Abstract
In Japan, overweight/obesity in adults defined as a body mass index of 25 kg/m2 or over has roughly doubled among middle-aged men over the past few decades. In parallel with a population rightward shift in the degree of obesity, the proportion of hypertension attributed to overweight has increased. There is an indication that the incidence of ischemic stroke and coronary heart disease remains stable or has been increasing among men. These facts indicate that the relative importance of cardiovascular diseases (CVD) risk factors may have changed. Although it was confirmed at an individual level that the degree of obesity was positively associated with CVD incidence, there is a sizeable proportion of individuals who are at an increased CVD risk state without being overweight/obese in today’s Japan. Thus, further implementation and promotion of activities are needed to bring about meaningful changes in the obesity trend in communities that are harmonized with other domains of CVD prevention activities.
Keywords: Cardiovascular disease, Obesity, Hypertension, Japan, Epidemiology, Prevention
Introduction
Stroke mortality had been much higher in Japan compared with other industrialized populations until it declined steeply between 1965 and 1990 due mainly to a decrease in the level of blood pressure [1], and by improvement in nutritional status [2]. At the same time, coronary heart disease (CHD) mortality remains as low as one-third to one-fifth of that in the United States [3] even with the westernization of lifestyles that has brought about increases in blood cholesterol levels and the degree of obesity. However, there are some indications that the decline of stroke incidence decelerated or stopped [4, 5], and CHD incidence increased [6, 7]. In this review, we first describe the population trend in the degree of obesity as measured by the body mass index (BMI), and review prospective cohort studies that reported associations of obesity measures and metabolic syndrome (MetS) with cardiovascular diseases (CVD) in Japanese. We then review literature that reported secular and geographical trends in the incidence of CVD subtypes, including ischemic stroke subtypes and percutaneous coronary intervention (PCI) to help our understanding of shifts of CVD risk factors and their determinants, including obesity.
Predictive diagnostics, targeted preventive measures and personalized medicine (PPPM) is a new paradigm proposed by the European Association for Predictive, Preventive and Personalised Medicine [8]. For the primary prevention of CVD, population-based prevention aligned with identification of and intervention to high-risk individuals who have high estimated CVD risk, are essential. In order to enable these activities, cycles of research, formation and implementation of guideline and regulation, and evaluation are necessary. To efficiently and effectively facilitate this process, communication among medical and public health professionals is especially important [9].
From a PPPM perspective, we derive conclusions that implementation and promotion of activities for bringing about meaningful changes in the obesity trend are essential. However, this effort should be harmonized with other domains of CVD prevention activities, such as measures against smoking and salt intake.
Obesity trend in Japan
In Japan, obesity in adults defined as a BMI of 30 kg/m2 or over [10] has roughly doubled over the past few decades in men, although the absolute prevalence is only 3% [11] in contrast to much higher prevalence in OECD countries (16%, average) [12] or in the United States (34%) [13]. If obesity is defined by a BMI greater than or equal to 25 kg/m2 (Japanese criterion) [14], 28.6% of men and 20.6% of women were obese in 2008. The average BMIs have been increasing consistently since 1950 except for younger women [11, 15] (Figs. 1, 2). Namely, the average BMI of women aged 30–39 and that of women aged 40–49 have been decreasing from 1975 to 1985, respectively. However, if aging-related changes of BMI by birth cohorts are compared, aging during middle age seems to be related to weight gain on average even in younger generation women (born in 1960’s), who weighed less than the older generation at a younger age (30–39), but gained thereafter at least through their sixties (Figs. 3, 4). It is noteworthy that younger generation men enter middle age with a higher BMI, and they experience a continuous increase of BMI. These observations are partly supported by a longitudinal analysis of repeatedly-measured body weight among the same individuals [16].
Fig. 1.

Secular changes in the mean body mass index in Japanese men, National Health and Nutritional Survey in Japan 1950–2006
Fig. 2.

Secular changes in the mean body mass index in Japanese women, National Health and Nutritional Survey in Japan 1950–2006
Fig. 3.
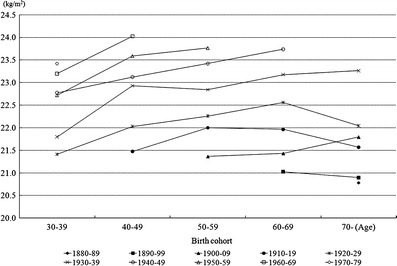
Changes in the mean body mass index with age by birth cohort of Japanese men, National Health and Nutritional Survey in Japan 1950–2005
Fig. 4.
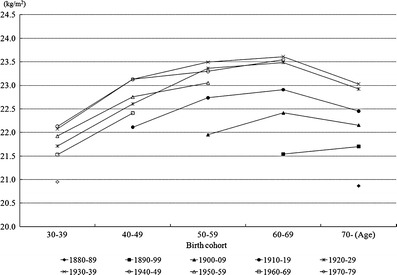
Changes in the mean body mass index with age by birth cohort of Japanese women, National Health and Nutritional Survey in Japan 1950–2005
Urban and rural difference of obesity trend
It was reported that the mean BMI of men in an urban community has increased from 22.5 kg/m2 in the earliest survey (1963–1966) to 23.8 kg/m2 in the last survey (2000–2003) [7] (Table 1). The mean BMI of women in an urban community, however, decreased from 23.4 to 22.8 kg/m2 during the same period. Contrarily, the mean BMI increased in both men and women in a rural community (22.6 to 24.0 kg/m2 in men and 23.1 to 24.3 kg/m2 in women). In the Hisayama Study of a suburban community, the mean BMI also increased from 21.3 kg/m2 in 1961 to 23.5 kg/m2 in 2002 in men and from 21.7 to 22.9 kg/m2 in women [17]. A national survey also found that prevalence of overweight (BMI ≥25 kg/m2) among men increased regardless of the residential areas, whereas that among women aged 50 or over in urban areas has also been decreasing [18].
