Abstract
Suicidality and suicide has been associated with many risk factors, while recent clinical and epidemiological studies increasingly point to a potential link between sleep loss or sleep disturbances and suicidality. This review on studies of sleep disturbances associated with suicidality, i.e., suicidal ideation, suicide attempt and completed suicide suggests a frequent association especially with insomnia and nightmares but also hypersomnia and sleep panic attacks. In suicidal insomniacs with comorbid psychiatric disorders, there is some evidence for an even independent predictive nature of sleep problems for suicidality. Considerations on the shared neurobiology, risk assessment and treatment options complement the overview. Thus, sleep disturbances may qualify as an individual treatable target of personalised medicine in the clinical routine as well as in suicide prevention programmes. A more detailed assessment of sleep problems and identification of specific risk domains in primary or secondary prevention of suicidality seem to be a future area of high importance.
Keywords: Sleep disturbances, Nightmares, Suicidality, Personalised risk assessment, Suicide prevention, Mental disorders
Introduction
Suicide is a complex health problem and a worldwide leading cause of death with high annual mortality rates, e.g. approximately 30,000 persons in the United States in 2010 [1] or 10,000 persons in Germany in 2009 [2]. Multiple neurobiological, medical and psychosocial variables of influence on developing suicidal tendencies are being discussed [3–7] while it has been estimated that up to 90% of suicide completers have previously suffered from a psychiatric disorder [8].
On the other hand sleep disturbances are very common and have a major impact on physical and mental health, and they are part of many psychiatric disorders [9, 10]. A close association between suicidality and sleep disturbances especially insomnia has been discussed for a while with recently increasing concerns [6, 11–14], but only few studies indeed focused on the potential predictive quality of sleep disturbances or sleep loss for suicidal ideation and behaviours (e.g., [15–17]). Assessment and treatment of individual sleep disturbances might represent a personalised preventive measure of suicidality and suicide. This article aims at giving an overview of the current topics of research in this area.
Suicidality and sleep disorders
Sleep loss and Insomnia
Insomnia is the most common sleep problem with about one third of the general population suffering [10] but only a small number of epidemiological studies investigated suicidality and insomnia complaints by assessing subjective sleep variables (Table 1).
Table 1.
Sleep disturbances and suicidality—selected studies in adults from 1997–2011
| Study | Sample | Design and N | Sleep disturbance/ variables | Specified Outcome | Principle Finding |
|---|---|---|---|---|---|
| Ağargün et al. 1997 [48] | Depressed patients | Cross-sectional N = 41 | Sleep quality, sleep duration, sleep latency, sleep effiency | Suicidal behaviour | Poor subjective sleep quality is associated with suicidal behaviour in depressed patients |
| Ağargün et al. 1997 [49] | Depressed patients | Cross-sectional N = 113 | Insomnia, hypersomnia | Suicidal thoughts | Hypersomnia and insomnia are associated with suicidal thoughts in depressed patients |
| Ağargün et al. 1998 [62] | Patients with panic disorder | Cross-sectional N = 67 | Insomnia, sleep panic | Suicidal tendencies | Recurrent sleep panic is associated with suicidal tendencies in patients with panic disorder |
| Ağargün et al. 1998 [28] | Depressed patients | Cross-sectional N = 63 | Nightmares | Suicidal thoughts | Frequent nightmares are associated with suicidal thoughts in depressed patients especially feamles |
| Hall et al. 1999 [23] | Emergency patients after suicide attempt | Cross-sectional N = 100 | Partial and global insomnia | Suicide attempt | Partial and global insomnia is associated with suicide attempt in emergency patients |
| Krakow et al. 2000 [34] | Female sexual assault survivors | Cross-sectional N = 153 | Sleep breathing and sleep movement disorders | Suicidal ideation | Potential sleep breathing and sleep movement disorders are associated with suicidal ideation in female sexual assault survivors |
| Tanskanen et al. 2001 [27] | Population survey | Prospective N = 36,211 | Nightmares | Completed suicide | The frequency of nightmares is directly associated with higher risk of suicide in the general population |
| Turvey et al. 2002 [43] | Population survey | Prospective N = 14,456 | Poor sleep quality | Late-life suicide | Poor sleep quality is associated with late-life suicide in the general population |
| Bernert et al. 2005 [13] | Depressed outpatients | Cross-sectional N = 176 | Insomnia, nightmares | Suicidal ideation | After controlling for variables only nightmares (but not insomnia) are associated with suicidal ideation in depressed outpatients |
| Chellappa et al. 2006 [32] | Depressed outpatients | Cross-sectional N = 70 | Excessive daytime sleepiness | Suicidal ideation | Excessive daytime sleepiness is associated with suicidal ideation in depressed outpatients |
| Ağargün et al. 2007 [29] | Depressed patients with and without melancholic features | Cross-sectional N = 100 | Insomnia, nightmares | Suicide attempt | Middle and terminal insomnia and nightmares are associated with suicide attempt in patients with melancholic depression |
| Sjöström et al. 2007 [24] | Suicide attempters | Cross-sectional N = 165 | Insomnia, nightmares | Suicide attempt | Nightmares are associated with a 5-fold increase in risk for high suicidality in suicide attempters |
| Wallander et al. 2007 [41] | Patients with sleep disorders | Cohort study with nested case-control analysis N = 12,437 | Sleep disorders | Completed suicide | Relative 1-year mortality risk due to suicide is 3-fold higher in patients with sleep disorders |
| Goodwin et al. 2008 [15] | Population survey | Cross-sectional N = 8,098 | Short sleep | Suicidal ideation, suicide attempt | Short sleep is associated with increased odds of suicidal ideation and suicide attempt |
| Sjöström et al. 2009 [26] | Suicide attempters | Prospective N = 165 | Nightmares, difficulty initiating sleep, difficulty maintaining sleep, | Repeated suicide attempt | Frequent nightmares (but not difficulties in initiating/ maintaining sleep nor early morning qwakening) at baseline but predict repeated suicide attempts |
| Wojnar et al. 2009 [16] | Population survey | Cross-sectional N = 5,692 | Early morning awaking, difficulty initiating sleep, difficulty maintaining sleep, insomnia | Suicidal thoughts, plans and attempts | The presence of any sleep problem is associated with greater risk for suicidality among community residents |
| McCall et al. 2010 [51] | Patients with depression and insomnia symptoms in clinical trial | Prospective (fluoxetine±eszoplicone) N = 60 | Insomnia | Suicidal ideation | Insomnia severity (but not depressed mood) corresponds to greater intensity of suicidal thinking during a depression clinical trial |
| Li et al. 2010 [17] | Psychiatric outpatients | Cross-sectional N = 1,231 | Insomnia, nightmares | Suicide risk | Frequent insomnia and recurrent nightmares are associated with enhanced suicide attempts among psychiatric outpatients |
| Brower et al. 2011 [97] | Population survey | Cross-sectional N = 5,692 | Insomnia, use of sedatives-hypnotics | Suicidal thoughts and attempts | Insomnia and use of sedatives-hypnotics are associated with enhanced suicidality among household respondents |
| Chin et al. 2011 [19] | Population survey | Cross-sectional N = 6,969 | Sleep duration | Suicidal ideation | Short sleep is associated with suicidal ideation in women |
| Krakow et al. 2011 [25] | Sleep center patients | Cross-sectional N = 1,584 | Sleep disturbances | Suicidal ideation | Sleep centre patients with suicidal ideation show a greater frequency or severity of sleep problems |
| Rod et al. 2011 [18] | Population survey | Prospective N = 16,989 | Sleep disturbances | Completed suicide | Men with ≥3 types of sleep disturbances have an almost 5 times’ higher risk of committing suicide |
| Blasco-Fontecilla et al. 2011 [22] | Psychiatric suicide attempters /-non-attempters, healthy controls | Cross-sectional N = 1,076 | Short sleep (= <5 h) | Suicide attempts | Short sleep is frequent in male suicide attempters and associated with severity of suicidal behaviour in women |
Based upon McCall et al. 2010 [51]
Detailed reports of sleep problems (difficulty initiating sleep, maintaining sleep, early morning awaking, and insomnia) were identified to be significantly associated with an increased risk of suicidality, i.e. suicidal ideation, plans or attempts (unadjusted odds ratio´s, OR’s = 4.2–9.09) in the preceding 12 months in a representative adult sample using data from an American representative survey (National Comorbidity Survey Replication) [16]. This relationship remained stable in most cases after controlling for diagnoses of depression, anxiety disorder and substance abuse. Remarkably, difficulty in initiating sleep predicted suicidal ideation and planning, problems in maintaining sleep predicted suicidal ideation and suicidal attempt, and early morning awaking and insomnia scores were predictive for all three suicidal dimensions (suicide ideation, planning and attempt) (OR’s = 1.2–3.0) [16]. These results on abnormalities in multiple subjective sleep variables are complemented by the Danish follow-up GAZEL study between 1990 and 2009 that showed completed suicide was almost fivefold enhanced in men who reported of three types or more of sleep disturbances [18].
