL kanamycin and 100 µg/mL chloramphenicol and transcomplemented strain was designated as ΔkpnOΩkpnO.
The PhoB homolog, KP1_2137 (designated PhoBKP) is located starting from nucleotides 2081389 bp to 2082102 bp (phoBKP: 714 bp, 237aa) in the genome sequence of K. pneumoniae NTUH-K2044 [20]. A 380 bp internal fragment from phoBKP was amplified by PCR using ΔphoBKP-F and ΔphoBKP-R, and null mutant denoted ΔphoBKP was constructed following standard procedures as mentioned above. Intact phoBKP was amplified along with its native promoter using primer NT-3 and primer CT-4 and cloned into a pCRIITOPO-CAT plasmid. The selected recombinant plasmid harbouring the intact phoBKP gene was transformed into the respective isogenic mutant by electroporation to generate ΔphoBKPΩ phoBKP.
Mutant (ΔkpnO and ΔphoBKP) and complemented strains generated in this study (ΔkpnOΩkpnO and ΔphoBKPΩ phoBKP) were characterized; their phenotypes were compared with the WT.
Tests for Hypermucoviscosity
The mutant, complemented and WT strains were streaked onto LB agar plates and incubated at 37°C overnight. A standard bacteriologic loop was used to stretch a mucoviscous string from the colony. Hypermucoviscosity was defined by the formation of viscous strings >5 mm in length when a loop was used to stretch the colony on agar plate which was considered the positive string test [48]. The strains to be tested were cultured 12 h in LB broth at 37°C and subjected to centrifugation at 4000rpm for 3 mins to check reduction in mucoidy. For exopolysaccharide analysis [49], cells were grown to late log phase in shaking culture and stained with crystal violet followed by treatment with 20% copper sulphate solution (Anthony's capsule staining methodology). Samples were visualized using an Olympus microscope work station. CPS was extracted from 12 h grown bacterial suspensions adjusted to ∼108 cells per ml with Zwittergent 3–14 detergent. The amount of uronic acid was then measured according to the method described previously [50]. Each experiment was performed in triplicate.
In vitro Growth Curves
To examine bacterial growth in vitro, overnight cultures were diluted 1∶100 and subcultured for 10 h. The growth kinetics was monitored with LB at different pH (3.0, 6.0, 7.0, 8.0 and 12.0). The growth inhibition assay was performed as described previously [21]. The efflux pump inhibitors (10 µg/ml) used in this study was CCCP or reserpine (Sigma, St. Louis, MO). Efflux pump inhibitors had no intrinsic antibacterial activity against wild type strain at the concentration used in the experiments.
Osmotic, Bile, Disinfectant Challenge Assays
Various stress assays were performed as described previously [50]. Briefly mutant, complemented and WT strains were grown to mid-exponential phase, cultures were spread onto LB agar plates containing different concentrations of NaCl (0.075 M, 0.15 M, 0.25 M, 0.5 M, 0.75 M, 1 and 2 M), bile (0.2%, 0.5%, 0.75%, 1.0%, and 2.0%), disinfectants (benzalkonium chloride and chlorhexidine) (3.2 µg/ml, 6.4 µg/ml, 12.8 µg/ml, 25.6 µg/ml, 51.2 µg/ml) respectively. The results are expressed as the ratio of the number of colony forming units obtained from LB cultures containing different concentrations of NaCl, bile and disinfectants to the number of colony forming units obtained from control cultures (LB agar alone). These experiments were performed at least three times.
Heat Shock Challenge Assay
The wild type and mutant was exposed to different temperatures for heat shock assay such as 30°C, 60°C and 72°C, survival was checked on LB and LB Kan (100 µg/ml) plates respectively.