Table 1.
Trends in age-adjusted mean body mass index and systolic blood pressure in the Hisayama and the Akita-Osaka Studies
| Men | Women | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1960’s | 1970’s | 1980’s | 1990’s | 2000’s | 1960’s | 1970’s | 1980’s | 1990’s | 2000’s | |
| Body mass index (kg/m2) | ||||||||||
| Hisayamaa | 21.3 | 21.7 | 22.8 | NA | 23.5 | 21.7 | 22.5 | 22.9 | NA | 22.9 |
| Akitab | 22.6 | 23.1 | 22.9 | 23.2 | 24.0 | 23.1 | 24.0 | 23.9 | 23.9 | 24.3 |
| Osakab | 22.5 | 22.3 | 22.7 | 23.3 | 23.8 | 23.4 | 22.9 | 22.6 | 22.9 | 22.8 |
| Systolic blood pressure (mmHg) | ||||||||||
| Hisayamaa | 162 | 157 | 151 | NA | 148 | 163 | 161 | 154 | NA | 149 |
| Akitab | 150 | 141 | 136 | 133 | 132 | 142 | 135 | 132 | 129 | 129 |
| Osakab | 135 | 135 | 132 | 131 | 132 | 135 | 130 | 130 | 129 | 128 |
| Diastolic blood pressure (mmHg) | ||||||||||
| Hisayamaa | 91 | 90 | 87 | NA | 89 | 88 | 87 | 83 | NA | 86 |
| Akitab | 87 | 86 | 85 | 83 | 86 | 83 | 81 | 80 | 79 | 81 |
| Osakab | 80 | 81 | 80 | 84 | 85 | 80 | 79 | 78 | 80 | 80 |
aData for Hisayama was from Kubo et al. [17]
bData for Akita and Osaka were from Kitamura et al. [7]
NA indicates not available.
Mean values of the Hisayama Study were among hypertensive subjects (systolic blood pressure ≥140 mmHg or diastolic blood pressure ≥90 mmHg, or current use of antihypertensive agents)
Measurements were carried out in 1961, 1974, 1988, and 2002 in the Hisayama Study, and in periods 1964–66, 1976–79, 1984–87, 1992–95, and 2000–03 in the Akita-Osaka Study
Association of degree of obesity with blood pressure
In the same studies that reported secular BMI changes in rural/suburban and urban men and women, mean blood pressure (BP) changes were also described [7, 17]. Although systolic BP decreased in both men and women from either rural/suburban or urban communities, the magnitude of the decrease was more prominent in rural/suburban men and women and in urban women than in urban men. Further, diastolic BP increased in urban men. These observations imply the existence of two sets of factors with opposite directions; one characteristic of previous rural areas and the other more typical of recent urban areas, especially, men. Indeed, hypertension without being overweight used to constitute a majority of the hypertension cases in rural communities in 1960’s, but it decreased significantly by the 1980’s [19]. This change was accompanied by increases in overweight and also in the proportion of hypertension among the overweight. Furthermore, a correlation between BMI and diastolic BP was not present in the 1960’s in rural men aged 40 to 49; however, it emerged in the 1970’s and became stronger in the 1980’s. In contrast, the prevalence of hypertension in urban men has been increasing since the 1990’s [20]. This is partly due to a continuous increase in the prevalence of overweight, but the authors have suggested other factors besides obesity such as mental stress, increased workload and sleep deprivation since the increase has also been observed in individuals without overweight.
Although further nationwide studies are warranted, hypertension attributed to overweight/obesity is increasing in Japan. Prospective studies have also confirmed the associations [21–23]. Since it was reported that the strongest risk factor for the development of hypertension was a higher BMI, and that 40% of new hypertension cases was attributed to overweight/obese in US women with 66% of women being overweight/obesity [24], it would be reasonable to take measures against overweight/obesity as one way to prevent hypertension in Japan as well.
Stroke and ischemic stroke subtypes
Ischemic stroke consists of three major subtypes with different etiologies: lacunar, nonlacunar thrombotic (atherothrombotic), and cardioembolic. The underlying vascular or non-vascular pathophysiologies of each subtype differ, such as lipohyalinosis and microatheroma for lacunar stroke, or atherosclerosis for atherothrombotic stroke. Intracerebral hemorrhage (ICH) is also characterized by lipohyalinosis [25]. Lipohyalinosis is arteriosclerosis of the arteriole, and characterized by degeneration of the media of small arteries with replacement of vascular muscle by lipid deposits and collagen (sclerosis) and loss of structural integrity of the vessel wall [26]. Therefore, risk factors for lacunar stroke and ICH overlap, among which hypertension is the most important [27]. The rapid decrease of stroke mortality in Japan since 1965 can be attributed to the decrease in ICH [5], which is due to improvement in hypertension control, the downward shift of population blood pressure distribution and also to improvement in nutritional status manifested as an increase in blood cholesterol level [28]. It was also hypothesized that ischemic stroke subtypes may be shifting from lacunar to atherothrombotic stroke predominance [4, 17], as observed in Western populations [29]. In the Hisayama Study, there was a relative increase of atherothrombotic infarction (22% to 32%) and decrease of lacunar infarction (65% to 41%) in men, although the overall stroke incidence rate decreased from 8.7 in men and 4.3 in women per 1,000 person-years in the first cohort (1961–1973) to 3.9 in men and 2.6 in women in the third cohort (1988–2001) [17]. The proportion of lacunar stroke in an urban community was similar [30] to that in the Hisayama Study (50% to 60% in both men and women), but this study did not find a similar secular trend.