Adult data from the “Korean National Health and Nutrition Examination Survey” showed an association between decrease in sleep time and increase in suicidal ideation in women [19]. Analysis of another representative adults sample in the United States (National Comorbidity Survey) gave evidence that short sleep was associated with 2.5 to 3fold increase in suicidal ideation and suicide attempt [15]. However, the effect on suicidal attempt was predominantly explained by panic attacks, mood and substance use disorders. Liu et al. showed that sleep duration below 8 h was associated with an increase in risk of suicide attempts in Chinese community adolescents [20]. Notably, as in adolescents the sleep duration and its association with suicidal attempts and various other risky behaviours will probably have to be evaluated somewhat differently [21] the body of this particular literature will not be discussed in this overview. However, in a very recent study addressing this issue [22] short sleep ≤ 5 h was found to be a marker of severity of suicidal behaviour among female suicide attempters but not male in comparison to other psychiatric patients without any suicide attempts and healthy controls. Thus, some authors assume sleep duration to be a relatively simple way for screening of sleep loss as a potential marker of individuals at risk of suicidality [6].
Suicide risk assessment plays a key role in clinical practise but associated clinical studies on sleep problems are still rare albeit findings are in line with the outcome in epidemiological investigations. Hall et al. [23] examined emergency patients after serious suicide attempts. A detailed review of symptoms and common suicide risk factors revealed that the presence or absence of suicidal ideation or a specific plan did not define patients at risk for serious suicide attempts while rather the presence of insomnia but also of severe anxiety and/or panic attacks, depressed mood, recent loss of close personal relationship, alcohol and substance abuse, feelings of hopelessness, helplessness and worthlessness was most predictive. Importantly 46% of the patients reported global insomnia, 92% of the patients reported partial insomnia, i.e., difficulty falling asleep, sleep continuity disorder and early morning awaking. As only 14% of suicide attempters had suicidal thoughts with any previous plan prior to the suicide attempt that was potentially of impulsive or reactive nature, insomnia in this study was more frequently found prior to severe and near-lethal suicide attempts than specific suicide plans [23]. Sjöström et al. [24] found similar rates with 89% of patients admitted after suicide attempts to report on sleep disturbances with main complaints of difficulties initiating sleep (73%), difficulties maintaining sleep (69%), nightmares (66%) and early morning awakening (58%).
Another recent large-scale clinical study among psychiatric outpatients in China using a detailed sleep questionnaire strengthened the evidence of an association between insomnia and suicidality [17]. Frequent insomnia was independently associated with enhanced incidence of suicidal attempts (OR = 6.96) as well as lifetime prevalence of suicide attempts (OR = 1.55) [17]. Focusing on patients presenting at a community based private sleep medical centre Krakow et al. [25] demonstrated that suicidality was indeed common, too. Overall 13.3% of patients reported suicidal ideation showing significant associations between greater frequency of severity of sleep problems and insomnia, but also nightmares and other parasomnias and mostly independent of depression severity. Importantly, suicidal ideation was evaluated as clinically significant in 4.5% of patients [25].
Nightmares
There is body of literature on nightmares and suicidality strongly pointing to its link [13, 24, 26, 27]. In a large and prospective Finish population-based follow-up study the frequency of nightmares was directly related to the risk of suicide [27]. The adjusted relative risk of suicide was 57% higher in subjects with occasional nightmares and 105% higher in frequent nightmares as compared to subjects without any nightmare experiences [27].
One outpatient study [24] found nightmares in 66% of medical and psychiatric patients and nightmares were associated with a 5-fold increase in risk for high suicidality. This relationship remained stable after adjustment for psychiatric diagnosis and psychiatric symptom intensity. In the 2-month follow-up of patients after a first suicide attempt and admission to hospital frequent nightmares predicted a repeated attempt (OR = 3.15) (but neither difficulties initiating/maintaining sleep nor early morning awaking) with a further heightened risk (OR = 5.20) when nightmares were also reported at follow-up [26]. In the study of Li et al. [17] recurrent nightmares were significantly and independently associated with an increased incidence of suicide attempts 1 year after questionnaire assessment in psychiatric outpatients. Another clinical outpatient study investigated frequency and severity of symptoms of nightmares, suicidality and depression [13]. Insomnia and nightmares were significantly associated with depressive and suicidal symptoms, but after controlling for additional variables, e.g., depression and sex, only nightmares remained associated with suicidal ideation, and this effect in trend was a little stronger in women [13].
On the other hand, patients with major depression, who reported frequent and frightening nightmares, showed higher suicidality than those without any nightmares (particularly women) [28]. Higher rates of nightmares and insomnia were also found in melancholic depression with suicide attempts as opposed to melancholic non-attempters, but there were no differences in non-melancholic depressed patients without or without attempts [29]. The authors conclude that melancholic features like feeling worse in the morning might be associated to enhanced risk of suicidality via a more negative affect and dream content though this hypothesis remains subject to further studies.
In addition, psychotropic medication was independently associated with recurrent nightmares, i.e., antidepressants, particularly selective serotonin reuptake inhibitors (SSRI), serotonin-norepinephrine reuptake inhibitors (SRNI), heterocyclics, and non-benzodiazepine hypnotics were independently associated with recurrent nightmares after adjustment for confounding variables [17].
Others parasomnias
Misinterpretation of suicidal behaviour (“pseudo-suicide”) in patients with parasomnias has been discussed especially in the forensic context due to injuries or violent behaviours but these are to be diagnosed as sleep-related complex behaviours like sleep walking or others and therefore are regarded to be without premeditation, conscious awareness, or individual responsibility [30]. However, idiopathic REM sleep behaviour disorder (RBD) may also lead to conflicts with the bed partner and subsequent suicidality to be resolved by drug treatment of the RBD [31].
Hypersomnia
As daytime sleepiness or fatigue might also be a symptom of depression a careful investigation of hypersomnia in depressed patients is always advised too. However, a Brazilian cross-sectional sample of psychiatric outpatients was the first to describe a strong relationship between excessive daytime sleepiness (EDS) and symptoms of depression as well as suicidal ideation [32]. With regard to obstructive sleep apnoae the presence of symptoms of sleep-related breathing disorder (SRBD) was associated with depressive symptoms [13, 33], but in the outpatient study of Bernert et al. [13] there was no association of SRBD with symptoms of suicidality. Nevertheless, women who were assigned to a posttraumatic stress disorder (PTSD) programme revealed higher scores for depression and suicidal ideation if they also experienced a SRBD [34]. Moreover, there is the interesting case of a 74-year-old male outpatient, who presented not only with depressive mood and severe suicidal ideation including active suicide plans, but also further confirmed severe EDS and heavy disruptive snoring [35]. Although the patient declined psychiatric hospitalisation and any antidepressant medication he agreed to a combined polygraphic sleep study corresponding to a severe sleep apnoae. After self-titration nCPAP treatment not only his sleep quality improved but there were no symptoms of depression and suicidal ideation two weeks later either and he stayed in remission until follow-up for three months [35]. Thus, depression with suicidal ideation may also occur as a symptom of untreated SAS in a medical emergency situation.
Further sleep disorders
Of note, there are no studies on suicidality in narcolepsy; however, one has to be aware that the occasional odd behaviour might be mistaken as suicidal action [36]. Another highly prevalent sleep disorder, the restless legs syndrome (RLS) is frequently comorbid with depressive syndromes possibly due to a monaminergic deficit (e.g., [37, 38]). Here, whether the RLS disorder itself or the treatment with dopaminergic drugs that are known to enhance impulsivity may also lead to subsequent suicidality is a matter of current debate [39].
Sleep disturbances in psychiatric disorders associated with suicidality
Patients with major depression are at highest suicide risk followed by patients addicted to alcohol and patients with schizophrenia [5]. At the same time sleep disturbances are frequent in patients with psychiatric disorders [9, 40, 41], e.g., about 75% of psychiatric inpatients were found to suffer from sleep disorders [40]. Sleep disturbances with complaints of insomnia or hypersomnia lead to a 2.5 fold rise in mental disorders [9]. Moreover, persistent insomnia is associated with much higher incidences of major depression (OR = 39.8, 95%, CI = 19.8–80.0) [42], but also some increase in anxiety disorder and substance dependence [42]. Deaths due to suicide were seen 7-fold enhanced over a one year period in patients with sleep disorders as opposed to age- and sex-matched controls but this effect concerned mainly patients with associated psychiatric diagnoses [41]. In a community-based prospective study (N = 14,456 including 21 completed suicides) over a 10-year period, poor sleep quality and depressive symptoms were among the factors that predicted late-life suicide [43].
Depression
Sleep disturbances and especially insomnia are a core symptom of depression [44, 45] and double the risk of developing a depression [46]. Although both entities share a common neurobiology like alterations in neurotransmission and genetic polymorphisms, hypothalamo-pituitary-adrenal (HPA) overactivity, or impaired neuronal plasticity [47] that are also important for suicidality (see below) only few studies in fact focused on analysing the relationship between these variables supporting the hypothesis that comorbid depression and sleep disturbances is related to suicidality.
Agargun et al. [48] demonstrated that poor subjective sleep quality as measured with the Pittsburgh Sleep Quality Inventory (PSQI) was associated with suicidal behaviour in major depression. Suicidal depressive patients reported significantly higher scores of subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency and PSQI global scores than non-suicidal patients. He also found higher rates of middle and terminal insomnia in suicide attempters with melancholic depression. In the group of non-melancholic depressed patients there was no such finding [29]. Besides, not only depressed patients with insomnia but also those with hypersomnia were significantly more likely to become suicidal than depressive patients without sleep disturbances [49]. However, in another outpatient study higher scores of suicidality were found in depressed patients with insomnia than in depressives with excessive sleepiness [50].