Oxidative and Nitrostative Stress Tolerance Assay
In this susceptibility test, small Whatman 3 MM paper disks (6 mm) were impregnated with different amount of H2O2 (10 µl of 3%, 10% and 30%) and later air dried as reported before [50]. The different strains were grown to the mid-log phase (OD600 nm 0.2) and were uniformly spread over an LB agar plate. Next, filter paper disks impregnated with specific concentrations of H2O2 was placed at the centre on to the agar surface. The culture was then incubated at 37°C for 12–24 hours. The diameter of a zone of inhibition was measured (in millimeters) which is a qualitative measure of the inhibitory activity of a compound. The data represents the distances from the edge of the disks to the end of the clear zone, where growth begins. Each experiment was repeated at least three times. The sensitivity of cells to oxidative stress was tested by exposing stationary-phase bacteria diluted in LB medium (OD600 nm 0.2) at 37°C to 0.07894 mM, 0.7894 mM, 1.5788 mM, 2.3682 mM and 3.1576 mM for 1 h. Viable cells were counted by plating them onto agar plates before and after exposure to H2O2, and results are expressed as survival percentages.
Sodium nitroprusside (SNP) and acidified nitrite were used to generate nitrostative stress to check cell growth against these NO releasing agents [24]. Growth of cultures against SNP was determined as described previously [21]. Briefly, different strains were grown aerobically in LB medium up to OD600 nm of 0.2. The cells were then treated with different concentrations of SNP and growth was monitored at OD600 nm at an interval of every one hour. To check the response of cultures against acidified nitrite, growth profile of different strains, were determined at pH 6.0 and 7.0 in buffered LB medium supplemented with 10 and 30 mM sodium nitrite and compared with the WT by observing OD600 nm periodically.
Kirby Bauer Disc Diffusion Assay
Strains in this study were examined for resistance to different antibiotics by using commercial discs (Hi Media, Bombay, India) as described previously [21], according to the interpretation criteria recommended by Clinical and Laboratory Standards Institute CLSI [51].
Determination of MIC
MIC of antibiotics was tested using E-strips. Interpretation was done as per the criteria approved by CLSI. E. coli ATCC 25922 was used as a reference strain (control) as recommended.
OMP Preparation
OMPs were purified by the method as described previously [13]. Cells were harvested by centrifugation 5000 g for 15–20 mins and were suspended in 50 mM Tris-HCl buffer (pH 7.4) containing 5 mM phenylmethylsulfonyl fluoride and sonicated for 15 mins. The crushed material was treated with DNase and RNase (each at 100 µg/ml), and the unbroken cells were removed by centrifugation (10,000 × g for 10 min). The crude envelope fraction was collected from the supernatant by centrifugation at 105,000× g for 1 h at 4°C. The pellet containing the crude envelope fraction was treated with 0.5% (wt/vol) sarkosyl (Sigma) solution to selectively solubilise the inner membrane part. The insoluble OM fraction was recovered as pellet by centrifugation at 105,000× g for 1 h at 4°C. The pellet was washed and stored at −20°C until used. Protein contents of membrane preparations were determined by the method of bicinchoninic acid (BCA) method (Pierce BCA protein assay kit, cat# 23225) with bovine serum albumin (BSA) (Sigma) as standard.
Gene Cloning, Expression, Purification and Electrophoretic Mobility Shift Assays (EMSA)
The DNA-binding transcriptional regulator gene phoB was amplified using gene specific primers, phoB-F and phoB-R has NdeI and BamHI sites of the pET28C vector to generate an N-terminal His6-PhoB fusion protein. All clones were confirmed by sequencing and transformed into E. coli BL21 (DE3). After induction with 0.2 mM isopropyl 1-thio-β-d-galactopyranoside, PhoB protein was purified through Qiagen Ni2+nitrilotriacetic acid columns. The protein was dialysed using Tris buffer pH 8.0. The ability of PhoB to bind kpnO promoter was tested by EMSA. The kpnO promoter region was amplified using promkpnO-F and promkpnO-R primers (Table 3) and subjected to EMSA with purified PhoB protein. Briefly, end-labelled (using [γ-32P] ATP) PCR products were incubated with increasing concentrations (in a range of 50 nM to 500 nM) of PhoB in binding buffer (10 mM Tris-HCl, pH 8.0, 2 mM EDTA, 0.5 mM DTT, 50 mM NaCl, 10% glycerol, and 1 µg of poly(dI·dC). The complexes were run on 5% native polyacrylamide gel electrophoresis (PAGE) gels for 2 h. The gel was then dried and exposed to the phosphor screen for image analysis. To confirm that the interaction between PhoB and the promoter region of kpnO was specific, experiments with competitive (specific: 10 fold excess of cold promoter and non-specific: poly dI-dC) and non-competitive inhibitor (BSA) were also performed.