These rapid (about 30-year) trends indicate changes in environment and behavioral factors that would have brought shifts in the risk factors [19]. As stated earlier, overweight/obesity is attributed more to the development of hypertension [19, 20, 31]. Overweight/obesity has other metabolic impacts such as diabetes. Since diabetes is a significant risk factor for all the ischemic stroke subtypes [29], the current overweight/obesity trend may increase the relative importance of diabetes and other metabolic disorders in the development of stroke and its subtypes in the Japanese population [32, 33].
Associations of obesity measures with ischemic stroke
Findings on the associations of obesity measures with ischemic stroke from individual cohort studies may seem inconsistent (Table 2) with null [34–36], positive association only in women [37–40], and positive association only in men [41]. The reasons for the inconsistency are not clear due to differences in sample sizes, obesity measures and the references used, or covariates in the statistical models; however, baseline years of the studies with null findings are generally old (1960’s to 1970’s). Recently, a pooling project reported a meta-analysis finding based on individual participant data from 16 existing high-quality prospective cohort studies in Japan comprising both rural and urban areas [42]. In this prospective study with 1,113 incident strokes, hazard ratios (HRs) for total stroke, cerebral infarction, and ICH of men with BMI 27.0 kg/m2 or greater were 1.80 (95% confidence interval: 1.31–2.47), 1.86 (1.28–2.69), and 2.19 (1.10–4.38) compared to those with BMI less than 21.0 kg/m2. The respective values in women were 1.64 (1.24–2.16), 1.68 (1.16–2.43), and 1.75 (1.01–3.05). These associations, especially of ICH, were found to be mediated by systolic BP. Thus, it is plausible that BMI is positively associated with cerebral hemorrhage and infarction, and that overweight/obesity increases stroke risk partly through the elevation of BP. Yet, it is still unknown why earlier studies did not find a significant association between BMI and stroke incidence. Recently, the population attributable fraction (PAF) of normal and higher BP in reference to optimal BP (systolic BP <120 mmHg and diastolic BP <80 mmHg) for stroke incidence [43] were reported to have decreased from the earliest cohort initiated in the 1960’s to the latest cohort started in the 1980’s, and which were considered to suggest an increase in the contribution of other, possibly obesity-related, factors [44]. Indeed, PAF of obesity to cerebral infarction increased gradually from 6% in the first cohort to 9% in the third cohort in the Hisayama Study, although the statistical significance of the difference was not indicated in this study [17]. Since obesity is associated with a wide range of CVD risk factors, positive associations between obesity measures and each ischemic stroke subtype were also reported from the Atherosclerosis Risk in the Communities Study consisting of African-Americans and Caucasians in four US communities [45]. Collectively, avoidance of obesity offers the potential of reducing stroke in Japan.
Table 2.
Cohort studies reporting associations of obesity measures with cardiovascular diseases in Japanese
| Study | Study period | Population | Endpoint | Findings |
|---|---|---|---|---|
| Hisayama Study (Yonemoto et al., 2010) [41] | 1988–2000 | 2,421 residents in a suburban community aged 40–79 | Stroke (107 cerebral infarction and 51 ICH) | BMI ≥23.0 kg/m2 was associated with increased CI incidence only in men compared with BMI <21.0 kg/m2. The association was independent of mediators including systolic blood pressure, ECG abnormalities, and diabetes. |
| Hisayama Study (Tanizaki et al., 2000) [40] | 1961–1993 | 1,621 residents in a suburban community aged 40 or over | Cerebral infarction subtypes (298 cerebral infarction cases, 56% lacunar) | Continuous BMI was positively associated with lacunar stroke incidence only in women independent of age, systolic blood pressure and ECG-LVH. |
| JPHC Study (Chei et al., 2008) [23] | 1990–2001 | 43,235 men and 47,444 women aged 40–69 living in nine administrative areas each covered by a public health center | CHD (399 in men and 119 in women) | Compared with BMI 23.0–24.9 kg/m2, BMI ≥30.0 kg/m2 was associated with higher incidence of CHD only in men in age- and multivariate-adjusted models. |
| JPCH Study (Saito et al., 2010) [37] | 1990–2005 | 32,847 men and 38,875 women aged 40–69 living in nine areas | Total stroke (1,181 in men and 838 in women) | BMI was positively associated with cerebral infarction and ICH incidence only in women. The associations were independent of histories of hypertension and diabetes. |
| Stroke subtypes (1,143 cerebral infarction, 616 ICH and 251 subarachnoid hemorrhage) | ||||
| Suita Study (Furukawa et al., 2010) [38] | 1989–2005 | 5,474 residents in urban communities aged 30 to 79 | CVD (207 strokes and 133 myocardial infarctions) | Waist circumference 84 cm or greater (top quartile) was associated with increased stroke incidence only in women compared with the lowest quartile (waist circumference <70 cm). |
| JALS (Yatsuya et al., 2010) [42] | Baseline year ranged from 1985 to 1999 | Meta-analysis of 16 cohorts using individual data (n = 45,235, ages 40 to 89). 82.7 % of the participants were from communities and 17.3 from work-site. | CVD | Incidence of cerebral infarction and ICH were positively associated with BMI in both men and women. Most BMI association with stroke incidence was explained by systolic blood pressure. BMI was positively associated with myocardial infarction only in men. The association was not totally explained by total cholesterol and systolic blood pressure. |
| Total strokes (n = 1,113) | ||||
