In this issue of The EPMA Journal, we have collected contributions from 11 countries that cover several geopolitical regions in Europe, Asia and USA; the contributions provide expert opinions on timely and highly-relevant topics:
➢ Overview of current healthcare organisation and future outlook
➢ Health promotion and work
➢ The role of laboratory medicine in healthcare
➢ Economic concerns: personalised medicine and comparative effectiveness of research in an era of fixed budgets.
Previous specialised issues of The EPMA Journal 2010 dedicated to PPPM in diabetes, neurodegenerative diseases and cancer have created a robust platform to discuss the topic which the current journal-issue is dedicated to, namely, an overview of healthcare. On a global scale, this is a unique concept presenting
➢ comprehensive review of historic, cultural, demographic, ethnic, socio-economical, political, and other aspects which contribute to creation of current healthcare systems
➢ comparisons of data / information both from Europe and worldwide in order to share issue-related experiences and to learn from each other about advantages and disadvantages of single healthcare systems.
The main objectives of these efforts are to mark the stakeholders in the field, to consolidate professional groups and to prepare expert recommendations of how to optimise approaches for cost-effective personalisation of healthcare.
In this issue we have collected the expert opinion from 11 countries that cover several regions in Europe, Asia and USA, as demonstrated in Fig. 1:
➢ Austria: Kurt Krapfenbauer (EPMA-Board of Directors) and Dietmar Thurnher (National Representative of EPMA in Austria) with co-authors; two contributions—1st article “The role of laboratory medicine in healthcare: quality requirements of immunoassays, standardisation and data management in prospective medicine” and 2nd article “Economic concerns about global healthcare in lung, head and neck cancer: meeting the economic challenge of predictive, preventive and personalized medicine”
➢ Bavaria / Germany: Kneginja Richter (Representative of EPMA in Bavaria, Germany); the contribution “Health promotion and work: prevention of shift work disorders in companies”
➢ Bulgaria: Dimiter Dimitrov (National Representative of EPMA in Bulgaria); the contribution “Current healthcare in Bulgaria: time for predictive diagnostics and preventive medicine”
➢ Germany: Andrea Döring and Paul Friedemann, (National Representative of EPMA in Germany); the contribution “The German healthcare system”
➢ Macedonia: Nikola Kamcev (Representative of the EPMA Institutional member) and Kneginja Richter (National Representative of EPMA in Macedonia); the contribution “Health Organization in Republic of Macedonia—the place of preventive health care in the medical health system: advantages and disadvantages”
➢ Serbia & Montenegro: Dragica Radojkovic (National Representative of EPMA in Serbia & Montenegro) and co-author; the contribution “Healthcare in Serbia in transition period”
➢ Slovak Republic: Marko Kapalla (National Representative of EPMA in Slovakia) with co-authors; the contribution “An overview of the healthcare system in the Slovak Republic”
➢ Taiwan: Willie Sai Ho Chan (National Representative of EPMA in Taiwan); the contribution “Taiwan’s healthcare report 2010”
➢ Turkey: Munis Dundar (Director of the National EPMA-Board in Turkey responsible for Genetic Research & Contacts to Governmental Institutions), with co-authors; the contribution “Healthcare in overview of Turkey“
➢ UK: Konstantina Grosios (National Representative of EPMA in UK) and Peter Gahan (Director in the EPMA-Board responsible for Education) with a co-author; the contribution “Overview of healthcare in the UK”
➢ USA: Paul Brown; the contribution “Personalized medicine and comparative effectiveness research in an era of fixed budgets”.
Fig. 1.
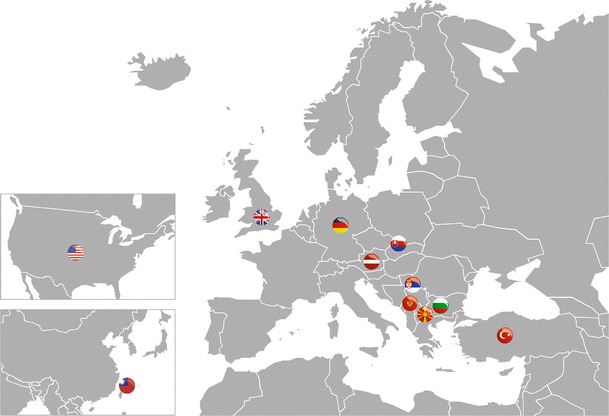
The map demonstrates corresponding geopolitical designation of contributions published with this journal-issue. Corresponding states / contributors are listed below in the alphabetical order
An excellent review-article from the United Kingdom by K. Grosios et al. overviews the governmental 2010 White Paper “Equity and excellence: Liberating the National Health System”, which announced a strategy on how to “create a more responsive, patient-centred National Health System, which achieves outcomes that are among the best in the world” [K. Grosios et al., “Overview of healthcare in the UK”]. The article gives a statement on current PPPM-elements in the national healthcare of the UK. This information should serve as the basis for a comparative analysis in the future to understand, whether current health programmes work effectively.
Principles of the German healthcare system are clearly defined in the excellent review by A. Döring and P. Friedemann, with a particular focus on the payment profile for medical services. Health insurance models are analysed across social layers as the decisive factor in the structure, content and quality of medical services in the national healthcare system [A. Döring and P. Friedemann, “The German healthcare system”]. The article identifies potential stakeholders, who are essentially involved in the practical implementation of personalised medicine.
An interesting article, prepared by the National EPMA-Representative in Slovakia, M. Kapalla (with co-authors) stresses the important mission of governmental institutions in creating and implementing PPPM-related healthcare programmes at the national level. This article indicates the importance of their implementation in the European context, particularly in accordance with population needs and well in consensus with professionals involved in the field [M. Kapalla et al., “An overview of the healthcare system in the Slovak Republic”].