RNA Isolation and Real-time Reverse Transcription PCR (RT-PCR)
Total RNA was extracted from the log-phase cultures of wild-type and phoB KP mutant using the RNeasy Mini Kit (Qiagen) according to the manufacturer's instructions. Total RNA was digested with DNase I to ensure the removal of contaminating genomic DNA prior to cDNA synthesis. Aliquots of 500 ng of DNase I treated total RNA served as template for complementary DNA (cDNA) synthesis using SuperScript III Reverse Transcriptase (Invitrogen). The cDNA samples were diluted 1∶100 and 2 µL was used per 25 µL quantitative PCR reaction for kpnO and were performed using gene specific primers (Table 3). Gene expression levels were monitored by real time RT-PCR using Maxima SYBR Green qPCR master mix (Fermentas) in an iCycler thermal cycler (Bio-Rad) and the melting curve analysis were carried out to confirm amplification of a single product. Total RNA was isolated from at least two separately grown replicate cultures. All real time RT-PCR experiments were performed in triplicate, with rpoB as an internal control.
Caenorhabditis Elegans Killing Assay
Bacterial virulence (both agar and liquid killing) assays were performed using nematode model, C. elegans strain Bristol N2 as described previously with slight modifications [52], [53]. To examine the ability of wild-type, mutant and E. coli OP50 strains to kill C. elegans, bacterial lawns of the K. pneumoniae and an E. coli control strain were prepared on nematode growth (NG) media and incubated at 37°C for 6 h. The plates were kept at room temperature for 1 hr and then seeded with L4-stage worms (25 to 30 per plate). Further the seeded plates were incubated at 25°C and examined for live worms under a stereomicroscope (Leica MS5) after every 24 hours. When the worm did not react to touch it was considered dead. At least five replicates repeated three times were performed for each selected strain.
Bioinformatic Analysis and Statistical Analysis
Multiple sequence alignments were carried out using the Clustal program www.ebi.ac.uk Homology searches, similarities and identities analysis and conserved domain architecture analysis were performed using NCBI Internet server [54], Simple Modular Architecture Research Tool (SMART) www.smart.embl-heidelberg.de and NCBI conserved domain search. All data are presented as means ± the standard error of the mean. Plotting and calculation of the standard deviation was performed in Microsoft Excel. Statistical analysis was performed on crude data by using a paired Student t test. P values of <0.05 were considered significant.
Supporting Information
Oxidative stress assays. Survival of K. pneumoniae and ΔkpnO strains upon exposure to oxidative stress with 0.07894 mM, 0.7894 mM, 1.5788 mM, 2.3682 mM and 3.1576 mM. After 1 h of treatment with 0.07894 mM hydrogen peroxide, only 47% of ΔkpnO cells survived in comparison to 95% of the wild-type cells. The differences between the mutant and its parental wild-type strain are statistically significant (P<0.05) for all H2O2 concentrations. The standard errors of the means from three independent assays are shown.
(TIF)
Nitrostative challenge assays. Growth pattern of WT, ΔkpnO in the presence of sodium nitrite. In the presence of 30 mM NO donor, growth kinetics of ΔkpnO cells was ∼7.0 fold lower as compared to WT at pH 7.0.