| Cerebral infarction (n = 725) ICH (n = 229) | ||||
| Myocardial infarctions (n = 190) | ||||
| CIRCS (Iso et al., 2007) [39] | 1975–2001 | 9,087 residents in five communities aged 40 to 69. | Ischemic heart disease (n = 116) | Overweight (BMI ≥25.0 kg/m2) was associated with ischemic heart disease in men and cerebral infarction in women. The associations were not independent of confounding variables and serum total cholesterol. |
| (baseline year varies by communities) | Cerebral infarction (n = 256) | |||
| Shibata Study (Nakayama et al., 1997) [35] | 1977–1992 | 2,302 residents in a rural community aged 40 or over | Total stroke (n = 142) | There were no significant associations between relative weight and cerebral infarction and ICH incidence (insignificant positive association). |
| Cerebral infarction (n = 76) | ||||
| ICH (n = 27) | ||||
| Taisho Study (Tanaka et al., 1982) [34] | 1967–1977 | 772 men and 901 women who lived in a rural community aged 40 or over | Total stroke (n = 115) | There were no significant associations between relative weight and cerebral infarction and ICH incidence (insignificant inverse association). |
| Cerebral infarction (n = 81) | ||||
| ICH (n = 30) | ||||
| Honolulu Heart Program (Curb and Marcus, 1991) [36] | 1965–1985 | 7,585 men of Japanese ancestry living in Hawaii aged 45–65 | CHD and stroke | BMI was associated with CHD incidence in both hypertensive and nonhhpertensive men. BMI was not associated with stroke incidence in either hypertensive or nonhypertensive men. |
| Ni-Hon-San Study (Robertson et al., 1977) [49] | 1968–1970 (Hawaii) | 1,963 residents in Japan and 7,705 in Hawaii aged 45–68 | CHD (n = 47 in Hawaii and 22 in Japan) | Relative weight was associated with CHD in men in Hawaii but not in men in Japan. |
| 1965–1972 (Japan) |
Increasing trend of CHD in middle-aged urban men
In the Akita-Osaka Study, clinical data on PCI have also been collected since 1980, and a significant increase in the incidence of CHD was observed between the periods 1980 to 1987 and 1996 to 2004 among urban (Osaka) middle-aged men [7]. Age-adjusted incidence of myocardial infarction increased from 45 per 100,000 person-years in the 1960’s to 90 in the last survey period between 1996 and 2003. CHD including PCI increased from 56 per 100,000 person-years in the 1980’s to 127 in the aforementioned last survey period. A previous autopsy study revealed that the pathology of myocardial infarction among urban men included a larger infarction associated with hypercholesterolemia-derived atherosclerosis of the coronary arteries as observed in Western populations compared to that found in rural men, which was smaller and disseminated infarction associated with hypertension-derived atherosclerosis of coronary arteries [46]. Therefore, the increase of CHD among middle-aged urban men from the 1980s could be due to a concurrent increase in mean total cholesterol level and BMI. AMI incidence rates in rural/suburban men were also reported to have increased in the Takashima AMI registry from 66.5 per 100,000 person-years in 1990–92 to 100.7 in 1999 to 2001 [47]. In the Hisayama Study, however, CHD incidence was shown to be constant from the first to the third cohort for both men and women [48], except in men aged 80 or over who experienced a linear increase (statistical significance of the trend was not indicated in this study).
Associations of obesity measures with CHD
Due to the small number of incidents in women, most previous studies in Japan did not find an association of the degree of obesity with the CHD incidence in women (Table 2). In the Ni-Hon-San Study, relative weight was not associated with CHD; however, the number of CHD cases was very small (n = 22 in Japan) [49]. Later studies generally found positive associations between BMI and CHD in men. BMI was positively associated with CHD in the Honolulu Heart Program [36]. BMI ≥25 kg/m2 was associated with an increased incidence of ischemic heart disease in men in the CIRCS Study [39]. BMI ≥30 kg/m2 was associated with an increased incidence of CHD compared to those with BMI 23.0–24.9 kg/m2 in the JPHC Study [23]. In the aforementioned pooling project of existing cohort studies, the association in men was confirmed: compared to those with a BMI of less than 21.0 kg/m2, HR for MI of men with a BMI of 27.0 or greater was 2.84 (1.52–5.29) and that of women was 1.13 (0.47–2.74) [42]. Further, adjustment for total cholesterol, systolic BP, high-density lipoprotein cholesterol, and diabetes, possible mediators, did not totally explain the association between BMI and myocardial infarction. The authors suggested the existence of other unmeasured factors that mediate the association, such as prothrombotic factors or low-grade systematic inflammation, and implied that avoidance of obesity offers the potential of reducing CHD in Japan.
Risks related to metabolic syndrome and its screening
Metabolic syndrome (MetS) is a cluster of risk factors for CVD and type 2 diabetes mellitus, which occur together more often than by chance alone [50].
Although various diagnostic criteria have been proposed by different organizations [50], the risk factors included are generally common: raised blood pressure, dyslipidemia (raised triglycerides and lowered high-density lipoprotein cholesterol), raised fasting glucose, and abdominal obesity. While the criteria proposed by the International Diabetes Federation (IDF) as well as the fact that Japanese made abdominal obesity an obligatory component [51] (Table 3), the criteria of the American Heart Association/National Heart, Lung, and Blood Institute (AHA/NHLBI) do not mandate abdominal obesity as a required risk factor; three abnormal findings out of five will qualify a person for the MetS.
Table 3.