McCall et al. [51] identified insomnia as an indicator of suicidal ideation (suicide item taken from the Hamilton rating scale of depression, HRDS) during a clinical medication trial of SSRI and hypnotics (fluoxetine±eszopiclone) in comorbid depression and insomnia. The strong impact of insomnia is underlined as insomnia severity remained an independent factor of suicidal ideation even in the combination with the severity either of anhedonia or depressed mood [51]. Otherwise, patients who received treatment for their insomnia showed a decrease in their depressive symptoms [52] pointing to its potential secondary nature like Taylor [14] already commented that in some cases insomnia may be instigating, perpetuating or exacerbating depression.
Bipolar disorder
Sleep disturbances in patients with bipolar disorder are coming more into focus as impaired sleep may also be a predictor of manic episodes and residual insomnia or hypersomnia in the euthymic period may facilitate a bipolar relapse [53, 54]. Eidelmann et al. [55] found a positive correlation between the variability in falling asleep time and concurrent depressive symptoms while sleep efficiency positively correlated with concurrent manic symptoms. An association of psychomotor agitation and other non-euphoric hypomania symptoms with insomnia was observed in patients retrospectively classified as major depressive disorder (N = 314), and the agitated subsample also showed higher levels of suicidal ideation [56]. Summarising preliminary findings of sleep disturbances and suicidality in bipolar patients may point to some association, too. Whether sleep items included in charts of lifetime rhythmicity of manic depressive features might be identified as a potential marker for bipolar patients at risk for suicide [57] is another interesting approach for future research.
Schizophrenia
Sleep disorders are also common in patients with schizophrenia most notably insomnia with deficit in initiating and maintaining sleep [58] corresponding to polysomnographic findings of prolonged sleep-onset latency, a decrease in sleep efficiency and changes in REM- and NonREM sleep. Interestingly, enhanced REM-activity (rapid-eye-movement) and -time was found to be associated with suicidal behaviour in psychotic patients with schizophrenia or schizoaffective disorder while the difference against non-suicidal patients became less significant after excluding the schizoaffective suicidal patient group [59]. In line with these findings REM sleep time was increased in schizophrenia patients with suicidal ideation and attempts as opposed to non-suicidal schizophrenics [60]. Here, more detailed replication studies are needed to examine the potential independence of psychiatric diagnosis with regard to EEG abnormalities in suicidal behaviour. Of note, one would also have to take into account possible side effects of antipsychotics that may affect the sleep-wake rhythms negatively or even provoke parasomnias and accidental suicides [61].
Panic disorder and PTSD
Patients with panic disorder often complain about sleep disorders, especially sleep panic [62]. Some authors propose the highly frequent nocturnal panic attacks as a more severe variation of panic disorder [63]. The co-occurrence of panic disorder with major depression is extremely high [11, 62, 64, 66] and a vast majority of comorbid patients also experience insomnia [65, 66]. It is assumed that this comorbidity seems to be a potential modifier in developing suicidality. In an early study Fawcett et al. identified panic attacks and global insomnia among nine clinical features that were associated with suicide within 1 year in psychiatric patients with major affective disorders (N = 954) [64]. Moreover, recurrent sleep panickers showed an association with suicidal tendencies [66]. However, sleep panic alone was not found to be a risk factor for suicidality but it seems to be a decisive modifier towards a more severe panic disorder [62].
Among PTSD sufferers insomnia and nightmares are the most commonly reported subjective sleep disturbances [34, 67]. They even reported more weeks per year with sleep difficulties than subjects with other psychiatric disorders (adult separation anxiety, alcohol dependence, and major depression) [67]. Krakow et al. analysed sleep in female sexual assault survivors with PTSD and additional registering of sleep SRBD and sleep movement disorders. The women with both types of sleep disorder suffered from greater depression and suicidality [34].
Impulsivity, aggression, and substance abuse
Evidence for an association of personality features like impulsivity and aggression to sleep disturbances comorbid with suicidality is sparse and calls for expansion of studies. In patients with borderline personality disorder (BPD) difficulties in sleeping were seen to be associated with a higher risk of suicide attempts [57]. Some evidence also comes from a study of insomnia in male prisoners (N = 1,462), where insomnia was significantly related to actual suicidality as well as lifetime history of suicide attempts. Still, several confounders like axis 1 psychiatric disorder, childhood trauma, neuroticism, low resilience, and anger were significantly associated with insomnia [68].
Alcoholism is also associated with an increased risk of impulsivity and suicidal behaviour [69]. In alcoholic patients either with or without secondary depression increased REM density at admission and decreased total sleep time at about 2–4 weeks of abstinence predicted relapse three months later [70]. Sleep disturbance in alcoholic patients might therefore be a sign of worse outcome of illness and go along with a higher risk for suicidality.
Aetiological links of sleep disturbances und suicidality
Serotonin
Among the neurotransmitters serotonin is considered to be a major candidate for an aetiological link between sleep disturbances and suicidality [11]. Serotonin promotes waking states and the initiation of sleep with successive inhibition of slow wave sleep (SWS) and rapid-eye-movement (REM) sleep. Serotonergic neurons of the dorsal raphe nucleus steadily fire during waking but their release of serotonin declines during SWS and reaches its nadir during REM sleep [71]. Administration of several selective serotonergic receptor antagonists in rodents as well as in humans including those with chronic insomnia and mood disorders led to an increase of SWS and a reduction of REM sleep [72]. Contrariwise insomnia is related to reduced serotonergic function, e.g., sleep restriction for 4 h over 8 days led to a desensitisation of 5HT1A receptor system in rats [73].
In depression, SWS was correlated to serotonin metabolite (5-HIAA) in the cerebrospinal fluid, e.g. in depression [74]. SSRI treatment in depression resulted in REM suppression and impairment of sleep efficiency [75, 76], and the disruption of antidepressive treatments (SSRI, TCA) was followed by a fivefold increase in suicidal behaviours [77]. In addition, impairment of serotonergic activity was found after completed suicide in the brainstem and in the cerebrospinal fluid of suicide attempters and in individuals with high rates of violent aggression and impulsivity [3, 78–80], as well as reduced serotonin synthesis in the prefrontal cortex of suicide attempters [81]. Moreover, in patients with the same psychiatric diagnoses, the genotypes carrying the s allele of the serotonin transporter gene promoter (5-HTTLPR) were significantly more frequent in suicide attempters than in non-attempters (p = .004) [82].
The findings of a “low serotonin syndrome” in violent suicide attempts encouraged the hypothesis that serotonin is responsible for the relationship between sleep disturbances and suicide [11, 83–85]. Receiving not enough sleep is a problem of modern society like in Japan where sleep duration is the lowest in the world while suicidality is rising [6]. Kohyama suggested that people with sleep disturbances and a subsequent sleep debt are unlikely to perform sufficient physical activity to activate serotonergic activity to a desirable level [6]. While paradoxical sleep deprivation might increase the activity of the serotonergic system, total sleep debt is probably related to suicidality through reduced serotonin levels. But it was also argued that sleep deprivation is known to increase the activity of the serotonergic system and mood in depressed patients [86] though may not necessarily imply an association of sleep loss and serotonin in suicidality [87].
Some other neurotransmitter or hormonal candidates
However, a possible relationship between sleep depth and suicide cannot be decisively attributed to a single neurotransmitter system [84]. Recently a group of hypothalamic peptides is coming to the fore. The orexins or hypocretins are involved in the regulation of sleep, appetite and state of arousal. Patients (N = 101) who were enrolled shortly after suicide attempt showed a significant negative correlation between orexin in cerebrospinal fluid and global illness [88]. One might hypothesise that reduced orexin levels could therefore be involved in the aetiology of sleep disturbances and suicidality.
With regard to the HPA axis a dysfunction of cortisol secretion with increased levels in the evening nadir before sleep onset has been related to suicidality and suicide attempts in depression [89, 90]. Likewise a dysregulation of the delta sleep-inducing peptide (DSIP) and its association to cortisol secretion was suggested as candidate hormone in patients with major depression with suicide attempts [91].
EEG sleep abnormalities
Further evidence for a neurobiological link between sleep disturbances and suicidality is provided by polysomnographic studies. EEG sleep characteristics in depressed adults revealed an increase in REM sleep time (and phasic activity in the second REM period but less delta counts in the fourth Non-REM period) in the subgroup with a history of suicide attempts [92]. Similar sleep profiles with shortened REM latency and increase in REM percentage in suicidal ideation and behaviour were replicated in patients with depression or schizophrenic psychosis [59, 93]. In a study with depressed patients (N = 26), who underwent 3 nights of polysomnographic recordings subjects with higher suicidal scores, had a significantly shorter mean REM latency and a higher mean REM percentage than the non-suicidal subjects [93]. However, several EEG studies in depressed adolescents particularly underline the findings of an increase in REM activity [89]. Moreover, alterations of REM related negative dream like contents and associations with suicidal tendencies as suggested by Agargun et al. were interpreted as a failure to self-regulate mood and integrate affect into long-term memory networks during sleep [93].