(TIF)
Growth inactivation assays. Inactivation assays using ciprofloxacin (0.005 µg/ml). The efflux pump inhibitors CCCP was used at a concentration of 10 µg/ml in the experiment. The mean values of three independent experiments have been used for plotting the graph.
(TIF)
Nitrostative challenge assays. Effect of SNP (20 mM and 30 mM) on growth kinetics of WT and ΔphoB KP.
(TIF)
In vitro inactivation assays. Growth inactivation assays using ciprofloxacin (0.005 µg/ml). The efflux pump inhibitors CCCP was used at a concentration of 10 µg/ml in the experiment. The mean values of three independent experiments have been used for plotting the graph.
(TIF)
Acknowledgments
We are highly thankful to our Director, CSIR-Institute of Microbial Technology (IMTECH), Chandigarh, for providing excellent facility to carry out this work. DNA sequencing and service facilities provided in IMTECH is highly appreciated. We are also grateful to Dr Jin-Town Wang, National Taiwan University Hospital for providing K. pneumoniae NTUH-K2044 and plasmids. We are extremely thankful to Dr. Kavita Babu, IISER, Mohali, India for giving C. elegans strain Bristol N2 and E. coli OP50 as a kind gift.
Footnotes
Competing Interests: The authors have declared that no competing interests exist.
Funding: The research has been supported by intramural funds from the Institute of Microbial Technology (IMTECH) (http://www.imtech.res.in/) and Department of Biotechnology (http://dbtindia.nic.in) (No.BT/01/1YBAl2009). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Glauert AM, Thornley MJ. The topography of the bacterial cell wall. Annu Rev Microbiol. 1969;23:159–198. doi: 10.1146/annurev.mi.23.100169.001111. [DOI] [PubMed] [Google Scholar]
- 2.Nikaido H. Porins and specific diffusion channels in bacterial outer membranes. J Biol Chem. 1994;269:3905–3908. [PubMed] [Google Scholar]
- 3.Schirmer T. General and specific porins from bacterial outer membranes. J Struct Biol. 1998;121:101–109. doi: 10.1006/jsbi.1997.3946. [DOI] [PubMed] [Google Scholar]
- 4.Hall MN, Silhavy TJ. Genetic analysis of the major outer membrane proteins of Escherichia coli. Annu Rev Genet. 1981;15:91–142. doi: 10.1146/annurev.ge.15.120181.000515. [DOI] [PubMed] [Google Scholar]
- 5.Achouak W, Heulin T, Pages JM. Multiple facets of bacterial porins. FEMS Microbiol Lett. 2001;199:1–7. doi: 10.1111/j.1574-6968.2001.tb10642.x. [DOI] [PubMed] [Google Scholar]
- 6.Buchanan SK. Beta-barrel proteins from bacterial outer membranes: structure, function and refolding. Curr Opin Struct Biol. 1999;9:455–461. doi: 10.1016/S0959-440X(99)80064-5. [DOI] [PubMed] [Google Scholar]
- 7.Nikaido H, Vaara M. Molecular basis of bacterial outer membrane permeability. Microbiol Rev. 1985;49:1–32. doi: 10.1128/mr.49.1.1-32.1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Davies J, Davies D. Origins and evolution of antibiotic resistance. Microbiol Mol Biol Rev. 2010;74:417–433. doi: 10.1128/MMBR.00016-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Podschun R, Ullmann U. Klebsiella spp. as nosocomial pathogens: epidemiology, taxonomy, typing methods, and pathogenicity factors. Clin Microbiol Rev. 1998;11:589–603. doi: 10.1128/cmr.11.4.589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Khanfar HS, Bindayna KM, Senok AC, Botta GA. Extended spectrum beta-lactamases (ESBL) in Escherichia coli and Klebsiella pneumoniae: trends in the hospital and community settings. J Infect Dev Ctries. 2009;3:295–299. doi: 10.3855/jidc.127. [DOI] [PubMed] [Google Scholar]