Components of metabolic syndrome in Japan [51]
| Abdominal obesity (obligatory component) | ≥85 cm in men and ≥90 cm in women |
| Raised blood pressure | Systolic blood pressure ≥130 mmHg or |
| Diastolic blood pressure ≥85 mmHg | |
| Dyslipidemia | Triglycerides ≥150 mg/dl or |
| High-density lipoprotein cholesterol <40 mg/dl in men and <50 mg/dl in women | |
| Raised fasting glucose | Fasting glucose ≥100 mg/dl |
The goal of population-based screening of MetS would be to identify a risk state for the development of CVD and diabetes in order to intervene. To maximize public health, the tool used must not overlook a substantial proportion of high-risk individuals, who eventually develop the conditions. In a European population-based study, non-obese people with two or more IDF MetS factors were less prevalent than IDF MetS individuals, but their CVD mortality rate was comparable to that of individuals with IDF MetS [52]. The PAF calculated from the data was 10.0% for men with two or more risk factors without abdominal obesity and 28.2% for men that met IDF MetS criteria. This suggests that IDF criteria would miss at least an opportunity to provide interventions to such individuals. In Japan, there were reportedly more non-overweight individuals with a constellation of risk factors than overweight individuals with the same constellation (i.e., IDF MetS equivalent) in the general population, with both groups having a similar mortality risk [53]. Hence, the PAF was reported to be greater in non-overweight individuals with two or more risk factors (9.4%) than in overweight individuals with the same number of risk factors (7.8%). As similar findings were repeatedly reported [54–58], there has been concern regarding the appropriateness of the public health screening that currently excludes such individuals from the diagnosis of MetS in Japan. Therefore, at the screening level, focusing only on the abdominal obesity-prerequisite IDF MetS cannot be recommended in current Japan where a large proportion of individuals are in a risk state for CVD without being overweight. Nevertheless, IDF MetS is easy to understand pathophysiologically, and interventions targeting abdominal obesity have proved to be effective [59]. The reason is yet unclear for the high prevalence of a risk factor constellation without being overweight in Japan. How to effectively intervene in such cases must also be investigated.
Concluding remarks and outlook
Obesity is a major health concern for most of the world given its already high prevalence. Obesity prevalence has doubled or tripled in many countries since 1980, and is still projected to increase. Even though various measures and actions have been undertaken to avoid fulfillment of this projection, it is almost certain that an obesity epidemic persists. This epidemic seems to have been affecting some age-, sex-, and area-subgroups of the population disproportionately. However, overall and recent trends do not seem to differ considerably.
Even in a relatively lean population like the Japanese, an association has been established between adiposity and CVD risk factors, including hypertension, diabetes mellitus, and dyslipidemia. Thus, the notion that obesity confers increased CVD risk seems plausible. However, there is a sizeable proportion of individuals who are at an increased CVD risk state without being currently overweight/obese. Public health activities to prevent CVD and promote population health should not overlook this fact.
Although a current public health screening and intervention program in Japan that started in 2008 has considerably raised public awareness of obesity and metabolic syndrome, it overemphasized measures to deal with abdominal obesity to the detriment of predictive diagnosis and targeted prevention. Consequently, the intervention program has tended to overlook the opportunity to intervene with non-obese high risk individuals, such as lean hypertensives. More extensive communication is necessary among medical and public health professionals as well as health and insurance administrators to amend the act for this program [60]. We conclude that further implementation and promotion of activities to bring about meaningful changes in the obesity trend in rural and urban communities are needed. However, such activities should be harmonized with other domains of CVD prevention activities.
Acknowledgements
This work was supported in part by a Grant-in-Aid for Scientific Research (KAKENHI) (22390133) by the Japan Society for the Promotion of Science (JSPS) and grants from the Japan Arteriosclerosis Prevention Fund (JAPF).
Footnotes
H. Iso is a National Representative of EPMA in Japan
References
- 1.Ueshima H, Sekikawa A, Miura K, Turin TC, Takashima N, Kita Y, Watanabe M, Kadota A, Okuda N, Kadowaki T, Nakamura Y, Okamura T. Cardiovascular disease and risk factors in Asia: a selected review. Circulation. 2008;118:2702–9. doi: 10.1161/CIRCULATIONAHA.108.790048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Iso H, Sato S, Kitamura A, Naito Y, Shimamoto T, Komachi Y. Fat and protein intakes and risk of intraparenchymal hemorrhage among middle-aged Japanese. Am J Epidemiol. 2003;157:32–9. doi: 10.1093/aje/kwf166. [DOI] [PubMed] [Google Scholar]
- 3.Iso H. Changes in coronary heart disease risk among Japanese. Circulation. 2008;118:2725–9. doi: 10.1161/CIRCULATIONAHA.107.750117. [DOI] [PubMed] [Google Scholar]
- 4.Kubo M, Kiyohara Y, Ninomiya T, Tanizaki Y, Yonemoto K, Doi Y, Hata J, Oishi Y, Shikata K, Iida M. Decreasing incidence of lacunar vs other types of cerebral infarction in a Japanese population. Neurology. 2006;66:1539–44. doi: 10.1212/01.wnl.0000216132.95207.b4. [DOI] [PubMed] [Google Scholar]
- 5.Shimamoto T, Komachi Y, Inada H, Doi M, Iso H, Sato S, Kitamura A, Iida M, Konishi M, Nakanishi N, et al. Trends for coronary heart disease and stroke and their risk factors in Japan. Circulation. 1989;79:503–15. doi: 10.1161/01.cir.79.3.503. [DOI] [PubMed] [Google Scholar]
- 6.Kitamura A, Iso H, Iida M, Naito Y, Sato S, Jacobs DR, Nakamura M, Shimamoto T, Komachi Y. Trends in the incidence of coronary heart disease and stroke and the prevalence of cardiovascular risk factors among Japanese men from 1963 to 1994. Am J Med. 2002;112:104–9. doi: 10.1016/S0002-9343(01)01053-1. [DOI] [PubMed] [Google Scholar]
- 7.Kitamura A, Sato S, Kiyama M, Imano H, Iso H, Okada T, Ohira T, Tanigawa T, Yamagishi K, Nakamura M, Konishi M, Shimamoto T, Iida M, Komachi Y. Trends in the incidence of coronary heart disease and stroke and their risk factors in Japan, 1964 to 2003: the Akita-Osaka study. J Am Coll Cardiol. 2008;52:71–9. doi: 10.1016/j.jacc.2008.02.075. [DOI] [PubMed] [Google Scholar]
- 8.Costigliola V. Preface. EPMA J. 2010;1:1–2. doi: 10.1007/s13167-010-0013-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Golubnitschaja O. Time for new guidelines in advanced diabetes care: Paradigm change from delayed interventional approach to predictive, preventive & personalized medicine. EPMA J. 2010;1:3–12. doi: 10.1007/s13167-010-0014-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.World Health Organization. BMI classification. (http://apps.who.int/bmi/index.jsp?introPage=intro_3.html).