Overall, these EEG alterations findings seem to represent an aggravation of sleep profiles in depression with loss of sleep continuity and loss of SWS as well as disinhibition of REM sleep with shortened REM latency and a high REM density also linked to corticoid overdrive and low serotonergic activity [47].
In general, there is a paucity of EEG studies that focus on the potential link between severity of suicidal ideation and behaviour to sleep profiles beyond of psychiatric disorder. However, polysomnography of nightmares for example show abrupt awakening usually from REM sleep typically lasting for about 10 min in association with vivid dreamlike features [94] on the one hand. Here, REM suppressing serotonergic antidepressant agents with may be of help. On the other hand, polysomnographic findings of difficulties of initiating sleep and/or maintaining sleep in insomnia show a loss of SWS and REM going along with an increase in sleep latency and awakenings and reduced sleep efficiency [94]. Here, 5HT2 receptor antagonists may improve SWS in these individuals. Similar serotonergic agents that enhance serotonergic neurotransmission decrease aggression, impulsivity, and suicidal behaviour [83], and the underlying neurobiological link between the EEG abnormalities in sleep disturbances and suicidality needs special focus in particular studies.
Hypnotics
Hypnotics have been related to an increase in mortality in the general population [12, 95]. In contrast, positive effects of hypnotics on insomnia in depression have been demonstrated (e.g. [96]) but no such study focused on items of suicidal ideation as it was often postulated as an exclusion criterion [97] or this piece of information was not given [51].
Nonetheless, the use of sedatives-hypnotics (in particular zolpidem and zaleplon) was a stronger predictor for suicidal thoughts and attempts than insomnia in household respondents (N = 5,692) [98]. In the elderly (+65) population sedative treatment even revealed a 14-fold increase of risk for late life suicide, and after adjustment for psychiatric (DSM-IV) disorders, only hypnotics but not antidepressants and antipsychotics still represented an independent risk factor for suicide [99]. Prescriptions of sedatives-hypnotics in the preceding 12 months were associated with suicidal thoughts, plans and attempts [98, 99], and a current prescription of hypnotics still leads to a four-fold increase in suicide risk in the elderly [99].
With regard to the use of antidepressants effective in treatment of depression the unclear issue of SSRI facilitating suicide has been analysed. There may be an associated protective factor of suicide attempt in adults and elderly with depression while the risk of suicide attempt may be increased among adolescents [100]. High dose-stimulant therapy in narcolepsy or idiopathic hypersomnia was not found to be related to suicide-related behaviours [101].
Circadian rhythms
The influence of biological and social “zeitgebers” is reflected in the diurnal variability of suicide attempts and deliberate self-injuries with a peak in the evening but completed suicides in the early morning (see overview in [83]). In line are findings in adolescents who were 24% more likely to suffer from depression (OR = 1.24) and 20% more likely to have suicidal ideation (OR = 1.20) with parentally set bedtimes of midnight or later than with early set bedtimes [102].
Chronobiology divides individuals into two chronotypes with morning types initiating their activities in the first hours of the day whereas evening types start later in the day with a larger variability in bed and rising times. Recent findings suggest that the development of major depression and sleep disorders is linked to a patients’ biological chronotype. While circadian morningness type may be a significant relief factor in depression the eveningness type has been linked with impulsivity and may represent a risk factor for suicidality, most notably of violent suicide attempts [103]. Here, the role of melatonin to circadian rhythms, sleep disturbances and suicidality remains open to research [104] as well as the role of a variety of potential circadian genes [105].
Shift work like other potential conditions leading to disruption of circadian rhythms might result in disruption of different psychological and physiological processes. An association of shift work and suicidal ideation was shown in policewomen with higher depressive symptoms and increase in day shift time hours, and among their male colleagues with higher PTSD symptoms with increasing afternoon hours [106]. Thus, interventions in shift work and jet lag should always be considered in patients with recurrent mood disorders, or at risk for suicide [107].
Psychological factors
Sociodemographic risk factors, e.g., education, financial income, employment, marital status, conflicts in partnership have a strong impact on suicidality [4, 7, 108], and here poor sleep may act as an additional stressor. However, the link of social stressors like work-related stress or unemployment and altered diurnal rhythms to comorbidity of sleep disturbances and suicide attempts or completed suicides remains an open question and a high number of unreported cases have to be assumed. Apart from the psychological variables impulsivity or aggression that are closely linked to the interplay between serotonin dysfunction and suicidality [78, 79], hopelessness belongs to the main psychological constructs that may act as moderators of suicidality [109]. Similarly, hopelessness has also been identified as a dysfunctional cognition that maintains maladaptive beliefs in sleep in chronic insomniacs [110] as well as in depressed insomniacs [111]. Hence, hopelessness in ever overcoming sleep problems would be one item of interest in sleep oriented assessment of suicidal tendencies. In fact, Fawcett et al. [64] noted hopelessness as one of nine features in depressed patients that was associated with suicide within one year. However, to further speculate about the role of potential psychosocial factors known to contribute to sleep disturbances—either comorbid with psychiatric disorders or not—resulting in suicidality would be out of the scope of this overview and these complex associations have not particularly been focused in studies so far.
Limitations
Current research lack studies with profound methodological designs addressing the particular issue on sleep loss or disturbances and suicidality including neurobiological markers. Most studies rely on subjective estimations on sleep and sleep variables only and there are hardly any objective measurements or only small polysomnographic recording EEG studies to verify sleep loss or sleep disorders in suicidality. Several prospective studies concentrating on the target syndromes like insomnia or nightmares have been linked to suicidality but were either non-clinical or cross-sectional and are not based on diagnostic interviews or examinations. Apart from Krakow et al. [34] there is a paucity of formal polysomnographic sleep studies resulting in diagnoses on sleep disorders and suicidality. On the other hand, results of clinical studies focusing on this link cannot be compared to sleep problems in the general population. Then, sometimes suicide items were taken from established investigator-rated questionnaires, e.g., for assessment of depression but were not primarily addressing different items of suicidality.
Moreover, the suggested bidirectional link between sleep disturbances or polysomnographic sleep abnormalities and suicidality on the basis of psychiatric disorders as a common pathway [11] cannot be entirely supported, as sleep disturbances frequently predicted suicidality independent of psychiatric diagnoses [5, 13, 17, 24, 25, 51]. In addition, a large number of confounders complicate the interpretation of findings. Among them and yet not properly identified are various chronic medical conditions related to insomnia that may also be a factor as risk for successive insomnia [112] as well as for suicidality [113].
Preventing suicide by risk assessment and treatment of sleep disturbances [Fig. 1]
Fig. 1.
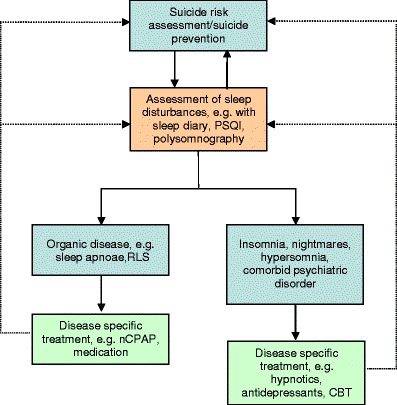
Assessment and treatment of sleep disturbances in suicide prevention
Personalised medicine applies particularly to the field to suicidality and individual patients’ needs. As opposed to managed care protocols physicians have to identify individual risk factors and treatment strategies decisions, and higher awareness of the potential link between sleep problems and suicidality is needed. Individuals, who suffer from sleep disturbances that may be a symptom of psychiatric distress or suicidality, do not frequently search for formal mental health treatment [16]. However, sleep disturbances represent a “modifiable” risk factor [64] of suicidality giving it a unique position among other risk factors. Sleep medicine interventions may be an option in secondary preventive programmes after suicide attempts or even qualify as a tool of primary prevention.
Identification of vulnerable individuals at high risk calls for a careful assessment of sleep and sleeping habits. Here, an individualised assessment is essential to identifying relevant risk factors. This assessment of individual sleep history and complains would also have to be included in the assessment of suicide risk factors (e.g., sociodemographic risk factors, current stressors, previous history of suicide attempts, substance abuse, family history). Further simple measures like psychometric instruments for sleep complains and sleep quality as well as sleep diaries may be included in the individual diagnostic procedure as well as advanced technology in sleep medicine diagnostics like ambulatory polysomnography. Differential diagnosis including organic diagnosis and disease specific treatments of sleep apnoae or restless legs seems mandatory.
Instructions in sleep hygiene are to be given as a basic principle for example lengthening sleep duration or setting regular bedtimes that could be protective against depression and suicidal ideation [84, 101]. The presence of insomnia or nightmares comorbid with depression will probably always demand an assessment of suicide risk and further actions while specific sleep medicine inventions like drug treatment are available for disorders like insomnia and nightmares suspected to enhance suicidal tendencies. In the hypnotic treatment one would have to take care of potential side effects with enhanced suicidality or consider non-pharmacologic strategies. One might also consider psychotherapy including cognitive behaviour therapy (CBT), interpersonal therapy (IPT) or dialectic behavioural therapy (DBT) to reduce suicidal tendencies in the context of depression, aggression or impulsivity. Moreover, therapeutic efforts in stabilising social rhythms [114] in mania, depression or beyond may not only promote stable sleep patterns and reduction of sleep disturbances but also prevent suicidal tendencies in a high risk patient population.