- 11.Wang H, Chen M, Xu Y, Sun H, Yang Q, et al. Antimicrobial susceptibility of bacterial pathogens associated with community-acquired respiratory tract infections in Asia: report from the Community-Acquired Respiratory Tract Infection Pathogen Surveillance (CARTIPS) study, 2009–2010. Int J Antimicrob Agents. 2011;38:376–383. doi: 10.1016/j.ijantimicag.2011.06.015. [DOI] [PubMed] [Google Scholar]
- 12.Daikos GL, Markogiannakis A. Carbapenemase-producing Klebsiella pneumoniae: might we still consider treating with carbapenems? Clin Microbiol Infect. 2011;17:1135–1141. doi: 10.1111/j.1469-0691.2011.03553.x. [DOI] [PubMed] [Google Scholar]
- 13.Tsai YK, Fung CP, Lin JC, Chen JH, Chang FY, et al. Klebsiella pneumoniae outer membrane porins OmpK35 and OmpK36 play roles in both antimicrobial resistance and virulence. Antimicrob Agents Chemother. 2011;55:1485–1493. doi: 10.1128/AAC.01275-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Martínez-Martínez L, Pascual A, Hernández-Allés S, Alvarez-Díaz D, Suárez AI, et al. Roles of beta-lactamases and porins in activities of carbapenems and cephalosporins against Klebsiella pneumoniae. Antimicrob Agents Chemother. 1999;43:1669–1673. doi: 10.1128/aac.43.7.1669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hernandez-Alles S, Alberti S, Alvarez D, Domenech-Sanchez A, Martinez-Martinez L, et al. Porin expression in clinical isolates of Klebsiella pneumoniae. Microbiology. 1999;145:673–679. doi: 10.1099/13500872-145-3-673. [DOI] [PubMed] [Google Scholar]
- 16.Garcia-Sureda L, Juan C, Domenech-Sanchez A, Alberti S. Role of Klebsiella pneumoniae LamB Porin in antimicrobial resistance. Antimicrob Agents Chemother. 2011;55:1803–1805. doi: 10.1128/AAC.01441-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kaczmarek FM, Dib-Hajj F, Shang W, Gootz TD. High-level carbapenem resistance in a Klebsiella pneumoniae clinical isolate is due to the combination of bla (ACT-1) beta-lactamase production, porin OmpK35/36 insertional inactivation, and down-regulation of the phosphate transport porin phoE. Antimicrob Agents Chemother. 2006;50:3396–3406. doi: 10.1128/AAC.00285-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Domenech-Sanchez A, Hernáandez-Alles S, Martinez-Martinez L, Benedi VJ, Alberti S. Identification and characterization of a new porin gene of Klebsiella pneumoniae: its role in beta-lactam antibiotic resistance. J Bacteriol. 1999;181:2726–2732. doi: 10.1128/jb.181.9.2726-2732.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Garcia-Sureda L, Domenech-Sanchez A, Barbier M, Juan C, Gasco J, et al. OmpK26, a novel porin associated with carbapenem resistance in Klebsiella pneumoniae. Antimicrob Agents Chemother. 2011;55:4742–4747. doi: 10.1128/AAC.00309-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wu KM, Li LH, Yan JJ, Tsao N, Liao TL, et al. Genome sequencing and comparative analysis of Klebsiella pneumoniae NTUH-K2044, a strain causing liver abscess and meningitis. J Bacteriol. 2009;191:4492–4501. doi: 10.1128/JB.00315-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Srinivasan VB, Vaidyanathan V, Mondal A, Rajamohan G. Role of the two component signal transduction system CpxAR in conferring cefepime and chloramphenicol resistance in Klebsiella pneumoniae NTUH-K2044. PLoS One. 2012;7:e33777. doi: 10.1371/journal.pone.0033777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gunn JS. Mechanisms of bacterial resistance and response to bile. Microbes Infect. 2000;2:907–913. doi: 10.1016/s1286-4579(00)00392-0. [DOI] [PubMed] [Google Scholar]