- 11.Office for Life-Style Related Diseases Control, General Affair Division, Health Service Bureau, Ministry of Health, Labor and Welfare, Japan. The National Health and Nutrition Survey in Japan, 2003–2007. (http://www.mhlw.go.jp/bunya/kenkou/kokumin-kenkou.html) (in Japanese).
- 12.Sassi F. Obesity and the economics of prevention. FIT NOT FAT. Paris: OECD Publishing; 2010. [Google Scholar]
- 13.Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults, 1999–2008. JAMA. 2010;303:235–41. doi: 10.1001/jama.2009.2014. [DOI] [PubMed] [Google Scholar]
- 14.New criteria for ‘obesity disease’ in Japan. Circ J. 2002;66:987–92. [DOI] [PubMed]
- 15.Office for Life-Style Related Diseases Control, General Affair Division, Health Service Bureau, Ministry of Health, Labor and Welfare, Japan. The National Nutrition Survey in Japan, 1950–2002. (http://www.nih.go.jp/eiken/chosa/kokumin_eiyou/) (in Japanese).
- 16.Matsushita Y, Takahashi Y, Mizoue T, Inoue M, Noda M, Tsugane S. Overweight and obesity trends among Japanese adults: a 10-year follow-up of the JPHC Study. Int J Obes (Lond) 2008;32:1861–7. doi: 10.1038/ijo.2008.188. [DOI] [PubMed] [Google Scholar]
- 17.Kubo M, Hata J, Doi Y, Tanizaki Y, Iida M, Kiyohara Y. Secular trends in the incidence of and risk factors for ischemic stroke and its subtypes in Japanese population. Circulation. 2008;118:2672–8. doi: 10.1161/CIRCULATIONAHA.107.743211. [DOI] [PubMed] [Google Scholar]
- 18.Yoshiike N, Kaneda F, Takimoto H.Epidemiology of obesity and public health strategies for its control in Japan Asia Pac J Clin Nutr 200211Suppl 8S727–31. 10.1046/j.1440-6047.11.s8.18.x12534700 [DOI] [Google Scholar]
- 19.Komachi Y. Recent trend in the research of hypertension in Japan. Characteristics of hypertension in Japan. Nippon Naika Gakkai Zasshi. 1988;77:1802–5. doi: 10.2169/naika.77.1802. [DOI] [PubMed] [Google Scholar]
- 20.Kitamura A, Kiyama M, Okada T, Maeda K, Ido M, Nakamura M, Shimamoto T, Iida M, Ishikawa Y. Trends in cardiovascular risk factors among urban Japanese male employees from 1977 to 2008. Sangyo Eiseigaku Zasshi. 2010;52:123–32. doi: 10.1539/sangyoeisei.B9019. [DOI] [PubMed] [Google Scholar]
- 21.Yamagishi K, Hosoda T, Sairenchi T, Mori K, Tomita H, Nishimura A, Tanigawa T, Iso H. Body mass index and subsequent risk of hypertension, diabetes and hypercholesterolemia in a population-based sample of Japanese. Nippon Koshu Eisei Zasshi. 2003;50:1050–7. [PubMed] [Google Scholar]
- 22.Ishikawa-Takata K, Ohta T, Moritaki K, Gotou T, Inoue S. Obesity, weight change and risks for hypertension, diabetes and hypercholesterolemia in Japanese men. Eur J Clin Nutr. 2002;56:601–7. doi: 10.1038/sj.ejcn.1601364. [DOI] [PubMed] [Google Scholar]
- 23.Chei CL, Iso H, Yamagishi K, Inoue M, Tsugane S. Body mass index and weight change since 20 years of age and risk of coronary heart disease among Japanese: the Japan Public Health Center-Based Study. Int J Obes (Lond) 2008;32:144–51. doi: 10.1038/sj.ijo.0803686. [DOI] [PubMed] [Google Scholar]
- 24.Forman JP, Stampfer MJ, Curhan GC. Diet and lifestyle risk factors associated with incident hypertension in women. JAMA. 2009;302:401–11. doi: 10.1001/jama.2009.1060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Konishi M, Iso H, Komachi Y, Iida M, Shimamoto T, Jacobs DR, Jr, Terao A, Baba S, Sankai T, Ito M. Associations of serum total cholesterol, different types of stroke, and stenosis distribution of cerebral arteries. The Akita Pathology Study. Stroke. 1993;24:954–64. doi: 10.1161/01.str.24.7.954. [DOI] [PubMed] [Google Scholar]
- 26.Ogata J, Yamanishi H, Ishibashi-Ueda H. Review: role of cerebral vessels in ischaemic injury of the brain. Neuropathol Appl Neurobiol. 2011;37:40–55. doi: 10.1111/j.1365-2990.2010.01141.x. [DOI] [PubMed] [Google Scholar]
- 27.Simon G. Why do treated hypertensives suffer strokes? An internist’s perspective. J Clin Hypertens. 2002;4:338–44. doi: 10.1111/j.1524-6175.2002.00686.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Iso H, Shimamoto T, Kitamura A, Iida M, Komachi Y. Trends of cardiovascular risk factors and diseases in Japan: implications for primordial prevention. Prev Med. 1999;29:S102–5. doi: 10.1006/pmed.1998.0402. [DOI] [PubMed] [Google Scholar]
- 29.Ohira T, Shahar E, Chambless LE, Rosamond WD, Mosley TH, Jr, Folsom AR. Risk factors for ischemic stroke subtypes: the Atherosclerosis Risk in Communities study. Stroke. 2006;37:2493–8. doi: 10.1161/01.STR.0000239694.19359.88. [DOI] [PubMed] [Google Scholar]