An excellent review-article has been prepared by W. S. H. Chan, updating the current healthcare system in Taiwan with dynamic developments and concomitant alterations [W. S. H. Chan “Taiwan’s healthcare report 2010”]. This article overviews healthcare expenditure around the globe and provides a comparative analysis of investments, corresponding medical services and achievements of several national healthcare systems, including countries in Asia, Europe and North America. Evaluation criteria estimating the efficiency of healthcare systems are also discussed in detail.
Due to its geopolitical location between Asia and Europe, Turkey demonstrates country-specific issues of its healthcare system. The matter is well reviewed in this journal-issue by M. Dundar with co-authors, who identify demographic particularities of the Turkish population, which the local healthcare system should be able to account. It also details corresponding national programmes under review and development according to the Vision 2020 and 2040 [M. Dundar et al., “Healthcare in overview of Turkey”].
Historic events that have occurred in the last two decades in the region of former Yugoslavia have had a tremendous impact on the current situation in regional single healthcare systems. This is clearly demonstrated with two review-articles from the area, by experts from Macedonia [N. Kamcev et al., “Health Organization in Republic of Macedonia—the place of preventative health care in the medical health system: advantages and disadvantages”] and Serbia [Z. Vlahovic and D. Radojkovic, “Healthcare in Serbia in transition period”]. The dramatic socio-economical re-organisation of the region after 1989 led to step-by-step changes in the healthcare model, namely
➢ from the concept of “national healthcare” with free medical services available for everyone
➢ through the intermediate “period of transition” beginning in 1991 with the dominating “private and market” concept
➢ to establishing of the current concept of sustainable healthcare system created on the basis of public and private property and organised with three levels, namely primary, secondary and tertiary healthcare.
A similar process of the re-organisation in the healthcare sector can be currently observed in the countries that recently entered the European Union. A representative review-article from Bulgaria has been prepared by D. Dimitrov, entitled “Current healthcare in Bulgaria: time for predictive diagnostics and preventive medicine”. So-called “medical tourism” is a new phenomenon in the national healthcare system, which drives the development of earmarked medical services.
In spite of the individuality of each national healthcare system, there is a common need to establish innovative programmes for targeted prevention and individualised treatment of chronic pathologies of epidemic scales, such as obesity and diabetes. The healthcare promotion obviously needs a supranational-coordinated action of global organisations, in harmony with corresponding national programmes.
With regards to the potential effect on employees of implementing innovative programmes for cost-effective health promotion, the importance of predictive diagnostics should be recognised by professional alliances, companies and employers in general. An excellent article is published in this journal-issue by K. Richter with co-authors, clearly demonstrating the serious consequences of shift-work sleep disorder. There is an urgent need for specialised educational programmes and corresponding guidelines that should introduce appropriate diagnostic approaches and improve the knowledge of both employers and jobholders in issue-related companies and organisations [K. Richter et al., “Health promotion and work: prevention of shift work disorders in companies”]. The resultant socio-economical benefits from these programmes are likely to be extremely high. Complementary to this topic, there is an important article dedicated to the elaboration of standards and data management in prospective medicine, which would lead to clearer guidelines regulating analytical validation strategies as discussed by T. Waerner and co-authors [T. Waerner et al., “The role of laboratory medicine in healthcare: quality requirements of immunoassays, standardisation and data management in prospective medicine”].
One of the central aspects in the performance of personalised medicine is the economic challenge of implementing cost-effective treatments and maintaining long-term investment in predictive diagnostics, followed by targeted preventive measures, as compared to the acute costs of late interventional medicine to treat manifested pathologies. This comprehensive subject is well analysed by two review-articles in this journal-issue. Ch. Ausweger (with co-authors) argues for the economical benefits of early and predictive in vitro diagnostics, especially in the area of individualised lung, head and neck cancer treatments [Ch. Ausweger et al., “Economic concerns about global healthcare in lung, head and neck cancer: meeting the economic challenge of predictive, preventive and personalized medicine”]. P. Brown overviews the potential and limitations of comparative effectiveness research to calculate effectiveness of PPPM, versus that of late medical intervention approaches [P. Brown, “Personalized medicine and comparative effectiveness research in an era of fixed budgets”]. In order to be widely adopted by stakeholders in routine clinical practice, innovative approaches to personalised medicine should be convincing in their cost effectiveness as well as short- and long-term financial viability.
How do we estimate the overall impact of personalised medicine and adopt innovative approaches in healthcare systems, whilst promoting early / predictive diagnostics, targeted preventive measures and individualised patient treatment on a global scale? The topic is discussed in detail in this issue, using innovative concept of data presentation created by The EPMA Journal to provide excellent examples of current healthcare systems, with consideration of possible scenarios and perspectives of future developments.
Vincenzo Costigliola
graduated in Medicine at the Naples University in Italy;
Since 1972—Family Practice;
Chief of Medical service in Italian Navy (Outpatients clinic, legal, occupational and preventive medicine);
Chief of the Internal Medicine Service; Chief of Medical Staff on Military ships;
Medical advisor: NATO; WEU (Western European Union) in Brussels, attached to the SHAPE (Supreme Headquarters Allied Powers Europe)
• President of EMA (European Medical Association)
• President of IRMA (International Rescue Medicine Association)
• President of EDA (European Depression Association)
• President of EPMA (European Association for Predictive, Preventive and Personalised Medicine) http://www.epmanet.eu/