- 23.Coudeyras S, Nakusi L, Charbonnel N, Forestier C. A tripartite efflux pump involved in gastrointestinal colonization by Klebsiella pneumoniae confers a tolerance response to inorganic acid. Infect Immun. 2008;76:4633–4641. doi: 10.1128/IAI.00356-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Stevanin TM, Ioannidis N, Mills CE, Kim SO, Hughes MN, et al. Flavohemoglobin Hmp affords inducible protection for Escherichia coli respiration, catalyzed by cytochromes bo' or bd, from nitric oxide. J Biol Chem. 2000;46:35868–35875. doi: 10.1074/jbc.M002471200. [DOI] [PubMed] [Google Scholar]
- 25.Di Martino P, Cafferini N, Joly B, Darfeuille-Michaud A. Klebsiella pneumoniae type 3 pili facilitate adherence and biofilm formation on abiotic surfaces. Res Microbiol. 2003;154:9–16. doi: 10.1016/s0923-2508(02)00004-9. [DOI] [PubMed] [Google Scholar]
- 26.Raffa RG, Raivio TL. A third envelope stress signal transduction pathway in Escherichia coli. Mol Microbiol. 2002;45:1599–1611. doi: 10.1046/j.1365-2958.2002.03112.x. [DOI] [PubMed] [Google Scholar]
- 27.De Wulf P, Lin ECC. Cpx two-component signal transduction in Escherichia coli: excessive CpxR-P levels underlie CpxA phenotypes. J. Bacteriol. 2000;182:1423–1426. doi: 10.1128/jb.182.5.1423-1426.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pages JM, James CE, Winterhalter M. The porin and the permeating antibiotic: a selective diffusion barrier in Gram-negative bacteria. Nat Rev Microbiol. 2008;12:893–903. doi: 10.1038/nrmicro1994. [DOI] [PubMed] [Google Scholar]
- 29.Lamarche MG, Wanner BL, Crepin S, Harel J. The phosphate regulon and bacterial virulence: a regulatory network connecting phosphate homeostasis and pathogenesis. FEMS Microbiol Rev. 2008;32:461–73. doi: 10.1111/j.1574-6976.2008.00101.x. [DOI] [PubMed] [Google Scholar]
- 30.Hsieh YJ, Wanner BL. Global regulation by the seven-component Pi signaling system. Curr Opin Microbiol. 2010;13:198–203. doi: 10.1016/j.mib.2010.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wanner BL. Gene regulation by phosphate in enteric bacteria. J Cell Biochem. 1993;51:47–54. doi: 10.1002/jcb.240510110. [DOI] [PubMed] [Google Scholar]
- 32.Raffa RG, Raivio TL. A third envelope stress signal transduction pathway in Escherichia coli. Mol Microbiol. 2002;45:1599–1611. doi: 10.1046/j.1365-2958.2002.03112.x. [DOI] [PubMed] [Google Scholar]
- 33.De E, Basle A, Jaquinod M, Saint N, Mallea M, et al. A new mechanism of antibiotic resistance in Enterobacteriaceae induced by a structural modification of the major porin. Mol Microbiol. 2001;41:189–198. doi: 10.1046/j.1365-2958.2001.02501.x. [DOI] [PubMed] [Google Scholar]
- 34.Low AS, MacKenzie FM, Gould IM, Booth IR. Protected environments allow parallel evolution of a bacterial pathogen in a patient subjected to long-term antibiotic therapy. Mol Microbiol. 2001;42:619–630. doi: 10.1046/j.1365-2958.2001.02647.x. [DOI] [PubMed] [Google Scholar]