- 30.Kitamura A, Nakagawa Y, Sato M, Iso H, Sato S, Imano H, Kiyama M, Okada T, Okada H, Iida M, Shimamoto T. Proportions of stroke subtypes among men and women > or =40 years of age in an urban Japanese city in 1992, 1997, and 2002. Stroke. 2006;37:1374–8. doi: 10.1161/01.STR.0000221714.96986.5f. [DOI] [PubMed] [Google Scholar]
- 31.Shimamoto T, Iso H, Sankai T, Iida M, Naito Y, Sato S, Kitamura A, Kiyama M, Konishi M, Terao A, Baba S, Ozawa H, Komachi Y. Can blood pressure in the elderly be reduced? Findings from a long-term population survey in Japan. Am J Geriatr Cardiol. 1994;3:42–50. [PubMed] [Google Scholar]
- 32.Fox CS, Coady S, Sorlie PD, D’Agostino RB, Sr, Pencina MJ, Vasan RS, Meigs JB, Levy D, Savage PJ. Increasing cardiovascular disease burden due to diabetes mellitus: the Framingham Heart Study. Circulation. 2007;115:1544–50. doi: 10.1161/CIRCULATIONAHA.106.658948. [DOI] [PubMed] [Google Scholar]
- 33.Iso H, Imano H, Kitamura A, Sato S, Naito Y, Tanigawa T, Ohira T, Yamagishi K, Iida M, Shimamoto T. Type 2 diabetes and risk of non-embolic ischaemic stroke in Japanese men and women. Diabetologia. 2004;47:2137–44. doi: 10.1007/s00125-004-1587-0. [DOI] [PubMed] [Google Scholar]
- 34.Tanaka H, Ueda Y, Hayashi M, Date C, Baba T, Yamashita H, Shoji H, Tanaka Y, Owada K, Detels R. Risk factors for cerebral hemorrhage and cerebral infarction in a Japanese rural community. Stroke. 1982;13:62–73. doi: 10.1161/01.str.13.1.62. [DOI] [PubMed] [Google Scholar]
- 35.Nakayama T, Date C, Yokoyama T, Yoshiike N, Yamaguchi M, Tanaka H. A 15.5-year follow-up study of stroke in a Japanese provincial city. The Shibata Study. Stroke. 1997;28:45–52. doi: 10.1161/01.str.28.1.45. [DOI] [PubMed] [Google Scholar]
- 36.Curb JD, Marcus EB. Body fat, coronary heart disease, and stroke in Japanese men. Am J Clin Nutr. 1991;53:1612S–5S. doi: 10.1093/ajcn/53.6.1612S. [DOI] [PubMed] [Google Scholar]
- 37.Saito I, Iso H, Kokubo Y, Inoue M, Tsugane S. Body mass index, weight change and risk of stroke and stroke subtypes: the Japan Public Health Center-based prospective (JPHC) study. Int J Obes (Lond). 2011;35:283–91. [DOI] [PubMed]
- 38.Furukawa Y, Kokubo Y, Okamura T, Watanabe M, Higashiyama A, Ono Y, Kawanishi K, Okayama A, Date C. The relationship between waist circumference and the risk of stroke and myocardial infarction in a Japanese urban cohort: the Suita study. Stroke. 2010;41:550–3. doi: 10.1161/STROKEAHA.109.569145. [DOI] [PubMed] [Google Scholar]
- 39.Iso H, Sato S, Kitamura A, Imano H, Kiyama M, Yamagishi K, Cui R, Tanigawa T, Shimamoto T. Metabolic syndrome and the risk of ischemic heart disease and stroke among Japanese men and women. Stroke. 2007;38:1744–51. doi: 10.1161/STROKEAHA.106.469072. [DOI] [PubMed] [Google Scholar]
- 40.Tanizaki Y, Kiyohara Y, Kato I, Iwamoto H, Nakayama K, Shinohara N, Arima H, Tanaka K, Ibayashi S, Fujishima M. Incidence and risk factors for subtypes of cerebral infarction in a general population: the Hisayama study. Stroke. 2000;31:2616–22. doi: 10.1161/01.str.31.11.2616. [DOI] [PubMed] [Google Scholar]
- 41.Yonemoto K, Doi Y, Hata J, Ninomiya T, Fukuhara M, Ikeda F, Mukai N, Iida M, Kiyohara Y. Body mass index and stroke incidence in a Japanese community: the Hisayama study. Hypertens Res. 2010;34:274–9. doi: 10.1038/hr.2010.220. [DOI] [PubMed] [Google Scholar]
- 42.Yatsuya H, Toyoshima H, Yamagishi K, Tamakoshi K, Taguri M, Harada A, Ohashi Y, Kita Y, Naito Y, Yamada M, Tanabe N, Iso H, Ueshima H. Body mass index and risk of stroke and myocardial infarction in a relatively lean population: meta-analysis of 16 Japanese cohorts using individual data. Circ Cardiovasc Qual Outcomes. 2010;3:498–505. doi: 10.1161/CIRCOUTCOMES.109.908517. [DOI] [PubMed] [Google Scholar]
- 43.2003 European Society of Hypertension-European Society of Cardiology guidelines for the management of arterial hypertension. J Hypertens 2003;21:1011–53. [DOI] [PubMed]
- 44.Imano H, Kitamura A, Sato S, Kiyama M, Ohira T, Yamagishi K, Noda H, Tanigawa T, Iso H, Shimamoto T. Trends for blood pressure and its contribution to stroke incidence in the middle-aged Japanese population: the Circulatory Risk in Communities Study (CIRCS) Stroke. 2009;40:1571–7. doi: 10.1161/STROKEAHA.108.538629. [DOI] [PubMed] [Google Scholar]