Potential impact of regular exercise on sleep behaviour and suicidality
Regular exercise appears to substantially improve sleep quality especially in less active individuals with sleep complaints as well as in patients with chronic insomnia [115–118]. On the other hand, the beneficial effect of exercise on mental health and psychic disorder especially depression is well established (e.g., [119, 120]). Physical activity is not only known for a strong protective association with depressive syndromes [121, 122] but also to reduce rates of rates of suicidal ideation [121], suicide attempts [122, 123] and completed suicides [124]. Potential mediators for the positive impact of regular exercise on sleep behaviour and suicidality possibly include affective, functional, and metabolic mediators specific to sleep architecture parameters [118] along with increase in self-esteem and perceived social support during sport participation [122]. Thus, regular and moderate physical activity should belong to the recommendations in individuals with sleep disturbances, who might also be at risk of low mood and suicidality.
Conclusion and outlook
Currently the available epidemiological and clinical studies strongly point to a link between sleep loss or sleep disturbances and suicidality, i.e., suicide ideation, suicide attempts or completed suicide. This seems to apply in particular for insomnia and nightmares that should at least be taken as a warning sign for precise assessment of suicidality. Most sleep problems or defined sleep disorders represent a treatable risk factor at comparatively low cost as opposed to the more complex suicide prevention strategies and programmes that are still not sufficiently effective.
Moreover, if sleep disturbances would in fact emerge as an independent predictive risk factor for suicidal tendencies and actions—as some of the studies suggest after adjustment for confounding factors and illnesses (e.g., depression, PTSD, alcohol)—Pigeon and Caine pose the question whether it is still premature to include sleep interventions in suicide prevention efforts or even imperative [85]. Kohyhama proposed that public health initiatives encouraging a longer duration of sleep may provide a simple way of prevention either in primary or secondary prevention in a high risk population [84]. At this stage prospective sleep studies and more objective measures of sleep disturbances, neurobiological and circadian variables are urgently warranted to enlighten the association of suicidality either with or without psychiatric disorders, to promote preventions and targeted therapies in reducing suicidal tendencies in vulnerable individuals, and to define the role of sleep medicine interventions in this area.
Assessment and treatment of individual sleep disturbances might represent a personalised preventive measure of suicidality and suicide behaviour and should therefore be included in everyday routine clinical history as well as in be especially targeted in primary and secondary suicide prevention programmes.
Acknowledgements
Parts of this work were supported by a grant given to the authors and were founded by the “STIFTUNG DEPRESSIONSFORSCHUNG”, Berlin/Germany, a registered non-profit organisation foundation of research in depression.
References
- 1.CDC. http://www.cdc.gov/Features/PreventingSuicide/ Accessed 30 April 2011.
- 2.Federal Statistical Office Germany “Statistisches Bundesamt. Ergebnisse der Todesursachenstatistik für Deutschland“. 2009. http://www.destatis.de/jetspeed/portal/cms/Sites/destatis/Internet/DE/Content/Publikationen/Fachveroeffentlichungen/Gesundheit/Todesursachen/Todesursachenstatistik5232101097015,property=file.xls Accessed 30 April 2011.
- 3.Mann JJ. Neurobiology of suicidal behavior. Nat Rev Neurosci. 2003;4:819–828. doi: 10.1038/nrn1220. [DOI] [PubMed] [Google Scholar]
- 4.Agerbo E. High income, employment, postgraduate education, and marriage: a suicidal cocktail among psychiatric patients. Arch Gen Psychiatry. 2007;64:1377–1384. doi: 10.1001/archpsyc.64.12.1377. [DOI] [PubMed] [Google Scholar]
- 5.Bertolote JM, Mello-Santos C, Botega NJ. Detecting suicide risk at psychiatric emergency services. Rev Bras Psiquiatr. 2010;32:87–95. doi: 10.1590/S1516-44462010000600005. [DOI] [PubMed] [Google Scholar]
- 6.Kohyama J. Sleep, serotonin, and suicide in Japan. J Physiol Anthropol. 2011;30:1–8. doi: 10.2114/jpa2.30.1. [DOI] [PubMed] [Google Scholar]
- 7.Pompili M, Innamorati M, Szanto K, Vittorio C, Conwell Y, Lester D, Tatarelli R, Girardi P, Amore M. Life events as precipitants of suicide attempts among first-time suicide attempters, repeaters, and non-attempters. Psychiatry Res. 2011;186:300–305. doi: 10.1016/j.psychres.2010.09.003. [DOI] [PubMed] [Google Scholar]
- 8.Mann JJ, Apter A, Bertolote J, Beautrais A, Currier D, Haas A, Hegerl U, Lonnqvist J, Malone K, Marusic A, Mehlum L, Patton G, Phillips M, Rutz W, Rihmer Z, Schmidtke A, Shaffer D, Silverman M, Takahashi Y, Varnik A, Wasserman D, Yip P, Hendin H. Suicide prevention strategies: a systematic review. JAMA. 2005;294:2064–2074. doi: 10.1001/jama.294.16.2064. [DOI] [PubMed] [Google Scholar]
- 9.Ford DE, Kamerow DB. Epidemiologic study of sleep disturbances and psychiatric disorders. An opportunity for prevention? JAMA. 1989;262:1479–1484. doi: 10.1001/jama.262.11.1479. [DOI] [PubMed] [Google Scholar]
- 10.Ohayon M. Epidemiology of insomnia: what we know and what we still need to learn. Sleep Med Rev. 2002;6:97–111. doi: 10.1053/smrv.2002.0186. [DOI] [PubMed] [Google Scholar]
- 11.Singareddy RK, Balon R. Sleep and suicide in psychiatric patients. Ann Clin Psychiatry. 2001;13:93–101. doi: 10.1023/a:1016619708558. [DOI] [PubMed] [Google Scholar]
- 12.Kripke DF, Garfinkel L, Wingard DL, Klauber MR, Marler MR. Mortality associated with sleep duration and insomnia. Arch Gen Psychiatry. 2002;59:131–136. doi: 10.1001/archpsyc.59.2.131. [DOI] [PubMed] [Google Scholar]
- 13.Bernert RA, Joiner TE, Jr, Cukrowicz KC, Schmidt NB, Krakow B. Suicidality and sleep disturbances. Sleep. 2005;28:1135–1141. doi: 10.1093/sleep/28.9.1135. [DOI] [PubMed] [Google Scholar]
- 14.Taylor DJ. Insomnia and depression. Sleep. 2008;31:447–448. doi: 10.1093/sleep/31.4.447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Goodwin RD, Marusic A. Association between short sleep and suicidal ideation and suicide attempt among adults in the general population. Sleep. 2008;31:1097–1101. [PMC free article] [PubMed] [Google Scholar]
- 16.Wojnar M, Ilgen MA, Wojnar J, McCammon RJ, Valenstein M, Brower KJ. Sleep problems and suicidality in the National Comorbidity Survey Replication. J Psychiatr Res. 2009;43:526–531. doi: 10.1016/j.jpsychires.2008.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Li SX, Lam SP, Yu MW, Zhang J, Wing YK. Nocturnal sleep disturbances as a predictor of suicide attempts among psychiatric outpatients: a clinical, epidemiologic, prospective study. J Clin Psychiatry. 2010;71:1440–1446. doi: 10.4088/JCP.09m05661gry. [DOI] [PubMed] [Google Scholar]
- 18.Rod NH, Vahtera J, Westerlund H, Kivimaki M, Zins M, Goldberg M, Lange T. Sleep disturbances and cause-specific mortality: results from the GAZEL cohort study. Am J Epidemiol. 2011;173:300–309. doi: 10.1093/aje/kwq371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chin YR, Lee HY, So ES. Suicidal ideation and associated factors by sex in Korean adults: a population-based cross-sectional survey. Int J Public Health. 2011. doi:10.1007/s00038-011-0245-9. [DOI] [PubMed]
- 20.Liu X. Sleep and adolescent suicidal behavior. Sleep. 2004;27:1351–1358. doi: 10.1093/sleep/27.7.1351. [DOI] [PubMed] [Google Scholar]
- 21.Yen CF, King BH, Tang TC. The association between short and long nocturnal sleep durations and risky behaviours and the moderating factors in Taiwanese adolescents. Psychiatry Res. 2010;179:69–74. doi: 10.1016/j.psychres.2009.02.016. [DOI] [PubMed] [Google Scholar]