- 35.Bradford PA, Urban C, Mariano N, Projan SJ, Rahal JJ, et al. Imipenem resistance in Klebsiella pneumoniae is associated with the combination of ACT-1, a plasmid-mediated AmpC beta-lactamase, and the loss of an outer membrane protein. Antimicrob Agents Chemother. 1997;41:563–569. doi: 10.1128/aac.41.3.563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Crowley B, Benedí VJ, Doménech-Sánchez A. Expression of SHV-2 beta-lactamase and of reduced amounts of OmpK36 porin in Klebsiella pneumoniae results in increased resistance to cephalosporins and carbapenems. Antimicrob Agents Chemother. 2002;46:3679–3682. doi: 10.1128/AAC.46.11.3679-3682.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lee K, Yong D, Choi YS, Yum JH, Kim JM, et al. Reduced imipenem susceptibility in Klebsiella pneumoniae clinical isolates with plasmid-mediated CMY-2 and DHA-1 beta-lactamases co-mediated by porin loss. Int J Antimicrob Agents. 2007;29:201–206. doi: 10.1016/j.ijantimicag.2006.09.006. [DOI] [PubMed] [Google Scholar]
- 38.Yum JH, Kim S, Lee H, Yong D, Lee K, et al. Emergence and wide dissemination of CTX-M-type ESBLs, and CMY-2- and DHA-1-type AmpC beta-lactamases in Korean respiratory isolates of Klebsiella pneumoniae. J Korean Med Sci. 2005;20:961–965. doi: 10.3346/jkms.2005.20.6.961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mena A, Plasencia V, García L, Hidalgo O, Ayestarán JI, et al. Characterization of a large outbreak by CTX-M-1-producing Klebsiella pneumoniae and mechanisms leading to in vivo carbapenem resistance development. J Clin Microbiol. 2006;44:2831–2837. doi: 10.1128/JCM.00418-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Moller JK. Monitoring antimicrobial drug resistance in hospital microorganisms. Definition of problems and methods. Dan Med Bull. 1990;37:263–274. [PubMed] [Google Scholar]
- 41.Hu WS, Chen HW, Zhang RY, Huang CY, Shen CF. The expression levels of outer membrane proteins STM1530 and OmpD, which are influenced by the CpxAR and BaeSR two-component systems, play important roles in the ceftriaxone resistance of Salmonella enterica serovar Typhimurium. Antimicrob Agents Chemother. 2011;55:3829–3837. doi: 10.1128/AAC.00216-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Russell AD. Biocide use and antibiotic resistance: the relevance of laboratory findings to clinical and environmental situations. Lancet Infect Dis. 2003;3:794–803. doi: 10.1016/s1473-3099(03)00833-8. [DOI] [PubMed] [Google Scholar]
- 43.Karatzas KA, Webber MA, Jorgensen F, Woodward MJ, Piddock LJ, et al. Prolonged treatment of Salmonella enterica serovar Typhimurium with commercial disinfectants selects for multiple antibiotic resistance, increased efflux and reduced invasiveness. J Antimicrob. Chemother. 2007;60:947–955. doi: 10.1093/jac/dkm314. [DOI] [PubMed] [Google Scholar]
- 44.Krachler AM, Woolery AR, Orth K. Manipulation of kinase signaling by bacterial pathogens. J Cell Biol. 2011;195:1083–1092. doi: 10.1083/jcb.201107132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Begic S, Worobec EA. Regulation of Serratia marcescens ompF and ompC porin genes in response to osmotic stress, salicylate, temperature and pH. Microbiology. 2006;152:485–491. doi: 10.1099/mic.0.28428-0. [DOI] [PubMed] [Google Scholar]
- 46.Pratt LA, Hsing W, Gibson KE, Silhavy TJ. From acids to osmZ: multiple factors influence synthesis of the OmpF and OmpC porins in Escherichia coli. Mol Microbiol. 1996;20:911–917. doi: 10.1111/j.1365-2958.1996.tb02532.x. [DOI] [PubMed] [Google Scholar]