- 45.Yatsuya H, Yamagishi K, North KE, Brancati FL, Stevens J, Folsom AR. Associations of obesity measures with subtypes of ischemic stroke in the ARIC Study. J Epidemiol. 2010;20:347–54. doi: 10.2188/jea.JE20090186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Konishi M, Iso H, Iida M, Naito Y, Sato S, Komachi Y, Shimamoto T, Doi M, Ito M. Trends for coronary heart disease and its risk factors in Japan: epidemiologic and pathologic studies. Jpn Circ J. 1990;54:428–35. doi: 10.1253/jcj.54.428. [DOI] [PubMed] [Google Scholar]
- 47.Rumana N, Kita Y, Turin TC, Murakami Y, Sugihara H, Morita Y, Tomioka N, Okayama A, Nakamura Y, Abbott RD, Ueshima H. Trend of increase in the incidence of acute myocardial infarction in a Japanese population: Takashima AMI Registry, 1990–2001. Am J Epidemiol. 2008;167:1358–64. doi: 10.1093/aje/kwn064. [DOI] [PubMed] [Google Scholar]
- 48.Kubo M, Kiyohara Y, Kato I, Tanizaki Y, Arima H, Tanaka K, Nakamura H, Okubo K, Iida M. Trends in the incidence, mortality, and survival rate of cardiovascular disease in a Japanese community: the Hisayama study. Stroke. 2003;34:2349–54. doi: 10.1161/01.STR.0000090348.52943.A2. [DOI] [PubMed] [Google Scholar]
- 49.Robertson TL, Kato H, Gordon T, Kagan A, Rhoads GG, Land CE, Worth RM, Belsky JL, Dock DS, Miyanishi M, Kawamoto S. Epidemiologic studies of coronary heart disease and stroke in Japanese men living in Japan, Hawaii and California. Coronary heart disease risk factors in Japan and Hawaii. Am J Cardiol. 1977;39:244–9. doi: 10.1016/S0002-9149(77)80198-7. [DOI] [PubMed] [Google Scholar]
- 50.Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, Fruchart JC, James WP, Loria CM, Smith SC., Jr Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation. 2009;120:1640–5. doi: 10.1161/CIRCULATIONAHA.109.192644. [DOI] [PubMed] [Google Scholar]
- 51.Definition and the diagnostic standard for metabolic syndrome—Committee to evaluate diagnostic standards for metabolic syndrome. Nippon Naika Gakkai Zasshi 2005;94:794–809 (in Japanese). [PubMed]
- 52.Gao W. Does the constellation of risk factors with and without abdominal adiposity associate with different cardiovascular mortality risk? Int J Obes (Lond) 2008;32:757–62. doi: 10.1038/sj.ijo.0803797. [DOI] [PubMed] [Google Scholar]
- 53.Saito I, Iso H, Kokubo Y, Inoue M, Tsugane S. Metabolic syndrome and all-cause and cardiovascular disease mortality: Japan Public Health Center-based Prospective (JPHC) Study. Circ J. 2009;73:878–84. doi: 10.1253/circj.CJ-08-1025. [DOI] [PubMed] [Google Scholar]
- 54.Irie F, Iso H, Noda H, Sairenchi T, Otaka E, Yamagishi K, Doi M, Izumi Y, Ota H. Associations between metabolic syndrome and mortality from cardiovascular disease in Japanese general population, findings on overweight and non-overweight individuals. Ibaraki Prefectural Health Study. Circ J. 2009;73:1635–42. doi: 10.1253/circj.CJ-08-0442. [DOI] [PubMed] [Google Scholar]
- 55.Kadota A, Hozawa A, Okamura T, Kadowak T, Nakmaura K, Murakami Y, Hayakawa T, Kita Y, Okayama A, Nakamura Y, Kashiwagi A, Ueshima H. Relationship between metabolic risk factor clustering and cardiovascular mortality stratified by high blood glucose and obesity: NIPPON DATA90, 1990–2000. Diabetes Care. 2007;30:1533–8. doi: 10.2337/dc06-2074. [DOI] [PubMed] [Google Scholar]
- 56.Kokubo Y, Okamura T, Yoshimasa Y, Miyamoto Y, Kawanishi K, Kotani Y, Okayama A, Tomoike H. Impact of metabolic syndrome components on the incidence of cardiovascular disease in a general urban Japanese population: the suita study. Hypertens Res. 2008;31:2027–35. doi: 10.1291/hypres.31.2027. [DOI] [PubMed] [Google Scholar]
- 57.Noda H, Iso H, Saito I, Konishi M, Inoue M, Tsugane S. The impact of the metabolic syndrome and its components on the incidence of ischemic heart disease and stroke: the Japan public health center-based study. Hypertens Res. 2009;32:289–98. doi: 10.1038/hr.2009.14. [DOI] [PubMed] [Google Scholar]
- 58.Saito I, Konishi M, Watanabe K, Kondo H, Fujimotos K, Okada K. The metabolic syndrome and risk of stroke in a rural community in Japan. Nippon Koshu Eisei Zasshi. 2007;54:677–83. [PubMed] [Google Scholar]
- 59.Klein S, Burke LE, Bray GA, Blair S, Allison DB, Pi-Sunyer X, Hong Y, Eckel RH. Clinical implications of obesity with specific focus on cardiovascular disease: a statement for professionals from the American Heart Association Council on Nutrition, Physical Activity, and Metabolism: endorsed by the American College of Cardiology Foundation. Circulation. 2004;110:2952–67. doi: 10.1161/01.CIR.0000145546.97738.1E. [DOI] [PubMed] [Google Scholar]
- 60.Une H. A questionnaire survey on the annual health check-up and guidance system targeted on the metabolic syndrome. Nippon Koshu Eisei Zasshi. 2009;56:371–81. [PubMed] [Google Scholar]