- 22.Blasco-Fontecilla H, Alegria AA, Lopez-Castroman J, Legido-Gil T, Saiz-Ruiz J, de Leon J, Baca-Garcia E. Short self-reported sleep duration and suicidal behavior: a cross-sectional study. J Affect Disord. 2011. doi:10.1016/j.jad.2011.04.003. [DOI] [PubMed]
- 23.Hall RC, Platt DE, Hall RC. Suicide risk assessment: a review of risk factors for suicide in 100 patients who made severe suicide attempts. Evaluation of suicide risk in a time of managed care. Psychosomatics. 1999;40:18–27. doi: 10.1016/S0033-3182(99)71267-3. [DOI] [PubMed] [Google Scholar]
- 24.Sjöström N, Waern M, Hetta J. Nightmares and sleep disturbances in relation to suicidality in suicide attempters. Sleep. 2007;30:91–95. doi: 10.1093/sleep/30.1.91. [DOI] [PubMed] [Google Scholar]
- 25.Krakow B, Ribeiro JD, Ulibarri VA, Krakow J, Joiner TE Jr. Sleep disturbances and suicidal ideation in sleep medical center patients. J Affect Disord. 2011;131:422–7. [DOI] [PubMed]
- 26.Sjöström N, Hetta J, Waern M. Persistent nightmares are associated with repeat suicide attempt: a prospective study. Psychiatry Res. 2009;170(2–3):208–211. doi: 10.1016/j.psychres.2008.09.006. [DOI] [PubMed] [Google Scholar]
- 27.Tanskanen A, Tuomilehto J, Viinamäki H, Vartiainen E, Lehtonen J, Puska P. Nightmares as predictors of suicide. Sleep. 2001;24:844–847. [PubMed] [Google Scholar]
- 28.Ağargün MY, Cilli AS, Kara H, Tarhan N, Kincir F, Oz H. Repetitive and frightening dreams and suicidal behavior in patients with major depression. Compr Psychiatry. 1998;39:198–202. doi: 10.1016/S0010-440X(98)90060-8. [DOI] [PubMed] [Google Scholar]
- 29.Ağargün MY, Besiroglu L, Cilli AS, Gulec M, Aydin A, Inci R, Selvi Y. Nightmares, suicide attempts, and melancholic features in patients with unipolar major depression. J Affect Disord. 2007;98:267–270. doi: 10.1016/j.jad.2006.08.005. [DOI] [PubMed] [Google Scholar]
- 30.Mahowald MW, Schenck CH, Goldner M, Bachelder V, Cramer-Bornemann M. Parasomnia pseudo-suicide. J Forensic Sci. 2003;48:1158–1162. [PubMed] [Google Scholar]
- 31.Yeh SB, Schenck CH. A case of marital discord and secondary depression with attempted suicide resulting from REM sleep behavior disorder in a 35-year-old woman. Sleep Med. 2004;5:151–154. doi: 10.1016/j.sleep.2003.09.008. [DOI] [PubMed] [Google Scholar]
- 32.Chellappa SL, Araújo JF. Excessive daytime sleepiness in patients with depressive disorder. Rev Bras Psiquiatr. 2006;28:126–129. doi: 10.1590/S1516-44462006000200010. [DOI] [PubMed] [Google Scholar]
- 33.Skobel E, Norra C, Sinha A, Breuer C, Hanrath P, Stellbrink C. Impact of sleep-related breathing disorders on health-related quality of life in patients with chronic heart failure. Eur J Heart Fail. 2005;7:505–511. doi: 10.1016/j.ejheart.2004.07.020. [DOI] [PubMed] [Google Scholar]
- 34.Krakow B, Artar A, Warner TD, Melendrez D, Johnston L, Hollifield M, Germain A, Koss M. Sleep disorder, depression, and suicidality in female sexual assault survivors. Crisis. 2000;21:163–170. doi: 10.1027//0227-5910.21.4.163. [DOI] [PubMed] [Google Scholar]
- 35.Krahn LE, Miller BW, Bergstrom LR. Rapid resolution of intense suicidal ideation after treatment of severe obstructive sleep apnea. J Clin Sleep Med. 2008;4:64–65. [PMC free article] [PubMed] [Google Scholar]
- 36.Bell M, Tate L, Fowler DL. Narcolepsy mimicking suicidal carbon monoxide poisoning. Am J Forensic Med Pathol. 1989;10:226–228. doi: 10.1097/00000433-198909000-00011. [DOI] [PubMed] [Google Scholar]
- 37.Norra C, Töpfer R, Stegelmeyer U, Wälte D, Saß H. Subjective ratings of psychopathological symptoms and impaired quality of life in Restless Legs Syndrome. Sleep Res Online. 1999;2:311. [Google Scholar]
- 38.Hornyak M, Benes H, Eisensehr I, Haan J, Kassubek J, Peglau I, et al. Depression in restless legs syndrome. Pathogenesis, assessment, and implications for treatment. Nervenarzt. 2009;80:1160–6, 1164–6, 1168. [DOI] [PubMed]
- 39.Dang D, Cunnington D, Swieca J. The emergence of devastating impulse control disorders during dopamine agonist therapy of the restless legs syndrome. Clin Neuropharmacol. 2011;34:66–70. doi: 10.1097/WNF.0b013e31820d6699. [DOI] [PubMed] [Google Scholar]
- 40.Benca RM. Sleep in psychiatric disorders. Neurol Clin. 1996;14:739–764. doi: 10.1016/S0733-8619(05)70283-8. [DOI] [PubMed] [Google Scholar]
- 41.Wallander MA, Johansson S, Ruigómez A, García Rodríguez LA, Jones R. Morbidity associated with sleep disorders in primary care: a longitudinal cohort study. Prim Care Companion J Clin Psychiatry. 2007;9:338–345. doi: 10.4088/PCC.v09n0502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Breslau N, Roth T, Rosenthal L, Andreski P. Sleep disturbance and psychiatric disorders: a longitudinal epidemiological study of young adults. Biol Psychiatry. 1996;39:411–418. doi: 10.1016/0006-3223(95)00188-3. [DOI] [PubMed] [Google Scholar]
- 43.Turvey CL, Conwell Y, Jones MP, Phillips C, Simonsick E, Pearson JL, Wallace R. Risk factors for late-life suicide: a prospective, community-based study. Am J Geriatr Psychiatry. 2002;10:398–406. [PubMed] [Google Scholar]
- 44.American Psychiatric Association (APA). Diagnostic and statistical manual of mental disorders, 5th edn. DSM-IV-TR. Washington, DC: APA; 2000.
- 45.Tsuno N, Besset A, Ritchie K. Sleep and depression. J Clin Psychiatry. 2005;66:1254–1269. doi: 10.4088/JCP.v66n1008. [DOI] [PubMed] [Google Scholar]
- 46.Baglioni C, Battagliese G, Feige B, Spiegelhalder K, Nissen C, Voderholzer U, et al. Insomnia as a predictor of depression: a meta-analytic evaluation of longitudinal epidemiological studies. J Affect Disord. 2011. doi:10.1016/j.jad.2011.01.011. [DOI] [PubMed]
- 47.Benca RM, Peterson MJ. Insomnia and depression. Sleep Med. 2008;9:3–9. doi: 10.1016/S1389-9457(08)70010-8. [DOI] [PubMed] [Google Scholar]
- 48.Ağargün MY, Kara H, Solmaz M. Subjective sleep quality and suicidality in patients with major depression. J Psychiatr Res. 1997;31:377–381. doi: 10.1016/S0022-3956(96)00037-4. [DOI] [PubMed] [Google Scholar]
- 49.Ağargün MY, Kara H, Solmaz M. Sleep disturbances and suicidal behavior in patients with major depression. J Clin Psychiatry. 1997;58:249–251. doi: 10.4088/JCP.v58n0602. [DOI] [PubMed] [Google Scholar]
- 50.Chellappa SL, Araújo JF. Sleep disorders and suicidal ideation in patients with depressive disorder. Psychiatry Res. 2007;153:131–136. doi: 10.1016/j.psychres.2006.05.007. [DOI] [PubMed] [Google Scholar]
- 51.McCall WV, Blocker JN, D’Agostino R, Jr, Kimball J, Boggs N, Lasater B, Rosenquist PB. Insomnia severity is an indicator of suicidal ideation during a depression clinical trial. Sleep Med. 2010;11:822–827. doi: 10.1016/j.sleep.2010.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Isaac F, Greenwood KM. The relationship between insomnia and depressive symptoms: genuine or artifact? Neuropsychiatr Dis Treat. 2011;7:57–63. doi: 10.2147/NDT.S16267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Plante DT, Winkelman JW. Sleep disturbance in bipolar disorder: therapeutic implications. Am J Psychiatry. 2008;165:830–843. doi: 10.1176/appi.ajp.2008.08010077. [DOI] [PubMed] [Google Scholar]
- 54.Kaplan KA, Gruber J, Eidelman P, Talbot LS, Harvey AG. Hypersomnia in inter-episode bipolar disorder: does it have prognostic significance? J Affect Disord. 2011. doi:10.1016/j.jad.2011.03.013. [DOI] [PMC free article] [PubMed]
- 55.Eidelman P, Talbot LS, Gruber J, Harvey AG. Sleep, illness course, and concurrent symptoms in inter-episode bipolar disorder. J Behav Ther Exp Psychiatry. 2010;41:145–149. doi: 10.1016/j.jbtep.2009.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Olgiati P, Serretti A, Colombo C. Retrospective analysis of psychomotor agitation, hypomanic symptoms, and suicidal ideation in unipolar depression. Depress Anxiety. 2006;23:389–397. doi: 10.1002/da.20191. [DOI] [PubMed] [Google Scholar]
- 57.Balestrieri M, Rucci P, Sbrana A, Ravani L, Benvenuti A, Gonnelli C, et al. Lifetime rhythmicity and mania as correlates of suicidal ideation and attempts in mood disorders. Compr Psychiatry. 2006;47:334–341. doi: 10.1016/j.comppsych.2006.01.004. [DOI] [PubMed] [Google Scholar]