- 47.Nishino K, Nikaido E, Yamaguchi A. Regulation and physiological function of multidrug efflux pumps in Escherichia coli and Salmonella. Biochim Biophys Acta. 2009;1794:834–843. doi: 10.1016/j.bbapap.2009.02.002. [DOI] [PubMed] [Google Scholar]
- 48.Fang CT, Chuang YP, Shun CT, Chang SC, Wang JT. A novel virulence gene in Klebsiella pneumoniae strains causing primary liver abscess and septic metastatic complications. J Exp Med. 2004;199:697–705. doi: 10.1084/jem.20030857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Shemesh M, Kolter R, Losick R. The biocide chlorine dioxide stimulates biofilm formation in Bacillus subtilis by activation of the histidine kinase KinC. J Bacteriol. 2010;192:6352–6356. doi: 10.1128/JB.01025-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hennequin C, Forestier C. oxyR, a LysR-type regulator involved in Klebsiella pneumoniae mucosal and abiotic colonization. Infect Immun. 2009;77:5449–5457. doi: 10.1128/IAI.00837-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Clinical and Laboratory Standards Institute. Performance standards for antimicrobial susceptibility testing. CLSI M100-S20U. Clinical and Laboratory Standards Institute. Wayne, PA. 2010.
- 52.Bialek S, Lavigne JP, Chevalier J, Marcon E, Leflon-Guibout V, et al. Membrane efflux and influx modulate both multidrug resistance and virulence of Klebsiella pneumoniae in a Caenorhabditis elegans model. Antimicrob Agents Chemother. 2010;54:4373–4378. doi: 10.1128/AAC.01607-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Moy TI, Ball AR, Anklesaria Z, Casadei G, Lewis K, et al. Identification of novel antimicrobials using a live-animal infection model. Proc Natl Acad Sci USA. 2006;103:10414–10419. doi: 10.1073/pnas.0604055103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Altschul SF, Madden TL, Schäffer AA, Zhang J, Zhang Z, et al. Gapped BLAST and PSI-BLAST: a new generation of protein database search programs. Nucleic Acids Res. 1997;25:3389–3402. doi: 10.1093/nar/25.17.3389. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Oxidative stress assays. Survival of K. pneumoniae and ΔkpnO strains upon exposure to oxidative stress with 0.07894 mM, 0.7894 mM, 1.5788 mM, 2.3682 mM and 3.1576 mM. After 1 h of treatment with 0.07894 mM hydrogen peroxide, only 47% of ΔkpnO cells survived in comparison to 95% of the wild-type cells. The differences between the mutant and its parental wild-type strain are statistically significant (P<0.05) for all H2O2 concentrations. The standard errors of the means from three independent assays are shown.
(TIF)
Nitrostative challenge assays. Growth pattern of WT, ΔkpnO in the presence of sodium nitrite. In the presence of 30 mM NO donor, growth kinetics of ΔkpnO cells was ∼7.0 fold lower as compared to WT at pH 7.0.
(TIF)
Growth inactivation assays. Inactivation assays using ciprofloxacin (0.005 µg/ml). The efflux pump inhibitors CCCP was used at a concentration of 10 µg/ml in the experiment. The mean values of three independent experiments have been used for plotting the graph.
(TIF)
Nitrostative challenge assays. Effect of SNP (20 mM and 30 mM) on growth kinetics of WT and ΔphoB KP.
(TIF)
In vitro inactivation assays. Growth inactivation assays using ciprofloxacin (0.005 µg/ml). The efflux pump inhibitors CCCP was used at a concentration of 10 µg/ml in the experiment. The mean values of three independent experiments have been used for plotting the graph.
(TIF)