- 58.Monti JM, Monti D. Sleep disturbance in schizophrenia. Int Rev Psychiatry. 2005;17:247–253. doi: 10.1080/09540260500104516. [DOI] [PubMed] [Google Scholar]
- 59.Keshavan MS, Reynolds CF, Montrose D, Miewald J, Downs C, Sabo EM. Sleep and suicidality in psychotic patients. Acta Psychiatr Scand. 1994;89:122–125. doi: 10.1111/j.1600-0447.1994.tb01498.x. [DOI] [PubMed] [Google Scholar]
- 60.Lewis CF, Tandon R, Shipley JE, DeQuardo JR, Jibson M, Taylor SF, Goldman M. Biological predictors of suicidality in schizophrenia. Acta Psychiatr Scand. 1996;94:416–420. doi: 10.1111/j.1600-0447.1996.tb09883.x. [DOI] [PubMed] [Google Scholar]
- 61.Seeman MV. Sleepwalking, a possible side effect of antipsychotic medication. Psychiatr Q. 2011;82:59–67. doi: 10.1007/s11126-010-9149-8. [DOI] [PubMed] [Google Scholar]
- 62.Ağargün MY, Kara H. Recurrent sleep panic, insomnia, and suicidal behavior in patients with panic disorder. Compr Psychiatry. 1998;39:149–151. doi: 10.1016/S0010-440X(98)90074-8. [DOI] [PubMed] [Google Scholar]
- 63.Merritt-Davis O, Balon R. Nocturnal panic: biology, psychopathology, and its contribution to the expression of panic disorder. Depress Anxiety. 2003;18:221–227. doi: 10.1002/da.10150. [DOI] [PubMed] [Google Scholar]
- 64.Fawcett J, Scheftner WA, Fogg L, Clark DC, Young MA, Hedeker D, Gibbons R. Time-related predictors of suicide in major affective disorder. Am J Psychiatry. 1990;147:1189–1194. doi: 10.1176/ajp.147.9.1189. [DOI] [PubMed] [Google Scholar]
- 65.Singareddy RK, Uhde TW. Nocturnal sleep panic and depression: relationship to subjective sleep in panic disorder. J Affect Disord. 2009;112:262–266. doi: 10.1016/j.jad.2008.04.026. [DOI] [PubMed] [Google Scholar]
- 66.Singareddy RK, Balon R. Sleep in posttraumatic stress disorder. Ann Clin Psychiatry. 2002;14:183–190. doi: 10.1023/a:1021190620773. [DOI] [PubMed] [Google Scholar]
- 67.Lauterbach D, Behnke C, McSweeney LB. Sleep problems among persons with a lifetime history of posttraumatic stress disorder alone and in combination with a lifetime history of other psychiatric disorders: a replication and extension. Compr Psychiatry. 2011. doi:10.1016/j.comppsych.2011.01.007. [DOI] [PubMed]
- 68.Carli V, Roy A, Bevilacqua L, Maggi S, Cesaro C, Sarchiapone M. Insomnia and suicidal behaviour in prisoners. Psychiatry Res. 2011;185:141–144. doi: 10.1016/j.psychres.2009.10.001. [DOI] [PubMed] [Google Scholar]
- 69.Sher L. Alcoholism and suicidal behavior: a clinical overview. Acta Psychiatr Scand. 2006;113:13–22. doi: 10.1111/j.1600-0447.2005.00643.x. [DOI] [PubMed] [Google Scholar]
- 70.Clark CP, Gillin JC, Golshan S, Demodena A, Smith TL, Danowski S, Irwin M, Schuckit M. Increased REM sleep density at admission predicts relapse by three months in primary alcoholics with a lifetime diagnosis of secondary depression. Biol Psychiatry. 1998;43:601–607. doi: 10.1016/S0006-3223(97)00457-5. [DOI] [PubMed] [Google Scholar]
- 71.Ursin R. Serotonin and sleep. Sleep Med Rev. 2002;6:57–69. doi: 10.1053/smrv.2001.0174. [DOI] [PubMed] [Google Scholar]
- 72.Monti JM. Serotonin control of sleep-wake behavior. Sleep Med Rev. 2011;15:269–81. [DOI] [PubMed]
- 73.Roman V, Walstra I, Luiten PG, Meerlo P. Too little sleep gradually desensitizes the serotonin 1A receptor system. Sleep. 2005;28:1505–1510. [PubMed] [Google Scholar]
- 74.Benson KL, Faull KF, Zarcone VP., Jr The effects of age and serotonergic activity on slow-wave sleep in depressive illness. Biol Psychiatry. 1993;33:842–844. doi: 10.1016/0006-3223(93)90027-B. [DOI] [PubMed] [Google Scholar]
- 75.Trivedi MH, Rush AJ, Armitage R. Effects of fluoxetine on the polysomnogram in outpatients with major depression. Neuropsychopharmacology. 1999;10:447–459. doi: 10.1016/S0893-133X(98)00131-6. [DOI] [PubMed] [Google Scholar]
- 76.Vogel GW, Buffenstein A, Minter K, Hennessey A. Drug effects on REM sleep and on endogenous depression. Neurosci Biobehav Rev. 1990;14:49–63. doi: 10.1016/S0149-7634(05)80159-9. [DOI] [PubMed] [Google Scholar]
- 77.Yerevanian BI, Koek RJ, Feusner JD, Hwang S, Mintz J. Antidepressants and suicidal behaviour in unipolar depression. Acta Psychiatr Scand. 2004;110:452–458. doi: 10.1111/j.1600-0447.2004.00437.x. [DOI] [PubMed] [Google Scholar]
- 78.Asberg M. Neurotransmitters and suicidal behavior. The evidence from cerebrospinal fluid studies. Ann N Y Acad Sci. 1997;836:158–181. doi: 10.1111/j.1749-6632.1997.tb52359.x. [DOI] [PubMed] [Google Scholar]
- 79.Linnoila VM, Virkkunen M. Aggression, suicidality, and serotonin. J Clin Psychiatry. 1992;53:46–51. [PubMed] [Google Scholar]
- 80.Mann JJ, Brent DA, Arango V. The neurobiology and genetics of suicide and attempted suicide: a focus on the serotonergic system. Neuropsychopharmacology. 2001;24:467–477. doi: 10.1016/S0893-133X(00)00228-1. [DOI] [PubMed] [Google Scholar]
- 81.Leyton M, Paquette V, Gravel P, Rosa-Neto P, Weston F, Diksic M. Benkelfat, alpha-[11C]Methyl-L-tryptophan trapping in the orbital and ventral medial prefrontal cortex of suicide attempters. Eur Neuropsychopharmacol. 2006;16:220–223. doi: 10.1016/j.euroneuro.2005.09.006. [DOI] [PubMed] [Google Scholar]
- 82.Lin P, Tsai G. Association between serotonin transporter gene promoter polymorphism and suicide: results of a meta-analysis. Biol Psychiatry. 2004;55:1023–1030. doi: 10.1016/j.biopsych.2004.02.006. [DOI] [PubMed] [Google Scholar]
- 83.Bernert RA, Joiner TE. Sleep disturbances and suicide risk: a review of the literature. Neuropsychiatr Dis Treat. 2007;3:735–743. doi: 10.2147/ndt.s1248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Kohyama J. More sleep will bring more serotonin and less suicide in Japan. Med Hypotheses. 2010;75:340. doi: 10.1016/j.mehy.2010.03.035. [DOI] [PubMed] [Google Scholar]
- 85.Pigeon WR, Caine ED. Insomnia and the risk for suicide: does sleep medicine have interventions that can make a difference? Sleep Med. 2010;11:816–817. doi: 10.1016/j.sleep.2010.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Adrien J. Neurobiological bases for the relation between sleep and depression. Sleep Med Rev. 2002;6:341–345. [PubMed] [Google Scholar]
- 87.Pires GN, Andersen ML, Kahan V, Araujo P, Galduróz JC, Tufik S. Is serotonin responsible for the relationship between sleep debt and suicide? A comment on Kohyama’s hypothesis. Med Hypotheses. 2010;75:675. doi: 10.1016/j.mehy.2010.07.015. [DOI] [PubMed] [Google Scholar]
- 88.Brundin L, Petersén A, Björkqvist M, Träskman-Bendz L. Orexin and psychiatric symptoms in suicide attempters. J Affect Disord. 2007;100:259–263. doi: 10.1016/j.jad.2006.10.019. [DOI] [PubMed] [Google Scholar]
- 89.Dahl RE, Puig-Antich J, Ryan ND, Nelson B, Dachille S, Cunningham SL, Trubnick L, Klepper TP. EEG sleep in adolescents with major depression: the role of suicidality and inpatient status. J Affect Disord. 1990;19:63–75. doi: 10.1016/0165-0327(90)90010-6. [DOI] [PubMed] [Google Scholar]
- 90.Mathew SJ, Coplan JD, Goetz RR, Feder A, Greenwald S, Dahl RE, Ryan ND, Mann JJ, Weissman MM. Differentiating depressed adolescent 24 h cortisol secretion in light of their adult clinical outcome. Neuropsychopharmacology. 2003;28:1336–1343. doi: 10.1038/sj.npp.1300184. [DOI] [PubMed] [Google Scholar]
- 91.Westrin A, Ekman R, Träskman-Bendz L. High delta sleep-inducing peptide-like immunoreactivity in plasma in suicidal patients with major depressive disorder. Biol Psychiatry. 1998;43:734–739. doi: 10.1016/S0006-3223(97)00254-0. [DOI] [PubMed] [Google Scholar]
- 92.Sabo E, Reynolds C, Kupfer D, Berman SR. Sleep, depression and suicide. Psychiatry Res. 1991;36:265–277. doi: 10.1016/0165-1781(91)90025-K. [DOI] [PubMed] [Google Scholar]
- 93.Ağargün MY, Cartwright R. REM sleep, dream variables and suicidality in depressed patients. Psychiatry Res. 2003;119:33–39. doi: 10.1016/S0165-1781(03)00111-2. [DOI] [PubMed] [Google Scholar]
- 94.American Academy of Sleep Medicine. International classification of sleep disorders, 2nd edn. Diagnostic and coding manual. American Academy of Sleep Medicine, Westchester, IL; 2005.
- 95.Mallon L, Broman JE, Hetta J. Is usage of hypnotics associated with mortality? Sleep Med. 2009;10:279–286. doi: 10.1016/j.sleep.2008.12.004. [DOI] [PubMed] [Google Scholar]
- 96.Londborg PD, Smith WT, Glaudin V, Painter JR. Short-term cotherapy with clonazepam and fluoxetine: anxiety, sleep disturbance and core symptoms of depression. J Affect Disord. 2000;61:73–79. doi: 10.1016/S0165-0327(99)00195-0. [DOI] [PubMed] [Google Scholar]
- 97.Bech P, Krystal A, Walsh J, Rubens R, Caron J, Wessel T, Amato D, Roth T, McCall WV, Fava M. Analysis of individual items of the Hamilton depression scale in a study of eszopiclone/fluoxetine co-therapy. Eur Psychiatry. 2007;22(Suppl 1):S224. doi: 10.1016/j.eurpsy.2007.01.748. [DOI] [Google Scholar]
- 98.Brower KJ, McCammon RJ, Wojnar M, Ilgen MA, Wojnar J, Valenstein M. Prescription sleeping pills, insomnia, and suicidality in the National Comorbidity Survey Replication. J Clin Psychiatry. 2011;72:515–521. doi: 10.4088/JCP.09m05484gry. [DOI] [PubMed] [Google Scholar]
- 99.Carlsten A, Waern M. Are sedatives and hypnotics associated with increased suicide risk of suicide in the elderly? BMC Geriatr. 2009;9:20. doi: 10.1186/1471-2318-9-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Barbui C, Tansella M. Suicide prevention strategies and mental disorders. Epidemiol Psichiatr Soc. 2009;18:169–171. [PubMed] [Google Scholar]
- 101.Auger RR, Goodman SH, Silber MH, Krahn LE, Pankratz VS, Slocumb NL. Risks of high-dose stimulants in the treatment of disorders of excessive somnolence: a case-control study. Sleep. 2005;28:667–672. doi: 10.1093/sleep/28.6.667. [DOI] [PubMed] [Google Scholar]
- 102.Gangwisch JE, Babiss LA, Malaspina D, Turner JB, Zammit GK, Posner K. Earlier parental set bedtimes as a protective factor against depression and suicidal ideation. Sleep. 2010;33:97–106. doi: 10.1093/sleep/33.1.97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Selvi Y, Aydin A, Atli A, Boysan M, Selvi F, Besiroglu L. Chronotype differences in suicidal behavior and impulsivity among suicide attempters. Chronobiol Int. 2011;28:170–175. doi: 10.3109/07420528.2010.535938. [DOI] [PubMed] [Google Scholar]
- 104.Stanley M, Brown GM. Melatonin levels are reduced in the pineal glands of suicide victims. Psychopharmacol Bull. 1988;24:484–488. [PubMed] [Google Scholar]
- 105.Mendlewicz J. Disruption of the circadian timing systems: molecular mechanisms in mood disorders. CNS Drugs. 2009;23:15–26. doi: 10.2165/11318630-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 106.Violanti JM. Police suicide research: conflict and consensus. Int J Emerg Ment Health. 2008;10:299–307. [PubMed] [Google Scholar]
- 107.Woo JM, Postolache TT. The impact of work environment on mood disorders and suicide: evidence and implications. Int J Disabil Hum Dev. 2008;7:185–200. doi: 10.1515/IJDHD.2008.7.2.185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Alaräisänen A, Miettunen J, Lauronen E, Räsänen P, Isohanni M. Good school performance is a risk factor of suicide in psychoses: a 35-year follow up of the Northern Finland 1966 Birth Cohort. Acta Psychiatr Scand. 2006;114:357–362. doi: 10.1111/j.1600-0447.2006.00800.x. [DOI] [PubMed] [Google Scholar]
- 109.Johnson J, Wood AM, Gooding P, Taylor PJ, Tarrier N. Resilience to suicidality: the buffering hypothesis. Clin Psychol Rev. 2011;31:563–591. doi: 10.1016/j.cpr.2010.12.007. [DOI] [PubMed] [Google Scholar]
- 110.Espie CA, Inglis SJ, Harvey L, Tessier S. Insomniacs’ attributions. Psychometric properties of the dysfunctional beliefs and attitudes about sleep scale and the sleep disturbance questionnaire. J Psychosom Res. 2000;48:141–148. doi: 10.1016/S0022-3999(99)00090-2. [DOI] [PubMed] [Google Scholar]
- 111.Carney CE, Edinger JD, Manber R, Garson C, Segal ZV. Beliefs about sleep in disorders characterized by sleep and mood disturbance. J Psychosom Res. 2007;62:179–188. doi: 10.1016/j.jpsychores.2006.08.006. [DOI] [PubMed] [Google Scholar]
- 112.Taylor DJ, Mallory LJ, Lichstein KL, Durrence HH, Riedel BW, Bush AJ. Comorbidity of chronic insomnia with medical problems. Sleep. 2007;30:213–218. doi: 10.1093/sleep/30.2.213. [DOI] [PubMed] [Google Scholar]
- 113.Druss B, Pincus H. Suicidal ideation and suicide attempts in general medical illnesses. Arch Intern Med. 2000;160:1522–1526. doi: 10.1001/archinte.160.10.1522. [DOI] [PubMed] [Google Scholar]
- 114.Frank E, Swartz HA, Kupfer DJ. Interpersonal and social rhythm therapy: managing the chaos of bipolar disorder. Biol Psychiatry. 2000;48:593–604. doi: 10.1016/S0006-3223(00)00969-0. [DOI] [PubMed] [Google Scholar]
- 115.King AC, Oman RF, Brassington GS, Bliwise DL, Haskell WL. Moderate-intensity exercise and self-rated quality of sleep in older adults. A randomized controlled trial. JAMA. 1997;277:32–37. doi: 10.1001/jama.277.1.32. [DOI] [PubMed] [Google Scholar]
- 116.Passos GS, Poyares D, Santana MG, Garbuio SA, Tufik S, Mello MT. Effect of acute physical exercise on patients with chronic primary insomnia. J Clin Sleep Med. 2010;6:270–275. [PMC free article] [PubMed] [Google Scholar]
- 117.Reid KJ, Baron KG, Lu B, Naylor E, Wolfe L, Zee PC. Aerobic exercise improves self-reported sleep and quality of life in older adults with insomnia. Sleep Med. 2010;11:934–940. doi: 10.1016/j.sleep.2010.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Buman MP, Hekler EB, Bliwise DL, King AC. Moderators and mediators of exercise-induced objective sleep improvements in midlife and older adults with sleep complaints. Health Psychol. 2011. doi:10.1037/a0024293. [DOI] [PMC free article] [PubMed]
- 119.North TC, McCullagh P, Tran ZV. Effect of exercise on depression. Exerc Sport Sci Rev. 1990;18:379–415. doi: 10.1249/00003677-199001000-00016. [DOI] [PubMed] [Google Scholar]
- 120.Stathopoulou G, Powers MB, Berry AC, Smiths J, Otto MW. Exercise interventions for mental health: a quantitative and qualitative review. Clin Psychol Sci Pract. 2006;13:179–193. doi: 10.1111/j.1468-2850.2006.00021.x. [DOI] [Google Scholar]
- 121.Adams TB, Moore MT, Dye J. The relationship between physical activity and mental health in a national sample of college females. Women Health. 2007;45:69–85. doi: 10.1300/J013v45n01_05. [DOI] [PubMed] [Google Scholar]
- 122.Taliaferro LA, Rienzo BA, Pigg RM, Jr, Miller MD, Dodd VJ. Associations between physical activity and reduced rates of hopelessness, depression, and suicidal behavior among college students. J Am Coll Health. 2009;57:427–436. doi: 10.3200/JACH.57.4.427-436. [DOI] [PubMed] [Google Scholar]
- 123.Simon TR, Powell KE, Swann AC. Involvement in physical activity and risk for nearly lethal suicide attempts. Am J Prev Med. 2004;27:310–315. doi: 10.1016/j.amepre.2004.07.003. [DOI] [PubMed] [Google Scholar]
- 124.Andriessen K, Krysinska K. Can sports events affect suicidal behavior? A review of the literature and implications for prevention. Crisis. 2009;30:144–152. doi: 10.1027/0227-5910.30.3.144. [DOI] [PubMed] [Google Scholar]


